Penicillin

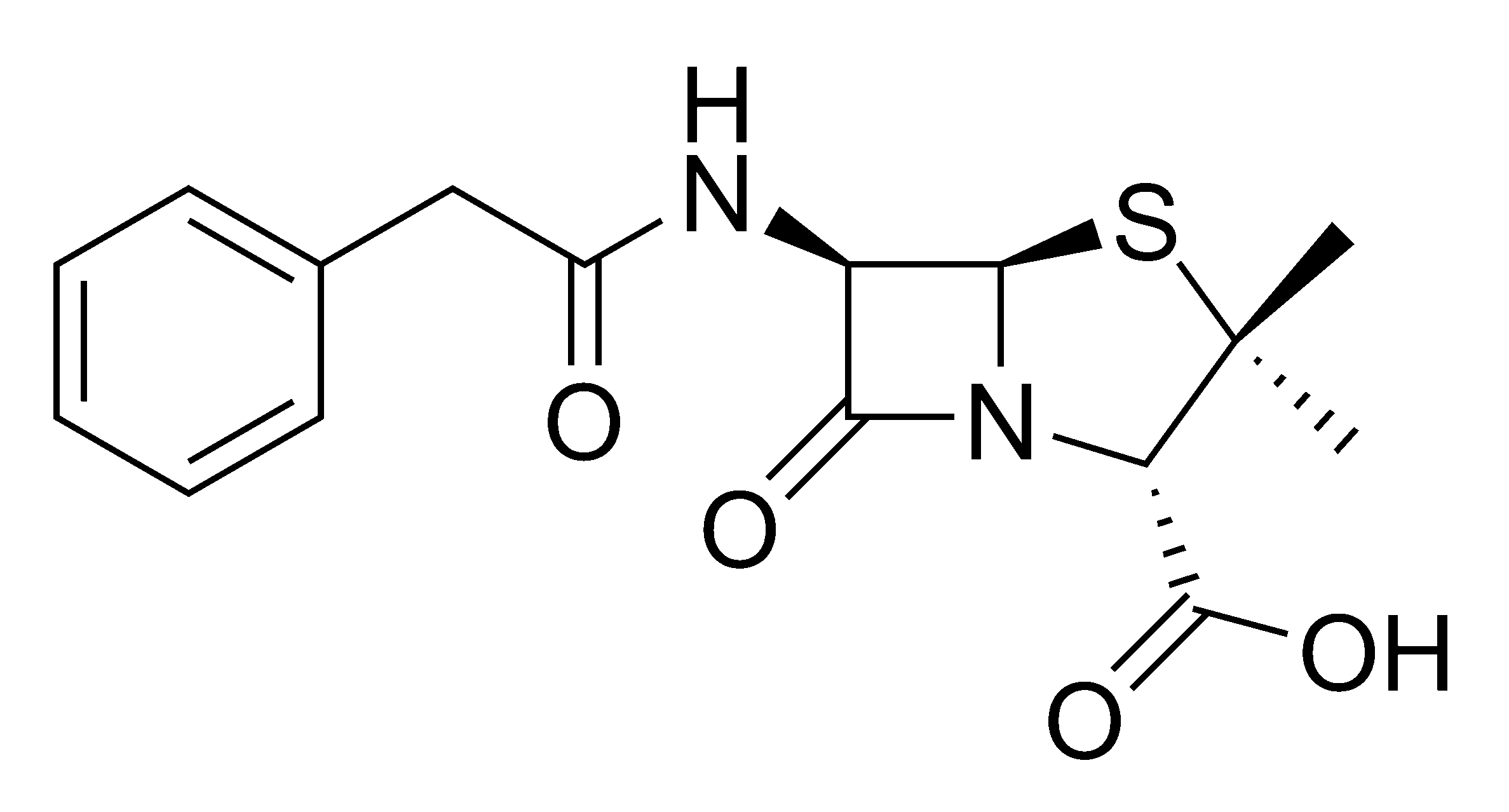
Penicillin refers to a group of β-lactam antibiotics used in the treatment of bacterial infections caused by susceptible, usually Gram-positive, organisms. The name "penicillin" can also be used in reference to a specific member of the penicillin group. Penicillins have the molecular formula R-C9H11N2O4S, where R is a variable side chain.
History
Penicillin was originally isolated from the Penicillium chrysogenum (formerly Penicillium notatum) mold. The antibiotic effect was originally discovered by French medical student Ernest Duchesne studying Penicillium glaucum in 1896, but his discovery was ignored by the Institut Pasteur. Another Institut Pasteur scientist, Costa Rican Clodomiro Picado Twight was the first to record the antibiotic effect of Penicillium in 1923.
