Talk:Vitamin D/Archive 1
| This is an archive of past discussions about Vitamin D. Do not edit the contents of this page. If you wish to start a new discussion or revive an old one, please do so on the current talk page. |
| Archive 1 | Archive 2 | Archive 3 | → | Archive 5 |
[Dead links]
Dead links:
- http://www.orst.edu/dept/lpi/infocenter/vitamins/vitaminD/index.html
- http://www.innvista.com/health/healvitd.htm
--Menchi 23:02 15 Jul 2003 (UTC)
Natural source of vitamine D
Does anybody know if there is an easily eatable natural source of vitamine D without huge amount of vitamine A inside the same package ? —Preceding unsigned comment added by 83.228.145.50 (talk • contribs) 14:52, 1 January 2006
- The sun, actually. —Preceding unsigned comment added by 80.202.97.157 (talk • contribs) 09:10, 5 September 2006
I doubt this information
Although I am not an expert, I have problems with this bit:
Oral overdose of vitamin D3
Overdose is extremely rare whilst mild deficiencies are very common.
For overdose to occur chronic doses of 100x the standard RDA each day, over many months is normally required. The RDA itself is in fact more than 200x less than the amount that may be generated in even a few minutes of midday sunshine. But whilst the sunshine generated quantity is self-limiting, vitamin pills are not and this has led to widespread concern, which may have been very much misplaced.
In practice, all common foods and correctly formulated vitamin pills essentially contain far too little for overdose to ever occur in normal circumstances. Indeed, Stoss therapy involves taking a dose over a thousand times the daily RDA once every few months and even then often fails to normalise vitamin D3 levels in the body.
However, oral overdose has been recorded due to manufacturing and industrial accidents and leads to hypercalcemia and atheroschlerosis, so overdose is very definitely possible.
"100x" and "200x" are very arbitrary numbers, and I have problems even with the x's. I guess "times" would be more professional, and There is no specified amount in weight, which I think is more scientifically sound. In addition, the details are very arbitrary yet extreme, refering to "amount generated in a few minutes of sunshine" and such.blueaster
- The world is not clear-cut- vitamin D production varies with age, skin colour etc.WolfKeeper
In addition, the article suggests that even with supplements and treatment, people can still lack vitamin D while I remember a News Magazine article stating that people should avoid vitamin D supplements while sunlight and foods should be a sufficient source.blueaster
- I've checked the nutritional breakdown of foods. Most foods contain no vitamin D. A very few, like eggs contain 20%. It's nearly impossible to get the RDA from unsupplemented food alone. (Oily fish is about the only really good source). And the RDA will eventually leave you deficient. Sunlight depends on latitude and exposure at the right time (n.b. ~20% of Indians - in India - are borderline deficient).WolfKeeper
- To be honest, I think scientists don't know what the optimum intake of vitamin D is. There is a reasonable argument that says that the RDA is too low. The argument that says it is too high, or unnecessary seems quite weak. As I understand it, it's looking at the moment like the RDA will increase.WolfKeeper
Also, from basic nutritional knowledge, I know that as vitamin D is a fat-soluble vitamin, it can be stored for periods and does not have to be consumed as often as water-soluble ones (not K, A, D, or E).blueaster
- That's quite true. But the potential storage is *massive* compared to the daily RDA; and there seem to be chemical reactions that control the level provided you aren't taking more than 200x the RDA or so.WolfKeeper
In addition, I distinctly remember reading in my chemistry textbook that a group of scientists killed and ate a polar bear during a trip and they all came down with vitamin D poisoning, as the liver of a polar bear contains about 1300 times the recomended daily amount of vitamin D. blueaster
- No, deaths and illnesses from polar bear liver are due to vitamin A. Vitamin A is unquestionably more toxic- even the RDA isn't much less than the amount needed to max out the liver stores, and the excess is very definitely toxic. There's even evidence that sub-rda amounts of vitamin A cause osteoporosis. Vitamin A is very scary. I've been on Accutane, so I know about vitamin A toxicity first hand. WolfKeeper
- Vitamin A is unquestionably more toxic.
hint: next time do some research prior to state such nonsenses. You have no idea, calciferols are potent poisons. Vitamin A is considered only "harmful", calciferols are "very toxic". You'd know this if you took 10 minutes of your time and used google before writing something like this.--Spiperon 14:06, 13 October 2006 (UTC)
So this claim with a treatment with recieving 1000 times RDA seems ridiculous. And I do not understand how it is plausible for any accident to end in oral consumption of vitamin D during manufacture.I could think up of a slap-stick scene that results in this, but not anything that would happen in real life.
- The article does say that overdose is very rare. There has been a case of incorrectly formulated vitamin pills where they had 1000x the correct dose. WolfKeeper
I highly suspect that this part of the article is biased and has been written by either a misinformed person who is not an expert (although I am not an expert either), or a person in whose business interests are involved with the sale of vitamin D supplements. WE NEED AN EXPERT TO EVALUATE THIS RIGHT NOW!!!. And I do not know why it is called "D3". blueaster
- Just for the record, I wrote the bit you have criticised. I don't have any financial involvement in any vitamin D production, sale or anything else. So far as I can tell, vitamin D toxicity essentially never happens. It all looks like a big mess up. Vitamin D toxicity involves taking an entire bottle of tablets everyday for months, and you can't get it from food. Vitamin A toxicity- you can get that by eating a not-ridiculous amount of liver or a few tablets a day. If you can find any information that contradicts what I have written, please point us to it, I'd love for a bit more balance in this article if there's any to be found.WolfKeeper
- You all above may doubt and consider vitamins D to be safe, but its still vitamin D3 that is used as a rodenticide (rat and mice poison). And no, calciferols, as defined by LD50, are far more toxic than retinol/axerophthol (vitamin A). Just try to take 100.000 IU/kg (that is 2.5 mg (cholecalciferol)/kg), you'll see. And if you look on MSDS's of retinol and calciferols, you will see that vitamin A is labeled as "harmful" (Xn), whereas vitamins D are all labeled "very toxic" (T+), which is quite a difference. Think about it.--Spiperon 14:02, 13 October 2006 (UTC)
Vitamin D toxicity can and did happen. It causes metastatic soft tissue calcification. It can be fatal. In the heydey of vitamin D supplementation, earlier in the last century, many cases of toxicity and even death were recorded. (See: Bicknell and Prescott: The Vitamins in Medicine, 3rd Ed., 1952 -- great reviews of vitamin therapy up to that date.) Vitamin D in doses of 100-150,000 IUs per day were used in the treatment of several diseases, including tuberculosis, lupus and autoimmune diseases. This treatment was often successful, but such vitamin D doses are on the verge of the toxic, and some subjects did succumb to poisoning. Today, vitamin D poisoning is rare, mostly because the high-potency preparations that were available at that time are not now available. Given the current vitamin D mania (haha), high-potency preps will probably become available once again, and toxicity cases will be reported. Still in all vitamin D deficiency is unquestionably much more important as a public health issue than vitamin D intoxication ever was, or ever will be. --AEL—Preceding unsigned comment added by 216.86.90.226 (talk • contribs) 05:06, 28 August 2006
By the way, the vitamin A phobia is a bit much, here. Vitamin A can be toxic, like vitamin D, but you have to take a whole hell of a lot of it. Also, there is old evidence (see, again, The Vitamins in Medicine, vitamin D monograph) as well as new evidence, that vitamins A and D are complementary or even synergistic in important ways, and that they should probably always be used together -- just as they often occur in nature. For example (back to The Vitamins in Medicine), it seems that supplementary vitamin A protects against vitamin D intoxication, at least in animals (no human clinical work is available, AFAIK). At the same time, from more modern literature it appears that vitamin A inhibits the enzyme that degrades vitamin D (medline # 16289102), thereby extending the active life of vitamin D. There is also evidence (pre-clinical) that the combination of vitamins A and D have anti-cancer effects beyond that of either vitamin alone. (And recall that vitamin A is an anti-cancer vitamin, also.) But, you might ask, how could vitamin A protect against vitamin D intoxication while also being "pro- vitamin-D", biochemically? I don't know the answer, but my guess is that it is a matter of dose and circumstance. Often, what occurs at one dose can be reversed at a much higher dose, or under different conditions. Vitamin A might have a "pro-vitamin-D" effect at physiologic levels, but then reverse itself and act, effectively, as an anti-vitamin-D at higher levels or under the circumstance of vitamin D intoxication. I expect that vitamin A will indeed protect against vitamin D intoxication in humans -- at least in humans who are smart enough to take the two (naturally associated) vitamins together, rather than mega-dosing with them separately. I also expect that vitamin D will protect against vitamin A intoxication. Just eyeballing the thing, that would seem a no-brainer, since vitamin D has actions on calcium metabolism roughly the opposite of vitamin A. Bottom line: take vitamin A and D as they come in granny's old-fashioned cod liver oil! For the most part, forget isolated vitamin D, isolated omega-3s, etc. Use the whole food for multiple benefits AND protection against any possible untoward effects. Use isolated vitamin D in modest amounts, perhaps for the winter months, if you live in a northern clime and/or if you have a lot of melanin (i.e. if you're black). But whatever you do, keep up with the cod liver oil. --AEL [who owns no stock in cod liver oil companies. :-) ] —Preceding unsigned comment added by 216.86.90.226 (talk • contribs) 05:36, 28 August 2006
Is vitamin D truly a "vitamin"?
The current (Aug 14, 2005) version of the entry about vitamin D starts off with the implication that it is improperly referred to as a vitamin. I have a problem with this. Originally, vitamins were identified and measured based on their "bioactivity", their efficacy in animal models. The discovery of vitamins surely owes much to the rickets that resulted when animals were housed away from natural light sources, in rooms lit by the incandescent light bulb. The rickets that ensued in laboratory rats could be cured by adding some cod liver oil to their diets. The result was the discovery of the accessory food factor, antirachitic A.
Casimir Funk's 1912 book (in German, translated to English in 1922) refers repeatedly to vitamine A (the first "vitamin") as "antirachitic A". (cited in Wikipedia under "vitamin"). I emphasize that what was originally called vitamin A had antirachitic bioactivity; i.e. the first vitamin was what we now call vitamin D.
