Interstitial nephritis
| Interstitial nephritis | |
|---|---|
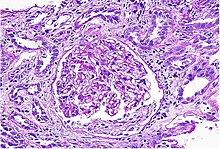 | |
| Acute Interstitial Nephritis on light microscopy | |
| Specialty | Nephrology |
Interstitial nephritis, also known as tubulointerstitial nephritis, is inflammation of the area of the kidney known as the interstitium, which consists of a collection of cells, extracellular matrix, and fluid surrounding the renal tubules.[1] In addition to providing a scaffolding support for the tubular architecture, the interstitium has been shown to participate in the fluid and electrolyte exchange as well as endocrine functions of the kidney.[1] There are a variety of known factors that can provoke the inflammatory process within the renal interstitium, including pharmacologic, environmental, infectious and systemic disease contributors. The spectrum of disease presentation can range from an acute process to a chronic condition with progressive tubular cell damage and renal dysfunction.
Signs and symptoms
Interstitial nephritis may present with a variety of signs and symptoms, many of these nonspecific. Fever is the most common, occurring in 30-50% of patients, particularly those with drug-induced interstitial nephritis.[2] Other general symptoms that occur with variable frequency include nausea, vomiting, fatigue, lack of appetite, and weight loss. More specific symptoms, such as flank pain, pain with urination, and visible blood in the urine, as well as signs like hypertension can be helpful in increasing suspicion for the diagnosis.[3] The "classic" triad of symptoms reported in early documented cases consisted of rash, joint pain, and increased eosinophils in the blood; however, more recent epidemiology suggests that this grouping of symptoms only occurs in a small minority (5-10%) of patients.[4]
Causes
Common causes include infection, or reaction to medication such as an analgesic or antibiotics such as methicillin (meticillin). Reaction to medications causes 71%[5] to 92%[6] of cases.
Drugs
| Class | Examples |
|---|---|
| Antibiotic | β-lactams (e.g. penicillins, cephalosporins), sulfonamides (e.g. trimethoprim-sulfamethoxazole), fluoroquinolones (e.g. ciprofloxacin), macrolides (e.g. vancomycin, erythromycin), anti-tuberculins (e.g. rifampin, ethambutol), chloramphenicol |
| Antiviral | Acyclovir, atazanavir, abacavir, indinavir |
| Pain | Nonsteroidal antiinflammatory drugs (e.g. ibuprofen, naproxen), selective COX-2 inhibitors (e.g. celecoxib) |
| Gastrointestinal | Proton pump inhibitors (e.g. omeprazole, lansoprazole), H2-receptor blockers (e.g. cimetidine), 5-aminosalicylates (e.g. mesalamine) |
| Antiseizure | Phenytoin, carbamazepine, phenobarbital |
| Diuretic | Hydrochlorothiazide, furosemide, triamterene, chlorthalidone |
| Chemotherapy | Tyrosine kinase inhibitors (e.g. sunitinib), checkpoint inhibitors (e.g. ipilimumab, nivolumab, pembrolizumab, atezolizumab) |
| Other | Allopurinol, Chinese herbs |
This disease is also caused by other diseases and toxins that damage the kidney. Both acute and chronic tubulointerstitial nephritis can be caused by a bacterial infection in the kidneys known as pyelonephritis, but the most common cause is by an adverse reaction to a medication. The medications that are known to cause this sort of reaction are β-lactam antibiotics such as penicillin[8] and cephalexin, and nonsteroidal anti-inflammatory drugs (aspirin less frequently than others), as well as proton-pump inhibitors, rifampicin, sulfa medications, fluoroquinolones, diuretics, allopurinol, mesalamine, and phenytoin. The time between exposure to the drug and the development of acute tubulointerstitial nephritis can be anywhere from 5 days to 5 months (fenoprofen-induced).
Diagnosis
At times, there are no symptoms of this disease, but when they do occur they are widely varied and can occur rapidly or gradually.[5][9][10][11][12] When caused by an allergic reaction, the symptoms of acute tubulointerstitial nephritis are fever (27% of patients),[5] rash (15% of patients),[5] and enlarged kidneys. Some people experience dysuria, and lower back pain. In chronic tubulointerstitial nephritis the patient can experience symptoms such as nausea, vomiting, fatigue, and weight loss. Other conditions that may develop include a high concentration of potassium in the blood, metabolic acidosis, and kidney failure.
