Pancreatic islets

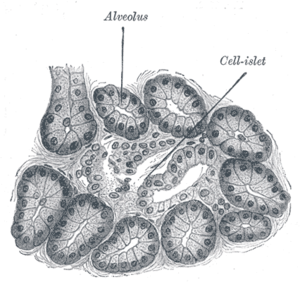
The endocrine (i.e., hormone-producing) cells of the pancreas are grouped in the islets of Langerhans. Discovered in 1869 by the famous German pathological anatomist Paul Langerhans, the islets of Langerhans constitute approximately 1 to 2% of the mass of the pancreas. There are about one million islets in a healthy adult human pancreas, which are distributed evenly throughout the organ, and their combined weight is 1 to 1.5 grams.
Cell types
Hormones produced in the Islets of Langerhans are secreted directly into the blood flow by (at least) four different types of cells:[1]
- Alpha cells releasing glucagon (15-20%)
- Beta cells producing insulin and amylin (65-80% of the islet cells)
- Delta cells producing somatostatin (3-10%)
- PP cells containing pancreatic polypeptide (3%-5%)
- Epsilon cells containing ghrelin
Islets can influence each other through paracrine and autocrine communication, and beta-cells are coupled electrically to beta cells (but not to other cell types).
Paracrine feedback
The paracrine feedback system of the islets of Langerhans has the following structure:
- Insulin: Activates beta cells and inhibits alpha cells.
- Glucagon: Activates alpha which activates beta cells and delta cells.
- Somatostatin: Inhibits alpha cells and beta cells
Electrical activity
Electrical activity of pancreatic islets has been studied using patch clamp techniques, and it has turned out that the behavior of cells in intact islets differs significantly from the behaviour of dispersed cells.
As a treatment for type I diabetes
Since the beta cells in islets of Langerhans are destroyed in type I diabetes, clinicians and researchers are actively pursuing islet transplantation technology as a means of curing this disease.
Islet transplantation which currently requires immunosuppression would be safer for type-1 diabetics if the need for lifelong immunosuppression were eliminated.
Transplantation
With the possibility of restoring beta cells, the Chicago Project headed at University of Illinois at Chicago Medical Center is probing for a way to regenerate beta cells in the islets and have them cultivate on their own within a human pancreas. With that being said, beta cells experience apoptosis early and thus become destroyed within a normal-functioning pancreas. The source of this seems to come from the transfer of Pander, a gene that enters in by attaching to RNA. This process of RNA transportation can be found in the glucose that bombards the beta cells. The genetic encoding found within Pander causes the beta cells to stop during the S phase of mitosis and head straight to apotasis. This ceases much of the reproduction of beta cells within the islets.
References in pop culture
- A Harlan Ellison short story titled "Adrift Just Off the Islets of Langerhans: Latitude 38° 54' N, Longitude 77° 00' 13" W" appears in his collection Deathbird Stories. (Those coordinates locate the intersection of H and 2nd N.E. in Washington, D.C., behind Union Station)
- American parodist "Weird Al" Yankovic released a song entitled Pancreas on his album Straight Outta Lynwood, which continually repeats the lyrics "Insulin, Glucagon, comin' from the Islets of Langerhans" during the final minute of the song.
- On their comedy album How Can You Be in Two Places at Once When You're Not Anywhere at All, The Firesign Theatre referred to immigrants who came "from little towns with strange names like Smegma, Spasmodic, Frog, and the far-flung Isles of Langerhans".
- In the Lord of the Rings parody book Bored of the Rings by the Harvard Lampoon, the map features two islands situated close to each other labled "The Isles of Langerhans".
External links
- MeSH A03.734.414
- Histology image: 80_14 at the University of Oklahoma Health Sciences Center - "Pancreas"
Gallery
Hormones/Islet Architecture
-
Mouse islet immunostained for pancreatic polypeptide.
-
Mouse islet immunostained for insulin.
-
Mouse islet immunostained for glucagon.