Why are we now even thinking of the question whether vitamin D, with its antirachitic bioactivity, is or is not truly a "vitamin"? It is a debate that hinges on the misconception that a vitamin is something that must only be available through the diet. That concept is a misunderstanding. Indeed, vitamin D is truly a vitamin in every sense of the word.
Probably the best way to think of vitamin D (cholecalciferol) is as "the sunshine vitamin". What we need to consume orally, as for the rats in their dimly lit rooms of long ago, should be designed to replace what we are not getting from sunshine.
The real debate should be whether vitamin D2 is truly a vitamin. That molecule is not naturally present in primates, and it has different bioactivity potency than cholecalciferol. Furthermore, should the many "vitamin D analogs" being developed by the pharmaceutical industry to mimic the hormone derived from the vitamin D molecule be called, vitamin D? I would argue that these compounds that relate to pharmacology should never ever be called "vitamin".
This debate has gone on for years. For a supposedly authoratative paper that deserves much revision because it is wrong in its definition of vitamin D, the reader may wish to go to the IUPAC website IUPAC-IUB Joint Commission on Biochemical Nomenclature (JCBN) Nomenclature of Vitamin D Recommendations 1981 at the following address: http://www.chem.qmul.ac.uk/iupac/misc/D.html —Preceding unsigned comment added by Reinhold (talk • contribs) 20:45, 14 August 2005(UTC)
"Irridated"?
...what's this about D5 being also known as "irridated 7-dehydrositosterol"? Is that supposed to be "irradiated", perhaps? Does anyone have any clue as to what this means? Google shows "irridate" and "irridation" being used only as misspellings for "irradiate" and "irradiation", and "irridated" is only found in Wikimirrors of this very article - but giving the formal name of a substance as "irradiated (whatever)" doesn't make any sense.
Normally, I'd consider it to be just tiny gibberish-vandalism, and snip it out wholesale, but the fact that it was contributed by a registered user with a substantial edit history who continued making reasonable edits afterwards... I dunno.
I'm going to be bold and snip it out, but I left him a (slightly more detailed) message on his talk page about this, and if anyone else knows what the hell it means, could you explain? Thanks. DS 14:23, 14 September 2005 (UTC)
- Yeah, AFAIK they produce it by exposing fat bearing products to UV (i.e. irradiated with UV); and the vitamin D gets created automagically (or some such thing). That's how the fortification works. So you snipped out correct info. Congrats.WolfKeeper 12:23, 28 August 2006 (UTC)
gasp
From typing in some ingredients from my calcium/vit D supplement into google, I have found:
vitamin D is more of a horomone, not a vitamin
and we make more than enough vitamin D with 20 minutes of sunshine a day, but taking supplements risks overdose (we obviously wouldnt produce it ourselves to the point of poisoning, however)
- It's not true *most* of the year in *most* of Europe for example. Between summer exposures you're running on stores which gradually deplete. The stores are large, but studies have shown that say more than 10% of people in even very sunny climates (India!) are clinically deficient at any one time. That's not good! From the figures I've seen, the risks of overdose from pills provided you don't take absolutely ridiculous numbers of pills is, quite frankly, zero. I suppose if you lived in Hawaii, went out in the midday sun for 20 minutes everyday, AND took handfulls of pills, maybe you might, eventually hit overdose. But probably skin cancer would get you first.WolfKeeper 08:39, 23 September 2005 (UTC)
i will have to either find many sites that say this, or find a scientific journal piece that verifies this, but how come I dont remember reading this information on this article?
btw, i googled Cholecalciferol to get the sites. Blueaster 02:27, 23 September 2005 (UTC)
Correction needed in refrence to Breastfeeding and Vit D deficenciey
The following refrences show that if the Mother has sufficent amounts of Vitamin D it will be passed on the the child.
American Journal of Clinical Nutrition, Vol. 79, No. 5, 717-726, May 2004. Other references can be found by searching Sunlight Deficiency, Vitamin D, and Breastfeeding by AMMAWELL since Im new at this I will correct the info when I figure it out Smilesalot2u 01:15, 1 December 2005 (UTC)
Citation needed
I find this statement to be dubious: "For example, in the United States, those living north of a line from San Francisco to Atlanta will not be able to produce it at all for 3 to 6 months a year." If it is true, I think it needs a citation. Plus San Francisco and Atlanta differ greatly in latitude. It makes no sense to use a line that is not even close to being parallel to a latitude line. —Preceding unsigned comment added by Edgar181 (talk • contribs) 11:58, 19 January 2006
Of course, you never lose the ability to produce vitamin D. It is all a matter of how much, given the limited sun exposure at certain latitudes, and given typical (indoors, lots of clothes) lifestyles. --AEL —Preceding unsigned comment added by 216.86.90.226 (talk • contribs) 04:51, 28 August 2006
Correction of RDA figure needed
Hmm, here in America anyway, 200 I.U. equates to 50% RDA. 400 I.U. is, according to at least three of the supplements I have, in fact 100% RDA of Vitamin D. I would request the figures be corrected to correspond with reality, if no one objects. Please, folks, are my pill bottles lying or is the info on this particular Wiki article incorrect/outmoded? Is 100% RDA of Vitamin D 200 I.U. or 400 I.U.? —Preceding unsigned comment added by 70.226.168.195 (talk • contribs) 17:21, 1 February 2006
- In the UK I have pills marked: 10 micrograms, 400 IU 'EC RDA 200%'. And another marked: 7.5 micrograms 300 IU, RDA 150%WolfKeeper 02:39, 2 February 2006 (UTC)
- See [1] they have different RDAs for different age groups. Maybe your pills are for seniors???WolfKeeper 02:42, 2 February 2006 (UTC)
Steroid?
The following link says that it's a steroid. [2]WolfKeeper 20:54, 2 April 2006 (UTC)
- Many people (physicians, physiologists, university professors) make the mistake of saying that vitamin D is a steroid. This is probably because (like steroids) it is derived from cholesterol and has carbon backbone that resembles the steroid backbone. Nevertheless, all steroids have four fused rings. Vitamin D does not have four fused rings, hence it is not a steroid. --David Iberri (talk) 20:58, 2 April 2006 (UTC)
In reality, Vitamin D is a seco-sterol molecule. But since its derived from 7 dehydro-cholesterol, people say that it is a steroid hormone. seco-sterol is the correct term and should be in the article (so I will put it there next to fat soluble). srlasky 17:32, 25 April 2006 (UTC)
- I've also encountered the term lysosteroid and used it in a related article (though I can't immediately recall which one) a while back. I'll see if I can dig that up when I have a moment. --David Iberri (talk) 04:46, 26 April 2006 (UTC)
- Apparently no one else has heard of lysosteroid, as googling returns a single page—the one I recently edited (Cholecalciferol). :-( So I've changed it to secosteroid, which is in very wide use. Now I'm off to complain to my biochem professor for using lysosteroid to begin with... Thanks for clearing this up, srlasky. --David Iberri (talk) 16:24, 28 April 2006 (UTC)
Units of measure
How much is "3.5 oz."? The article ounce gives two different units of mass (avoirdupois ounce = 28.35 g and troy ounce = 31.1025 g) and two different units of volume(28.41 ml and 29.57ml).
How much is "1 tablespoon"? —Preceding unsigned comment added by Urod (talk • contribs) 00:45, 24 April 2006
Cleanup Request
I would flag this article for cleanup, but I am unsure which cleanup tag to use. At the current point in time, the article is missing critical information in various sections, and as such, is troublesome to understand. If you read through the overview, you should understand what I mean. So, yeah. If someone with a little more experience at this than me put the right cleanup tag on the article, that would be great. LuNatic 03:40, 8 June 2006 (UTC)
Analogues like the KH 1060
I see that the Vitamin D analogues redirect to here. But recent developpements of analogues like the KH 1060 are considerable enought to brake the redirect, at least an article for those analogues now used as potent inhibitors of proliferation in studies. Fad (ix) 00:17, 11 July 2006 (UTC)
References Deleted:
I deleted the reference section. Please put the references back. —Preceding unsigned comment added by 24.10.221.159 (talk • contribs) 22:56, 1 August 2006
Evolution of human skin color
"Melanin screens UV rays oflight so dark skin is much less efficient at generating vitamin D. It would therefore be expected that people with darker skin originally with lighter skin would suffer from deficiencies more frequently, especially if they live at higher latitudes or have an urban lifestyle, and there is much evidence that this is the case. Vitamin D deficiency and osteomalacia are known to be endemic in dark-skinned populations in the UK (particularly those from South Asia)."
Isn't this the very selective pressure that favored fair skin in Europeans and Asians? If so, this should be mentioned (with appropriate source). — Philwelch t 07:57, 23 July 2006 (UTC)
The article suggests that it's near impossible to get proper vitamin D in winter at high latitudes. If this is the case, I wonder why Inuit peoples aren't very pale when considering they historically have lived near the Arctic Circle. Peoplesunionpro 17:41, 15 September 2006 (UTC)
- They would get a lot of vitamin D from their diet. The kinds of foods they eat has plenty.WolfKeeper 17:50, 15 September 2006 (UTC)
Other area's of action
I have a small problem with the 'classical' nature of this article. I appreciate the acuracy of most of the info relating to synthesis, calcium homeostasis etc. However, apart from a few mentions, the actions of vitamin D in the brain are largely ignored. In terms of synthesis, 1,25 vitamin D3 (the active form) can be synthesised in the brain and converted to 1,24 vit D3. The steroid argument is neither a yes or no. Vitamin D3 can be considered a 'neuroactive steroid' due to local synthesis in addition to rapid non-genomic effects. The fact that the vitamin D receptor (VDR) belongs to the steroid superfamily of receptors also supports this idea.
In regards to other comments already added. Vit A and D have complex interactions due to the VDR creating heterodimers with the RXR (vit A receptor), this isn't my area of expertise however. Vitamin D overdoses extremelely rare as mentioned and warrant a lot less discussion than that of the actual healthy level of vitamin D. The statement 'levels should be between 40 and 60 ng/mL (100 to 150 nMol/L) for optimal health' is incorrect or innacurate atleast, you find me a paper suggesting this is the level for OPTIMAL health and I will find you a paper that says a different level. As far as I am aware, we aren't sure what a healthy level is, different countries have different levels of fortification built around different guidelines. The lack of understanding regarding vitamin D's effects outside of calcium/phosphorous homeostasis is too limited to accurately quantify a healthy dose, this should be mentioned also.
