Synovial fluid
| Synovial fluid | |
|---|---|
 A typical joint | |
| Details | |
| Identifiers | |
| Latin | synovia |
| MeSH | D013582 |
| TA98 | A03.0.00.031 |
| TA2 | 1535 |
| FMA | 12277 |
| Anatomical terminology | |
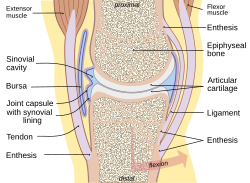
Synovia, more often called synovial fluid,[help 1] is a viscous, non-Newtonian fluid found in the cavities of synovial joints. With its egg white–like consistency,[1] the principal role of synovial fluid is to reduce friction between the articular cartilage of synovial joints during movement.
Structure
The inner membrane of synovial joints is called the synovial membrane and secretes synovial fluid into the joint cavity. Synovial fluid is an ultrafiltrate from plasma, and contains proteins derived from the blood plasma and proteins that are produced by cells within the joint tissues.[2] The fluid contains hyaluronan secreted by fibroblast-like cells in the synovial membrane, lubricin (proteoglycan 4; PRG4) secreted by the surface chondrocytes of the articular cartilage and interstitial fluid filtered from the blood plasma.[3] This fluid forms a thin layer (roughly 50 μm) at the surface of cartilage and also seeps into microcavities and irregularities in the articular cartilage surface, filling all empty space.[4] The fluid in articular cartilage effectively serves as a synovial fluid reserve. During movement, the synovial fluid held in the cartilage is squeezed out mechanically to maintain a layer of fluid on the cartilage surface (so-called weeping lubrication). The functions of the synovial fluid include:
- reduction of friction — synovial fluid lubricates the articulating joints[5][page needed]
- shock absorption — as a dilatant fluid, that possesses rheopectic properties,[6] becoming more viscous under applied pressure; the synovial fluid in diarthrotic joints becomes thick the moment shear is applied in order to protect the joint and subsequently, thins to normal viscosity instantaneously to resume its lubricating function between shocks.[7] [dubious – discuss]
- nutrient and waste transportation — the fluid supplies oxygen and nutrients and removes carbon dioxide and metabolic wastes from the chondrocytes within the surrounding cartilage
- molecular sieving - pressure within the joint forces hyaluronan in the fluid against the synovial membrane forming a barrier against cells migrating into, or fluid migrating out of, the joint space. This function is dependent on the molecular weight of the hyaluronan.[8]
Composition
Synovial tissue is sterile and composed of vascularized connective tissue that lacks a basement membrane. Two cell types (type A and type B) are present: Type A is derived from blood monocytes, and it removes the wear-and-tear debris from the synovial fluid. Type B produces hyaluronan. Synovial fluid is made of hyaluronic acid and lubricin, proteinases, and collagenases. Synovial fluid exhibits non-Newtonian flow characteristics; the viscosity coefficient is not a constant and the fluid is not linearly viscous. Synovial fluid has rheopexy characteristics; viscosity increases and the fluid thickens over a period of continued stress.[9] Normal synovial fluid contains 3–4 mg/ml hyaluronan (hyaluronic acid),[10] a polymer of disaccharides composed of D-glucuronic acid and D-N-acetylglucosamine joined by alternating beta-1,4 and beta-1,3 glycosidic bonds.[11][unreliable medical source?] hyaluronan is synthesized by the synovial membrane and secreted into the joint cavity to increase the viscosity and elasticity of articular cartilages and to lubricate the surfaces between synovium and cartilage.[12][unreliable medical source?]
Synovial fluid contains lubricin (also known as PRG4) as a second lubricating component, secreted by synovial fibroblasts.[13] Chiefly, it is responsible for so-called boundary-layer lubrication, which reduces friction between opposing surfaces of cartilage. There also is some evidence that it helps regulate synovial cell growth.[14]
It also contains phagocytic cells that remove microbes and the debris that results from normal wear and tear in the joint.
