Brachial plexus
| Brachial plexus | |
|---|---|
 The right brachial plexus with its short branches, viewed from in front. | |
| Details | |
| From | C5, C6, C7, C8, T1 |
| Innervates | Sensory and motor innervation to the upper limb |
| Identifiers | |
| Latin | plexus brachialis |
| MeSH | D001917 |
| TA98 | A14.2.03.001 |
| TA2 | 6395 |
| FMA | 5906 |
| Anatomical terms of neuroanatomy | |
The brachial plexus is a network of nerve fibers, running from the spine, formed by the ventral rami of the lower four cervical and first thoracic nerve roots (C5-C8, T1). It proceeds through the neck, the axilla (armpit region), and into the arm. It is a network of nerves passing through the cervico-axillary canal to reach axilla and supplies brachium (upper arm), antebrachium (forearm) and hand.
Function
The brachial plexus is responsible for cutaneous and muscular innervation of the entire upper limb, with two exceptions: the trapezius muscle innervated by the spinal accessory nerve (CN XI) and an area of skin near the axilla innervated by the intercostobrachial nerve.
Lesions can lead to severe functional impairment.[1]
Anatomy
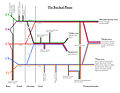
The brachial plexus is divided into Roots, Trunks, Divisions, Cords, and Branches. There are five "terminal" branches and numerous other "pre-terminal" or "collateral" branches that leave the plexus at various points along its length.
Root
The five roots are the five anterior rami of the spinal nerves, after they have given off their segmental supply to the muscles of the neck. The brachial plexus emerges at five different levels; C5, C6, C7, C8, and T1.
Trunk
These roots merge to form three trunks:
Division
Each trunk then splits in two, to form six divisions:
- anterior divisions of the upper, middle, and lower trunks
- posterior divisions of the upper, middle, and lower trunks
Cord
These six divisions will regroup to become the three cords. The cords are named by their position with respect to the axillary artery.
- The posterior cord is formed from the three posterior divisions of the trunks (C5-C8,T1)
- The lateral cord is the anterior divisions from the upper and middle trunks (C5-C7)
- The medial cord is simply a continuation of the anterior division of the lower trunk (C8,T1)
Branches
The branches are listed below. Most branch from the cords, but a few branch (indicated in italics) directly from earlier structures. The five on the left are considered "terminal branches".
Diagram
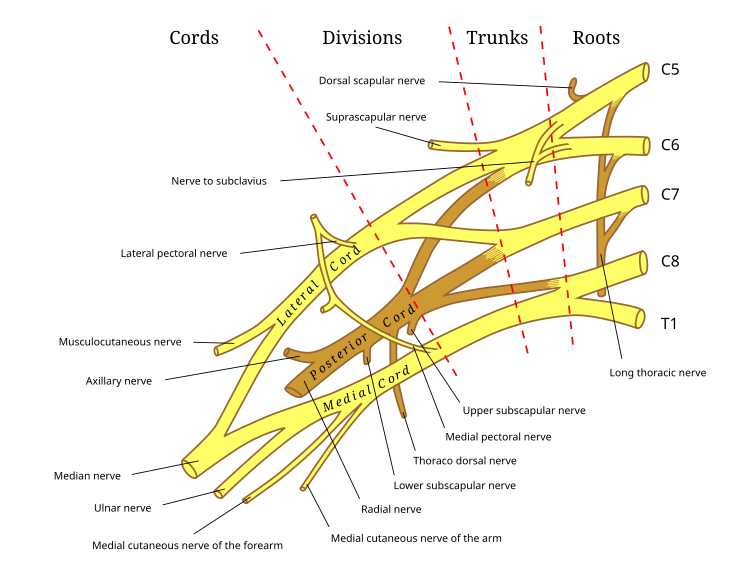


Specific branches
Bold indicates primary spinal root component of nerve. Italics indicate spinal roots that frequently, but not always, contribute to the nerve.