Lastly, there should be more focus also on the anti-cancer research being done with vitamin D and the epilogues be created for this purpose. To me this article appears to be a well documented view of vitamin D 10 years ago and needs critical updates according to new research which should also be reflected as a larger sum of the total article. I would add to it myself but I am a beginner at wiki-ing...
please feel free to add any comments regarding disagreement with the above, I am not scared of critism and I love a good debate :) I have purposely left cites out for two reasons, 1. I am lazy 2. cites are only needed in the article or when an alterate opinion has been presented, when this is done I will add cites :) —Preceding unsigned comment added by Malarac (talk • contribs) 20:45, 24 September 2006(UTC)
Snow?
Article says: "For example, in the United States, those living north of a line from San Francisco to Philadelphia (about 40 degrees of latitude) will not be able to produce it in significant quantities for 3 to 6 months a year." What about those that often live around snow cover during winter? Snow reflects a high percentage of UV. Peoplesunionpro 19:10, 30 October 2006 (UTC)
Problem? (this should be on the talk page)
I was about to fix a syntax error when I came across this. This should not be in the article space, it appears to be some sort of argument:
I have moved the "problematic" parts of the section What is it: vitamin, steroid or secosteroid? here.
(The following paragraph is extremely contentious. It cites people who have never published in the field of vitamin D nutrition, and it confuses vitamin D with the hormone made from it. The paragraph is interesting because it is an example of why it is so difficult to provide the public with vitamin D in doses high enough to actually make much of a difference to the health of adults. While the author may have been well intended, the result here is a superficial confusion that only pretends to be well cited science):
In May 2006, Professor Ronald M. Evans, a Fellow of the Salk Institute, delivered a continuing medical education seminar to FDA's Center for Drug Evaluation and Research. In response to a question of what the impact on public health policy should be, given that "vitamin D" is actually a secosteroid, rather than a vitamin, he indicated that he would not supplement with "vitamin D" in the food chain.[2] This position is also supported by new evidence that vitamin D supplementation is harmful in many chronic autoimmune diseases (see section on "In Chronic Disease" below), and not just those previously identified (sarcoidosis, granulomatous malignancy such as lymphoma, oat-cell lung cancer, or when cancer has spread to the bone).[3]
Thus, based on its activity, vitamin D is most accurately viewed as a secosteroid with a high degree of steroidal activity. This indicates the need for further investigation of whether vitamin D supplementation is generally beneficial.--DO11.10 23:12, 2 November 2006 (UTC)
- Oh dear I've found more:
- An equilibrium is achieved in the skin whereby longer exposure to UVB simply degrades the product as fast as it is generated. Animal species evolved through natural selection to survive optimally in sunshine. Excessive synthesis of vitamin D from prolonged sun exposure is highly unlikely. In the 1960's it was thought that darkly pigmented skin existed to protect against vitamin D toxicity; however, dark skin is the default skin color of humans, it prevents breakdown of micronutrients in dermal capillaries. White skin was favored by natural selection because the mis-shapen pelvis of young women with rickets would have resulted in death because of a constricted birth canal.
- Strictly speaking, vitamin D is indeed a true vitamin. In fact, the first vitamine, "antirachitic A" was determined based on the bioactivity of vitamin D. That is, the thing that cure rickets was the thing that led to what we regard as a vitamin. How ironic that some now think that vitamin D is not a "true vitamin", because it can be manufactured by the body. This semantic debate reflects a misinterperetation discussed elsewhere in this encyclopedia, under "vitamin".
- These MUST be referenced by a reliable source.
- Update: I am reverting edits by User-multi error: "207.188.64.6" is not a valid project or language code (help). this page back to the version by User-multi error: "24.44.168.110" is not a valid project or language code (help).. These kinds of additions to articles are not acceptable, and arguments should be initatied on the talk page.--DO11.10 23:33, 2 November 2006 (UTC)
Response to the paragraph above. I am an active scientist specializing in the vitamin D for over 3 decades. I do write vitamin D articles in REAL encyclopedias. I am at the point where I am giving up on trying to help out Wikipedia. The concept for the encyclopedia is nice, but where do you separate real science from superficial misinterperetation?
The writer of the preceding paragraph is trying to function like a good editor. But how unfortunate that the writer needs to revert to a "reliable source", and insist on "discussing" these things on this page instead. I WAS the person who initiated this kind of discussion (I wrote item 4 above), but after many months, there is zero evidence anybody notices. I tried to fix up the text of the vitamin D article, but evidently need to add literature citations? I don't have the time to figure out how to do that. Encyclopedia entries usually don't include more than a couple of key citations. The list of citations to the Wikipedia vit D article was so long and often useless, that I saw little point to adding anything more of them (you could reference back to Wikipedia's own definition of "vitamin" where I did provide references, Stedman's Medical Dictionary for one, but who takes that seriously?).
In a democracy like Wikipedia, the garbage piles up, and the vitamin D article is showing more nonsense information than it should. The article is repetive and contradictory, because the article has become too long. A contributor really has to assimilate a ton of information before it is possible to add anything new or useful to it.
I for one have no time to fix up this article if my efforts have to be second-guessed. Sorry, I know the previous writer was being a well-meaning editor, but the process of writing this kind of encyclopedia is just not working out here. This article is getting out of hand.—Preceding unsigned comment added by 207.188.64.6 (talk • contribs)
- First of all, please let me be the among the first to welcome you to Wikipedia. It was never my intention to make you feel unwelcome. I hope that you take the time to review the changes I have made to the Vitamin D article. I went back over your additions, and found that you had made several needed and useful contributions. The problem was the addition of some argumentative language that you included with those useful contributions. I have added many of your contributions back, save these argumentative pieces (and a section that I could not easily verify). As I mentioned above I edited the page with the intention of fixing a syntax error that occurred right below one of your edits, which is why I noticed it and removed it. The rest of your edits, in my mind, were then tinged with an air of suspicion. I hope that you reconsider your comments above, I for one would value contributions such as the useful ones you added. (But please no arguments on the article page.)
- After reading, (and rereading this article a number of times) I agree with you that it has some major and distinct problem that are not easily fixed. While I do not know what your specific issues were some things that I noticed were 1) The steroid/vitamin debate is, in addition to being wrong, a moot point [regarding whether or not people should take supplements]. Also, I believe that the statements made by Ronald Evans were either misrepresented or taken out of context, as his published record does not indicate his expertise on the subject of vitamin supplements. 2) A heavy reliance on articles written by one author, and members of the same group. 3) Articles by other authors appear to be added as "puffers" in order to make a connection, that has not been proven, appear more scientific. 4) Overall repetition and contradiction that makes the article confusing, I have attempted to fix some of this. It was only with great trepidation (or trepination:))that I did not delete several sections of this article, I can only hope that other editors, such as yourself, see fit to adopt the article, and make it into what it should be.--DO11.10 23:41, 4 November 2006 (UTC)
Objectivity?
I do not believe that the section on vitamin D and chronic illnesses is objective. Virtually all of the findings are from Dr. Trevor Marshall, and while the section talks of 'increasing recognition' of his findings, the truth is that he has been unable to get them published in any medical journal and is frustrated because they have not been met with recognition, but scorn. I am not an expert, and Marshall could be right -- but his views are far from mainstream or accepted, and should not be presented as such. --Garsecg
- The comments of the user above piqued my interest so I set out to see if what he/she asserted was correct. In fact I find that according to the following article there is little current research that suggests that any of these diseases are caused by CWDB
- Cell Wall-deficient Bacteria as a Cause of Infections: a Review of the Clinical Significance J Int Med Res 2005;33(1):1-20.
- "While there is no direct evidence that their presence results in disease, laboratory data suggest that CWDB (Cell Wall-deficient Bacteria or L-form bacteria) are intracellular organisms that can revert to wild-type bacteria (WTB) outside the cell. CWDB are suggested to up-regulate to a more aggressive pathological form when an adverse environment threatens their survival inside cells, and they may in that theoretical situation cause symptoms of disease. Difficulties in proving this theory limit the acceptance of CWDB as disease-causing organisms. CWDB do not fulfil the first and third postulates of Koch, and many microbiologists do not believe they cause any harm to the host."
- About the specific studies cited in THIS article; "There was no uniformity in the methods described in these studies and most of the studies that have been conducted in the setting of rheumatology and osteomyelitis are at least 20 years old. We have not found any RCTs (randomized clinical trials) in this setting that have attempted to link CWDB to clinical outcomes, so the conclusions from the case reports discussed above should be interpreted with caution."
- Finally the authors conclude that: "The techniques used to identify CWDB are not uniform and many are questionable. In addition the evidence used to argue for their clinical significance is mainly based on case reports or small prospective series. For these reasons many are skeptical about the clinical significance of CWBD and recent clinical trials have also questioned the relevance of these atypical organisms to disease."
- Therefore, all statements and references to CWDB and L-form bacteria will be removed since any relevance in this article is directly related to their ability to cause disease. I will check out several other parts of this article, if anyone has any thoughts...--DO11.10 03:50, 23 November 2006 (UTC)
- The following comment was left on my talk page:
- to DOI11:10 re: Your rejection of our peer-reviewed publications on Vitamin D and Disease
- Dear Sir/madam,
- I notice that you are deprecating the learned work of myself and my professional colleagues. I sign my name to my work, but I have looked in vain for a name or a telephone number that I could call to contact you. I was taught that science is based on collaboration, not on suppressing the work of others. I would welcome a chat so that we can reconcile the misunderstandings which seem to have arisen.
- Sincerely
- Professor Trevor G Marshall, PhD, Director, Autoimmunity Research Foundation
- Trevmar 04:01, 28 November 2006 (UTC)
In response: I am not sure how you can conclude that I am "deprecating the learned work of you and your professional colleagues". I presented information from the paper I cited in which the researchers concluded that CWDB are not responsible for the clinical manifestations of disease. I then removed the statements about CWDB and disease for the reasons I stated above. That, in my opinion, is "science", not "suppressing the works of others". Addressing my edits, I do not feel that they were heavy handed. In addition to removing the CWDB statements (in all about five sentences) I moved a bunch of material to improve the article flow, deleted some material that was repeated in the article, adjusted the references so that they were uniform, deleted several references that did not seem to be applicable or were only marginally useful (free abstract only with no real relevance on the abstract page), and added full text links to several references. Most of these edits had very little to do with your work. Also, I notice that while you accuse me of the above, you did not contact Garsecg, I wonder why that is?--DO11.10 17:54, 28 November 2006 (UTC)
Dear DOI11:10,
- Guys, there is life beyond the Internet - only a very small fraction of medical knowledge resides on the Internet - text books, conferences, and direct collaborations overwhelm the subset of knowledge to be found online.
