Middle cerebral artery
| Middle cerebral artery | |
|---|---|
 Outer surface of cerebral hemisphere, showing areas supplied by cerebral arteries. (Pink is region supplied by middle cerebral artery.) | |
 The arterial circle and arteries of the brain. The middle cerebral arteries (top of figure) arise from the internal carotid arteries. | |
| Details | |
| Source | internal carotid arteries |
| Branches | anterolateral central arteries |
| Vein | middle cerebral vein |
| Supplies | cerebrum |
| Identifiers | |
| Latin | arteria cerebri media |
| MeSH | D020768 |
| TA98 | A12.2.07.046 |
| TA2 | 4509 |
| FMA | 50079 |
| Anatomical terminology | |
The middle cerebral artery (MCA) is one of the three major paired arteries that supplies blood to the cerebrum. The MCA arises from the internal carotid and continues into the lateral sulcus where it then branches and projects to many parts of the lateral cerebral cortex. It also supplies blood to the anterior temporal lobes and the insular cortices.
The left and right MCAs rise from trifurcations of the internal carotid arteries and thus are connected to the anterior cerebral arteries and the posterior communicating arteries, which connect to the posterior cerebral arteries. The MCAs are not considered a part of the Circle of Willis.[1]
Branches
The MCA can be classified into 4 parts:[2]
- M1: The sphenoidal segment, so named due to its origin and loose lateral tracking of the sphenoid bone. Although known also as the horizontal segment, this may be misleading since the segment may descend, remain flat, or extend posteriorly the anterior (dorsad) in different individuals. The M1 segment perforates the brain with numerous anterolateral central (lateral lenticulostriate) arteries, which irrigate the basal ganglia.
- M2: Extending anteriorly on the insula, this segment in known as the insular segment. It is also known as the Sylvian segment when the opercular segments are included. The MCA branches may bifurcate or sometimes trifurcate into trunks in this segment which then extend into branches that terminate towards the cortex.
- M3: The opercular segments and extends laterally exteriorly from the insula towards the cortex. This segment is sometimes grouped as part of M2.
- M4: These finer terminal or cortical segments irrigate the cortex. They begin at the external of the Sylvian fissure and extend distally away on the cortex of the brain.
Although the M2-M3 segments may split into 2 are 3 main trunks (terminal branches) with an upper trunk, lower trunk and occasionally a middle trunk. Bifurcations and trifurcations occurs in 50% and 25% of the cases respectively. Other cases include duplication of the MCA at the internal carotid artery (ICA) or an accessory MCA (AccMCA) which arise not from the ICA but as a branch from the anterior cerebral artery. [3] The middle trunk that exist in parts of the population, when present provides the pre-Rolandic, Rolandic, anterior parietal, posterior parietal and the angular artery for irrigation instead of the upper and lower trunks.
The branches (ramus) of the MCA can be described by the areas that they irrigate.
Frontal lobe
- Lateral frontobasal (orbitiofrontal): This branches out anterior, superior and laterally to vascularize the inferior frontal gyrus. This "competes" in size with the frontal polar branch of the anterior cerebral artery
- Prefrontal arteries: thes arteries fan out over the insula and exit to the cortex via the media surface of the frontal operculum. The arteries fan superiorly over the pars triangularis and vascularizes the inferior and middle frontal gyrus. Near the superior frontal gyrus these arteries anastamoses with branches from the pericallosal artery of the anterior cerebral artery.
- Pre-Rolandic artery (precentral): The artery extends out on the media surface of the operculum and supplies the posterior parts of the middle and inferior frontal gyri as well as the lower parts of the pre-central gyrus. This artery branches once or twice and is relatively invariant across anatomies.
- Rolandic arteries (central): The artery extends out and exits from the central portion of the operculum, then passing inside the central sulcus. This artery bifurcates in 72% of individuals and irrigate the posterior pre-central gyrus and the inferior portion of the post-central gyrus.
Parietal lobe
- Anterior parietal: This artery usually originates from the anterior or middle MCA trunk. In some cases it branches from the rolandic artery or from the posterior parietal artery. Extends the interparietal sulcus and descends slightly posteriorly.