Clinical significance
Collection
Synovial fluid may be collected by syringe in a procedure termed arthrocentesis, also known as joint aspiration.
Classification
Synovial fluid may be classified into normal, noninflammatory, inflammatory, septic, and hemorrhagic:
| Normal | Noninflammatory | Inflammatory | Septic | Hemorrhagic | |
| Volume (ml) | <3.5 | >3.5 | >3.5 | >3.5 | >3.5 |
| Viscosity | High | High | Low | Mixed | Low |
| Clarity | Clear | Clear | Cloudy | Opaque | Mixed |
| Color | Colorless/straw | Straw/yellow | Yellow | Mixed | Red |
| WBC/mm3 | <200 | <2,000[15] | 5,000[15]-75,000 | >50,000[15] | Similar to blood level |
| Polys (%) | <25 | <25[15] | 50[15]-70[15] | >70[15] | Similar to blood level |
| Gram stain | Negative | Negative | Negative | Often positive | Negative |
Glucose (mg/dl) concentration in synovial fluid is nearly equal to serum.
- Synovial fluid viscosity
Normal:
- Normal
- Traumatic arthritis
- Degenerative (Osteo) arthritis
- Pigmented villonodular synovitis
Normal or decreased:
- Systemic lupus erythematosus
Decreased:
- Rheumatic fever
- Rheumatoid arthritis
- Gout
- Pyogenic (Septic) arthritis
- Tubercular arthritis
Pathology

Many synovial fluid types are associated with specific diagnoses:[16][17]
- Noninflammatory (Group I)
- Osteoarthritis, degenerative joint disease
- Trauma
- Rheumatic fever
- Chronic gout or pseudogout
- Scleroderma
- Polymyositis
- Systemic lupus erythematosus
- Erythema nodosum
- Neuropathic arthropathy (with possible hemorrhage)
- Sickle-cell disease
- Hemochromatosis
- Acromegaly
- Amyloidosis
- Inflammatory (Group II)
- Rheumatoid arthritis
- Reactive arthritis
- Psoriatic arthritis
- Acute rheumatic fever
- Acute gout or pseudogout
- Scleroderma
- Polymyositis
- Systemic lupus erythematosus
- Ankylosing spondylitis
- Inflammatory bowel disease arthritis
- Infection (viral, fungal, bacterial) including Lyme disease
- Acute crystal synovitis (gout)
- Septic (Group III)
- Pyogenic bacterial infection
- Septic arthritis
- Hemorrhagic
- Trauma
- Tumors
- Hemophilia/coagulopathy
- Scurvy
- Ehlers-Danlos syndrome
- Neuropathic arthropathy
Analysis
Glucose (mg/dl) concentration in synovial fluid is nearly equal to serum.
The cytological and biochemical analysis of human synovial fluid began around 1940 using cadaver-derived fluid and comparing characteristics to those of, for instance, bovine synovial fluid.[18]
Chemistry
The mucin clot test is a very old approach to determining if an inflammatory infiltrate is present. In this test, acetic acid is added to the synovial fluid specimen. In a normal specimen, this should lead to a congealing of the hyaluronic acid, forming a 'mucin clot.' If inflammation is present, a mucin clot is not formed (the hyaluronic acid is degraded).[19]
Lactate is elevated in septic arthritis, usually above 250 mg/dL.
Complement factors are decreased in rheumatoid arthritis and lupus arthritis.
Microscopy
Microscopic analysis of synovial fluid is performed to evaluate for cell count and crystals. Crystals include monosodium urate, calcium pyrophosphate, hydroxyapatite and corticosteroid crystals.[19]
Monosodium urate crystals are seen in gout/gouty arthritis and appear as needle-shaped negatively birefringent crystals varying in length from 2 to 20 µm. With negative birefringence, the crystals appear yellow in parallel light and blue with perpendicular light.
