Glucocorticoid


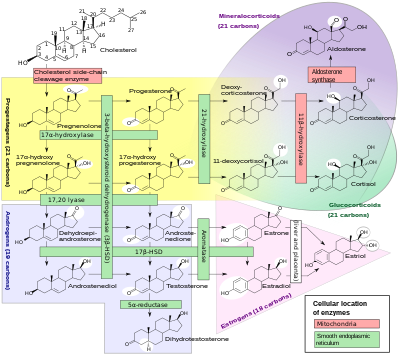
Glucocorticoids (GC) are a class of steroid hormones that bind to the glucocorticoid receptor (GR), which is present in almost every vertebrate animal cell. The name glucocorticoid (glucose + cortex + steroid) derives from their role in the regulation of the metabolism of glucose, their synthesis in the adrenal cortex, and their steroidal structure (see structure to the right).
GCs are part of the feedback mechanism in the immune system that turns immune activity (inflammation) down. They are therefore used in medicine to treat diseases that are caused by an overactive immune system, such as allergies, asthma, autoimmune diseases and sepsis. GCs have many diverse (pleiotropic) effects, including potentially harmful side effects.[1] They also interfere with some of the abnormal mechanisms in cancer cells, so they are used in high doses to treat cancer.
GCs cause their effects by binding to the glucocorticoid receptor (GR). The activated GR complex in turn up-regulates the expression of anti-inflammatory proteins in the nucleus (a process known as transactivation) and represses the expression of pro-inflammatory proteins in the cytosol by preventing the translocation of other transcription factors from the cytosol into the nucleus (transrepression).[1]
Glucocorticoids are distinguished from mineralocorticoids and sex steroids by their specific receptors, target cells, and effects. In technical terms, corticosteroid refers to both glucocorticoids and mineralocorticoids (as both are mimics of hormones produced by the adrenal cortex), but is often used as a synonym for glucocorticoid.
Cortisol (or hydrocortisone) is the most important human glucocorticoid. It is essential for life, and it regulates or supports a variety of important cardiovascular, metabolic, immunologic, and homeostatic functions. Glucocorticoid receptors are found in the cells of almost all vertebrate tissues. Various synthetic glucocorticoids are available; these are used either as replacement therapy in glucocorticoid deficiency or to suppress the immune system.
Effects
Glucocorticoid effects may be broadly classified into two major categories: immunological and metabolic. In addition, glucocorticoids play important roles in fetal development.
Immune
As discussed in more detail below, glucocorticoids through interaction with the glucocorticoid receptor:
- up-regulate the expression of anti-inflammatory proteins
- down-regulate the expression of pro-inflammatory proteins
Metabolic
The name "glucocorticoid" derives from early observations that these hormones were involved in glucose metabolism. In the fasted state, cortisol stimulates several processes that collectively serve to increase and maintain normal concentrations of glucose in blood.
Metabolic effects:
- Stimulation of gluconeogenesis, particularly in the liver: This pathway results in the synthesis of glucose from non-hexose substrates such as amino acids and glycerol from triglyceride breakdown, and is particularly important in carnivores and certain herbivores. Enhancing the expression of enzymes involved in gluconeogenesis is probably the best-known metabolic function of glucocorticoids.
- Mobilization of amino acids from extrahepatic tissues: These serve as substrates for gluconeogenesis.
- Inhibition of glucose uptake in muscle and adipose tissue: A mechanism to conserve glucose.
- Stimulation of fat breakdown in adipose tissue: The fatty acids released by lipolysis are used for production of energy in tissues like muscle, and the released glycerol provide another substrate for gluconeogenesis.
Excessive glucocorticoid levels resulting from administration as a drug or hyperadrenocorticism have effects on many systems. Some examples include inhibition of bone formation, suppression of calcium absorption (both of which can lead to osteoporosis), delayed wound healing, muscle weakness, and increased risk of infection. These observations suggest a multitude of less-dramatic physiologic roles for glucocorticoids.