| From | Nerve | Roots[2] | Muscles | Cutaneous |
| roots | dorsal scapular nerve | C4, C5 | rhomboid muscles and levator scapulae | - |
| roots | long thoracic nerve | C5, C6, C7 | serratus anterior | - |
| roots | branch to phrenic nerve | C5 | - | - |
| upper trunk | nerve to the subclavius | C5, C6 | subclavius muscle | - |
| upper trunk | suprascapular nerve | C5, C6 | supraspinatus and infraspinatus | - |
| lateral cord | lateral pectoral nerve | C5, C6, C7 | pectoralis major and pectoralis minor (by communicating with the medial pectoral nerve) | - |
| lateral cord | musculocutaneous nerve | C5, C6, C7 | coracobrachialis, brachialis and biceps brachii | becomes the lateral cutaneous nerve of the forearm |
| lateral cord | lateral root of the median nerve | C5, C6, C7 | fibres to the median nerve | - |
| posterior cord | upper subscapular nerve | C5, C6 | subscapularis (upper part) | - |
| posterior cord | thoracodorsal nerve (middle subscapular nerve) | C6, C7, C8 | latissimus dorsi | - |
| posterior cord | lower subscapular nerve | C5, C6 | subscapularis (lower part ) and teres major | - |
| posterior cord | axillary nerve | C5, C6 | anterior branch: deltoid and a small area of overlying skin posterior branch: teres minor and deltoid muscles |
posterior branch becomes upper lateral cutaneous nerve of the arm |
| posterior cord | radial nerve | C5, C6, C7, C8, T1 | triceps brachii, supinator, anconeus, the extensor muscles of the forearm, and brachioradialis | skin of the posterior arm as the posterior cutaneous nerve of the arm |
| medial cord | medial pectoral nerve | C8, T1 | pectoralis major and pectoralis minor | - |
| medial cord | medial root of the median nerve | C6-T1 | fibres to the median nerve | portions of hand not served by ulnar or radial |
| medial cord | medial cutaneous nerve of the arm | C8, T1 | - | front and medial skin of the arm |
| medial cord | medial cutaneous nerve of the forearm | C8, T1 | - | medial skin of the forearm |
| medial cord | ulnar nerve | C8, T1 | flexor carpi ulnaris, the medial two bellies of flexor digitorum profundus, the intrinsic hand muscles except the thenar muscles and the two most lateral lumbricals | the skin of the medial side of the hand and medial one and a half fingers on the palmar side and medial two and a half fingers on the dorsal side |
Some mnemonics for remembering the branches:
- Posterior cord branches
- STAR - subscapular (upper and lower), thoracodorsal, axillary, radial
- RATS- Radial nerve, Axillary nerve, Thoracodorsal nerve, Subscapular (Upper & Lower)nerve.
- ULTRA - upper subscapular, lower subscapular, thoracodorsal, radial, axillary
- ULNAR- Upper subscapular nerve, Lower subscapular nerve,Nerve to lattissimus dorsi, Axillary nerve, Radial nerve.
- Lateral Cord Branches
- LLM "Lucy Loves Me" - lateral pectoral, lateral root of the median nerve, musculocutaneous
- Love Me Latha (LML) - Lateral pectoral nerve, Musculocutaneous nerve, Lateral root of Median Nerve.
- Look My Lancer-Lateral pectoral nerve, Musclocutaneous nerve,Lateral root of Median nerve.
- Medial Cord Branches
- MMMUM "Most Medical Men Use Morphine" - medial pectoral, medial cutaneous nerve of arm, medial cutaneous nerve of forearm, ulnar, medial root of the median nerve
- Union of 4 Medials - Ulnar nerve, Medial cutaneous nerve of arm, Medial cutaneous nerve of forearm, Medial pectoral nerve, Medial root of Median Nerve.
- 5 main nerves of brachial plexus, in order laterally to medially
- "My Aunty Recognized My Uncle" - Musculocutaneous, axillary, radial, median, ulnar
Injuries
Injuries to the brachial plexus affect cutaneous sensations and movements in the upper limb. They can be caused by stretching, diseases, and wounds to the lateral cervical region (posterior triangle) of the neck or the axilla. Depending on the location of the injury, the signs and symptoms can range from complete paralysis to anesthesia. Testing the patient's ability to perform movements and comparing it to their normal side is a method to assess the degree of paralysis. A common brachial plexus injury is from a hard landing where the shoulder widely separates from the neck (such as in the case of motorcycle accidents or falling from a tree). These stretches can cause ruptures to the superior portions of the brachial plexus or avulse the roots from the spinal cord. Upper brachial plexus injuries are frequent in newborns when excessive stretching of the neck occurs during delivery. Studies have shown a relationship between birth weight and brachial plexus injuries; however, the number of cesarean deliveries necessary to prevent a single injury is high at most birth weights.[3] For the upper brachial plexus injuries, paralysis occurs in those muscles supplied by C5 and C6 like the deltoid, biceps, brachialis, and brachioradialis. A loss of sensation in the lateral aspect of the upper limb is also common with such injuries. An inferior brachial plexus injury is far less common, but can occur when a person grasps something to break a fall or a baby's upper limb is pulled excessively during delivery. In this case, the short muscles of the hand would be affected and cause the inability to form a full fist position.[4] In order to differentiate between a pre ganglionic and a post ganglionic type of injury on clinical examination one has to keep the following points in mind. In pre ganglionic injuries there will be loss of sensation above the level of clavicle, presence of pain in an otherwise insensate hand, presence of ipsilateral Horner's syndrome and loss of function of muscles supplied by branches arising directly from roots i.e. long thoracic nerve palsy leading to winging of scapula and elevation of ipsilateral diaphragm due to phrenic nerve palsy.
Acute brachial plexus neuritis is a neurological disorder that is characterized by the onset of severe pain in the shoulder region. Additionally, the compression of cords can cause pain radiating down the arm, numbness, paresthesia, erythema, and weakness of the hands. This kind of injury is common for people who have prolonged hyperabduction of the arm when they are performing tasks above their head.
Prevention
Definition
Brachial plexus injuries can be defined as an injury which affects the nerves which send signals from the spine to your shoulder.[5] This can be caused by the shoulder being pushed down and the head being pulled up which causes the nerves to be stretched or torn. Injuries associated with malpositioning commonly effect the brachial plexus nerves rather than other peripheral nerve groups.[6][7] Due to the brachial plexus nerves being very sensitive to position, there are very limited ways of preventing such injuries. The most common victims of brachial plexus injuries consist of victims of motor vehicle accidents and newborns.