I made a civil suggestion to you, a REAL WORLD suggestion, in relative private, that you phone me so that we could talk through your misunderstandings. I am saddened to see the manner in which you have responded.
As for contacting 'Garsecg,' I clicked on the link for his name and got nothing. No identification, no email address. So what am I expected to do? Is there some way for me to contact this Garsecg??
- Sincerely, Professor Trevor G Marshall, Director, Autoimmunity Research Foundation.
Trevmar 10:50, 29 November 2006 (UTC)
- Considering that the conversation that you propose to DO11.10 is directly related to this page I think that it is completely appropriate that they would then post it here for discussion. And while you are suggesting a "real word" solution not everyone feels the need to talk to people in the real world to solve a problem that is occuring online. I know I wouldn't be willing to pick up the phone and call anyone from Wikipedia to resolve anything.
- I don't feel that DO10.11's edits were done to "suppress" your work and (keeping in mind I knew nothing about the subject until viewing the page) the edits they made seem even and not directed at causing someone distress but at actually improving the article. Nigelthefish 20:35, 29 November 2006 (UTC)
- Your insistance that I contact you "in private" deeply concerns me, and I will not contact you "in private" to further discuss my edits, as it would deprive other readers of reading for themselves what you have to say regarding this matter.--DO11.10 18:21, 30 November 2006 (UTC)
Vitamin D in Chronic Illness
In the previous section Garsecg writes, "I do not believe that the section on vitamin D and chronic illnesses is objective. Virtually all of the findings are from Dr. Trevor Marshall." On November 23, 2006, DO11.10 cut the section "Vitamin D in Chronic Illness", perhaps for similar reasons.
- I did not delete the entire section--DO11.10.
The question of the section's objectivity is worth discussion.Sure, the section may have been ripe for the inclusion of a contrary viewpoint. What I'm going to take issue with here is DO11.10's choice to completely excise the entire section. That was wrong.
There is increasing recognition that Th1 immune inflammation, occurring in rheumatic diseases can result in excessive numbers of activated macrophages converting 25-hydroxyvitamin D (25D) to its active 1,25 dihydroxyvitamin D (1,25D) hormonal form.[9][8][13][14]
- (8??, 9 is a paper written by Dr. Marshall, 13 is from 1991, increasing evidence?, 14 is about Crohn's disease and says the 1,25D comes from intestine I don't see any mention of macrophages)
This can lead to vitamin D dysregulation/hypersensitivity, which can lead to hypervitaminosis D, hypercalcemia and other symptoms. This is recognized as occurring in sarcoidosis and other diseases.[21]
Serum vitamin D, measured by the precursor, 25D, may appear to be deficient in chronic diseases in which vitamin D dysregulation occurs, because it is being depleted due to excessive conversion into the active 1,25D form by macrophages.[21] (This happens in the kidney not by "active" macrophages [3]) In this situation, supplementation with vitamin D may lead to an even greater elevation of an already elevated level of the 1,25D hormone.[9][8]
- (The medical community offers an opposing hypothesis that Vitamin D (as a Vitamin D Receptor, VDR ligand) induces Dendritic cells to acquire tolerogenic properties that favor the induction of regulatory T cells rather than effector T cells[4]. In light of this raising the level of VDR ligand by increasing Vitamin D would treat several chronic/autoimmune diseases who's primary etiologies involve effector T-cell mediated inflammation.)
Marshall showed that elevated levels of 1,25D are able to cause dysfunction of alpha 2 thyroid receptors and glucocorticoid receptors, thus interfering with endocrine function and the adaptive immune response.[5] (There is that name again.)
Research on vitamin D[8][10] has also focused on its role in combating viruses and bacteria. Tiny L-form bacteria, named after the Lister Institute where they were first described by Kleinberger-Nobel in 1934.[22] L-form bacteria lack a cell wall and can hide inside cells, including immune cells, like macrophages. There is increasing evidence of L-form bacteria in diseases like systemic lupus erythematosus,[23][24] rheumatoid arthritis,[25][26][27] Crohn's disease,[28] sarcoidosis[9][10][29][30][31] and multiple sclerosis.[8][32]
- (My citation above, and at least a half dozen more papers, show that L-form bacteria do not cause these diseases. Also this "increasing evidence" is taken from papers published in the following years: 1984, 1982, 1989, 1996, 2002, 1982, 2000, (and another of Dr. Marshall's papers), that doesn't sound like "increasing evidence" to me.)
Molecular modeling research[33] indicates that when 25D is high enough, it actually displaces 1,25D bound to the vitamin D receptor (VDR). This interaction may block innate immunity and bacterial killing, suppressing a reaction associated with bacterial killing, called the Jarisch-Herxheimer Reaction.
- (The Herxheimer Reaction refers to the release of endotoxin when large numbers of organisms are killed by antibiotics in syphilitic tissues; believed to be due to a rapid release of syphilis antigen and is associated with allergic reaction in the patient, the association here baffles me?)
This anti inflammatory effect may explain why vitamin D gives appears to be helpful in the short term. However, if L-form bacteria are proven to be the underlying cause of these diseases, this suppression of the inflammatory innate immune response may allow bacteria to increase, causing disease.[33][8][10] (How can you reference a hypothesis, it is a question???) The immunosuppressive effect of vitamin D is similar to the effect of steroid hormones, which is not surprising, as it binds to steroid receptors(as discussed above).
- (Again, my citation above, and at least a half dozen more papers, show that L-form bacteria do not cause these diseases.)
The success of a new antibacterial protocol[34]
- (This link is to Dr. Marshall's foundation and this protocol is called The Marshall Protocol)
that includes lowering of vitamin D levels, supports the importance of vitamin D dysregulation in many chronic diseases.[8][10][9] (Dr. Marshall's papers) The role of vitamin D and the vitamin D receptor (VDR) is also shown by the effectiveness of olmesartan, an angiotensin receptor blocker, as part of this new protocol.
- (That's Odd both the wikipedia article and the Physicians Desk Reference say that this medication is prescribed for high blood pressure, neither make any mention of the vitamin D receptor (the VDR))
Olmesartan acts through binding to the VDR, among other effects.[9][33] (Again, Dr. Marshall's papers, this is starting to seem a bit biased)
This new research on vitamin D's effects and the role of vitamin D dysregulation may require reinterpretation of much past research supporting vitamin D supplementation in the prevention and treatment of many chronic diseases.[8][10] (Again, referencing and idea not a fact)
- So it was for those specific reasons that I deleted the PARTS of this section that I did, the rest was moved into the overdose section. Okay back to your post---DO11.10 23:32, 29 November 2006 (UTC)
The preponderance of current research has it that: 1. Vitamin D is indisputably immunomodulatory, and 2. Vitamin D has a significant and increasingly documented role in chronic illness.
- I agree with point one and point two.
Dr. Marshall does have a body of peer-reviewed research on Vitamin D in chronic illness, and so do a substantial number of other researchers, a number of whom were also mentioned-- Rasjaree, Mawer, Abreu, etc. In any case, there is certainly enough published research here to merit inclusion in a Wikipedia article.
- Rasjaree, Mawer, Abreu, they're still there.
If I may offer my most objective take on this issue, the debate is not whether there is any such connection between Vitamin D and the immune system. Rather, it is whether chronic immunological-type diseases are in fact autoimmune or not. (You may think I'm straying, but I'm not.)
- Since this article is about vitamin D, the relevance to vitamin D seems crucial to any debate.
There are a number of researchers, some of whom think chronic illness is caused by an overactive Vitamin D receptor; others assert (in peer-reviewed research and in significant numbers) that chronic illness is caused by an underactive VDR. Knowing what we know now, no article about Vitamin D or the immune system can ever be complete without some sort of substantial discussion of the other.
- But you don't present ANY of this "peer-reviewed research and in significant numbers" that opposes your viewpoint. That violates Wikipedia policy WP:NPOV.
I try to make a habit of not questioning the integrity of another Wikipedian, so I'll just say once more that DO11.10 made a mistake when s/he cut the whole section, "Vitamin D in Chronic Illness." What s/he should have done was try to assiduously incorporate into the article what I would call here the alternative hypothesis. The thinking to which Dr. Marshall subscribes is sufficiently adopted among large segments of the medical research community and asserted in published research that to completely leave it out would be a disservice to readers of Wikipedia. Palbert 01:08, 29 November 2006 (UTC)
- Alternative hypothesis?? I notice that you didn't include any alternative hypotheses in this section when your wrote it, although the papers were out there. Further the article aboutCell Wall-deficient Bacteria and disease is not "alternative", it flatly refutes the connection you attempt to make. And if "The thinking to which Dr. Marshall subscribes is sufficiently adopted among large segments of the medical research community" where are those references?
- As for your insinuation regarding my integrity I think that my User contributions address my integrity quite clearly.
- As an aside a simple Google search turns up a Paul Albert who appears to be a friend/patient of Dr. Marshall's Paul Albert Posted: Mon Apr 17th, 2006 08:30, seems that might be the same person as Palbert (talk · contribs · logs), which sounds to me like a Conflict of Interest.--DO11.10 23:32, 29 November 2006 (UTC)
"not everyone feels the need to talk to people in the real world"
This thought from 'Nigelthefish' (above) says it all. Yet you are collaborating in creating a work-product, Wikipedia.org, which is being read by real people, many of whom are sick and looking for answers. Real people are being influenced by what they read here.
I would remind you that I am at least the second expert who has registered their disgust with the way this science is being edited. Like my colleague from Canada (207.188.64.6, above), I am appalled by the misplaced energy I see being displayed here.
Sincerely, Professor Trevor G Marshall, PhD, Director, Autoimmunity Research Foundation.