Developmental
Glucocorticoids have multiple effects on fetal development. An important example is their role in promoting maturation of the lung and production of the surfactant necessary for extrauterine lung function. Mice with homozygous disruptions in the corticotropin-releasing hormone gene (see below) die at birth due to pulmonary immaturity. In addition, they are necessary for normal brain development, by initiating terminal maturation, remodelling axons and dendrites, and affecting cell survival.[2]
Mechanism of action
Transactivation
Glucocorticoids bind to the cytosolic glucocorticoid receptor (GR). This type of receptor is activated by ligand binding. After a hormone binds to the corresponding receptor, the newly-formed receptor-ligand complex translocates itself into the cell nucleus, where it binds to glucocorticoid response elements (GRE) in the promoter region of the target genes resulting in the regulation of gene expression. This process is commonly referred to as transactivation.[3]
The proteins encoded by these upregulated genes have a wide range of effects including for example:[3]
- anti-inflammatory – lipocortin I and p11/calpactin binding protein
- increased gluconeogenesis – glucose-6-phosphatase and tyrosine aminotransferase
Transrepression
The opposite mechanism is called transrepression. The activated hormone receptor interacts with specific transcription factors (such as AP-1 and NF-κB) and prevents the transcription of targeted genes. Glucocorticoids are able to prevent the transcription of pro-inflammatory genes, including interleukins IL-1B, IL-4, IL-5, and IL-8, chemokines, cytokines, GM-CSF, and TNFA genes.[3]
Dissociation
The ordinary glucocorticoids do not distinguish among transactivation and transrepression and influence both the "wanted" immune and "unwanted" genes regulating the metabolic and cardiovascular functions. Intensive research is aimed at discovering selectively acting glucocorticoids that will be able to repress only the immune system.[4][5]
Genetically modified mice which express a modified GR which is incapable of DNA binding are still responsive to the antiinflammatory effects of glucocorticoids while the stimulation of gluconeogenesis by glucocorticoids is blocked.[6] This result strongly suggests that most of the desirable antiinflammatory effects are due to transrepression while the undesirable metabolic effects arise from transactivation, a hypothesis also underlying the development of selective glucocorticoid receptor agonists.
Non-genomic
Glucocorticoids have been shown to exert a number of rapid actions that are independent of the regulations of gene transcription.
Binding of corticosteroids to the glucocorticoid receptor (GR) stimulates phosphatidylinositol 3-kinase and protein kinase AKT, leading to endothelial nitric oxide synthase (eNOS) activation and nitric oxide dependent vasorelaxation.[7] Membrane associated GR has been shown to mediate lymphocytolysis.[8][9][10] Finally some glucocorticoids have been shown to rapidly inhibit the release of the inflammatory prostaglandin PGE2 and this effect is blocked by the glucocorticoid receptor antagonist RU-486 and this effect is not affected by protein synthesis inhibitors. This data together suggests a non-genomic mechanism of action.[11]
Pharmacology
A variety of synthetic glucocorticoids, some far more potent than cortisol, have been created for therapeutic use. They differ in the pharmacokinetics (absorption factor, half-life, volume of distribution, clearance) and in pharmacodynamics (for example the capacity of mineralocorticoid activity: retention of sodium (Na+) and water; see also: renal physiology). Because they permeate the intestines easily, they are primarily administered per os (by mouth), but also by other methods, such as topically on skin. More than 90 percent of them bind different plasma proteins, however with a different binding specificity. Endogenous glucocorticoids and some synthetic corticoids have high affinity to the protein transcortin (also called CBG, corticosteroid-binding globulin), whereas all of them bind albumin. In the liver, they quickly metabolise by conjugation with a sulfate or glucuronic acid, and are secreted in the urine.
Glucocorticoid potency, duration of effect, and overlapping mineralocorticoid potency varies. Cortisol (hydrocortisone) is the standard of comparison for glucocorticoid potency. Hydrocortisone is the name used for pharmaceutical preparations of cortisol. Data refer to oral dosing, except when mentioned. Oral potency may be less than parenteral potency because significant amounts (up to 50% in some cases) may not be absorbed from the intestine. Fludrocortisone, DOCA, and aldosterone are, by definition, not considered glucocorticoids, although they may have minor glucocorticoid potency, and are included in this table to provide perspective on mineralocorticoid potency.
