Plantar fascia
| Plantar fascia | |
|---|---|
 Muscles of the sole of the foot. First layer (closest to the skin on the sole of the foot). Plantar aponeurosis visible at top center. | |
| Details | |
| Identifiers | |
| Latin | aponeurosis plantaris |
| TA98 | A04.7.03.031 |
| TA2 | 2718 |
| FMA | 45171 |
| Anatomical terminology | |
The plantar fascia is the thick connective tissue (aponeurosis) which supports the arch on the bottom (plantar side) of the foot. It runs from the tuberosity of the calcaneus (heel bone) forward to the heads of the metatarsal bones (the bone between each toe and the bones of the mid-foot).
Structure
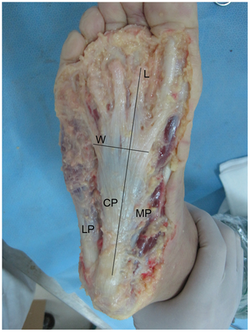
LP, lateral part; CP, central part; MP, medial part; L, length; W, width.

The plantar fascia is a broad structure that spans between the medial calcaneal tubercle and the proximal phalanges of the toes. Recent studies suggest that the plantar fascia is actually an aponeurosis rather than true fascia. The Dorland’s Medical Dictionary defines an aponeurosis as: (i) a white, flattened or ribbon-like tendinous expansion, serving mainly to connect a muscle with the parts that it moves, (ii) a term formerly applied to certain fasciae. Further, it defines the plantar aponeurosis as bands of fibrous connective tissue radiating toward the bases of the toes from the medial process of the tuber calcanei (posterior half of the calcaneus).
The plantar fascia is made up of predominantly longitudinally oriented collagen fibers. There are three distinct structural components: the medial component, the central component (plantar aponeurosis), and the lateral component (see diagram at right). The central component is the largest and most prominent.
In younger people the plantar fascia is also intimately related to the Achilles tendon, with a continuous fascial connection between the two from the distal aspect of the Achilles to the origin of the plantar fascia at the calcaneal tubercle. However, the continuity of this connection decreases with age to a point that in the elderly there are few, if any, connecting fibers. There are also distinct attachments of the plantar fascia and the Achilles tendon to the calcaneus so the two do not directly contact each other. Nevertheless, there is an indirect relationship whereby if the toes are dorsiflexed, the plantar fascia tightens via the windlass mechanism. If a tensile force is then generated in the Achilles tendon it will increase tensile strain in the plantar fascia. Clinically, this relationship has been used as a basis for treatment for plantar fasciitis, with stretches and night stretch splinting being applied to the gastrocnemius/soleus muscle unit.
Function

The plantar fascia contributes to support of arch of the foot by acting as a tie-rod, where it undergoes tension when the foot bears weight. One biomechanical model estimated it carries as much as 14% of the total load of the foot. In an experiment using cadavers, it was found that failure of the plantar fascia averaged at loads of 1189 ± 244 newtons[1] (121 ± 24 kgf or 267 ± 55 lbf). Failure most often occurred at the proximal attachment to the calcaneus, which is consistent with the usual location of symptoms (i.e. in plantar fasciitis). Complete rupture or surgical release of the plantar fascia leads to a decrease in arch stiffness and a significant collapse of the longitudinal arch of the foot. By modeling it was predicted such conditions would result in a 17% increase in vertical displacement and a 15% increase in horizontal elongation of the foot when it was loaded at 683 newtons (154 lbf).[2] Surgical release also significantly increases both stress in the plantar ligaments and plantar pressures under the metatarsal heads. Although most of the figures mentioned above are from either cadaver studies or investigations using models, they highlight the relatively large load the plantar fascia is subjected to while contributing to the structural integrity of the foot.
Gait
The plantar fascia also has an important role in dynamic function during gait. It was found the plantar fascia continuously elongated during the contact phase of gait. It went through rapid elongation before and immediately after mid-stance, reaching a maximum of 9% to 12% elongation between mid-stance and toe-off.[3] During this phase the plantar fascia behaves like a spring, which may assist in conserving energy. In addition, the plantar fascia has a critical role in normal mechanical function of the foot, contributing to the "windlass mechanism". When the toes are dorsiflexed in the propulsive phase of gait, the plantar fascia becomes tense, resulting in elevation of the longitudinal arch and shortening of the foot (see 3A). One can liken this mechanism to a cable being wound around the drum of a windlass (see 3B); the plantar fascia being the cable, the metatarsal head the drum, and the handle, the proximal phalanx.
Clinical significance
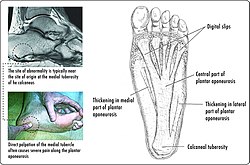
Plantar fasciitis
- Plantar fasciitis is an often painful degenerative process of the plantar fascia.
- Calcaneal spur (heel spur) is a small calcified bone extension (osteophyte) located on the inferior aspect of the calcaneus or on the back of the heel at the insertion of the Achilles tendon. The condition is typically a response to plantar fasciitis over a period of time. It may also be related to ankylosing spondylitis, typically in children.
Other
- Plantar fibromatosis is a relatively uncommon non-malignant thickening of the plantar fascia.
- Psoriatic arthritis is a type of inflammatory arthritis that may affect the plantar fascia.
- Plantar fascial rupture/tear is a relatively uncommon painful tearing of the plantar fascia. The tear can be full or partial.[4]
Additional images
-
The plantar fascia (also known as the plantar aponeurosis) is located superficially plantar side of the foot.
See also
References
- ^ H. B. Kitaoka; Z. P. Luo; E. S. Growney; L. J. Berglund; K. N. An (October 1994). "Material properties of the plantar aponeurosis". Foot & ankle international. 15 (10): 557–560. doi:10.1177/107110079401501007. PMID 7834064.
- ^ G. A. Arangio, C. Chen and W. Kim (June 1997). "Effect of cutting the plantar fascia on mechanical properties of the foot". Clinical Orthopaedics and Related Research (339): 227–231. PMID 9186224.
- ^ Amit Gefen (March 2003). "The in vivo elastic properties of the plantar fascia during the contact phase of walking". Foot & ankle international. 24 (3): 238–244. PMID 12793487.
- ^ "Plantar Fascial Tears". American Foot & Leg Specialists. 2016-10-17. Retrieved 2018-04-23.
External links
- Plantar fascia at the Duke University Health System's Orthopedics program
- soleoffoot at The Anatomy Lesson by Wesley Norman (Georgetown University) (soleoffoot1)
- Heel Pain Symptoms. Plantar Fasciitis diagnosis and treatment | Patient; plantar fasciitis at Patient.info