Motorcycle accidents
Motorcyclists who are involved accidents are very susceptible to brachial plexus injuries due to the nature of the collision. "Brachial plexus injuries were identified in 54 of 4538 patients presenting to a regional trauma facility… Motor vehicle accidents were the most frequent cause overall."[8]
Many of these patients were forced to undergo reconstructive surgery. During physical therapy, the position of the brachial plexus became very important in order to avoid further damage.[9] "The risk can be reduced by thorough release of the tissues from the inferior surface of the clavicle before mobilization of the fracture fragments."[3] By wearing protective gear, like a helmet, a motorcyclist can help prevent nerve damage after collisions.

Injuries During Birth
Brachial Plexus injuries also become an issue during the delivery of newborns. "…there were 80 brachial plexus injuries identified, for an incidence of 1.03 per 1000 live birth."[6] Nerve damage has been connected to birth weight with larger newborns being more susceptible to the injury but it also has to do with the delivery methods. Although very hard to prevent during live birth, doctors must be able to deliver a newborn with precise and gentle movements in order to decrease chances of injuring the child.
Additional images
This section contains an unencyclopedic or excessive gallery of images. |

-
Superficial dissection of the right side of the neck, showing the carotid and subclavian arteries.
-
The axillary artery and its branches.
-
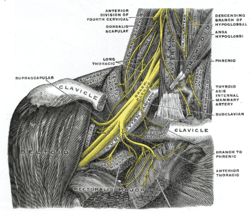
Nerves in the infraclavicular portion of the right brachial plexus in the axillary fossa.
-
Cutaneous nerves of right upper extremity.
-
Diagram of segmental distribution of the cutaneous nerves of the right upper extremity.
-
The right sympathetic chain and its connections with the thoracic, abdominal, and pelvic plexuses.
-
Side of neck, showing chief surface markings.
-
Brachial plexus with areas of roots, trunks, divisions and cords marked.
-
Color-coded diagram of brachial plexus illustrating roots of associated nerves.
-
Dissection of brachial plexus
-
Brachial plexus
-
Brachial plexus
-
Brachial plexus
-
Brachial plexus
-
Brachial plexus
See also
- Brachial plexus injury
- Anesthesia of the brachial plexus (concerning nerve blocks for surgical procedures)
References
- ^ Moore, K.L.; Agur, A.M. (2007). Essential Clinical Anatomy (3rd ed.). Baltimore: Lippincott Williams & Wilkins. pp. 434–5. ISBN 978-0-7817-6274-8.
- ^ Moore, K.L.; Agur, A.M. (2007). Essential Clinical Anatomy (3rd ed.). Baltimore: Lippincott Williams & Wilkins. pp. 430–1. ISBN 978-0-7817-6274-8.
- ^ a b Ecker, Jeffrey L.; Greenberg, James A.; Norwitz, Errol R.; Nadel, Allan S.; Repke, John T. (1997). "Birth Weight as a Predictor of Brachial Plexus Injury". Obstetrics & Gynecology. 89 (5): 643–47. doi:10.1016/S0029-7844(97)00007-0. PMID 9166293.
- ^ Moore, Keith (2006). Clinically Oriented Anatomy. Philadelphia: Lippincott Williams & Wilkins. pp. 778–81. ISBN 0-7817-3639-0.
- ^ http://www.mayoclinic.com/health/brachial-plexus-injury/DS00897/Brachial[full citation needed]
- ^ a b Cooper, DE; Jenkins, RS; Bready, L; Rockwood Jr, CA (1988). "The prevention of injuries of the brachial plexus secondary to malposition of the patient during surgery". Clinical orthopaedics and related research (228): 33–41. PMID 3342585.
- ^ Jeyaseelan, L.; Singh, V. K.; Ghosh, S.; Sinisi, M.; Fox, M. (2013). "Iatropathic brachial plexus injury: A complication of delayed fixation of clavicle fractures". The Bone & Joint Journal. 95-B (1): 106–10. doi:10.1302/0301-620X.95B1.29625. PMID 23307682.
- ^ Midha, Rajiv (1997). "Epidemiology of Brachial Plexus Injuries in a Multitrauma Population". Neurosurgery. 40 (6): 1182–8, discussion 1188–9. PMID 9179891.
- ^ http://www.webmd.com/pain-management/tc/physical-therapy-topic-overview[full citation needed]
External links
- lesson3brachialplexus at The Anatomy Lesson by Wesley Norman (Georgetown University)
- Tutorial at Newcastle University
- Blog about Brachial Plexus Injury
- Brachial Plexus Injury/Illustration, Cincinnati Children's Hospital Medical Center
- Learn the Brachial Plexus in Five Minutes or Less by Daniel S. Romm, M.D. and Dennis A. Chu Chu, M.D. [1]
- Brachial Plexus Injury/Illustration, Cincinnati Children's Hospital Medical Center