Oral rehydration therapy: Difference between revisions
←Replaced content with 'hi' |
Willking1979 (talk | contribs) m Reverted edits by 24.14.123.240 to last revision by Chaldor (HG) |
||
| Line 1: | Line 1: | ||
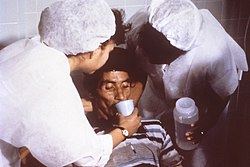
[[Image:Cholera rehydration nurses.jpg|right|thumb|250px|Nurses encouraging a patient to drink an Oral Rehydration Solution to combat dehydration caused by cholera.]] |
|||
hi |
|||
'''Oral rehydration therapy''', (also '''ORT''', '''oral rehydration salts''' or '''solutions (ORS)''', '''oral electrolyte'''), is a simple, cheap, and effective treatment for [[dehydration]] associated with [[diarrhea]], particularly [[gastroenteritis]], such as that caused by [[cholera]] or [[rotavirus]]. ORT consists of a [[solution]] of [[salt]]s and [[sugars]] which is [[Route of administration#Enteral|administered orally]]. It is used around the world, but is most important in the [[developing country|developing world]], where it saves millions of children from death due to [[diarrhea]]—the second leading cause of death in children under five.<ref>[http://www.unicef.org/publications/index_42623.html UNICEF. State of the World's Children 2008.]</ref> |
|||
== History == |
|||
Prescriptions from the ancient physician [[Sushruta]] date back over 2500 years with treatment of acute diarrhea with [[rice]] water, [[coconut water|coconut juice]], and [[carrot]] soup. However, this knowledge did not carry over to the Western world, as dehydration was found to be the major cause of death secondary to the 1829 cholera pandemic in Russia and Western Europe. In 1831, [[William Brooke O'Shaughnessy|William O'Shaughnessy]] noted the loss of water and salt in the stool of cholera patients and prescribed [[Intravenous therapy|intravenous fluid therapy]] to compensate. The results were remarkable, as patients who were on the brink of death from dehydration recovered. The mortality rate of cholera dropped from 70% to 40% with the use of [[Tonicity#Hypertonicity|hypertonic]] IV solutions.<ref name=guerrant_ort_history>{{cite journal |last=Guerrant |first=Richard L.|coauthors=Benedito A Carneiro-Filho, Rebecca A. Dillingham |year=2003 |month=August |title=Cholera, diarrhea, and oral rehydration therapy: triumph and indictment |journal=Clinical infectious diseases |volume=37 |issue=3 |pages=398-405 |pmid=12884154 |url=http://www.journals.uchicago.edu/doi/abs/10.1086/376619 |accessdate=2008-07-15}}</ref> |
|||
[[Robert Cade]], Dana Shires, Harry James Free, and Alejandro de Quesada were the medical researchers at the [[University of Florida]] who created the original Gatorade thirst quencher in 1965.<ref name=born>{{cite web |url=http://www.gatorade.com/history/born_in_the_lab/ |title=Born in the Lab |publisher=Gatorade |accessdate=2008-11-22}}</ref> The [[Florida Gators|Gators]] football coach, [[Ray Graves]], was frustrated with the performance of his players during the hot summer football practices, and asked the team doctor, one of Cade’s associates, for his insight. Cade and his research team came across the unique mix of water, [[sodium]], [[sugar]], [[potassium]], [[phosphate]], and lemon juice that is now known as Gatorade in honor of the football team, the Gators. |
|||
The football team credited Gatorade with their first [[Orange Bowl (game)|Orange Bowl]] win over the [[Georgia Institute of Technology|Georgia Tech]] [[Georgia Tech Yellow Jackets|Yellow Jackets]] in 1967, and the drink became an instant phenomenon. The Yellow Jackets coach [[Bud Carson]], when asked why they lost, replied: "We didn’t have Gatorade. That made the difference."<ref name="inventions">{{cite web|title=''Football Inventions That Shaped the Modern Game''|url=http://www.inventhelp.com/Football_Inventions.asp|date=2007-09-06|accessdate=2007-09-06}}</ref> Contrary to popular belief, the University of Florida did not come up with the sports drink that is now known as Gatorade. The team doctor for the FSU football team, Dr. R.A. Johnson, began producing a sports drink that he called "Seminole Firewater" as early as 1962. Dr. Johnson blended sugar and lime flavoring with electrolytes (salts) to help keep the players hydrated and to prevent cramping. In 1964 at an annual Seminar of Collegiate sports physicians and athletic trainers held in Tallahassee, Fl., a representative from the University of Florida found out about the discovery that sodium and potassium keeps athletes better hydrated because it gives back to the body what is lost through sweat. They returned to Gainesville and, after being tested on the UF football players, the name "Gatorade" was given. The University of Florida requested a certified patent in 1967 for the drink that Dr. Johnson had freely shared with the public. |
|||