| Name | Glucocorticoid potency | Mineralocorticoid potency | Duration of action (t1/2 in hours) |
| Hydrocortisone (Cortisol) | 1 | 1 | 8 |
| Cortisone acetate | 0.8 | 0.8 | oral 8, intramuscular 18+ |
| Prednisone | 3.5-5 | 0.8 | 16-36 |
| Prednisolone | 4 | 0.8 | 16-36 |
| Methylprednisolone | 5-7.5 | 0.5 | 18-40 |
| Dexamethasone | 25-80 | 0 | 36-54 |
| Betamethasone | 25-30 | 0 | 36-54 |
| Triamcinolone | 5 | 0 | 12-36 |
| Beclometasone | 8 puffs 4 times a day equals 14 mg oral prednisone once a day |
- | - |
| Fludrocortisone acetate | 15 | 200 | 24 |
| Deoxycorticosterone acetate (DOCA) | 0 | 20 | - |
| Aldosterone | 0.3 | 200-1000 | - |
Therapeutic use
Glucocorticoids may be used in low doses in adrenal insufficiency. In much higher doses, oral or inhaled glucocorticoids are used to suppress various allergic, inflammatory, and autoimmune disorders. Inhaled glucocorticoids are the first-line treatment for Asthma. They are also administered as posttransplantory immunosuppressants to prevent the acute transplant rejection and the graft-versus-host disease. Nevertheless, they do not prevent an infection and also inhibit later reparative processes.
Physiological replacement
Any glucocorticoid can be given in a dose that provides approximately the same glucocorticoid effects as normal cortisol production; this is referred to as physiologic, replacement, or maintenance dosing. This is approximately 6-12 mg/m²/day (m² refers to body surface area (BSA), and is a measure of body size; an average man is 1.7 m²).
Immunosuppression
Glucocorticoids suppress the cell-mediated immunity. They act by inhibiting genes that code for the cytokines IL-1, IL-2, IL-3, IL-4, IL-5, IL-6, IL-8 and IFN-γ, the most important of which is IL-2. Smaller cytokine production reduces the T cell proliferation.[14]
Glucocorticoids do however not only reduce T cell proliferation, but also lead to another well known effect called glucocorticoid induced apoptosis. The effect is more prominent in immature T cells that still reside in the thymus, but also affect peripheral T cells. The exact mechanism underlying this glucocorticoid sensitivity still remains to be elucidated.[citation needed]
Glucocorticoids also suppress the humoral immunity, causing B cells to express smaller amounts of IL-2 and of IL-2 receptors. This diminishes both B cell clone expansion and antibody synthesis. The diminished amounts of IL-2 also causes fewer T lymphocyte cells to be activated.
Since glucocorticoid is a steroid, it regulates transcription factors; another factor it down-regulates is the expression of Fc receptors on macrophages, so there is a decreased phagocytosis of opsonised cells.[citation needed]
Anti-inflammatory
Glucocorticoids are potent anti-inflammatories, regardless of the inflammation's cause. Glucocorticoids' primary anti-inflammatory mechanism is lipocortin-1 (annexin-1) synthesis. Lipocortin-1 both suppresses phospholipase A2, thereby blocking eicosanoid production, and inhibits various leukocyte inflammatory events (epithelial adhesion, emigration, chemotaxis, phagocytosis, respiratory burst, etc...). In other words, Glucocorticoids not only suppress immune response, but also inhibit the two main products of inflammation, prostaglandins and leukotrienes. In addition, glucocorticoids also suppress cyclooxygenase (both COX-1 and COX-2) expression much like NSAIDs, potentiating the anti-inflammatory effect.
Glucocorticoids marketed as anti-inflammatories are often topical formulations, such as nasal sprays for rhinitis or inhalers for asthma. These preparations have the advantage of only affecting the targeted area, thereby reducing side effects or potential interactions.
Hyperaldosteronism
Glucocorticoids can be used in the management of familial hyperaldosteronism type 1. They are not effective however, for use in the type 2 condition.
