Placenta: Difference between revisions
m Reverted edits by 70.137.153.252 (talk) to last revision by ZéroBot (HG) |
Tag: shouting |
||
| Line 22: | Line 22: | ||
==Structure== |
==Structure== |
||
In humans, the placenta averages 22 cm (9 inch) in length and 2–2.5 cm (0.8–1 inch) in thickness (greatest thickness at the center and become thinner peripherally). It typically weighs approximately 500 grams (1 lb). It has a dark reddish-blue or maroon color. It connects to the fetus by an [[umbilical cord]] of approximately 55–60 cm (22–24 inch) in length that contains two arteries and one vein.<ref>[http://www.aafp.org/afp/980301ap/yetter.html Examination of the placenta]</ref> The umbilical cord inserts into the chorionic plate (has an eccentric attachment). Vessels branch out over the surface of the placenta and further divide to form a network covered by a thin layer of cells. This results in the formation of villous tree structures. On the maternal side, these villous tree structures are grouped into lobules called cotyledons. In humans the placenta usually has a disc shape, but size varies vastly between different mammalian species.<ref>http://www.vivo.colostate.edu/hbooks/pathphys/reprod/placenta/structure.html Placental Structure and Classification</ref> |
In humans, the placenta averages 22 cm (9 inch) in length and 2–2.5 cm (0.8–1 inch) in thickness (greatest thickness at the center and become thinner peripherally). It typically weighs approximately 500 grams (1 lb). It has a dark reddish-blue or maroon color. It connects to the fetus by an [[umbilical cord]] of approximately 55–60 cm (22–24 inch) in length that contains two arteries and one vein.<ref>[http://www.aafp.org/afp/980301ap/yetter.html Examination of the placenta]</ref> The umbilical cord inserts into the chorionic plate (has an eccentric attachment). Vessels branch out over the surface of the placenta and further divide to form a network covered by a thin layer of cells. This results in the formation of villous tree structures. On the maternal side, these villous tree structures are grouped into lobules called cotyledons. In humans the placenta usually has a disc shape, but size varies vastly between different mammalian species.<ref>http://www.vivo.colostate.edu/hbooks/pathphys/reprod/placenta/structure.html Placental Structure and Classification</ref> |
||
ROY MORRIS LOVES PLACENTAS....HE HAS A FROZEN ONE AT HOME |
|||
==Development== |
==Development== |
||
Revision as of 05:47, 15 June 2011
| Placenta | |
|---|---|
 Placenta | |
| Details | |
| Precursor | decidua basalis, chorion frondosum |
| Identifiers | |
| MeSH | D010920 |
| TE | E5.11.3.1.1.0.5 |
| Anatomical terminology | |
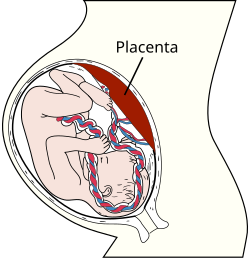
The placenta is an organ that connects the developing fetus to the uterine wall to allow nutrient uptake, waste elimination, and gas exchange via the mother's blood supply. Placentas are a defining characteristic of eutherian or "placental" mammals, but are also found in some snakes and lizards with varying levels of development up to mammalian levels.[1] The word placenta comes from the Latin for cake, from Greek plakóenta/plakoúnta, accusative of plakóeis/plakoús – πλακόεις, πλακούς, "flat, slab-like",[2] in reference to its round, flat appearance in humans. Prototherial (egg-laying) and metatherial (marsupial) mammals produce a choriovitelline placenta that, while connected to the uterine wall, provides nutrients mainly derived from the egg sac. The placenta develops from the same sperm and egg cells that form the fetus, and functions as a fetomaternal organ with two components, the fetal part (Chorion frondosum), and the maternal part (Decidua basalis).