Another pioneering researcher of Oral Rehydration Therapy was [[Hemendra Nath Chatterjee]], a Bengali scientist from West Bengal, India. Chatterjee started research on blood of Cholera <ref>http://www.journals.elsevierhealth.com/periodicals/trstmh/article/PII0035920346900430/abstract?showOmimLinks=true</ref>patient in 1946. In 1951 he discovered that in [[Bengal]] villages small epidemic of cholera is is treated by raw leaf juice of a common plant of Bengal called ''pathorchur'' (''[[Coleus aromaticus]]'')<ref>http://www.pubmedcentral.nih.gov/picrender.fcgi?artid=2501333&blobtype=pdf</ref>.In 1953 he first formulated and demonstrated the effectiveness of ORS (Orally Rehydrated Saline) for diarrhea management. His paper regarding this finding was published in Lancet at November 1953<ref>http://db.jhuccp.org/ics-wpd/exec/icswppro.dll?BU=http://db.jhuccp.org/ics-wpd/exec/icswppro.dll&QF0=DocNo&QI0=530036&TN=Popline&AC=QBE_QUERY&MR=30%25DL=1&&RL=1&&RF=LongRecordDisplay&DF=LongRecordDisplay</ref>. In that paper he states that [[Avomin]] can stop vomiting during cholera and then oral rehydration is possible. The formulation of the fluid replacement solution was 4 gm of sodium chloride, 25 gm of glucose and 1000 ml of water<ref>[http://db.jhuccp.org/ics-wpd/exec/icswppro.dll?BU=http://db.jhuccp.org/ics-wpd/exec/icswppro.dll&QF0=DocNo&QI0=530036&TN=Popline&AC=QBE_QUERY&MR=30%25DL=1&&RL=1&&RF=LongRecordDisplay&DF=LongRecordDisplay Control of vomiting in cholera and oral replacement of fluid; Chatterjee HN; Lancet. 1953 Nov 2;2(6795):1063 ]</ref><ref>[http://www.pubmedcentral.nih.gov/picrender.fcgi?artid=1036912&blobtype=pdf MAGIC BULLET: THE HISTORY OF ORAL REHYDRATION THERAPY; JOSHUA NALIBOW RUXIN]</ref>. |
|||
In 1950s, by [[animal testing|experimenting]] on [[rats]] and [[guinea pigs]], [[physiologist]]s discovered that [[sodium]] and [[glucose]] were [[Symporter|transported together]] across the [[gastrointestinal]] [[epithelium]]. Using [[histology|histological]] analysis and [[isotope]] studies, it was shown that the intestinal mucosa was not disrupted in cholera, as previously thought. These findings were confirmed in [[human experiments]], where it was shown that glucose-containing ORT significantly decreased the necessity for IV fluids by 70-80%. These studies showed similar result as Chatterjee and provided a physiological basis for the use of ORT in [[clinical medicine]].<ref name=guerrant_ort_history />. |
|||
The [[Bangladesh Liberation War]] in 1971 provoked a public health emergency in the refugee camps set up to house those fleeing the violence. With cholera spreading rapidly and death rates rising, medical teams ran out of intravenous fluids. [[Dilip Mahalanabis|Dr. Mahalanabis]], the head of [[International Centre for Diarrhoeal Disease Research]] ([[Bangladesh]]), instructed his staff to distribute Oral Rehydration Salts (ORS) to the refugee camps. In the refugee camps where ORS was being used to treat over 3,000 patients, the [[mortality rate|death rate]] was only 3%, compared to 20–30% in those camps using only intravenous fluid therapy. Others replicated these findings and found ORT can be used in babies. |
|||
In 2002, Drs. Norbert Hirschhorn, Dilip Mahalanabis, David R. Nalin, and Nathaniel F. Pierce were awarded the first [[Pollin Prize for Pediatric Research]], in recognition of their work in developing ORT.<ref name=Pollin>[[World Health Organisation]], Child and Adolescent Health Development. [http://www.who.int/child-adolescent-health/NEWS/news_8.htm The first Pollin Prize for Paediatric Research awarded to Oral Rehydration Therapy]. Issued November 2002, accessed August 21, 2006</ref> In May 2001, the International Centre for Diarrhoeal Disease Research, Bangladesh received the first Gates Award for Global Health in recognition of its role in developing Oral Rehydration Solution. In 2007, three former ICDDR,B scientists, Dr. Richard Alan Cash, Dr. Dilip Mahalanabis and Dr. David R. Nalin, were also individually honoured for their efforts in testing and implementing ORS, sharing the 2006 Prince Mahidol Award for public health, which is presented annually for outstanding contributions in public health and medicine. In addition to the award for public health, a separate award for medicine was also presented to Professor Stanley George Schultz in recognition of his research on sodium absorption, which provided an important basis for the discovery of ORS. Unfortunately Chatterjee did not get due credit as inventor<ref>http://www.ncbi.nlm.nih.gov/pubmed/13110052?ordinalpos=5&itool=EntrezSystem2.PEntrez.Pubmed.Pubmed_ResultsPanel.Pubmed_DefaultReportPanel.Pubmed_RVDocSum</ref> of ORS. Medical history (Medical History, 1994, 38: 363-397) explained it as follows: <blockquote>It is generally agreed that racism or the lack of a “scientific” rationale prevented the widespread adoption of his (hemendra’s) work” </blockquote> |