Resistance
Resistance to the therapeutic uses of glucocorticoids can present difficulty; for instance, 25% of cases of severe asthma may be unresponsive to steroids. This may be the result of genetic predisposition, ongoing exposure to the cause of the inflammation (such as allergens), immunological phenomena that bypass glucocorticoids, and pharmacokinetic disturbances (incomplete absorption or accelerated excretion or metabolism).[14]
Side-effects
Glucocorticoid drugs currently being used act nonselectively, so in the long run they may impair many healthy anabolic processes. To prevent this, much research has been focused recently on the elaboration of selectively-acting glucocorticoid drugs. These are the side-effects that could be prevented:
- immunosuppression
- hyperglycemia due to increased gluconeogenesis, insulin resistance, and impaired glucose tolerance (Diabetes mellitus, also known as steroid diabetes)
- increased skin fragility, easy bruising
- negative calcium balance due to reduced intestinal calcium absorption[15]
- Steroid-induced osteoporosis: reduced bone density (osteoporosis, osteonecrosis, higher fracture risk, slower fracture repair)
- weight gain due to increased visceral and truncal fat deposition (central obesity) and appetite stimulation
- adrenal insufficiency (if used for long time and stopped suddenly without a taper)
- muscle breakdown (proteolysis), weakness; reduced muscle mass and repair
- expansion of malar fat pads and dilation of small blood vessels in skin
- anovulation, irregularity of menstrual periods
- growth failure, pubertal delay
- increased plasma amino acids, increased urea formation; negative nitrogen balance
- excitatory effect on central nervous system (euphoria, psychosis)
- glaucoma due to increased cranial pressure
- cataracts
In high doses, hydrocortisone (cortisol) and those glucocorticoids with appreciable mineralocorticoid potency can exert a mineralocorticoid effect as well, although in physiologic doses this is prevented by rapid degradation of cortisol by 11β-hydroxysteroid dehydrogenase isoenzyme 2 (11β-HSD2) in mineralocorticoid target tissues. Mineralocorticoid effects can include salt and water retention, extracellular fluid volume expansion, hypertension, potassium depletion, and metabolic alkalosis.
The combination of clinical problems produced by prolonged, excess glucocorticoids, whether synthetic or endogenous, is termed Cushing's syndrome.
Withdrawal
In addition to the effects listed above, use of high-dose steroids for more than a week begins to produce suppression of the patient's adrenal glands because the exogenous glucocorticoids suppress hypothalamic corticotropin-releasing hormone (CRH) and pituitary adrenocorticotropic hormone (ACTH). With prolonged suppression, the adrenal glands atrophy (physically shrink), and can take months to recover full function after discontinuation of the exogenous glucocorticoid.
During this recovery time, the patient is vulnerable to adrenal insufficiency during times of stress, such as illness. While there is wide individual variation in suppressive dose and time for adrenal recovery, clinical guidelines have been devised to estimate potential adrenal suppression and recovery, to reduce risk to the patient. The following is one example, but many variations exist or may be appropriate in individual circumstances.[citation needed]
- If a patient has been receiving daily high doses for 5 days or less, they can be abruptly stopped (or reduced to physiologic replacement if patient is adrenal-deficient). Full adrenal recovery can be assumed to occur by a week afterward.
- If high doses were used for 6-10 days, reduce to replacement dose immediately and taper over 4 more days. Adrenal recovery can be assumed to occur within 2-4 weeks of completion of steroids.
- If high doses were used for 11-30 days, cut immediately to twice replacement, and then by 25% every 4 days. Stop entirely when dose is less than half of replacement. Full adrenal recovery should occur within 1-3 months of completion of withdrawal.
- If high doses were used more than 30 days, cut dose immediately to twice replacement, and reduce by 25% each week until replacement is reached.
- Then change to oral hydrocortisone or cortisone as a single morning dose, and gradually decrease by 2.5 mg each week. When a.m. dose is less than replacement, the return of normal basal adrenal function may be documented by checking 0800 cortisol levels prior to the morning dose; stop drugs when 0800 cortisol is 10 μg/dl. It is difficult to predict the time to full adrenal recovery after prolonged suppressive exogenous steroids; some people may take nearly a year.
- Flare-up of the underlying condition for which steroids are given may require a more gradual taper than outlined above.