Calcium pyrophosphate crystals are seen in pseudogout (also known as calcium pyrophosphate deposition disease or, CPPD). These crystals are rod-shaped or rhomboids varying in length from 2 to 20 µm and with positive birefringence (blue with parallel light, yellow with perpendicular light).
Hydroxyapatite crystals are small and negatively birefringent. They are usually only detectable with an Alizarin Red S stain.
Corticosteroid crystals may be seen following therapeutic corticosteroid injection into the joint space. They appear blunt, jagged, and show variable birefringence.[19]
Cracking joints
When the two articulating surfaces of a synovial joint are separated from one other, the volume within the joint capsule increases and a negative pressure results. The volume of synovial fluid within the joint is insufficient to fill the expanding volume of the joint and gases dissolved in the synovial fluid (mostly carbon dioxide) are liberated and quickly fill the empty space, leading to the rapid formation of a bubble.[20] This process is known as cavitation. Cavitation in synovial joints results in a high frequency 'cracking' sound.[21][22]
Etymology and pronunciation
The word synovia (/s[invalid input: 'ɨ']ˈnoʊviə/) came to English from New Latin,[23][24][25] where it was coined by Paracelsus.[24][25] Several dictionaries[26][27] indicate that the -ov- syllable of the word reflects the Greek ᾠόν and Latin ovum, cognates that both mean "egg" (which seems appropriate given the egg white–like nature of synovial fluid)—thus syn- + oo-/ovo- + -ia—although several others omit that aspect of the etymology,[23][24][25] and one states, "probably formed arbitrarily by Paracelsus."[25] Whether true or false, the connection to ovum is still helpful to students as a memory device.
Somewhat confusingly, the inflected form synovia can be either a principal (and uncountable) declined form referring to synovial fluid (synovia) or a second declined form as the plural of synovium (thus "synovial membranes", synovia). The avoidance of this ambiguity drives the use of the term synovial fluid to be more common than the use of its synonym synovia.
References
- ^ West, Sterling G. (2015). Rheumatology secrets. The secrets series (3rd ed.). Philadelphia: Elsevier Mosby. p. 19. ISBN 9780323037006. OCLC 908716294.
- ^ Bennike, Tue; Ayturk, Ugur; Haslauer, Carla M.; Froehlich, John W.; Proffen, Benedikt L.; Barnaby, Omar; Birkelund, Svend; Murray, Martha M.; Warman, Matthew L. (2014-09-03). "A Normative Study of the Synovial Fluid Proteome from Healthy Porcine Knee Joints". Journal of Proteome Research. 13 (10): 4377–4387. doi:10.1021/pr500587x. PMC 4184458. PMID 25160569.
- ^ Jay GD, Waller KA (2014). "The biology of lubricin: near frictionless joint motion". Matrix Biology. 39: 17–24. doi:10.1016/j.matbio.2014.08.008. PMID 25172828.

- ^ Edwards, Jo, ed. (2000). "Normal Joint Structure". Notes on Rheumatology. University College London. Archived from the original on 19 Nov 2012. Retrieved 5 April 2013.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ McCracken, Thomas, ed. (2000). New Atlas of Human Anatomy. China: MetroBooks. ISBN 9781586630973. OCLC 850877694.
- ^ Christorpher, GF. "The role of protein content on the steady and oscillatory shear rheology of model synovial fluids". Royal Society of Chemistry. 2014 (10): 5965–5973. doi:10.1039/C4SM00716F.
- ^ "Synovial fluid - OrthopaedicsOne Articles - OrthopaedicsOne". Retrieved 20 September 2016.
- ^ Sabaratnam S, Arunan V, Coleman PJ, Mason RM, Levick JR (2005). "Size selectivity of hyaluronan molecular sieving by extracellular matrix in rabbit synovial joints". The Journal of Physiology. 567 (Pt 2): 569–81. doi:10.1113/jphysiol.2005.088906. PMID 15961430.