|||
In 1978 the [[World Health Organization]] launched a worldwide campaign to reduce mortality related to diarrhea, with ORT as one of the principal elements of that program. |
|||
Between 1980 and 2000, ORT decreased the number of children under five dying of diarrhea from 4.6 million worldwide to 1.8 million — a 60% reduction. According to ''[[The Lancet]]'' (1978), ORT is "potentially the most important medical discovery of the 20th century". Despite the success and effectiveness of ORT, uptake of ORT has slowed, which may result in a decline in the progress on mortality rates from diarrheal disease unless swift action is taken to increase uptake of ORT.<ref>[http://www.who.int/bulletin/volumes/86/3/07-041384/en/index.html Ram P, Choi M, Blum L, et al. Declines in case management of diarrhoea among children less than five years old. ''Bulletin of the World Health Organization'' 2008;86(3):161-240.]</ref> |
|||
Today, the world production of ORS [[sachet]]s is around 500 million sachets per year. The [[children's rights]] agency [[UNICEF]] distributes them to families with children in around 60 [[developing country|developing countries]]. ORT represents a cheap and effective way of reducing the millions of deaths caused each year by diarrhea. ORT is part of "GOBI", a low cost program to increase child survival in developing countries, including '''G'''rowth monitoring, '''O'''RT, '''B'''reastfeeding, and '''I'''mmunization.<ref>{{cite web | url= http://www.unicef.org/publications/files/1946-2006_Sixty_Years_for_Children.pdf |
|||
| title= ''1946–2006 Sixty Years for Children'' |
|||
| year= 2006 | month= November | format= [[PDF]] | publisher= [[United Nations Children’s Fund]] |
|||
| accessdate= 2008-06-07 }}</ref> |
|||
== Physiology == |
|||
'''Oral rehydration therapy''' is widely considered to be the best method for combating the [[dehydration]] caused by [[diarrhea]] and/or [[vomit]]ing. |
|||
Various diseases cause damage to the [[intestine]], allowing water to flow from the blood into the intestine, depleting the body of both fluid and [[electrolyte]]s. This may be |
|||
* a direct destruction of the cells lining the intestine (the [[enterocyte]]s), |
|||
* a toxic effect causing them to lose their [[microvilli]] (the [[brush border]]), |
|||
* a toxic effect (by an [[enterotoxin]]) causing them to secrete water. |
|||
In the human body, water is absorbed and secreted passively; it follows the movement of salts, based on the principle of [[osmosis]]. So, in many cases, [[diarrhea]] is caused by intestine cells secreting [[salt]]s (primarily sodium) and water following passively along. |
|||
Simply drinking water is ineffective{{Fact|date=June 2008}} for 2 reasons: (1) the large intestine is usually secreting instead of absorbing water, and (2) [[electrolyte]] losses also need compensating. As such, the standard treatment is to restore fluids [[intravenous therapy|intravenously]] with water and salts. This requires trained personnel and materials which are not sufficiently available in the [[Third World]]. |
|||
However, it was discovered that the body can absorb a simple [[solution]] containing both sugar and salt. The dry ingredients can be mixed and packaged, and then the solution can be prepared and delivered by people with minimal training. One diarrhea mechanism (like in [[cholera]], which is a very dangerous form of profuse diarrhea), is an [[enterotoxin]] interfering with [[enterocyte]] [[cAMP]] and [[G-proteins]]. However, water can still be absorbed by cAMP-independent mechanisms, like the [[SGLT]]-transporter (sodium and glucose transporter, of which two types exist). This is achieved by combining [[salt]]s and [[glucose]]. |
|||
Oral rehydration can be accomplished by drinking frequent small amounts of an oral rehydration salt solution. |
|||
It is important to rehydrate with solutions that contain electrolytes, especially [[sodium]] and [[potassium]], so that [[electrolyte disturbance]]s may be avoided. Sugar is absolutely essential to improve adequate absorption of electrolytes and water, but the presence of sugar in ORS solutions does tend to cause [[diarrhea]] to worsen. Although oral rehydration with a sugar solution does not stop diarrhea, and the diarrhea contributes to further loss of fluids, oral rehydration helps replace these fluids. It thus keeps the body hydrated and gives the patient a greatly improved chance of surviving the diarrhea. If a broth can be prepared from simple carbohydrates and substituted for sugar in the solution, diarrhea can sometimes be reduced while oral rehydration remains effective. |
|||
Often [[sodium bicarbonate]] or [[sodium citrate]] is also added to formulas in an attempt to revert [[metabolic acidosis]]. |