See also
- GITR (glucocorticoid-induced TNF receptor)
- Glucocorticoid receptor
- Immunosuppressive drug
- Selective glucocorticoid receptor agonist (SEGRA)
- Topical steroid
References
- ^ a b Rhen T, Cidlowski JA (2005). "Antiinflammatory action of glucocorticoids--new mechanisms for old drugs". N. Engl. J. Med. 353 (16): 1711–23. doi:10.1056/NEJMra050541. PMID 16236742.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Lupien JS; et al. (2009). "Effects of stress throughout the lifespan on the brain, behaviour and cognition". Nature Reviews Neuroscience. 10: 434–445. doi:10.1038/nrn2639.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help) - ^ a b c Newton R (2000). "Molecular mechanisms of glucocorticoid action: what is important?". Thorax. 55 (7): 603–13. doi:10.1136/thorax.55.7.603. PMC 1745805. PMID 10856322.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Schäcke H, Rehwinkel H, Asadullah K (2005). "Dissociated glucocorticoid receptor ligands: compounds with an improved therapeutic index". Curr Opin Investig Drugs. 6 (5): 503–7. PMID 15912964.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Newton R, Holden NS (2007). "Separating transrepression and transactivation: a distressing divorce for the glucocorticoid receptor?". Mol. Pharmacol. 72 (4): 799–809. doi:10.1124/mol.107.038794. PMID 17622575.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Reichardt HM, Tronche F, Bauer A, Schütz G (2000). "Molecular genetic analysis of glucocorticoid signaling using the Cre/loxP system". Biol. Chem. 381 (9–10): 961–4. doi:10.1515/BC.2000.118. PMID 11076028.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Hafezi-Moghadam A, Simoncini T, Yang Z, Limbourg FP, Plumier JC, Rebsamen MC, Hsieh CM, Chui DS, Thomas KL, Prorock AJ, Laubach VE, Moskowitz MA, French BA, Ley K, Liao JK (2002). "Acute cardiovascular protective effects of corticosteroids are mediated by non-transcriptional activation of endothelial nitric oxide synthase". Nat. Med. 8 (5): 473–9. doi:10.1038/nm0502-473. PMID 11984591.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Cato AC, Nestl A, Mink S (2002). "Rapid actions of steroid receptors in cellular signaling pathways". Sci. STKE. 2002 (138): RE9. doi:10.1126/stke.2002.138.re9. PMID 12084906.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Gametchu B, Watson CS, Pasko D (1991). "Size and steroid-binding characterization of membrane-associated glucocorticoid receptor in S-49 lymphoma cells". Steroids. 56 (8): 402–10. doi:10.1016/0039-128X(91)90028-T. PMID 1788858.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Gametchu B, Watson CS, Shih CC, Dashew B (1991). "Studies on the arrangement of glucocorticoid receptors in the plasma membrane of S-49 lymphoma cells". Steroids. 56 (8): 411–9. doi:10.1016/0039-128X(91)90029-U. PMID 1788859.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Croxtall JD, van Hal PT, Choudhury Q, Gilroy DW, Flower RJ (2002). "Different glucocorticoids vary in their genomic and non-genomic mechanism of action in A549 cells". Br. J. Pharmacol. 135 (2): 511–9. doi:10.1038/sj.bjp.0704474. PMC 1573139. PMID 11815387.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ From Liapi and Chrousos (ref. 2); Chapter 14. Glucocorticoid Therapy and Adrenal Suppression; http://www.endotext.org/adrenal/adrenal14/ch01s02.html
- ^ Leung DY, Hanifin JM, Charlesworth EN; et al. (1997). "Disease management of atopic dermatitis: a practice parameter" (PDF). Ann. Allergy Asthma Immunol. 79 (3): 197–211. PMID 9305225. Retrieved 2009-07-09.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ a b Leung DY, Bloom JW (2003). "Update on glucocorticoid action and resistance". J. Allergy Clin. Immunol. 111 (1): 3–22, quiz 23. doi:10.1067/mai.2003.97. PMID 12532089.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Gennari C (1993). "Differential effect of glucocorticoids on calcium absorption and bone mass". Br. J. Rheumatol. 32 Suppl 2: 11–4. ISSN 1462-0332. PMID 8495275.
{{cite journal}}:|access-date=requires|url=(help); Unknown parameter|month=ignored (help)
External links
- Glucocorticoids at the U.S. National Library of Medicine Medical Subject Headings (MeSH)
- R. Bowen (2006-05-26). "Glucocorticoids". Colorado State University. Retrieved 2008-05-11.
{{cite web}}: Cite has empty unknown parameter:|coauthors=(help)