Structure
In humans, the placenta averages 22 cm (9 inch) in length and 2–2.5 cm (0.8–1 inch) in thickness (greatest thickness at the center and become thinner peripherally). It typically weighs approximately 500 grams (1 lb). It has a dark reddish-blue or maroon color. It connects to the fetus by an umbilical cord of approximately 55–60 cm (22–24 inch) in length that contains two arteries and one vein.[3] The umbilical cord inserts into the chorionic plate (has an eccentric attachment). Vessels branch out over the surface of the placenta and further divide to form a network covered by a thin layer of cells. This results in the formation of villous tree structures. On the maternal side, these villous tree structures are grouped into lobules called cotyledons. In humans the placenta usually has a disc shape, but size varies vastly between different mammalian species.[4] ROY MORRIS LOVES PLACENTAS....HE HAS A FROZEN ONE AT HOME
Development

The placenta begins to develop upon implantation of the blastocyst into the maternal endometrium. The outer layer of the blastocyst becomes the trophoblast which forms the outer layer of the placenta. This outer layer is divided into two further layers: the underlying cytotrophoblast layer and the overlying syncytiotrophoblast layer. The syncytiotrophoblast is a multinucleated continuous cell layer which covers the surface of the placenta. It forms as a result of differentiation and fusion of the underlying cytotrophoblast cells, a process which continues throughout placental development. The syncytiotrophoblast (otherwise known as syncytium), thereby contributes to the barrier function of the placenta.
The placenta grows throughout pregnancy. Development of the maternal blood supply to the placenta is suggested to be complete by the end of the first trimester of pregnancy (approximately 12–13 weeks).
Placental circulation
Maternal placental circulation
In preparation for implantation, the uterine endometrium undergoes 'decidualisation'. Spiral arteries in decidua are remodelled so that they become less convoluted and their diameter is increased. This increases maternal blood flow to the placenta and also decreases resistance so that blood flow is increased. The relatively high pressure as the maternal blood enters the intervillous space through these spiral arteries bathes the villi in blood. An exchange of gases takes place. As the pressure decreases, the deoxygenated blood flows back through the endometrial veins.
Maternal blood flow is approx 600–700 ml/min at term.
Fetoplacental circulation
Deoxygenated fetal blood passes through umbilical arteries to the placenta. At the junction of umbilical cord and placenta, the umbilical arteries branch radially to form chorionic arteries. Chorionic arteries, in turn, branch into cotyledon arteries. In the villi, these vessels eventually branch to form an extensive arteriocapillary venous system, bringing the fetal blood extremely close to the maternal blood; but no intermingling of fetal and maternal blood occurs ("placental barrier"[5]).
Endothelin and prostanoids cause vasoconstriction in placental arteries, while nitric oxide vasodilation.[6] On the other hand, there is no neural vascular regulation, and catecholamines have only little effect.[6]
Functions
Nutrition and immunity
The perfusion of the intervillous spaces of the placenta with maternal blood allows the transfer of nutrients and oxygen from the mother to the fetus and the transfer of waste products and carbon dioxide back from the fetus to the mother. Nutrient transfer to the fetus is both actively and passively mediated by proteins called nutrient transporters that are expressed within placental cells[citation needed].
Adverse pregnancy situations, such as those involving maternal diabetes or obesity, can increase or decrease levels of nutrient transporters in the placenta resulting in overgrowth or restricted growth of the fetus[citation needed].
IgG antibodies can pass through the human placenta, thereby providing protection to the fetus in uterus.[7]
Endocrine function
In humans, aside from serving as the conduit for oxygen and nutrients for fetus, the placenta secretes hormones (secreted by syncytial layer/syncytiotrophoblast of chorionic villi) that are important during pregnancy.
Hormones:
Human Chorionic Gonadotropin (hCG). The first placental hormone produced is hCG, which can be found in maternal blood and urine as early as the first missed menstrual period (shortly after implantation has occurred) through about the 100th day of pregnancy. This is the hormone analyzed by pregnancy test; a false-negative result from a pregnancy test may be obtained before or after this period. Women's blood serum will be completely negative for hCG by one to two weeks after birth. hCG testing is proof that all placental tissue is delivered. hCG is only present during pregnancy because it is secreted by the placenta, which is present only[8] during pregnancy. hCG also ensures that the corpus luteum continues to secrete progesterone and estrogen. Progesterone is very important during pregnancy because when its secretion decreases, the endometrial lining will slough off and pregnancy will be lost. hCG suppresses the maternal immunologic response so that placenta is not rejected.
