Chronic mucocutaneous candidiasis
| Chronic mucocutaneous candidiasis | |
|---|---|
| Other names | CMC[1] |
 | |
| Specialty | Infectious diseases, dermatology |
| Symptoms | Skin ulcer[2] |
| Types | CANDF1,2,3,4,5,6,7,8 and 9j |
| Diagnostic method | Thyroid function test, Liver function test[3][4] |
| Treatment | Systemic antifungal therapy[4] |
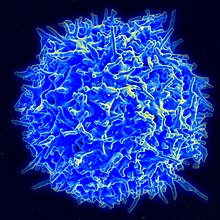
Chronic mucocutaneous candidiasis is an immune disorder of T cells.[4] It is characterized by chronic infections with Candida that are limited to mucosal surfaces, skin, and nails.[5]: 310 It can also be associated with other types of infections, such as human papilloma virus. An association with chromosome 2 has been identified.[medical citation needed]
Types
[edit]| Type | OMIMα | Gene | Locus |
|---|---|---|---|
| CANDF1 | 114580 | - | 2p |
| CANDF2 | 212050 | CARD9 | 9q34.3 |
| CANDF3 | 607644 | - | 11 |
| CANDF4 | 613108 | CLEC7A | 12p13.2-p12.3 |
| CANDF5 | 613953 | IL17RA | 22q11 |
| CANDF6 | 613956 | IL17F | 6p12 |
| CANDF7 | 614162 | STAT1 | 2q32 |
| CANDF8 | 615527 | TRAF3IP2 | 6q21 |
| CANDF9 | 616445 | IL17RC | 3q25 |
Signs and symptoms
[edit]The signs and symptoms of this condition are thickened skin, skin ulcer, dyspareunia, endocardium abnormality, vision problems, hepatitis, seizures, bloody urine, and meningitis.[2]
Associated diseases or conditions
[edit]There are a number of disorders associated with chronic mucocutaneous candidiasis including endocrine dysfunctions, vitiligo, malabsorption syndromes, neoplasms, and others. In most patients, chronic mucocutaneous candidiasis is correlated to abnormalities in cell-mediated immunity (T-lymphocyte mediated response)[citation needed]. The T-lymphocytes fail to produce the necessary cytokines that are required for immunity against Candida. Current effective treatments include anti-fungal drugs and, for long-term remissions, restoration of cellular immunity.[6]
Patients with autosomal-dominant mucocutaneous candidiasis may be at risk for epidermoid esophageal cancer due to the nitrosamine compounds produced by chronic candida infections.[citation needed][7]
Cause
[edit]Chronic mucocutaneous candidiasis can be inherited either autosomal dominant or autosomal recessive.[1] There are 9 types of this condition with the first CANDF1 being located at 2p22.3-p21 (cytogenetically).[8]
Mechanism
[edit]The mechanism the human immune system has is normally to fight an infection (like Candida). Initially, Th17 cells are made by the immune system, which in turn produces interleukin-17 (IL-17). This induces inflammation and white blood cells confront infection.[9]
Chronic mucocutaneous candidiasis mutations affect IL-17 by inhibiting its pathway. This in turn affects the human immune system's ability to fight infection, in total there are 9 possible types of this condition.[9][10]
-
Stat1(CANDF7 mutation on Chromosome 2q32)
-
CHR 2
Diagnosis
[edit]Chronic mucocutaneous candidiasis can be diagnosed in an affected individual via the following methods/tests:[3][4]
- Thyroid function test
- Liver function test
- Cellular immunity test
- Skin biopsy
- Genetic testing
Treatment
[edit]
Management for an individual with chronic mucocutaneous candidiasis consists of the following (relapse occurs once treatment is ceased, in many cases):[4][11]
- Systemic anti-fungal therapy (e.g., Fluconazole)
- Transfer factor
- Combination therapy
- Screening (annually)
See also
[edit]Notes
[edit]^ Indicates 9 references to specific, numbered pages in the Online Mendelian Inheritance in Man database.
References
[edit]- ^ a b RESERVED, INSERM US14 -- ALL RIGHTS. "Orphanet: Chronic mucocutaneous candidiasis". www.orpha.net. Archived from the original on 2017-07-14. Retrieved 2017-06-09.
{{cite web}}: CS1 maint: numeric names: authors list (link) - ^ a b "Candidiasis familial chronic mucocutaneous, autosomal recessive | Genetic and Rare Diseases Information Center (GARD) – an NCATS Program". rarediseases.info.nih.gov. Archived from the original on 2018-04-17. Retrieved 2017-06-09.
- ^ a b "Familial chronic mucocutaneous candidiasis - Conditions - GTR - NCBI". www.ncbi.nlm.nih.gov. Archived from the original on 2018-05-26. Retrieved 2017-06-09.
- ^ a b c d e "Chronic Mucocutaneous Candidiasis: Background, Pathophysiology, Epidemiology". Medscape. 3 May 2017. Archived from the original on 10 June 2017. Retrieved 8 June 2017.
- ^ James, William D.; Berger, Timothy G. (2006). Andrews' Diseases of the Skin: clinical Dermatology. Saunders Elsevier. ISBN 978-0-7216-2921-6.
- ^ Kirkpatrick, Charles H. (February 2001). "Chronic mucocutaneous candidiasis". The Pediatric Infectious Disease Journal. 20 (2): 197–206. doi:10.1097/00006454-200102000-00017. PMID 11224843.
- ^ Rosa DD, Pasqualotto AC, Denning DW. Chronic mucocutaneous candidiasis and oesophageal cancer. Med Mycol. 2008 Feb;46(1):85-91. doi: 10.1080/13693780701616023. PMID 17852718.
- ^ "OMIM Entry - % 114580 - CANDIDIASIS, FAMILIAL, 1; CANDF1". omim.org. Archived from the original on 31 March 2021. Retrieved 9 June 2017.
- ^ a b Reference, Genetics Home. "familial candidiasis". Genetics Home Reference. Archived from the original on 2017-06-27. Retrieved 2017-06-09.
- ^ Smeekens, Sanne P; van de Veerdonk, Frank L; Kullberg, Bart Jan; Netea, Mihai G (2013). "Genetic susceptibility to Candida infections". EMBO Molecular Medicine. 5 (6): 805–813. doi:10.1002/emmm.201201678. ISSN 1757-4676. PMC 3779444. PMID 23629947.
- ^ Teng, Joyce; Marqueling, Ann L.; Benjamin, Latanya (2016-12-15). Therapy in Pediatric Dermatology: Management of Pediatric Skin Disease. Springer. p. 265. ISBN 9783319436302. Archived from the original on 2023-01-12. Retrieved 2020-12-09.
Further reading
[edit]- Kauffman, Carol A.; Pappas, Peter G.; Sobel, Jack D.; Dismukes, William E. (2011). Essentials of Clinical Mycology. Springer Science & Business Media. ISBN 9781441966407. Retrieved 9 June 2017.
- Ostler, H. Bruce (2004). Diseases of the Eye and Skin: A Color Atlas. Lippincott Williams & Wilkins. ISBN 9780781749992. Retrieved 9 June 2017.