The serendipitous discovery was finally attributed to Scottish scientist Alexander Fleming in 1928, who noticed a halo of inhibition of bacterial growth around a contaminant blue-green mold on a Staphylococcus plate culture. Fleming concluded that the mould was releasing a substance that was inhibiting bacterial growth. He grew a pure culture of the mould and discovered that it was Penicillium notatum – he later named the bacterial inhibiting substance "penicillin" after the Penicillium notatum that released it. Fleming was convinced after conducting some more experiments that penicillin could not last long enough in the human body to kill pathogenic bacteria and stopped studying penicillin after 1931. It would prove to be one of the discoveries that changed modern medicine. In 1939, Australian scientist Howard Walter Florey and a team of researchers (Ernst Boris Chain, A. D. Gardner, Norman Heatley, M. Jennings, J.Orr-Ewing and G.Sanders) at the Sir William Dunn School of Pathology, University of Oxford made significant progress in showing the in vivo bacteriacidal action of penicillin. Their attempts to treat humans failed due to insufficient volumes of penicillin, but they proved its harmlessness and effect in mice. Penicillin's first real success was on Hardy Lamber. He was treated by Fleming himself in 1930. [1]
During World War II, penicillin made a major difference in the number of deaths and amputations caused by infected wounds amongst Allied forces. Availability was severely limited, however, by the difficulty of manufacturing large quantities of penicillin and by the rapid renal clearance of the drug necessitating frequent dosing. Penicillins are actively secreted and about 80% of a penicillin dose is cleared within three to four hours of administration. During those times it became common procedure to collect the urine from patients being treated so that the penicillin could be isolated and reused. (Silverthorn, 2004)
This was not a satisfactory solution, however, so researchers looked for a way to slow penicillin secretion. They hoped to find a molecule that could compete with penicillin for the organic acid transporter responsible for secretion such that the transporter would preferentially secrete the competitive inhibitor. The uricosuric agent probenecid proved to be suitable. When probenecid and penicillin are concomitantly administered, probenecid competitively inhibits the secretion of penicillin, increasing its concentration and prolonging its activity. The advent of mass-production techniques and semi-synthetic penicillins solved supply issues, and this use of probenecid declined. (Silverthorn, 2004) Probenecid is still clinically useful, however, for certain infections requiring particularly high concentrations of penicillins. (Rossi, 2004)
The chemical structure of penicillin was determined by Dorothy Crowfoot Hodgkin in the early 1940s, enabling synthetic production. A team of Oxford research scientists led by Australian Howard Walter Florey and including Ernst Boris Chain and Norman Heatley discovered a method of mass producing the drug. Florey and Chain shared the 1945 Nobel prize in medicine with Fleming for this work. Penicillin has since become the most widely used antibiotic to date and is still used for many Gram-positive bacterial infections.
Resistance
Antibiotic resistance to penicillin was first observed in 1947, shortly after its introduction. Resistance to penicillin is now common amongst many hospital acquired bacteria. One mechanism of resistance to penicillin is through the production of the β-lactamase enzyme by some bacterial strains, which breaks down the β-lactam ring of penicillin rendering it harmless. Resistance also arises through modifications to the penicillin-binding proteins (PBPs) in the bacterial cell wall. Bacteria resistant to a particular β-lactam antibiotic may sometimes remain sensitive to certain other β-lactam antibiotics.
Developments from penicillin
The narrow spectrum of activity of the penicillins, along with the poor activity of the orally-active phenoxymethylpenicillin, led to the search for derivatives of penicillin which could treat a wider range of infections.
The first major development was ampicillin, which offered a broader spectrum of activity than either of the original penicillins and allowed doctors to treat a broader range of both Gram-positive and Gram-negative infections. Further developments led to amoxicillin, with improved duration-of-action.
Further development yielded beta-lactamase-resistant penicillins including flucloxacillin, dicloxacillin and methicillin. These were important for their activity against beta-lactamase-producing bacteria such as Staphylococcus species. It is still no match for MRSA (Methicillin Resistant Staphylococcus aureus).
The last in the line of true penicillins were the antipseudomonal penicillins, such as ticarcillin and piperacillin, useful for their activity against Gram-negative bacteria. However, the usefulness of the beta-lactam ring was such that related antibiotics, including the mecillinams, the carbapenems and, most importantly, the cephalosporins, have it at the centre of their structures.
Mode of action
Main article: beta-lactam antibiotic
β-lactam antibiotics work by inhibiting the formation of peptidoglycan cross links in the bacterial cell wall. The beta-lactam moiety of penicillin binds to the enzyme (transpeptidase) that links the peptidoglycan molecules in bacteria, and this weakens the cell wall of the bacterium when it multiplies (in other words, the antibiotic causes cell cytolysis or death when the bacterium tries to divide). Scott Williams is generally credited with having postulated this hypothesis.
Variants in clinical use
The term "penicillin" is often used generically to refer to one of the narrow-spectrum penicillins, particularly benzylpenicillin.
Benzathine penicillin
Benzathine penicillin is slowly absorbed into the circulation, after intramuscular injection, and hydrolysed to benzylpenicillin in vivo. It is the drug-of-choice when prolonged low concentrations of benzylpenicillin are required and appropriate, allowing prolonged antibiotic action over 2–4 weeks after a single IM dose. It is marketed by Wyeth under the trade name Bicillin®.