|||
Recently, the ORS formulation was revised to reduce the sodium and glucose contents. This new, low-osmolarity ORS, improves the efficacy of ORS, reduces the need for unscheduled intravenous infusions, lowers stool volume, and causes less vomiting compared with standard ORS.<ref>[http://www.eddcontrol.org/files/Implementation_recommendations_WHO.pdf World Health Organization. Implementing the New Recommendations on the Clinical Management of Diarrhoea. 2006.]</ref> While the old formulation of ORS is still acceptable, the [[World Health Organization]] and [[UNICEF]] are now actively promoting this new formulation. |
|||
==UNICEF/WHO definition== |
|||
[[UNICEF]] and the [[WHO]] jointly maintain the official guidelines<ref name=who_ort_gen>{{cite web|title=WHO - The International Pharmacopoeia (Ph. Int.): Oral Rehydration|url=http://www.who.int/medicines/publications/pharmacopoeia/ors/en/|accessdate=2008-07-15}}</ref> for the contents of reduced [[osmolarity]] ORS packets. These guidelines are used by manufacturers of commercial ORT packets that are available for purchase and were last updated in 2006.<ref name=unicef_ort_update>{{cite web|title=UNICEF - Improved formula for oral rehydration salts to save children's lives|url=http://www.unicef.org/media/media_31825.html|accessdate=2008-07-15}}</ref> |
|||
A 1-liter preparation of ORT solution<ref name=ORT_solution>{{cite web|title=Sales perorales ad rehydratationem - Oral rehydration salts|url=http://www.who.int/medicines/publications/pharmacopoeia/Oralrehydrationsalts.pdf|accessdate=2008-07-15|format=pdf}}</ref> contains: |
|||
*[[sodium chloride]] (NaCl) - 2.6g |
|||
*[[trisodium citrate]] dehydrate - 2.9g |
|||
*[[potassium chloride]] (KCl) - 1.5g |
|||
*anhydrous [[glucose]] - 13.5g |
|||
There is an additional recommendation of [[zinc]] supplementation<ref name=who_ort_gen /> for the management of diarrheal disease in addition to ORT, particularly for pediatric patients. Preparations are available as a [[zinc sulfate]] solution for adults,<ref name=adult_zinc_sol>{{cite web|title=Zinc Sulfate|url=http://www.who.int/entity/medicines/publications/pharmacopoeia/QAS07_194rev1Zinc-sulf_FINAL.pdf|accessdate=2008-07-15|format=pdf}}</ref> a modified solution for children,<ref name=peds_zinc_sol>{{cite web|title=Paediatric Zinc Sulfate Oral Solution|url=http://www.who.int/entity/medicines/publications/pharmacopoeia/QAS07_195rev1Zinc-sulf-oral-solFINAL.pdf|accessdate=2008-07-15|format=pdf}}</ref> and also a tablet form for children.<ref name=peds_zinc_tablet>{{cite web|title=Paediatric Zinc Sulfate Tablets|url=http://www.who.int/entity/medicines/publications/pharmacopoeia/QAS07_193_rev1Zinc-sulf-tabFINAL.pdf|accessdate=2008-07-15|format=pdf}}</ref> |
|||
Although [[magnesium]] is a common ingredient in commercial electrolyte solutions, it is not part of the UNICEF/WHO guidelines for ORT. Severe diarrhea causes an isotonic loss of fluid from the body's [[extracellular compartment]]. Because very little magnesium is in this compartment, very little is lost in diarrhea and there is no need to replace it.{{Fact|date=July 2008}} |
|||
== Alternative Formulations == |
|||
There are several commercially available products<ref name= Kelly>{{cite journal | author = Kelly D, Nadeau J. | title = Oral Rehydration Solution: A “Low-Tech” Oft Neglected Therapy | journal = Nutrition Issues in Gastroenterology | volume = 21 | pages = 51–62 | year = 2004}}</ref><ref name= King >{{cite journal | author = King CK, Glass R, Bresee JS, Duggan C| title = Managing Acute Gastroenteritis Among Children: Oral Rehydration, Maintenance, and Nutritional Therapy | journal = Centers for Disease Control and Prevention. | volume = 52 | pages = 1–16| year = 2003}}</ref> but an inexpensive home-made solution consists of 8 level [[teaspoon]]s of [[sugar|table sugar]] (sucrose) and 1 level teaspoon of [[table salt]] mixed in 1 [[liter]] of boiled water ([http://www.rehydrate.org/solutions/homemade.htm#recipes Rehydration Project: Home made recipe]). Fructose (fruit sugar) or artificial sweeteners should not be substituted for the table sugar in this recipe. A half cup of [[orange juice]] or half of a mashed [[banana]] can be added to each liter both to add potassium and to improve taste.([http://www.who.int/topics/cholera/publications/en/first_steps.pdf]) This recipe is preferable to [[sports drink]]s which are formulated to rehydrate healthy individuals and so contain too much sugar and too little electrolytes for this purpose.<ref>[http://www.gatorade.com/formula_and_nutrition_info/ Nutrition Facts of Gatorade]</ref> |
|||