- Posterior parietal: Emerging from the posterior end of the Sylvian fissure and extends first posteriorly, and then anteriorly along the posterior of the parietal lobe. It also branches to the supramarginal gyrus.
- Angular: The angular artery is a significant terminal branch of the anterior or middle trunk of the MCA. It emerges from the Sylvian fissure and passes over the anterior transverse temporal gyrus and usually divides into two branches. One to the branches supply the angular gyrus while the other supplies the supramarginal gyrus, posterior superior temporal gyrus, and the parietooccipital arcus (sulcus).
- Temporaloccipital: The longest cortical artery, it run posteriorly and opposite to operculum centre upon its exit from the Sylvian fissure, it run parallel to the superior temporal sulcus and supplies the superior and inferior occipital gyri. This vessel anastamoses with the posterior cerebral artery and may exist as one or two arteries, 67% or 33% of the time, respectively.
Temporal lobe
- Temporopolar: The artery extends from the sphenoidal segment of the MCA via the operculum inferior surface and supplies the polar and anterior lateral portions of the temporal lobe. The vessel can be identified in 52% of normal angiograms
- Anterior temporal:This artery extends in the similar fashion and the temporopolar and vascularizes the same regions.
- Middle temporal: This artery extends from the Slyvian fissure opposite to the inferior frontal gyrus and suppies the superior and middle portion of the middle temporal lobe. It can be identified in 79% of angiograms.
- Posterior temporal:This artery extends out and away from the operculum and turns in a step-wise manner first inferiorly then posteriorly into the superior temporal sulcus than to the middle temporal sulcus. This vessel supplies the posterior portion of the temporal lobe and is the origin of several perforating arteries that irrigate the insula. It is readily identifiable most radiograms.
Areas supplied
Areas supplied by the middle cerebral artery include:
- The bulk of the lateral surface of the hemisphere; except for the superior inch of the frontal and parietal lobe (anterior cerebral artery), and the inferior part of the temporal lobe.
- Superior division supplies lateroinferior frontal lobe (location of Broca's area i.e. language expression)
- Inferior division supplies lateral temporal lobe (location of Wernicke's area i.e. language comprehension)
- Deep branches supply the basal ganglia as well as the internal capsule
Occlusion
Occlusion of the middle cerebral artery may result in the following defects:
- Paralysis (-plegia) or weakness (-paresis) of the contralateral face and arm (faciobrachial)
- Sensory loss of the contralateral face and arm.
- Damage to the dominant hemisphere (usually the left hemisphere, since most individuals are right-handed) results in aphasia i.e. Broca's or Wernicke's
- Damage to the non-dominant hemisphere (usually the right hemisphere) results in contralateral neglect syndrome
- Large MCA infarcts often have a gaze preference towards the side of the lesion, especially during the acute period. Contralateral homonymous hemianopsia is often present.
Additional images
-
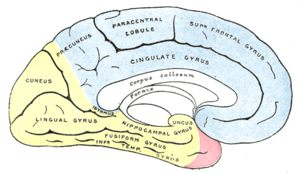
Medial surface of cerebral hemisphere, showing areas supplied by cerebral arteries.
-
Arteries at base of brain: middle cerebral artery at upper left. The temporal pole of the cerebrum and a portion of the cerebellar hemisphere have been removed on the right side. Inferior aspect (viewed from below).
See also
References
- ^ Moore KL, Dalley AR. Clinically Oriented Anatomy, 4th Ed., Lippincott Williams & Wilkins, Toronto. Copyright 1999. ISBN 0-683-06141-0.
- ^ Krayenbühl, Hugo; Yaşargil, Mahmut Gazi; Huber, Peter; Bosse, George (1982), Cerebral Angiography, Thieme, pp. 105–123, ISBN 9780865770676
- ^ Osborn, Anne G.; Jacobs, John M. (1999), Diagnostic Cerebral Angiography, Lippincott Williams & Wilkins, pp. 143–144, ISBN 9780397584048
External links
- MedEd at Loyola Neuro/neurovasc/navigation/mca.htm
- Anatomy photo:28:09-0215 at the SUNY Downstate Medical Center
- Template:RocheLexicon
- Blood supply at neuropat.dote.hu