- ^ <Oates, Katherine (2006). "Rheopexy of synovial fluid and protein aggregation". The Journal of the Royal Society Interface. 3: 167–74. doi:10.1098/rsif.2005.0086. PMC 1618490. PMID 16849228.
{{cite journal}}:|archive-date=requires|archive-url=(help); Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Hui, Alexander Y.; McCart, William J.; Masuda, Koichi; Firestein, Gary S.; Sah, Robert L. (Jan–Feb 2012). "A Systems Biology Approach to Synovial Joint Lubrication in Health, Injury, and Disease". Systems Biology and Medicine. Wiley Interdisciplinary Reviews. 4 (1): 15–7. doi:10.1002/wsbm.157. PMC 3593048. PMID 21826801.
- ^ "GlycoForum / Science of Hyaluronan". 15 December 1997.
- ^ "Joints". University of Washington Medicine - Department of Orthopaedics and Sports Medicine. Retrieved 2013-02-04.
- ^ Jay, GD; Britt, DE; Cha, CJ (March 2000). "Lubricin is a product of megakaryocyte stimulating factor gene expression by human synovial fibroblasts". J Rheumatol (abstract). 27 (3): 594–600. PMID 10743795.
- ^ Warman M (2003). "Delineating biologic pathways involved in skeletal growth and homeostasis through the study of rare Mendelian diseases that affect bones and joints". Arthritis Research & Therapy. 5 (Suppl 3): S2. doi:10.1186/ar804.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ a b c d e f g Table 6-6 in: Elizabeth D Agabegi; Agabegi, Steven S. (2008). Step-Up to Medicine (Step-Up Series). Hagerstwon, MD: Lippincott Williams & Wilkins. ISBN 0-7817-7153-6.
- ^ "Lupus Anticoagulant". Family Practice Notebook. Archived from the original on 18 January 2013. Retrieved 7 April 2013.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ American College of Rheumatology Archived September 5, 2004, at the Wayback Machine
- ^ Ropes, Marian W.; Rossmeisl, Elsie C.; Bauer, Walter (November 1940), "The Origin and Nature of Normal HUman Synovial Fluid" (scanned pages), J Clin Invest, 19 (6): 795–799, doi:10.1172/JCI101182, PMID 16694795, retrieved 6 April 2013 and references therein
- ^ a b c De Mais, Daniel (2009), Quick Compendium of Clinical Pathology (2nd ed.), Chicago: ASCP Press, ISBN 9780891895671, OCLC 692198047[pages needed]
- ^ Unsworth A, Dowson D, Wright V (1971). "'Cracking joints'. A bioengineering study of cavitation in the metacarpophalangeal joint". Ann Rheum Dis. 30 (4): 348–58. doi:10.1136/ard.30.4.348. PMC 1005793. PMID 5557778.
- ^ Watson P, Kernoham WG, Mollan RAB. A study of the cracking sounds from the metacarpophalangeal joint. Proceedings of the Institute of Mechanical Engineering [H] 1989;203:109-118.
- ^ "What makes your knuckles pop?". 3 August 2000. Retrieved 20 September 2016.
- ^ a b Merriam-Webster, Merriam-Webster's Unabridged Dictionary, Merriam-Webster.
- ^ a b c Houghton Mifflin Harcourt, The American Heritage Dictionary of the English Language, Houghton Mifflin Harcourt.
- ^ a b c d Oxford Dictionaries, Oxford Dictionaries Online, Oxford University Press.
- ^ Elsevier, Dorland's Illustrated Medical Dictionary, Elsevier.
- ^ Wolters Kluwer, Stedman's Medical Dictionary, Wolters Kluwer.
Further reading
- Warman M., Delineating biologic pathways involved in skeletal growth and homeostasis through the study of rare Mendelian diseases that affect bones and joints, Arthritis research & therapy 2003, 5(Suppl 3):5, doi:10.1186/ar804. Accessed 2015-11-14.