The online ''[[Merck Manual]]'' lists a recipe of "1 L of water to 3.5 g NaCl [salt], 2.9 g trisodium citrate (or 2.5 g NaHCO3 [Baking soda]), 1.5 g KCl [Salt substitute, Potassium chloride], and 20 g glucose"<ref>[http://www.merck.com/mmpe/sec19/ch276/ch276c.html Merck Manual: Oral Rehydration]</ref>. |
|||
==References== |
|||
{{reflist|2}} |
|||
== External links == |
|||
*[http://libdoc.who.int/hq/2006/WHO_FCH_CAH_06.1.pdf WHO Oral Rehydration Salts: Production of the new ORS] |
|||
*[http://rehydrate.org/ Rehydration Project] |
|||
*[http://www.who.int/docstore/bulletin/pdf/2000/issue10/bu0747.pdf "Reducing deaths from diarrhoea through oral rehydration therapy"], ''Bulletin of the World Health Organization'', 2000: '''78''' (10); 1246-1255. |
|||
*[http://www.supply.unicef.dk/catalogue/bulletin9.htm New formulation of Oral Rehydration Salts (ORS) with reduced osmolarity] - Technical Bulletin from UNICEF, describing the user of a weaker solution, with the aim of reducing stool output. |
|||
*[http://www.rainbowpediatrics.net/faq/12.3.html Rainbow Pediatrics Knowledgebase: The Oral Rehydration Therapy] |
|||
*[http://www.time.com/time/europe/magazine/article/0,13005,901061016-1543876,00.html A Simple Solution] - ''[[Time (magazine)|Time]]'', Sunday, [[October 8]], [[2006]]. |
|||
*[http://www.irc.nl/page/31514 Diarrhea: why is a simple and inexpensive treatment not more widely used?] IRC, Updated: Monday [[6 November]] [[2006]]. Accessed [[21 November]] [[2006]]. |
|||
{{cholera}} |
|||
[[Category:Development]] |
|||
[[Category:Medical treatments]] |
|||
[[Category:Cholera]] |
|||
[[de:WHO-Trinklösung]] |
|||
[[es:Sales de Rehidratación Oral]] |
|||
[[fa:او آر اس]] |
|||
[[nl:Oraal rehydratiemiddel]] |
|||
[[ja:経口補水塩]] |
|||
[[pt:Soro caseiro]] |
|||
[[fi:Oraalinen nestehoito]] |
|||
[[sv:Vätskeersättning]] |
|||
Revision as of 19:19, 15 February 2009
Oral rehydration therapy, (also ORT, oral rehydration salts or solutions (ORS), oral electrolyte), is a simple, cheap, and effective treatment for dehydration associated with diarrhea, particularly gastroenteritis, such as that caused by cholera or rotavirus. ORT consists of a solution of salts and sugars which is administered orally. It is used around the world, but is most important in the developing world, where it saves millions of children from death due to diarrhea—the second leading cause of death in children under five.[1]
History
Prescriptions from the ancient physician Sushruta date back over 2500 years with treatment of acute diarrhea with rice water, coconut juice, and carrot soup. However, this knowledge did not carry over to the Western world, as dehydration was found to be the major cause of death secondary to the 1829 cholera pandemic in Russia and Western Europe. In 1831, William O'Shaughnessy noted the loss of water and salt in the stool of cholera patients and prescribed intravenous fluid therapy to compensate. The results were remarkable, as patients who were on the brink of death from dehydration recovered. The mortality rate of cholera dropped from 70% to 40% with the use of hypertonic IV solutions.[2]
Robert Cade, Dana Shires, Harry James Free, and Alejandro de Quesada were the medical researchers at the University of Florida who created the original Gatorade thirst quencher in 1965.[3] The Gators football coach, Ray Graves, was frustrated with the performance of his players during the hot summer football practices, and asked the team doctor, one of Cade’s associates, for his insight. Cade and his research team came across the unique mix of water, sodium, sugar, potassium, phosphate, and lemon juice that is now known as Gatorade in honor of the football team, the Gators. The football team credited Gatorade with their first Orange Bowl win over the Georgia Tech Yellow Jackets in 1967, and the drink became an instant phenomenon. The Yellow Jackets coach Bud Carson, when asked why they lost, replied: "We didn’t have Gatorade. That made the difference."[4] Contrary to popular belief, the University of Florida did not come up with the sports drink that is now known as Gatorade. The team doctor for the FSU football team, Dr. R.A. Johnson, began producing a sports drink that he called "Seminole Firewater" as early as 1962. Dr. Johnson blended sugar and lime flavoring with electrolytes (salts) to help keep the players hydrated and to prevent cramping. In 1964 at an annual Seminar of Collegiate sports physicians and athletic trainers held in Tallahassee, Fl., a representative from the University of Florida found out about the discovery that sodium and potassium keeps athletes better hydrated because it gives back to the body what is lost through sweat. They returned to Gainesville and, after being tested on the UF football players, the name "Gatorade" was given. The University of Florida requested a certified patent in 1967 for the drink that Dr. Johnson had freely shared with the public.