Human Placental Lactogen (hPL [Human Chorionic Somatomammotropin]). This hormone is lactogenic and growth-promoting properties. It promotes mammary gland growth in preparation for lactation in the mother. It also regulates maternal glucose, protein, fat levels so that this is always available to the fetus.
Estrogen is referred to as the "hormone of women" because it stimulates the development of secondary female sex characteristics. It contributes to the woman's mammary gland development in preparation for lactation and stimulates uterine growth to accommodate growing fetus.
Progesterone is necessary to maintain endometrial lining of the uterus during pregnancy. This hormone prevents preterm labor by reducing myometrial contraction. Levels of progesterone are high during pregnancy.
Cloaking from immune system of mother
The placenta and fetus may be regarded as a foreign allograft inside the mother, and thus must evade from attack by the mother's immune system.
For this purpose, the placenta uses several mechanisms:
- It secretes Neurokinin B containing phosphocholine molecules. This is the same mechanism used by parasitic nematodes to avoid detection by the immune system of their host.[9]
- Also, there is presence of small lymphocytic suppressor cells in the fetus that inhibit maternal cytotoxic T cells by inhibiting the response to interleukin 2.[10]
However, the placental barrier is not the sole means to evade the immune system, as foreign fetal cells also persist in the maternal circulation, on the other side of the placental barrier.[11]
Other functions
The placenta also provides a reservoir of blood for the fetus, delivering blood to it in case of hypotension and vice versa, comparable to a capacitor.[12]
Birth
Placental expulsion begins as a physiological separation from the wall of the uterus. The period from just after the fetus is expelled until just after the placenta is expelled is called the third stage of labor. The placenta is usually expelled within 15–30 minutes of the baby being born.
Placental expulsion can be managed actively, for example by giving oxytocin via intramuscular injection followed by cord traction to assist in delivering the placenta. Alternatively, it can be managed expectantly, allowing the placenta to be expelled without medical assistance. A Cochrane database study[13] suggests that blood loss and the risk of postpartum bleeding will be reduced in women offered active management of the third stage of labour (needs updating).
Pathology

Numerous pathologies can affect the placenta.
- Placenta accreta (when the placenta implants too deeply, into actual muscle of uterine wall)
- Placenta praevia
- Placental abruption/abruptio placentae
Infections involving the placenta:
- Placentitis, such as the TORCH infections.
- Chorioamnionitis.
Cultural practices and beliefs
The placenta often plays an important role in various cultures, with many societies conducting rituals regarding its disposal. In the Western world, the placenta is most often incinerated.[14]
Some cultures bury the placenta for various reasons. The Māori of New Zealand traditionally bury the placenta from a newborn child to emphasize the relationship between humans and the earth.[15] Similarly, the Navajo bury the placenta and umbilical cord at a specially chosen site,[16] particularly if the baby dies during birth.[17] In Cambodia and Costa Rica, burial of the placenta is believed to protect and ensure the health of the baby and the mother.[18] If a mother dies in childbirth, the Aymara of Bolivia bury the placenta in a secret place so that the mother's spirit will not return to claim her baby's life.[19]
The placenta is believed by some communities to have power over the lives of the baby or its parents. The Kwakiutl of British Columbia bury girls' placentas to give the girl skill in digging clams, and expose boys' placentas to ravens to encourage future prophetic visions. In Turkey, the proper disposal of the placenta and umbilical cord is believed to promote devoutness in the child later in life. In Ukraine, Transylvania, and Japan, interaction with a disposed placenta is thought to influence the parents' future fertility.