Blood tests
About 23% of patients have a high level of eosinophils in the blood.[5]
Urinary findings
Urinary findings include:
- Eosinophiluria: Original studies with Methicillin-induced AIN showed sensitivity of 67% and specificity of 83%.[9][13] The sensitivity is higher in patients with interstitial nephritis induced by methicillin or when the Hansel's stain is used. However, a 2013 study showed that the sensitivity and specificity of urine eosinophil testing are 35.6% and 68% respectively.[14][15]
- Isosthenuria[16]
- Blood in the urine and occasional RBC casts[17]
- Sterile pyuria: white blood cells and no bacteria
- Nephrotic-range amount of protein in the urine may be seen with NSAID-associated AIN
Pathology
While non-invasive patient evaluation (physical examination, blood and urine testing, imaging studies) can be suggestive, the only way to definitively diagnosis interstitial nephritis is with a tissue diagnosis obtained by kidney biopsy. Pathologic examination will reveal the presence of interstitial edema and inflammatory infiltration with various while blood cells, including neutrophils, eosinophils, and lymphocytes. Generally, blood vessels and glomeruli are not affected. Electron microscopy shows mitochondrial damage in the tubular epithelial cells, vacuoles in the cytoplasm, and enlarged endoplasmic reticulum.[18]
Gallium scan
The sensitivity of an abnormal gallium scan has been reported to range from 60%[19] to 100%.[20]
Treatment
Treatment consists of addressing the cause, such as by removing an offending drug. There is no clear evidence that corticosteroids help.[6] Nutrition therapy consists of adequate fluid intake, which can require several liters of extra fluid.[21]
Prognosis
The kidneys are the only body system that are directly affected by tubulointerstitial nephritis. Kidney function is usually reduced; the kidneys can be just slightly dysfunctional, or fail completely.
In chronic tubulointerstitial nephritis, the most serious long-term effect is kidney failure. When the proximal tubule is injured, sodium, potassium, bicarbonate, uric acid, and phosphate reabsorption may be reduced or changed, resulting in low bicarbonate, known as metabolic acidosis, low potassium, low uric acid known as hypouricemia, and low phosphate known as hypophosphatemia. Damage to the distal tubule may cause loss of urine-concentrating ability and polyuria.
In most cases of acute tubulointerstitial nephritis, the function of the kidneys will return after the harmful drug is not taken anymore, or when the underlying disease is cured by treatment. If the illness is caused by an allergic reaction, a corticosteroid may speed the recovery kidney function; however, this is often not the case.
Chronic tubulointerstitial nephritis has no cure. Some patients may require dialysis. Eventually, a kidney transplant may be needed.
Epidemiology
Interstitial nephritis is uncommon (<1% incidence) in patients without any symptoms but occurs in about 10-15% of hospitalized patients with acute kidney injury of unknown cause.[2] While it can occur in patients of all ages, it is more common in elderly patients, perhaps due to increased exposure to drugs and other triggering causes.[2]
References
- ^ a b Zeisberg, Michael; Kalluri, Reghu (October 2015). [www.cjasn.org "Physiology of the Renal Interstitium"]. Clinical Journal of the American Society of Nephrology. 10: 1831–1840. doi:10.2215/CJN.00640114.
{{cite journal}}: Check|url=value (help) - ^ a b c d Brewster, Ursula C.; Rastegar, Asghar (2014), "Acute Interstitial Nephritis", National Kidney Foundation Primer on Kidney Diseases, Elsevier, pp. 312–317, ISBN 9781455746170, retrieved 2018-12-10
- ^ Meyers, Catherine M. (2014), "Chronic Tubulointerstitial Disease", National Kidney Foundation Primer on Kidney Diseases, Elsevier, pp. 390–396, ISBN 9781455746170, retrieved 2018-12-10
- ^ Brewster, Ursula C.; Rastegar, Asghar (2014), "Acute Interstitial Nephritis", National Kidney Foundation Primer on Kidney Diseases, Elsevier, pp. 312–317, ISBN 9781455746170, retrieved 2018-12-10
- ^ a b c d e Baker R, Pusey C (2004). "The changing profile of acute tubulointerstitial nephritis". Nephrol Dial Transplant. 19 (1): 8–11. doi:10.1093/ndt/gfg464. PMID 14671029.