Another pioneering researcher of Oral Rehydration Therapy was Hemendra Nath Chatterjee, a Bengali scientist from West Bengal, India. Chatterjee started research on blood of Cholera [5]patient in 1946. In 1951 he discovered that in Bengal villages small epidemic of cholera is is treated by raw leaf juice of a common plant of Bengal called pathorchur (Coleus aromaticus)[6].In 1953 he first formulated and demonstrated the effectiveness of ORS (Orally Rehydrated Saline) for diarrhea management. His paper regarding this finding was published in Lancet at November 1953[7]. In that paper he states that Avomin can stop vomiting during cholera and then oral rehydration is possible. The formulation of the fluid replacement solution was 4 gm of sodium chloride, 25 gm of glucose and 1000 ml of water[8][9].
In 1950s, by experimenting on rats and guinea pigs, physiologists discovered that sodium and glucose were transported together across the gastrointestinal epithelium. Using histological analysis and isotope studies, it was shown that the intestinal mucosa was not disrupted in cholera, as previously thought. These findings were confirmed in human experiments, where it was shown that glucose-containing ORT significantly decreased the necessity for IV fluids by 70-80%. These studies showed similar result as Chatterjee and provided a physiological basis for the use of ORT in clinical medicine.[2].
The Bangladesh Liberation War in 1971 provoked a public health emergency in the refugee camps set up to house those fleeing the violence. With cholera spreading rapidly and death rates rising, medical teams ran out of intravenous fluids. Dr. Mahalanabis, the head of International Centre for Diarrhoeal Disease Research (Bangladesh), instructed his staff to distribute Oral Rehydration Salts (ORS) to the refugee camps. In the refugee camps where ORS was being used to treat over 3,000 patients, the death rate was only 3%, compared to 20–30% in those camps using only intravenous fluid therapy. Others replicated these findings and found ORT can be used in babies.
In 2002, Drs. Norbert Hirschhorn, Dilip Mahalanabis, David R. Nalin, and Nathaniel F. Pierce were awarded the first Pollin Prize for Pediatric Research, in recognition of their work in developing ORT.[10] In May 2001, the International Centre for Diarrhoeal Disease Research, Bangladesh received the first Gates Award for Global Health in recognition of its role in developing Oral Rehydration Solution. In 2007, three former ICDDR,B scientists, Dr. Richard Alan Cash, Dr. Dilip Mahalanabis and Dr. David R. Nalin, were also individually honoured for their efforts in testing and implementing ORS, sharing the 2006 Prince Mahidol Award for public health, which is presented annually for outstanding contributions in public health and medicine. In addition to the award for public health, a separate award for medicine was also presented to Professor Stanley George Schultz in recognition of his research on sodium absorption, which provided an important basis for the discovery of ORS. Unfortunately Chatterjee did not get due credit as inventor[11] of ORS. Medical history (Medical History, 1994, 38: 363-397) explained it as follows:
It is generally agreed that racism or the lack of a “scientific” rationale prevented the widespread adoption of his (hemendra’s) work”
In 1978 the World Health Organization launched a worldwide campaign to reduce mortality related to diarrhea, with ORT as one of the principal elements of that program.