Trevmar 16:11, 30 November 2006 (UTC)
- You are right, this article is being read by people who are looking for answers and being influenced by what they read here, that is the reason why the people who read this article should be exposed to accurate, complete and unbiased information. It is this reasoning that promted me to remove, from this article, the grossly misinformed and inaccurate information from the sections that I did, as I outline above.
- The case involving IP user 207.188.64.6, is vastly different from this one, to compare the two situations would be, to use a cliche, like comparing apples to flying cars.
- In summary, I stand by my current edits, and will continue to make improvements to this article in the future.--DO11.10 18:39, 30 November 2006 (UTC)
Before working on a project
It is a good idea to learn how it works. WP is not short of essays on how it works. Midgley 15:09, 3 December 2006 (UTC)
- That is certainly good advice. But to whom/what are your comments directed? If you feel that I have done something wrong, please tell me or I am likely to do it again.--DO11.10 21:35, 3 December 2006 (UTC)
Vitamin D3 created 'in' or 'on' the skin
in her 1954 book, Adelle Davis wrote, "Most medical textbooks say that vitamin D is formed by sunlight on the oils IN the skin although it was proved 16 years ago[A.C. Helmer and C.H. Jansen] that the oils must first be ON the skin, then exposed to ultraviolet light, and later absorbed back into the body. If persons take a bath before going into the sunshine, the oils are washed off, and no vitamin D is formed; if they do not bathe before exposure to sunshine but bathe immediately afterward, the oils are removed before the vitamin can be absorbed into the body." what is the latest information?Sanfranciscojim 21:57, 18 January 2007 (UTC)
- I came to this article looking for an answer to the question of "where specifically is Vitamin D produced?" and was unable to find that information. Is it produced by cells of the epidermis, the dermis, or both? What is the role of oils, as brought up in the above comment? Provophys 18:28, 19 January 2007 (UTC)
Answers
Vitamin D is produced photochemically IN the skin from 7-dehydrocholesterol (not an "oil").
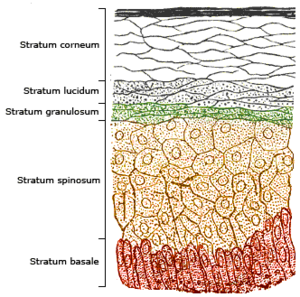
First off some background about the skin: It consists of two primary layers: the inner dermis, composed largely of connective tissue, and the outer thinner epidermis (see image). The thickness of the epidermis is <25 um and it contains five strata; from outer to inner they are the stratum corneum, (sometimes the lucidum), granulosum, spinosum, and basale.
"The highest concentrations of 7-dehydrocholesterol are found in the stratum basale and stratum spinosum. Accordingly, these two layers have the greatest capability for production of previtamin D3 and vitamin D3, whereas the other layers have a lesser capability."
Bathing removes dead skin cells from the stratum corneum, you can't "wash off" the deeper spinosum, and basale layers of the skin.
On another note "UVB affects the epidermis, and the two principal determinants [of generating Vitamin D] are the quantity (intensity) and quality (appropriate wavelength) of the UVB irradiation reaching the 7-dehydrocholesterol deep in the stratum basale and stratum spinosum."
- I will add this information to the article. And to answer the question below, you don't need sunlight to convert D2 (or D3) that you have ingested into active hormone, you just need sunlight to MAKE pre-vitamin D3 from 7-dehydrocholesterol, which is converted to active hormone, only when the vitamin is required, in the kidney.
- The following article is quoted and referenced here and provides more details: Sunlight, season, skin pigmentation, vitamin D, and 25-hydroxyvitamin D:integral components of the vitamin D endocrine system Anthony W Norman 1998. (Also, stop reading medical texts from 1954 :))
Hope this helps---DO11.10 19:41, 19 January 2007 (UTC)
Vitamin D2 vs D3
does one still need to have UV exposure when taking D2 for the correct metabolic process to proceed?Sanfranciscojim 22:06, 18 January 2007 (UTC) —The preceding unsigned comment was added by Sanfranciscojim (talk • contribs) 22:05, 18 January 2007 (UTC).
Ligand
I added a wikilink to the ligand term in the Role in immunomodulation section, but I'm not absolutely positive that it's the correct term. Could someone knoweldgable about the subject make sure it is correct please? Thanks.WLU 18:25, 23 January 2007 (UTC)
- That is the right term- thanks!--DO11.10 21:16, 23 January 2007 (UTC)
Possible typo in Overdose
Hi,
This is my first time ever posting to wikipidia so I'm not sure how this works. I hope I've come to the correct place.
In the Overdose section the third sentence reads:
Although normal food and pill vitamin D concentration levels are too low to be toxic, because of the high vitamin A content in cod-liver oil it is possible to reach poisonous levels, if taken in multiples of the normal dose.
I am confused by the mention of vitamin A. Either the mention of vitamin A is a typo or (more likely – given my lack of medical knowledge) somehow vitamin A increases the toxicity of vitamin D. If the latter case it true, perhaps, one of the contributors could put in a sentence or two about how high levels of vitamin A can cause one "to reach poisonous levels" of vitamin D.
Thanks (and if I'm in the wrong place please let me know) -Kevin —The preceding unsigned comment was added by 208.237.178.229 (talk) 16:10, 31 January 2007 (UTC).
- This is the right place. Yes that was a typo, I think that sentence was directly copied from the vitamin A article or something. I have changed it to vitamin "D". Good catch.--DO11.10 18:50, 31 January 2007 (UTC)
My understanding of this is that the original is correct because it is referring to the toxicity of excessive Vitamin A. For absolute clarity the passage should read, I believe, something along the lines of:
"Although normal food and pill vitamin D concentration levels are too low to be toxic, because of the high vitamin A content in cod-liver oil it is possible to reach poisonous levels of vitamin A, if taken in multiples of the normal dose in an attempt to increase the intake of vitamin D." This should not be difficult to verify...
FrancesB 88.105.136.210 20:50, 1 March 2007 (UTC)
Citation tag explained
The following addition is dubious.
The toxicity limit on Vitamin D is often questioned. Reinhold Vieth, a published vitamin D researcher, recommends 4000IU per day as an ideal amount for good health and points out that only levels above 95μg/day (3800 IU/day) may cause hypercalcemia.[4] Also, no normal human being (i.e not suffering from vitamin D hypersensitivy or other ilnesses) has ever contracted Vitamin D toxicity, despite the fact that a fair-skinned person who exposes themselves to the sun for 20 minutes can produce up to 20,000 IU per day.
- The first citation is quite poor, there must be a peer reviewed source out there.
- "Normal human being" is inappropriate, and pejorative.
- The second sentence will require citation for the amount produced. But, really, so what? People don't get vitamin D toxicity from the sun, toxicity comes from supplements or industrial accidents this was already stated above in the same passage.--DO11.10 18:22, 12 February 2007 (UTC)
Stifling Concept Improvement
You, User DO11.10 remind me of the people during the thousands of years of dispute over heliocentrism (look it up) that continually battled against the idea that the Earth was not indeed the center of the universe. You stifle any such improvements over the medical concept of "vitamin" D. Your cardinal rules of which you interpreted the wikipedia guidelines are ridiculously totalitarian. Those who are in the know, not you, don't come here to make immprovements because their ideas don't conform to your rules. It's quite a shame. You have much talent editing wikipedia, however that talent seems to repress ideas and concepts which don't fit your rule book. Wikipedia policeman, I wish only truth to prevail. I hope one day you realize your faults. Cuda918 20:12, 24 February 2007 (UTC)
- [Addendum: I have no idea which contributions you have made that I have then removed, as far as I can tell Cuda918 (talk · contribs · logs) has made only 1 edit prior to this one. Also in the past month or so the only content addition that was made to the article was the "toxicity" information above. You will have to be more specific.] I would certainly welcome additions to improve this article provided that they conform to Wikipedia's policies, such as additions that are:
- Neutral in their point of view and do not give undue weight to a significant-minority view,
- are not original research,
- are verifiabile and are accompanied by Reliable sources as outlined in the Scientific citation guidelines.
- If you find the above guidelines "ridiculously totalitarian" then I think you will find that many dedicated editors of Wikipedia will consistently stifle your improvements. My motivation for editing this article, and all of the other articles I have ever contributed to, is a genuine interest in maintaining the quality of the article and preserving accuracy and I apologize if you take offense to my (own personal) "cardinal rules".
- In closing, from the Wikipedia policy that users should avoid personal remarks: Wikipedia prospers on people working together toward improving articles. Anything else – especially attacks directed specifically at users – detracts from the wonderful thing that we are creating here.--DO11.10 05:31, 25 February 2007 (UTC)
- It isn't the guidelines, but your interpretation of them. As far as personal remarks are concerned you should try heeding your own warnings. I figured you used this public space as your own personal page/instant messenger anyway. Perhaps it isn't the "dedicated editors" that are the primary mode of stifling concept improvement but the media which is being used. I appreciate this insight you have given me and the talent to which you are on top of things. Cuda918 17:25, 26 February 2007 (UTC)
Excellent Vitamin D Webcasts available I present this here, because my own efforts to modify the regular vitamin D page have generally been deleted. My format for adding to the article does not match up to the criteria of user D011.10, who seems to function as the policeman of this part of Wikipedia. If there is someone suitably qualified to add these to the encyclopedia entry, the following would likely be of interest to some readers.There are now many professional-level webcasts available ensuing from a December 2006 meeting in Washington DC. http://app2.capitalreach.com/esp1204/servlet/tc?cn=asbmr&c=10169&s=20343&e=6950&& Alternatively, there is another more lay-person oriented webcast about vitamin D available at the following: http://www.direct-ms.org/presentations.html
p.s. the use in the article of the term "Vigantol" specifies a brand name. Something that should be a no-no. —Preceding unsigned comment added by 207.188.64.235 (talk • contribs)
- The first of the above links could potentially be included in the external links of the article, depending on their content. I've never heard of the American Society for Bone and Mineral Research, and it looks like it's funded by Eli Lilly, but it might be good if the podcasts have basic info and aren't just pushing vitamin/mineral supplements. I'd say the second one is out - anything with direct in the weblink has to be spam :) WLU 12:30, 26 February 2007 (UTC)
Re: Excellent Vitamin D Webcasts Available: I'm currently researching the effects of UVB light on vitamin D3 synthesis and I have just visited both these web casts. The first is a very interesting (but highly technical) series of research presentations made at a symposium entitled: Contemporary Diagnosis and Treatment of Vitamin D-Related Disorders, December 2006. Not "basic info" but very well presented info. Quite a few of the participants are names I have seen on papers in peer-reviewed journals. It's certainly not "pushing vitamin/mineral supplements", far from it.