Specific indications for benzathine pencillin include: (Rossi, 2004)
- prophylaxis of rheumatic fever
- early or latent syphilis
Benzylpenicillin (penicillin G)

Benzylpenicillin, commonly known as penicillin G, is the gold standard penicillin. Penicillin G is typically given by a parenteral route of administration because it is unstable to the hydrochloric acid of the stomach. Because the drug is given parenterally, higher tissue concentrations of penicillin G can be achieved than is possible with phenoxymethylpenicillin. These higher concentrations translate to increased antibacterial activity.
Specific indications for benzylpenicillin include: (Rossi, 2004)
- bacterial endocarditis
- meningitis
- aspiration pneumonia, lung abscess
- community-acquired pneumonia
- syphilis
- septicaemia in children
Phenoxymethylpenicillin (penicillin V)
Phenoxymethylpenicillin, commonly known as penicillin V, is the orally-active form of penicillin. It is less active than benzylpenicillin, however, and is only appropriate in conditions where high tissue concentrations are not required.
Specific indications for phenoxymethylpenicillin include: (Rossi, 2004)
- infections caused by Streptococcus pyogenes
- tonsilitis
- pharyngitis
- skin infections
- prophylaxis of rheumatic fever
- moderate-to-severe gingivitis (with metronidazole)
Procaine penicillin
Procaine penicillin (Bicillin®) is a combination of benzylpenicillin with the local anaesthetic agent procaine. This combination is aimed at reducing the pain and discomfort associated with a large intramuscular injection of penicillin.
Specific indications for procaine penicillin include: (Rossi, 2004)
- respiratory tract infections where compliance with oral treatment is unlikely
- syphilis
- cellulitis
Semi-synthetic penicillins
Structural modifications were made to the side chain of the penicillin nucleus in an effort to improve oral bioavailability, overcome penicillin-resistance, and increase the spectrum of action.
Narrow spectrum penicillinase-resistant penicillins
This group was developed to be effective against penicillin-resistant Gram-positive organisms, sometime called anti-staph penicillin.
Moderate spectrum penicillins
This group was developed to increase the spectrum of action and, in the case of amoxicillin, improve oral bioavailability.
Broad spectrum penicillins
Clavulanic acid was added to amoxicillin to increase efficacy against β-lactamase-producing organisms.
Extended Spectrum Penicillins
This group was developed to increase efficacy against Gram-negative organisms.
Adverse effects
Adverse drug reactions
Common adverse drug reactions (ADRs) for the penicillins include: diarrhea, nausea, rash, urticaria, superinfection (including candidiasis). (Rossi, 2004)
Infrequent ADRs include: fever, vomiting, erythema, dermatitis, angioedema, pseudomembranous colitis. (Rossi, 2004)
Pain and inflammation at the injection site is also common for parenterally-administered benzathine penicillin, benzylpenicillin, and to a lesser extent procaine penicillin.
Allergy/hypersensitivity
Allergic reactions to any β-lactam antibiotic may occur in up to 10% of patients receiving that agent. Anaphylaxis will occur in approximately 0.01% of patients. (Rossi, 2004) There is perhaps a 5-10% cross-sensitivity between penicillin-derivatives, cephalosporins and carbapenems; but this figure has been challenged by various investigators.
Nevertheless, the risk of cross-reactivity is sufficient to warrant the contraindication of all β-lactam antibiotics in patients with a history of severe allergic reactions (urticaria, anaphylaxis, interstitial nephritis) to any β-lactam antibiotic.
Biosynthesis

The precursor compound ACV-tripeptide (δ-(L-α-amino-adipate)-L-cysteine-D-valine) is biosynthesised in bacteria and fungi from the monomeric L-amino acids by the enzyme ACV-synthetase (EC 6.3.2.26), a nonribosomal peptide synthetase. The ACV-tripeptide is cyclised by isopenicillin-N-synthetase (EC 1.21.3.1) to isopenicillin N, thereby forming the beta-lactam nucleus. The isopenicillin N N-acyltransferase (EC 2.3.1.164) enzyme exchanges the side-chain, yielding a broad range of different penicillins depending on the CoA-bound carboxylic acids utilised. The synthesis of cephalosporin antibiotics also starts with isopenicillin N. (Moss, 2002)
See also
References
- Moss GP (2002). Penicillin biosynthesis. Retrieved 6 December 2004.
- Rossi S (Ed.) (2004). Australian Medicines Handbook 2004. Adelaide: Australian Medicines Handbook. ISBN 0-9578521-4-2.
- Silverthorn DU (2004). Human Physiology: An Integrated Approach (3 ed.). Pearson Education. ISBN 0-8053-5957-5
- http://www.wellesley.edu/Chemistry/Chem101/antibiotics/obit-a-miller.html First patient saved]