Between 1980 and 2000, ORT decreased the number of children under five dying of diarrhea from 4.6 million worldwide to 1.8 million — a 60% reduction. According to The Lancet (1978), ORT is "potentially the most important medical discovery of the 20th century". Despite the success and effectiveness of ORT, uptake of ORT has slowed, which may result in a decline in the progress on mortality rates from diarrheal disease unless swift action is taken to increase uptake of ORT.[12]
Today, the world production of ORS sachets is around 500 million sachets per year. The children's rights agency UNICEF distributes them to families with children in around 60 developing countries. ORT represents a cheap and effective way of reducing the millions of deaths caused each year by diarrhea. ORT is part of "GOBI", a low cost program to increase child survival in developing countries, including Growth monitoring, ORT, Breastfeeding, and Immunization.[13]
Physiology
Oral rehydration therapy is widely considered to be the best method for combating the dehydration caused by diarrhea and/or vomiting.
Various diseases cause damage to the intestine, allowing water to flow from the blood into the intestine, depleting the body of both fluid and electrolytes. This may be
- a direct destruction of the cells lining the intestine (the enterocytes),
- a toxic effect causing them to lose their microvilli (the brush border),
- a toxic effect (by an enterotoxin) causing them to secrete water.
In the human body, water is absorbed and secreted passively; it follows the movement of salts, based on the principle of osmosis. So, in many cases, diarrhea is caused by intestine cells secreting salts (primarily sodium) and water following passively along.
Simply drinking water is ineffective[citation needed] for 2 reasons: (1) the large intestine is usually secreting instead of absorbing water, and (2) electrolyte losses also need compensating. As such, the standard treatment is to restore fluids intravenously with water and salts. This requires trained personnel and materials which are not sufficiently available in the Third World.
However, it was discovered that the body can absorb a simple solution containing both sugar and salt. The dry ingredients can be mixed and packaged, and then the solution can be prepared and delivered by people with minimal training. One diarrhea mechanism (like in cholera, which is a very dangerous form of profuse diarrhea), is an enterotoxin interfering with enterocyte cAMP and G-proteins. However, water can still be absorbed by cAMP-independent mechanisms, like the SGLT-transporter (sodium and glucose transporter, of which two types exist). This is achieved by combining salts and glucose.
Oral rehydration can be accomplished by drinking frequent small amounts of an oral rehydration salt solution.
It is important to rehydrate with solutions that contain electrolytes, especially sodium and potassium, so that electrolyte disturbances may be avoided. Sugar is absolutely essential to improve adequate absorption of electrolytes and water, but the presence of sugar in ORS solutions does tend to cause diarrhea to worsen. Although oral rehydration with a sugar solution does not stop diarrhea, and the diarrhea contributes to further loss of fluids, oral rehydration helps replace these fluids. It thus keeps the body hydrated and gives the patient a greatly improved chance of surviving the diarrhea. If a broth can be prepared from simple carbohydrates and substituted for sugar in the solution, diarrhea can sometimes be reduced while oral rehydration remains effective.
Often sodium bicarbonate or sodium citrate is also added to formulas in an attempt to revert metabolic acidosis.
Recently, the ORS formulation was revised to reduce the sodium and glucose contents. This new, low-osmolarity ORS, improves the efficacy of ORS, reduces the need for unscheduled intravenous infusions, lowers stool volume, and causes less vomiting compared with standard ORS.[14] While the old formulation of ORS is still acceptable, the World Health Organization and UNICEF are now actively promoting this new formulation.
UNICEF/WHO definition
UNICEF and the WHO jointly maintain the official guidelines[15] for the contents of reduced osmolarity ORS packets. These guidelines are used by manufacturers of commercial ORT packets that are available for purchase and were last updated in 2006.[16]
A 1-liter preparation of ORT solution[17] contains:
- sodium chloride (NaCl) - 2.6g
- trisodium citrate dehydrate - 2.9g
- potassium chloride (KCl) - 1.5g
- anhydrous glucose - 13.5g
There is an additional recommendation of zinc supplementation[15] for the management of diarrheal disease in addition to ORT, particularly for pediatric patients. Preparations are available as a zinc sulfate solution for adults,[18] a modified solution for children,[19] and also a tablet form for children.[20]
Although magnesium is a common ingredient in commercial electrolyte solutions, it is not part of the UNICEF/WHO guidelines for ORT. Severe diarrhea causes an isotonic loss of fluid from the body's extracellular compartment. Because very little magnesium is in this compartment, very little is lost in diarrhea and there is no need to replace it.[citation needed]
Alternative Formulations
There are several commercially available products[21][22] but an inexpensive home-made solution consists of 8 level teaspoons of table sugar (sucrose) and 1 level teaspoon of table salt mixed in 1 liter of boiled water (Rehydration Project: Home made recipe). Fructose (fruit sugar) or artificial sweeteners should not be substituted for the table sugar in this recipe. A half cup of orange juice or half of a mashed banana can be added to each liter both to add potassium and to improve taste.([1]) This recipe is preferable to sports drinks which are formulated to rehydrate healthy individuals and so contain too much sugar and too little electrolytes for this purpose.[23]
The online Merck Manual lists a recipe of "1 L of water to 3.5 g NaCl [salt], 2.9 g trisodium citrate (or 2.5 g NaHCO3 [Baking soda]), 1.5 g KCl [Salt substitute, Potassium chloride], and 20 g glucose"[24].
