Pressure reactivity index
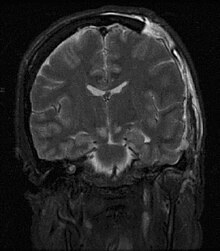
Pressure reactivity index or PRx is tool for monitoring cerebral autoregulation in the intensive care setting for patients with severe traumatic brain injury or subarachnoid haemorrhage, in order to guide therapy to protect the brain from dangerously high or low cerebral blood flow.
PRx uses mathematical algorithms to calculate the correlation between arterial blood pressure and intracranial pressure. PRx assesses for correlations at low frequencies, below 0.5 Hz, and thus ignores individual pulses while capturing the effects of respiratory-driven variation in arterial pressure as well as other longer-acting stimuli.
Under normal conditions, cerebral autoregulation ensures that cerebral blood flow is unchanged despite variations in blood pressure by regulating the cerebral vessels. For example, if the blood pressure increases, the cerebral vessels vasoconstrict to keep cerebral blood flow normal, whereas a decrease in blood pressure would lead to vasodilation of the cerebral vessels to increase blood flow. The cerebrovascular reactions to changes in blood pressure generates a corresponding effect on the intracranial pressure. When the blood pressure increases and the vessels vasoconstrict, the cerebral blood volume is reduced. According to the Monro-Kellie doctrine, less cerebral blood volume leads to a reduction in the intracranial pressure. If the blood pressure instead would decrease, the cerebral vessels would vasodilatate, with a resulting increase in cerebral blood volume.[1][2][3]
PRx and outcome prediction
A high PRx indicating disturbed pressure autoregulation predicts poor outcome in traumatic brain injury.[4][5]
PRx as a treatment target
PRx varies with the concurrent cerebral perfusion pressure (CPP) in a U-shaped way.[6] It has been suggested that the CPP with the lowest PRx is optimal (CPPopt) and CPP-values close to optimal have been associated with better outcome.[7][8] CPP values above CPPopt are believed to cause hyperemia, i.e. to high cerebral blood flow that may cause cerebral edema and intracranial hypertension, whereas CPP values below CPPopt are believed to cause hypoperfusion and ischemia resulting in tissue damage.
See also
References
- ^ Donnelly J, Czosnyka M, Adams H, Robba C, Steiner LA, Cardim D. Pressure Reactivity-Based Optimal Cerebral Perfusion Pressure in a Traumatic Brain Injury Cohort. Acta Neurochir Suppl. 2018; 126:209-212. PMID 29492563 [1]
- ^ Czosnyka M, Czosnyka Z, Smielewski P. Pressure reactivity index: journey through the past 20 years. Acta Neurochir (Wien). 2017 Nov; 159(11):2063-2065. PMID 28849287 [2]
- ^ Lang EW, Kasprowicz M, Smielewski P, Santos E, Pickard J, Czosnyka M. Short pressure reactivity index versus long pressure reactivity index in the management of traumatic brain injury. J Neurosurg. 2015 Mar; 122(3):588-94. PMID 25423266 [3]
- ^ Sorrentino, E., Diedler, J., Kasprowicz, M., Budohoski, K., Haubrich, C., Smielewski, P., Outtrim, J., Manktelow, A., Hutchinson, P. and Pickard, J. (2012). Critical thresholds for cerebrovascular reactivity after traumatic brain injury. Neurocritical care 16, 258-266.
- ^ Czosnyka, M., Smielewski, P., Kirkpatrick, P., Laing, R.J., Menon, D. and Pickard, J.D. (1997). Continuous assessment of the cerebral vasomotor reactivity in head injury. Neurosurgery 41, 11-19.
- ^ Czosnyka, M., Smielewski, P., Piechnik, S., Steiner, L.A. and Pickard, J.D. (2001). Cerebral autoregulation following head injury. Journal of neurosurgery 95, 756-763.
- ^ Aries, M.J., Czosnyka, M., Budohoski, K.P., Steiner, L.A., Lavinio, A., Kolias, A.G., Hutchinson, P.J., Brady, K.M., Menon, D.K. and Pickard, J.D. (2012). Continuous determination of optimal cerebral perfusion pressure in traumatic brain injury. Critical care medicine 40, 2456-2463.
- ^ Steiner, L.A., Czosnyka, M., Piechnik, S.K., Smielewski, P., Chatfield, D., Menon, D.K. and Pickard, J.D. (2002). Continuous monitoring of cerebrovascular pressure reactivity allows determination of optimal cerebral perfusion pressure in patients with traumatic brain injury. Critical care medicine 30, 733-738.