The second one is certainly not spam. It is a webcast of a lecture aimed at a "lay" audience by a Dr. Reinhold Vieth (again someone whose name is familiar) and it is made available through the website of what is apparently a small Canadian charity called DIRECT-MS, short for DIet REsearch into the Cause and Treatment of Multiple Sclerosis. I know nothing of this, but it looks completely genuine. The webcast can be accessed directly, bypassing the multiple sclerosis link, at: http://www.insinc.com/onlinetv/directms13oct2005 I would recommend this to anyone as an introduction to some of the more recent ideas emerging from some D3 studies, although some of these findings are still very controversial and I am sure this presentation will not be everyone's favourite, in particular those people "pushing vitamin/mineral supplements" !
FrancesB 88.105.136.210 21:15, 1 March 2007 (UTC)
Hemp seed
Hemp seed appears to have a lot of Vitamin D. This should probably be added along with shiitake mushrooms as a vegan source. But is it D2 or D3? Badagnani 19:22, 14 March 2007 (UTC)
Note
Note: Parathyroid hormone stimulates the activation of vitD so that osteocytes become activates and Ca concentration is increased. —Preceding unsigned comment added by 134.36.123.158 (talk) 17:18, 28 April 2008 (UTC)
--There are some inconsistencies in the micrograms=I.U. figures---
I seem to recall that 2.5. MGs equals 50,000 IUs. In the middle of the article, different figures do not equate, such as a 5X microgram increase equals a 10X IU increase. The exact figures should be verified and correced. —Preceding unsigned comment added by 71.163.209.112 (talk) 07:49, 18 May 2008 (UTC)
For some, diet may not be enough for Vitamin D
Legacy recommendations call for people from age 50 to 69 to get 400 international units (IUs) of vitamin D per day and for those over age 70 to get 600 IUs. Many researchers, however, suggest that 1000 to 4000 IUs may be needed. [5] Brian Pearson 04:52, 23 April 2007 (UTC)
Latitude factor
Following this sentence These wavelengths are present in sunlight at sea level when the sun is more than 45° above the horizon, or when the UV index is greater than 3. it might useful to add that the required solar elevation occurs daily within the tropics, daily during the spring and summer seasons at mid latitudes, and almost never within the arctic circles. The point to make apparent is that for many countries there is an annual cycle of boom and bust, which is a huge factor in the health issues associated with vit D.
Suggestion:
- At the latitude of Seattle, Montreal, Venice, and Christchurch NZ the sun rises to this elevation during spring and summer, but not during fall and winter, resulting in annual vitamin D cycles.
I picked well-known, longitudinally distant cities at 45 degree latitude; there are few such cities in the southern hemisphere apart from Christchurch. See List of cities by latitude.
- For the rest of the population, vitamin D levels tend to be lower, and crash in winter. In testing office workers in Toronto in winter, Dr. Vieth found the average was only about 40 nanomoles/L, or about one-quarter to one-third of what humans would have in the wild.
MaxEnt 14:30, 28 April 2007 (UTC)
60% cancer reduction
This is a shocking number, and hard to believe on face value. Twice the effect as compared to smoking. I did a little arithmetic on that.
http://www.bccancer.bc.ca/HPI/CancerStatistics/FF/AgeStan/Inc/default.htm
Cancer rates for women in BC run about 330/10,000 per year. 1200 women broken into two equal groups and followed for four years gives you 2400 women-years per group. At a rate of 330/10,000 with a 60% reduction in the non-control group gets you incidence rates of 7 and 2.8. How does one measure 2.8 cancers? Quite possibly, the actual numbers were 10 and 4. 14 total cancers in 4800 women-years is a rate of 291/100,000, which is quite realistic. If it breaks down 7 and 7, you have no result. Standard deviation sqrt(14) = 3.7. It looks to me like both sides of the study are within one standard deviation of a possible mean. I don't know off the cuff how to compute the null hypothesis properly, but it's certainly large enough to cast doubt. MaxEnt 16:24, 28 April 2007 (UTC)
- I thought about this some more. My calculation above assumed age-standardized rates. For a study of this size, it's extremely hard to achieve statistical significance with a mean rate this low. Almost certainly the population was biased toward older age groups to achieve a higher mean rate. Women over the age of 65 have a mean rate four times as high. http://www.bccancer.bc.ca/HPI/CancerStatistics/FF/Rates/incidence.htm If the mean rate for the age-skewed study group was 800/100,000, then 20 cancers are expected in the control group, and the 8 observed cancers in the experimental group (-60%) comes out 2.7 deviations below the mean. The study is much stronger if the experimental population was tilted toward advanced age. MaxEnt 17:47, 28 April 2007 (UTC)
- I would like to know if there has been less tanning recently than in years past when people seemed to believe tanned people were nicer looking and possibly more "healthful" looking. Brian Pearson 03:03, 6 May 2007 (UTC)
- I am confused. The article history shows that the results of this study were (first) added to the article by you. Are you disputing information that you - yourself - added?--DO11.10 00:28, 30 April 2007 (UTC)
- I don't think he is disputing it so much as he is wondering aloud how a reduction of that magnitude is possible. WatchAndObserve 14:56, 6 May 2007 (UTC)
How can a 60% reduction of cancer be possible? And what is the biologic mechanism that links vitamin D with cancer? A year ago I would have said there cannot be such a link because vitamin D affects calcium and bone cell metabolism which have no connection to most cancers. Or so I thought until I read an article in the November 11, 2006 issue of Science News by Janet Raloff, The Antibiotic Vitamin. The article says that vitamin D hormone 1,25-D is necessary for macrophages to produce antimicrobial peptides in the cathelicidin group to combat virus, fungus, and bacteria infections. The link with cancer is that macrophages also destroy damaged cells and cell fragments such as DNA. By the time a cell becomes malignant, its chromosomes and DNA are a chaotic mess. (See Scientific American, May 2007, pages 53-59.) Most chromosomes in cancer cells are mere fragments or completely missing, some are duplicated, and the DNA is rearranged and mutated. The genetic mechanisms that control growth and prevent unlimited growth, such apoptosis, telemere shortening, and intercellular communication are gone or inactivated. Hence, the macrophages, which kill malignant cells and destroy cell fragments, are the last defense against cancer. Since vitamin D is necessary for phagocytosis, vitamin D deficiency can allow malignant cells to multiply unchecked. Greensburger 17:37, 6 May 2007 (UTC)
- Cathelidicin also seems to be directly anti-carcinogenic though I don't know whether this is due to an anti-pathogenic effect, which i8t has, or some other cause. Though I'd be careful with some of these studies on Vit-D "deficiency". People with low 25-D are likely to be so because of either existing infection or liver or kidney problems, or overconversion to 1,25D. Most studies fail to account for these possibilities. --76.166.24.76 (talk) 03:20, 2 January 2009 (UTC)
At the very least the astonishing correlation in this study suggests that further research is justified. Staypuft9 16:06, 20 August 2007 (UTC)
New data is available: http://www.google.com/search?q=Vitamin+D+protects+cells+from+stress+that+can+lead+to+cancer&ie=utf-8&oe=utf-8 Artem-S-Tashkinov (talk) 18:27, 16 May 2008 (UTC)
Reference questioned
I am taking issue with the following statement:
One recent consensus concluded that for optimal prevention of osteoporotic fracture the blood calcidiol concentration should be higher than 30 ng/mL (US units), which is equal to 75 nmol/L (System International units).
The reference given is http://dietary-supplements.info.nih.gov/factsheets/vitamind.asp, but I don't see this information anywhere on the page. If nobody objects, I will be removing the reference from this statement and adding a 'citation needed' tag.WatchAndObserve 14:59, 29 April 2007 (UTC)
- I have changed the citation.--DO11.10 00:28, 30 April 2007 (UTC)
I have a doc that states it pretty clearly: [[6]] . Also, if you want you can watch worldwithoutcancer video on google videos, it's a pretty old movie that has had quite some controversy, but it also advocated (somesort of) D Vitamin. Cheers: Mr soros 02:16, 22 July 2007 (UTC)
Vitamin D; spelling of Mittelstaedt, Martin
Please note that the article entitled "Vitamin D" includes a citation by one Martin Mittlestadt. See citation no. 39. The name is incorrect. The correct form of his name is Martin Mittelstaedt. Cf. http://www.theglobeandmail.com/servlet/story/RTGAM.20070428.wxvitamin28/BNStory/specialScienceandHealth/home Boytinck 17:45, 1 July 2007 (UTC)
"A 2006 study published in the Journal of the American Medical Association, reported evidence of a link between Vitamin D deficiency and the onset of Multiple Sclerosis; the authors posit that this is due to the immune-response suppression properties of Vitamin D" the article cited doesn't mention this at all.