- ^ a b Clarkson M, Giblin L, O'Connell F, O'Kelly P, Walshe J, Conlon P, O'Meara Y, Dormon A, Campbell E, Donohoe J (2004). "Acute interstitial nephritis: clinical features and response to corticosteroid therapy". Nephrol Dial Transplant. 19 (11): 2778–83. doi:10.1093/ndt/gfh485. PMID 15340098.
- ^ Praga, Manuel; Appel, Gerald (2018-11-01). "Clinical manifestations and diagnosis of acute interstitial nephritis". UpToDate. Retrieved 2018-12-10.
{{cite web}}: Cite has empty unknown parameters:|dead-url=and|middle name=(help) - ^ Ohlsson, Arne; Shah, Vibhuti S; Ohlsson, Arne (2014). "Intrapartum antibiotics for known maternal Group B streptococcal colonization". doi:10.1002/14651858.CD007467.pub4.
{{cite journal}}: Cite journal requires|journal=(help) - ^ a b Rossert J (2001). "Drug-induced acute interstitial nephritis". Kidney Int. 60 (2): 804–17. doi:10.1046/j.1523-1755.2001.060002804.x. PMID 11473672.
- ^ Pusey C, Saltissi D, Bloodworth L, Rainford D, Christie J (1983). "Drug associated acute interstitial nephritis: clinical and pathological features and the response to high dose steroid therapy". Q J Med. 52 (206): 194–211. PMID 6604293.
- ^ Handa S (1986). "Drug-induced acute interstitial nephritis: report of 10 cases". CMAJ. 135 (11): 1278–81. PMC 1491384. PMID 3779558.
- ^ Buysen J, Houthoff H, Krediet R, Arisz L (1990). "Acute interstitial nephritis: a clinical and morphological study in 27 patients". Nephrol Dial Transplant. 5 (2): 94–9. doi:10.1093/ndt/5.2.94. PMID 2113219.
- ^ Schwarz A, Krause P, Kunzendorf U, Keller F, Distler A (2000). "The outcome of acute interstitial nephritis risk factors for the transition from acute to chronic interstitial nephritis". Clin Nephrol. 54 (3): 179–90. PMID 11020015.
- ^ Muriithi, A.K., S.H. Nasr, and N. Leung, Utility of urine eosinophils in the diagnosis of acute interstitial nephritis. Clinical Journal of The American Society of Nephrology: CJASN, 2013. 8(11): p. 1857-62.
- ^ Perazella, M.A. and A.S. Bomback, Urinary eosinophils in AIN: farewell to an old biomarker? Clinical Journal of The American Society of Nephrology: CJASN, 2013. 8(11): p. 1841-3.
- ^ Lins R, Verpooten G, De Clerck D, De Broe M (1986). "Urinary indices in acute interstitial nephritis". Clin Nephrol. 26 (3): 131–3. PMID 3769228.
- ^ Fogazzi, G.B., et al., Urinary sediment findings in acute interstitial nephritis. American Journal of Kidney Diseases, 2012. 60(2): p. 330-332
- ^ Alon, Uri S. (2015-11-12), "Pediatric Tubulointerstitial Nephritis", Pediatric Nephrology, Springer Berlin Heidelberg, pp. 1407–1428, ISBN 9783662435953, retrieved 2018-12-10
- ^ Graham G, Lundy M, Moreno A (1983). "Failure of Gallium-67 scintigraphy to identify reliably noninfectious interstitial nephritis: concise communication". J Nucl Med. 24 (7): 568–70. PMID 6864309.
- ^ Linton A, Richmond J, Clark W, Lindsay R, Driedger A, Lamki L (1985). "Gallium67 scintigraphy in the diagnosis of acute renal disease". Clin Nephrol. 24 (2): 84–7. PMID 3862487.
- ^ Mahan KL, Escott-Stump S (2003). "39". In Alexopolos Y (ed.). Krause's Food, Nutrition, & Diet Therapy (11th ed.). Philadelphia Pennsylvania: Saunders. p. 968. ISBN 0-7216-9784-4.