Several cultures believe the placenta to be or have been alive, often a relative of the baby. Nepalese think of the placenta as a friend of the baby's; Malaysian Orang Asli regard it as the baby's older sibling. The Ibo of Nigeria consider the placenta the deceased twin of the baby, and conduct full funeral rites for it.[18] Native Hawaiians believe that the placenta is a part of the baby, and traditionally plant it with a tree which can then grow alongside the child.[14]
In some cultures, the placenta is eaten, a practice known as placentophagy. In some eastern cultures, such as China and Hong Kong, the placenta is thought to be healthful and is used in medicine and various health products.[20]
Additional images
-
Fetus of about 8 weeks, enclosed in the amnion. Magnified a little over two diameters.
-
Picture of freshly delivered placenta and umbilical cord wrapped around Kelly clamps
-
Fresh human placenta
-
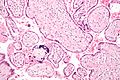
Micrograph of CMV placentitis.
See also
References
- ^ Pough et al. 1992. Herpetology: Third Edition. Pearson Prentice Hall:Pearson Education, Inc., 2002.
- ^ Henry George Liddell, Robert Scott, "A Greek-English Lexicon", at Perseus
- ^ Examination of the placenta
- ^ http://www.vivo.colostate.edu/hbooks/pathphys/reprod/placenta/structure.html Placental Structure and Classification
- ^ Placental blood circulation
- ^ a b Attention: This template ({{cite doi}}) is deprecated. To cite the publication identified by doi:10.1002/pd.1062, please use {{cite journal}} (if it was published in a bona fide academic journal, otherwise {{cite report}} with
|doi=10.1002/pd.1062instead. - ^ Simister, N.E., and Story, C.M. 1997. "Human placental Fc receptors and the transmission of antibodies from mother to fetus." Journal of Reproductive Immunology 37: 1-23.
- ^ Pillitteri, Adele(2010). Maternal and Child Health Nursing(6th Edition[Philippine Edition]): Lippincott Williams & Wilkins
- ^ "Placenta 'fools body's defences'". BBC News. 10 November 2007.
- ^ Clark DA, Chaput A, Tutton D (1986). "Active suppression of host-vs-graft reaction in pregnant mice. VII. Spontaneous abortion of allogeneic CBA/J x DBA/2 fetuses in the uterus of CBA/J mice correlates with deficient non-T suppressor cell activity". J. Immunol. 136 (5): 1668–75. PMID 2936806.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Williams Z, Zepf D, Longtine J; et al. (2008). "Foreign fetal cells persist in the maternal circulation". Fertil. Steril. 91 (6): 2593–5. doi:10.1016/j.fertnstert.2008.02.008. PMID 18384774.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 11299282, please use {{cite journal}} with
|pmid=11299282instead. - ^ Attention: This template ({{cite doi}}) is deprecated. To cite the publication identified by doi:10.1002/14651858.CD000007, please use {{cite journal}} (if it was published in a bona fide academic journal, otherwise {{cite report}} with
|doi=10.1002/14651858.CD000007instead. - ^ a b "Why eat a placenta?". BBC. 18 April 2006. Retrieved 8 January 2008.
- ^ Metge, Joan. 2005. "Working in/Playing with three languages: English, Te Reo Maori, and Maori Bod Language." In Sites N.S vol. 2, No 2:83-90.
- ^ Francisco, Edna (3 December 2004). "Bridging the Cultural Divide in Medicine". Minority Scientists Network. Retrieved 7 January 2008.
- ^ Shepardson, Mary (1978). "Changes in Navajo Mortuary Practices and Beliefs". American Indian Quarterly. University of Nebraska Press. Retrieved 7 January 2008. [dead link]
- ^ a b Buckley, Sarah J. "Placenta Rituals and Folklore from around the World". Mothering. Archived from the original on 6 January 2008. Retrieved 7 January 2008.
- ^ Davenport, Ann (2005). "The Love Offer". Johns Hopkins Magazine. Retrieved 7 January 2008.
{{cite web}}: Unknown parameter|month=ignored (help) - ^ Falcao, Ronnie. "Medicinal Uses of the Placenta". Retrieved 25 November 2008.
External links
- Additional Human placenta photography [1]
- The Placenta, gynob.com, with quotes from Williams Obstetrics, 18th Edition, F. Gary Cunningham, M.D., Paul C. MacDonald, M.D., Norman F. Grant, M.D., Appleton & Lange, Publishers.