External Link Video Add
I'd like to add a video in which Dr. DeLuca from University of Wisconsin discusses the history of the discovery and applications of Vitamin D. The link is http://www.researchchannel.org/prog/displayevent.aspx?rID=3751&fID=345 (this does not automatically open the video). Please let me know what you think. (ResearchChannel 19:42, 17 July 2007 (UTC))
- While the content of this video is great, (from what I saw... the history part was fascinating) the streaming quality was –well– bad. I tried the video in both WMP and Quicktime. In WMP the video paused to buffer seven or eight time in the first minute, and didn't get any better when I skipped around. The Quicktime version was better, no buffering issues, but when I tried to skip I lost the sound(?). Given that the video is 1 hour 18 minutes long both issues will probably hinder it's usefulness here. Granted it could be my settings or something (probably not my connection speed though, I am running at over 2,000 kbps). If it is possible to address these issues, I think that the video is certainly relevant and I would like to add a link. --DO11.10 18:30, 20 July 2007 (UTC)
Vitamin D in milk
I cannot find this information on the milk page: it is my understanding that Vitamin D is fat-soluble. Does this mean that skim milk cannot be fortified with it? Staypuft9 16:07, 20 August 2007 (UTC)
- My skimmed milk claims it is fortified with D. --Michael C. Price talk 16:29, 15 November 2007 (UTC)
- I'm pretty sure most skim milk has at least some fat Nil Einne (talk) 12:22, 27 December 2007 (UTC)
- I read that whole milk contains about 3% fat and skim milk contains about 0.5% fat, but I don't recall where I read it. Greensburger (talk) 17:35, 27 December 2007 (UTC)
Mortality benefit
In a meta-analysis of 18 studies, vitamin D (mean dose 528 IU) reduced the mortality risk by 7%. Exact mechanisms remain unclear, and more trials are needed. URL JFW | T@lk 21:43, 10 September 2007 (UTC)
In the Time.com article that discusses this meta-analysis, there is this sentence: " 'Throughout human evolution when the vitamin D system was developing, the 'natural' level... was probably around 50 ng/mL or higher,' writes Dr. Edward Giovannucci. Only in human evolution? Don't other animals need vitamin D too? If so, how do they make it if their skin is covered with fur? Greensburger 23:53, 13 September 2007 (UTC)
Some of the light will still reach their skin even with fur; and in many cases not all of their skin is covered with fur. Besides, a fair number of animals (particularly furry ones) tend to be carnivorous, and they can extract it from their prey's liver.WolfKeeper 04:27, 14 September 2007 (UTC)
Apologies for not linking an article, but I read once that furred animals, like cats, lick D off their coats during cleaning after sun exposure. Essentially, they are often 'orally' taking vitamin D from their fur (or prey), as long as they go outside. This is why diabetes (related to D deficiency) is seen in cats that don't go out in the sun, and hunt. —Preceding unsigned comment added by Mo79 (talk • contribs) 11:11, 18 September 2007 (UTC)
Does vitamin D actually promote reabsorption of calcium in kidneys?
The article currently states, "Vitamin D regulates the calcium and phosphorus levels in the blood by promoting their absorption from food in the intestines, and by promoting re-absorption of calcium in the kidneys."
It is my understanding that parathyroid hormone (PTH) promotes the re-absorption of calcium in the kidneys. Is it is actually vitamin D that does this, or a combination of vitamin D and PTH? If vitamin D is involved, what is the process?
An answer to this question, with a reference to an online medical research or review article, would be appreciated?
Leeirons (talk) 16:42, 11 December 2007 (UTC)
- The reference given (The Merck Manual) states the vitamin D and it metabolites "Enhance Ca reabsorption by the [kidney] tubules". "The conversion to 1,25(OH)2D [active vitamin D hormone] is regulated by its own concentration, parathyroid hormone (PTH), and serum concentrations of Ca and phosphate."--DO11.10 (talk) 18:43, 11 December 2007 (UTC)
Obesity, hibernation in other mammals. Cross reference to tanning/tanorexia/tanning addiction
Hibernation
"hibernating bears wake up when given vitamin D" looking for confirmation or reliable source/citation for this. http://www.arthritistrust.org/Articles/Sunshine%20Deficiency%20Diseases/index.htm
hibernating bears also have elevated parathyroid hormone which protects against bone loss. http://jeb.biologists.org/cgi/content/abstract/209/9/1630
Morbidly obese humans have decreased vitamin D and elevated PTH. (before and after gastric bypass, so surgery did not cause it). Vitamin D suggested as an additional factor. http://www.springerlink.com/content/c3387p46381j6113/
Anecdotal evidence for euphoric states/elevated/sleep disturbance mood during the summer months at high latitudes.
Vitamin D depletion and correlation with activity/anxiety/nervousness as adaptive behavior - preparation for winter? (might explain some angry bears in the fall and spring!). Looking for citations
Tanning and UV exposure:
would be good to reference the 20,000 IU of vitamin produced by 20 minutes of natural UV exposure and whether tanning beds produce this same effect. The human body's vitamin D production is naturally limited to about 20,000 IU/day. After the precursor is used up, no more vitamin D is produced. www.vitamindcouncil.com
216.18.16.98 (talk) 20:21, 17 December 2007 (UTC)johnpaulmorrison@hotmail.com
are there safety studies/estimates for rotating a UVB light (around the body, locally-applying, in turns) ?
As not a specialist around this field, first, I thought "UV" good for vitaminD could include UVA (blacklight) -- as for tanning. I thought, rotating the body-portions exposed to light, would lessen the skin-age problems associated with (also) UVA.
That UVB is necessary (as this wikipedia article is informing), that heightens the risk of that in-house-D-light plan of mine. Truly? Or, may we keep that in check, such that with UVB lights, could people fortify their bones with light at home? (If sun is good, how is a handheld UVB-light not? Why not talking about that?)
The rotating of the exposure is again a tool to lessen the strain on the skin-spot, probably (unless the skin gets used to that in time). cf. How diabethic people rotate insuline-injections, not to inject at a single spot all the time. What guidelines for amounts of such locally-applying UVB -- in turns? That would fortify this vitD article, I think. --FerzenR (talk) 09:44, 8 January 2008 (UTC)
Spectral sensitivity and synthesis of previtamin D3
The text summarizing the action of UVB in respect to wavelength segment is far too ambiguous, carries a factual error, and is not representative of actual process involved. It has been understood from experimentation and the resultant literature since the 1980s that optimal synthesis of 7-DHC to preD3 occurs in a relatively narrow band, from 295-300nm, with maximum conversion at 297nm. This segment is often referred to as D-UV.
As such, I am making necessary corrections to the text, and including corroborating references.
Pragmatist (talk) 17:36, 7 February 2008 (UTC)
"Per glass"
"fortified milk typically provides 100 IU per glass" Is that a big glass or a small glass? perhaps we can create the Big Glass and the Small Glass as a units of measurement specifically for the US, so that we can talk about 2.735642367 Big Glasses of something. 80.2.199.213 (talk) 16:32, 8 March 2008 (UTC)
- Checking the source I see that they meant a one pint glass. --Michael C. Price talk 17:49, 8 March 2008 (UTC)
- Milk contains 100 U of vitamin D per 8 oz, (240 ml). It is of interest that soy milk contains D2 and cow mild D3, at 100 IU per 8 oz serving. With D2 having less activity, and D2 assaying similarly to D3 in the usual 25 OH-D assay there is much potential for blood assays to misidentify individuals on Soy milk as having adequate Vitamin D levels. I usually get a 25-OH D level by LC/MS/MS to fractionate the D2 and D3. Kd4ttc (talk) 03:48, 28 January 2009 (UTC)
Role in coronary disease prevention?
There is evidence that vitamin helps hearts, and other evidence that it may raise cholesterol and harm hearts.
The reason may be that there is a window of ideal vitamin D nourishment, and levels below the lower threshold cause coronary problems while levels above the higher threshold tend to raise cholesterol (and harm hearts).
It may be that the cancer-preventing benefits of vitamin D may be maximized, while the possible heart-harming effects are minimized, if one takes three times the chosen dose every third day, with no vitamin D supplementation on the two days in-between.
Perhaps the title to this section lacks nuance, and the section should be re-titled to reflect that the relationship between vitamin D intake and cardiac events may be a bit more complicated than a straight-line correlation between so that higher and higher supplement levels must always result in lower and lower rates of cardiac events. —Preceding unsigned comment added by 68.166.202.4 (talk) 01:51, 21 March 2008 (UTC)
---
The rising of cholesterol levels could simply be because you're achieving repletion by supplements and not skin cholesterol conversion by UVB. Remember there is still debate about the cholesterol theory, and 'high' cholesterol might simply be an indicator of vitamin D deficiency. i.e. it's not high cholesterol clogging your arteries but lack of a natural anti-inflammatory to control inflammation. —Preceding unsigned comment added by Mo79 (talk • contribs) 10:38, 18 May 2008 (UTC)
- Or it could be the opposite. High cholesterol leads to more hormone D3 (the more accurate term for vitamin D, since it's not really a vitamin but is produced in-vivo). Inflammation triggers toll-like receptors which upregulate CYP27B1. CYP27B1 converts 25D (which is usually what is measured to determine deficiency) into the active form 1,25D creating an apparent deficiency, however 1,25D3 would be abundant in such a state. Higher 1,25D3 leads to increased activation of the hormone D receptor in individuals with functional hormone D receptors leading to increased blood levels of calcium. Activation of the hormone D receptor also stimulates demineralization of bone (Calcium from bones goes into the blood stream.) In the absence of sufficient Vitamin K (either from a lack in the diet or from a number of drugs, particularly blood thinners, which inhibit Vitamin K metabolism), this leads to calcification of soft tissue rather than bone mineralization, arteriosclerosis and heart disease in the long term. This seems accurate to me and I could source any step in the chain. The sequence as a whole, however, may constitute original research. There's good evidence, for instance that statins, which prevent cholesterol synthesis, actually help with osteoporosis. [7] This is not what you'd expect if Vitamin D were the cure for osteoporosis. --Ryan Wise (talk) 05:55, 26 August 2008 (UTC)
Footnotes format in coronary disease prevention need fixing
Sorry -- added, but can't seem to format.68.166.202.4 (talk) 02:31, 21 March 2008 (UTC)In over my head
Add section about benefits of vitamin D and fending off and/or fighting influenza
There was a study published which I think successfully explains why the flu is a winter illness, and why vitamin D supplementation in the winter months may help fend off the flu. I've included a link to the paper's abstract below (google scholar):
http://journals.cambridge.org/action/displayAbstract?fromPage=online&aid=529704
It would be great to get information from this paper into the wiki article on Vitamin D, and maybe also on the influenza page.... —Preceding unsigned comment added by L8daRa (talk • contribs) 18:12, 17 April 2008 (UTC)
External links should start with the superb Vitamin D Fact Sheet from the U.S.National Institutes of Health
- Vitamin D Fact Sheet from the U.S.National Institutes of Health —Preceding unsigned comment added by 68.165.11.156 (talk) 04:03, 19 May 2008 (UTC)
Too much D, like too little, a risk factor for breast cancer
- page not found --Ryan Wise (talk) 13:17, 2 June 2008 (UTC)
Children can tolerate more Vitamin D, though optimum is debateable
"According to the researchers, due to rapid skeletal growth, children and adolescents are more likely to be vitamin D deficient, and are far less likely to reach vitamin D levels that doctors would consider toxic." [8] Brian Pearson (talk) 22:55, 27 June 2008 (UTC)
- "Warfarin-induced artery calcification is accelerated by growth and vitamin D."[9]--Ryan Wise (talk) 04:18, 26 August 2008 (UTC)
Is D3 supplementation helpful?