References
- ^ UNICEF. State of the World's Children 2008.
- ^ a b Guerrant, Richard L. (2003). "Cholera, diarrhea, and oral rehydration therapy: triumph and indictment". Clinical infectious diseases. 37 (3): 398–405. PMID 12884154. Retrieved 2008-07-15.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ^ "Born in the Lab". Gatorade. Retrieved 2008-11-22.
- ^ "Football Inventions That Shaped the Modern Game". 2007-09-06. Retrieved 2007-09-06.
- ^ http://www.journals.elsevierhealth.com/periodicals/trstmh/article/PII0035920346900430/abstract?showOmimLinks=true
- ^ http://www.pubmedcentral.nih.gov/picrender.fcgi?artid=2501333&blobtype=pdf
- ^ http://db.jhuccp.org/ics-wpd/exec/icswppro.dll?BU=http://db.jhuccp.org/ics-wpd/exec/icswppro.dll&QF0=DocNo&QI0=530036&TN=Popline&AC=QBE_QUERY&MR=30%25DL=1&&RL=1&&RF=LongRecordDisplay&DF=LongRecordDisplay
- ^ Control of vomiting in cholera and oral replacement of fluid; Chatterjee HN; Lancet. 1953 Nov 2;2(6795):1063
- ^ MAGIC BULLET: THE HISTORY OF ORAL REHYDRATION THERAPY; JOSHUA NALIBOW RUXIN
- ^ World Health Organisation, Child and Adolescent Health Development. The first Pollin Prize for Paediatric Research awarded to Oral Rehydration Therapy. Issued November 2002, accessed August 21, 2006
- ^ http://www.ncbi.nlm.nih.gov/pubmed/13110052?ordinalpos=5&itool=EntrezSystem2.PEntrez.Pubmed.Pubmed_ResultsPanel.Pubmed_DefaultReportPanel.Pubmed_RVDocSum
- ^ Ram P, Choi M, Blum L, et al. Declines in case management of diarrhoea among children less than five years old. Bulletin of the World Health Organization 2008;86(3):161-240.
- ^ "1946–2006 Sixty Years for Children" (PDF). United Nations Children’s Fund. 2006. Retrieved 2008-06-07.
{{cite web}}: Unknown parameter|month=ignored (help) - ^ World Health Organization. Implementing the New Recommendations on the Clinical Management of Diarrhoea. 2006.
- ^ a b "WHO - The International Pharmacopoeia (Ph. Int.): Oral Rehydration". Retrieved 2008-07-15.
- ^ "UNICEF - Improved formula for oral rehydration salts to save children's lives". Retrieved 2008-07-15.
- ^ "Sales perorales ad rehydratationem - Oral rehydration salts" (pdf). Retrieved 2008-07-15.
- ^ "Zinc Sulfate" (pdf). Retrieved 2008-07-15.
- ^ "Paediatric Zinc Sulfate Oral Solution" (pdf). Retrieved 2008-07-15.
- ^ "Paediatric Zinc Sulfate Tablets" (pdf). Retrieved 2008-07-15.
- ^ Kelly D, Nadeau J. (2004). "Oral Rehydration Solution: A "Low-Tech" Oft Neglected Therapy". Nutrition Issues in Gastroenterology. 21: 51–62.
- ^ King CK, Glass R, Bresee JS, Duggan C (2003). "Managing Acute Gastroenteritis Among Children: Oral Rehydration, Maintenance, and Nutritional Therapy". Centers for Disease Control and Prevention. 52: 1–16.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Nutrition Facts of Gatorade
- ^ Merck Manual: Oral Rehydration
External links
- WHO Oral Rehydration Salts: Production of the new ORS
- Rehydration Project
- "Reducing deaths from diarrhoea through oral rehydration therapy", Bulletin of the World Health Organization, 2000: 78 (10); 1246-1255.
- New formulation of Oral Rehydration Salts (ORS) with reduced osmolarity - Technical Bulletin from UNICEF, describing the user of a weaker solution, with the aim of reducing stool output.
- Rainbow Pediatrics Knowledgebase: The Oral Rehydration Therapy
- A Simple Solution - Time, Sunday, October 8, 2006.
- Diarrhea: why is a simple and inexpensive treatment not more widely used? IRC, Updated: Monday 6 November 2006. Accessed 21 November 2006.
