Transitional cell carcinoma
| Transitional cell carcinoma | |
|---|---|
| Specialty | Oncology |
Transitional cell carcinoma (TCC, also urothelial cell carcinoma or UCC) is a type of cancer that typically occurs in the urinary system: the kidney, urinary bladder, and accessory organs. It is the most common type of bladder cancer and cancer of the ureter, urethra, and urachus. It is the second most common type of kidney cancer, but accounts for only 5% to 10% of all primary renal malignant tumors.
TCC arises from the transitional epithelium, a tissue lining the inner surface of these hollow organs.[1]
When the term "urothelial" is used, it specifically refers to a carcinoma of the urothelium, meaning a TCC of the urinary system.
Signs and symptoms
Signs and symptoms depend on the location and extent of the cancer: see for example Bladder cancer.
Causes
- certain drugs such as cyclophosphamide and phenacetin are known to predispose to bladder TCC.[2]
- long-term usage of analgesics
- radiation exposure
- somatic mutation such as deletion of Chromosome 9p,9q,11p,17p,13q,14q and over expression of RAS (oncogene) and epidermal growth factor receptor (EGFR)
- cigarette smoke
- naphthylamines and aniline dyes
Pathology
TCCs are often multifocal, with 30-40% of patients having more than one tumor at diagnosis. The pattern of growth of TCCs can be papillary, sessile (flat) or carcinoma-in-situ (CIS).
The most common site of TCC metastasis outside the pelvis is bone (35%); of these bone metastases, 40% are in the spine.[3]
Terminology
Transitional refers to the histological subtype of the cancerous cells as seen under a microscope.
Classification
The 1973 WHO grading system for TCCs (papilloma, G1, G2 or G3) is most commonly used despite being superseded by the 2004 WHO [4] grading (papillary neoplasm of low malignant potential (PNLMP), low grade and high grade papillary carcinoma).
Treatment
Transitional cell carcinoma (TCC) can be very difficult to treat. Treatment for localized stage TCC is surgical resection of the tumor, but reccurrence is common. Some patients are given mitomycin (which is a chemotherapeutic drug) into the bladder either as a one-off dose in the immediate post operative period (within 24 hrs) or a few weeks after the surgery as a six dose regimen.
Localized/ early TCC can also be treated with infusions of BCG into the bladder. These are given weekly for either 6 weeks (induction course) or 3 weeks(maintenance / booster dose). Side effects include a small chance of developing systemic Tuberculosis (T.B.) or the patient becoming sensitized to the BCG causing severe intolerance and a possible reduction in bladder volume due to scarring.
In patients with evidence of early muscular invasion, radical curative surgery in the form of a cysto-prostatectomy usually with lymph node sampling can also be performed. In such patients, a bowel loop is often used to create either a "neo-bladder" or an "ileal conduit" which act as a place for the storage of urine before it is evacuated from the body either via the urethra or a urostomy respectively.
Chemotherapy for TCC consists of the MVAC regimen (methotrexate, vinblastine, adriamycin and cisplatin).[citation needed]
Associations
It is associated with phenacetin, aniline dyes, cyclophosphamide, smoking, and those who drink excessive alcohol. It is also associated with hereditary nonpolyposis colorectal cancer.[citation needed]
Prostate
TCC can also be associated with the prostate.[5][6]
Additional images
-
Histopathology of urothelial carcinoma of the urinary bladder, showing a nested pattern of invasion. Transurethral biopsy. Hematoxylin and eosin.
-
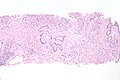
Histopathology of urothelial carcinoma of the urinary bladder.
-
Histopathology of urothelial carcinoma of the urinary bladder.
-
Micrograph of urethral urothelial cell carcinoma. H&E stain.
References
- ^ "transitional cell carcinoma" at Dorland's Medical Dictionary
- ^ Colin P, Koenig P, Ouzzane A, Berthon N, Villers A, Biserte J, Roupret M (2009). "Environmental factors involved in carcinogenesis of urothelial cell carcinomas of the upper urinary tract". BJU International. 104 (10): 1436–40. doi:10.1111/j.1464-410X.2009.08838.x. PMID 19689473.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Punyavoravut V, Nelson SD (1999). "Diffuse bony metastasis from transitional cell carcinoma of urinary bladder: a case report and review of literature". Journal of the Medical Association of Thailand. 82 (8): 839–43. PMID 10511795.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Sauter G, Algaba F, Amin MB, Busch C, Cheville J, Gasser T, Grignon D, Hofstaedter F, Lopez-Beltran A, Epstein JI. Noninvasive urothelial neoplasias: WHO classification of noninvasive papillary urothelial tumors. In World Health Organization classification of tumors. Pathology and genetics of tumors of the urinary system and male genital organs. Eble JN, Epstein JI, Sesterhenn I (eds): Lyon, IARCC Press, p. 110, 2004
- ^ Walsh DL, Chang SS (2009). "Dilemmas in the treatment of urothelial cancers of the prostate". Urologic Oncology. 27 (4): 352–7. doi:10.1016/j.urolonc.2007.12.010. PMID 18439852.
- ^ Njinou Ngninkeu B, Lorge F, Moulin P, Jamart J, Van Cangh PJ (2003). "Transitional cell carcinoma involving the prostate: a clinicopathological retrospective study of 76 cases". The Journal of Urology. 169 (1): 149–52. doi:10.1097/01.ju.0000042810.43380.36. PMID 12478124.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link)