I think there's some cause to question whether Vitamin D supplementation is helpful.
There are some who say that low levels of 25 D are caused by infection which causes 25 D to be converted to 1, 25 D in unhealthy amounts due to disregulation of the vitamin D receptor. Testing for 25 D showed lower levels in unhealthy people, but I can't find any controlled study demonstrating that D3 supplementation alone increased bone density superior to either calcium supplementation + D3 or calcium alone.
Likewise, it's anti-cancer effects only appear in short term trials and are comparable with other immunosuppressives such as prednisone in this regard. Benefits disappear with long term use.
see http://bacteriality.com/2007/09/15/vitamind/ and http://trevormarshall.com/BioEssays-Feb08-Marshall-Preprint.pdf —Preceding unsigned comment added by 63.166.226.83 (talk) 18:38, 4 June 2008 (UTC)
Also;
The ratio of total 25OHD3 and 1,25(OH)2D3 to plasma DBP, rather than total circulating vitamin D metabolites, may provide a more useful index of biological activity. Further studies are required to substantiate this hypothesis. http://www.ncbi.nlm.nih.gov/pubmed/16339300?ordinalpos=33&itool=EntrezSystem2.PEntrez.Pubmed.Pubmed_ResultsPanel.Pubmed_RVDocSum
CONCLUSIONS: Kidney-transplant recipients receiving modern immunosuppressive regimens with low doses of corticosteroids experience only minimal loss of BMD during the first posttransplant year. Cholecalciferol supplementation did not prevent posttransplant bone loss http://www.ncbi.nlm.nih.gov/pubmed/15714177?ordinalpos=45&itool=EntrezSystem2.PEntrez.Pubmed.Pubmed_ResultsPanel.Pubmed_RVDocSum --Ryan Wise (talk) 13:10, 2 June 2008 (UTC)
- In the article, it said, "In one study, hypercalciuria and bone loss occurred in four patients with documented vitamin D toxicity." Could 25,000 IU have actually caused some demineralization? Brian Pearson (talk) 03:42, 3 June 2008 (UTC)
- It should, yes. Especially in such high doses. --Ryan Wise (talk) 18:21, 13 June 2008 (UTC)
Re Reference #54
It [10] mentions COMA -- Committee on Medical Aspects of Food and Nutrition Policy (UK; disbanded in 2000). It had recommended, "...For individuals confined indoors, pregnant and lactating women, an intake of 0.01 mg/day..." I think this is a bit outdated. It's my understanding 2000 IU is more appropriate. Brian Pearson (talk) 22:54, 27 June 2008 (UTC)
An explaination for the French paradox
See http://www.thelancet.com/journals/lancet/article/PIIS014067360668971X/abstract http://sci.tech-archive.net/Archive/sci.med.nutrition/2007-09/msg00331.html Incidently, took daily 400iu pill last winter - no colds at all. 80.2.194.251 (talk) 15:53, 28 June 2008 (UTC)
A new separate section on "function"
I suggest moving the part in the lede explaining the functions of vitamin D into a new, separate section, as are done with most other vitamin articles. Afterwards, we can start gradually incorporating infos about vitamin D's functions that were formerly scattered in the article or left unmentioned. If no one objects...... Keith Galveston (talk) 09:11, 29 June 2008 (UTC)
Brain lesions and vitamin D
Considering all the talk of increasing vitamin D levels, this study entitled Calcium and vitamin D intakes are positively associated with brain lesions in depressed and non-depressed elders seems intriguing. It is cited by Vascular events in healthy older women receiving calcium supplementation: randomised controlled trial, which is cited by an editorial called Mixed messages, as well as a [Assessing benefits and risks of hormone therapy in 2008: New evidence, especially with regard to the heart review of hormone therapy in women]. II | (t - c) 02:51, 16 July 2008 (UTC)
Maybe they were taking too much calcium or estrogen or whatever. Maybe the problem was the calcium compound or the source of vit-D or whether it was D2 or D3. What is needed is a study that tested a first group who were taking more than 400 IU vit-D3 per day and no calcium supplements and a second group who were taking more than 1000 mg calcium per day and no vit-D (and not much sun). And matched for HRT and other things. Greensburger (talk) 04:05, 16 July 2008 (UTC)
- Yes, the abstract was vague about dosage. Wonder if the article has more detail. Brian Pearson (talk) 05:44, 22 July 2008 (UTC)
- Vitamin D only puts calcium into the blood. Without adequate vitamin K extra Vitamin D can lead to calcification of soft tissues. Menaquinone (K2) seems to be the best form of K to prevent this. Also, blood thinners (warfarin, aspirin) often interefere with K metabolism leading to increased calcification. --Ryan Wise (talk) 04:15, 26 August 2008 (UTC)
Can someone watch this page? Dont let the misleading part about mushrooms get reverted.
The article says that the findings were experimental. Prior to my edit, the wikipedia article sounds as if I go to the store today and buy them, that I'm buying the kind that were exposed to UVB ionizing radiation (specifically 295-297 nanometer). Mushrooms do not deserve to be on the list, but I'll let it slide since I dont want to offend the person who put in the work and cited it. Is a very interesting article you can read it here.
Also there seems to be misunderstanding about how the IU system works. IU measures effects of a serving, not the measurement of how many vitamins are in it. This is the reason why vitamin pills can't list serving size of 100% daily serving (measured in IU's) of a vitamin, unless it is absorbed and is equivalent to the biological benefits of eating a healthy diet which also yields those same 100% IU benefits for whatever vitamin in question. The explanation over at the IU page is very biased and makes it look like doctors/scientists are dumb since measurements are not easily understood, and actually more misunderstood.
If someone puts back mushrooms into the list and lets readers make the assumption that mushrooms have a full serving of vitamin D, please leave a message on my talk page, or try to work it out with them, as they may not have read the discussion page. Thanks Sentriclecub (talk) 21:02, 5 August 2008 (UTC)
- Perhaps something like this should be included: [11] Faro0485 (talk) 05:40, 27 September 2008 (UTC)
Request
I have some concerns regarding one anon user's edits to this article: http://en.wikipedia.org/wiki/Special:Contributions/76.113.156.31 Could someone take a look at them to see if they're alright? Thanks. --Phenylalanine (talk) 03:41, 5 September 2008 (UTC)
See: Vieth R, Bischoff-Ferrari H, Boucher BJ, et al. The urgent need to recommend an intake of vitamin D that is effective. Am J Clin Nutr 2007;85:649 –50. —Preceding unsigned comment added by 76.113.156.31 (talk) 14:57, 22 September 2008 (UTC)
Depression?
I believe the citation given for depression is inappropriate - I've given my reasons over at Talk:Hypovitaminosis D, which uses the same citation. --144.53.226.17 (talk) 00:16, 6 January 2009 (UTC)
Mushrooms
Mushrooms are not discussed in this article. Monterey Mushrooms, in California, is selling UV treated mushrooms which purport to have 869 percent the daily value of vitamin D. This is currently being studied by the FDA
American Journal of Clinical Nutrition, Vol. 69, No. 1, 95-98, January 1999 reports on a study of the bioavailabily of Vitamin D in some Finish mushrooms, and found that they were a real source of Vitamin D.
Various mushrooms are listed as a good source of vitamin D on other websites, and it seems like this is a real omission from your article.
67.183.202.117 (talk) 19:24, 6 January 2009 (UTC)
- You're wrong. See the subsection on biochemistry of D. You didn't read the whole article! SBHarris 04:11, 28 January 2009 (UTC)
Reference to PDR
The reference to the PDR on the web went to the consumer PDR site. There was no support there for safety at a dosage of up to 10000 units per day.—Preceding unsigned comment added by User:Kd4ttc (talk • contribs)
- The book does. I've removed the link, it was just for convenience anyway.--DO11.10 (talk) 06:50, 28 January 2009 (UTC)
VITAMIN D : The power of the sun, sometimes.
VITAMIN D : The power of the sun, sometimes.
Here is an important lead that hopefully someone can follow up on...
I had the opportunity to ask a Dr. Lower, whose office is located on Bay Street in Thunder Bay
While sunlight is an important source of Vitamin D, we should understand that being in the Northern Hemisphere, (people above the 40th parellel) during the winter the Sun's usefulness is severely restricted by the angle of the earth which increases the filtering process of the essential light rays. The earths atmosphere renders most natural light exposure during the winter months useless (the same effect as sunlight rays being filtered through glass).
The conclusion he suggested that most all people living in the Northern Hemisphere take a Vitamin D3 supplement, or the old fashioned treatment, Cod Liver Oil
--Caesar J.B. Squitti: Son of Maryann Rosso and Arthur Natale Squitti (talk) 20:35, 20 February 2009 (UTC)
Just in case someone removes this important information,(as already has been done...)
- ^ Marshall T.G. (2006) “Molecular genomics offers new insight into the exact mechanism of action of common drugs - ARBs, Statins, and Corticosteroids.” FDA CDER Visiting Professor presentation. FDA Biosciences Library, Accession QH447.M27 2006. Videorecording: http://autoimmunityresearch.org/fda-visiting-professor-7mar06.ram Slide presentation: http://autoimmunityresearch.org/fda_visiting-professor_7mar06_144dpi.pdf
- ^ Evans RM. (2006 June 7). “Nuclear Receptors in Drug-Drug Interactions and Metabolic Disease.” FDA CDER Visiting Professor presentation.
- ^ Waterhouse JC, Marshall TG, Fenter B, Mangin M, Blaney G. (2006). High levels of active 1,25-dihydroxyvitamin D despite low levels of the 25-hydroxyvitamin D precursor — implications of dysregulated vitamin D for diagnosis and treatment of chronic disease. In VD Stoltz (ed.), Vitamin D: New Research (pp 1–23). New York: Nova Science Publishers.
- ^ Vieth, Rheinhold, [http://www.insinc.com/onlinetv/directms13oct2005/softvnetplayer.htm Prospects for Vitamin D Nutrition], Friday, October 21, 2005
