Riboflavin: Difference between revisions
fixed citation references |
David notMD (talk | contribs) →Causes: adding content and refs about genetic defects causing riboflavin defic |
||
| Line 268: | Line 268: | ||
Subclinical deficiency has also been observed in women taking oral contraceptives, in the elderly, in people with [[eating disorder]]s, [[Alcoholism|chronic alcoholism]] and in diseases such as [[HIV]], [[inflammatory bowel disease]], [[diabetes]] and [[Heart disease|chronic heart disease]]. The Celiac Disease Foundation points out that a gluten-free diet may be low in riboflavin (and other nutrients) as enriched wheat flour and wheat foods (bread, pasta, cereals, etc.) are a major dietary contribution to total riboflavin intake.{{citation needed|date=June 2020}} |
Subclinical deficiency has also been observed in women taking oral contraceptives, in the elderly, in people with [[eating disorder]]s, [[Alcoholism|chronic alcoholism]] and in diseases such as [[HIV]], [[inflammatory bowel disease]], [[diabetes]] and [[Heart disease|chronic heart disease]]. The Celiac Disease Foundation points out that a gluten-free diet may be low in riboflavin (and other nutrients) as enriched wheat flour and wheat foods (bread, pasta, cereals, etc.) are a major dietary contribution to total riboflavin intake.{{citation needed|date=June 2020}} |
||
There are rare genetic defects that compromise riboflavin absorption, transport, metabolism or utilization by flavoproteins. One of these is riboflavin transporter deficiency, previously known as Brown-Vialetto-Van Laere syndrome. Variants of the genes SLC52A2 and SLC52A3 which code respectively, for transporter proteins RDVT2 and RDVT3 are defective. Infants and young children present with muscle weakness, cranial nerve deficits including hearing loss, sensory symptoms including sensory ataxia, feeding difficulties and respiratory difficulties which are caused by a sensorimotor axonal neuropathy and cranial neuropathy. When untreated, most infants with riboflavin transporter deficiency rapidly become ventilator dependent and die in the first decade of life. Treatment with oral supplementation of high amounts of riboflavin is lifesaving.<ref>{{cite journal |vauthors=Jaeger B, Bosch AM |title=Clinical presentation and outcome of riboflavin transporter deficiency: mini review after five years of experience |journal=J Inherit Metab Dis |volume=39 |issue=4 |pages=559–64 |date=July 2016 |pmid=26973221 |pmc=4920840 |doi=10.1007/s10545-016-9924-2 |url=}}</ref><ref>{{cite journal |vauthors=Cali E, Dominik N, Manole A, Houlden H |title=Riboflavin Transporter Deficiency |journal=GeneReviews [Internet] |volume= |issue= |pages= |date=2021 |pmid=26072523 |doi= |url=}}</ref> |
|||
===Diagnosis=== |
===Diagnosis=== |
||
Revision as of 11:55, 11 October 2021
 | |
 Chemical structure | |
| Clinical data | |
|---|---|
| Trade names | Many[1] |
| Other names | vactochrome, lactoflavin, vitamin G[2] |
| AHFS/Drugs.com | Monograph |
| License data |
|
| Routes of administration | By mouth, intramuscular, intravenous |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Elimination half-life | 66 to 84 minutes |
| Excretion | Urine |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| E number | E101, E101(iii) (colours) |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.001.370 |
| Chemical and physical data | |
| Formula | C17H20N4O6 |
| Molar mass | 376.369 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
Riboflavin, also known as vitamin B2, is a vitamin found in food and used as a dietary supplement.[1][3] It is required by the body for cellular respiration.[4]
Food sources include eggs, green vegetables, milk and other dairy products, meat, mushrooms, and almonds.[3] Some countries require its addition to grains.[3][5]
As a supplement, it is used to prevent and treat riboflavin deficiency, which affects the metabolism of iron.[3][4] Riboflavin may be given by mouth or injection, and is well-tolerated.[1] Riboflavin was discovered in 1920, isolated in 1933, and first synthesized in 1935.[2]
Definition
Riboflavin, also known as vitamin B2, is a vitamin found in food and sold as a dietary supplement.[3][4][6][7] It is used in food fortification programs in countries where deficiency is common.[8]
Synthesis
Biosynthesis
The biosynthesis of one riboflavin molecule requires ribulose 5-phosphate and guanosine triphosphate (GTP) as substrates.[9] The imidazole ring of GTP is hydrolytically opened, yielding a 5-amino-6-ribitylamino-2,4(1H,3H)-pyrimidinedione 5'-phosphate by a sequence of deamination, side chain reduction and dephosphorylation. Condensation of this molecule with 3,4-dihydroxy-2-butanone 4-phosphate obtained from ribulose 5-phosphate creates an unstable intermediate that converts to 6,7-dimethyl-8-ribityllumazine.[4][9]
Dismutation of two of this molecule, through action of the enzyme riboflavin synthase, yields riboflavin and a molecule of 5-amino-6-ribitylamino-2,4(1H,3H)-pyrimidinedione, which is recycled in the biosynthetic pathway.[4][7][9]
File:Mech 1.jpg File:Mech 2.jpg File:Mech 3.jpg File:Mech 4.jpg
Industrial synthesis
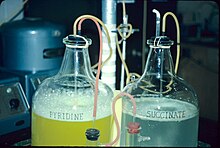
The industrial scale production of riboflavin uses various microorganisms, including filamentous fungi such as Ashbya gossypii, Candida famata and Candida flaveri, as well as the bacteria Corynebacterium ammoniagenes and Bacillus subtilis.[11] The last organism, genetically modified to both increase the production of riboflavin and to introduce an antibiotic (ampicillin) resistance marker, is employed at a commercial scale to produce riboflavin for feed and food fortification. Riboflavin is sometimes overproduced, possibly as a protective mechanism, by some bacteria in the presence of high concentrations of hydrocarbons or aromatic compounds. One such organism is Micrococcus luteus (American Type Culture Collection strain number ATCC 49442), which develops a yellow color due to production of riboflavin while growing on pyridine, but not when grown on other substrates, such as succinic acid.[10]
Functions
Flavin mononucleotide (FMN) and flavin adenine dinucleotide (FAD) function as cofactors for a variety of flavoprotein enzyme reactions:
- Flavoproteins of electron transport chain, including FMN in Complex I and FAD in Complex II
- FAD is required for the production of pyridoxic acid from pyridoxal (vitamin B6) by pyridoxine 5'-phosphate oxidase
- The primary coenzyme form of vitamin B6 (pyridoxal phosphate) is FMN dependent
- Oxidation of pyruvate, α-ketoglutarate, and branched-chain amino acids requires FAD in the shared E3 portion of their respective dehydrogenase complexes
- Fatty acyl CoA dehydrogenase requires FAD in fatty acid oxidation
- FAD is required to convert retinol (vitamin A) to retinoic acid via cytosolic retinal dehydrogenase
- Synthesis of an active form of folate (5-methyltetrahydrofolate) from 5,10-methylenetetrahydrofolate by methylenetetrahydrofolate reductase is FADH2 dependent
- FAD is required by Kynurenine 3-monooxygenase to convert tryptophan to niacin (vitamin B3)
- Reduction of the oxidized form of glutathione (GSSG) to its reduced form (GSH) by glutathione reductase is FAD dependent
Medical uses
Cornea thinning
Corneal ectasia is a progressive thinning of the cornea; the most common form of this condition is keratoconus. Corneal collagen crosslinking, causing an increase in corneal stiffness, is achieved by applying a riboflavin solution topically, then exposing to ultraviolet A light.[12][13]
Migraine
In its 2012 guidelines, the American Academy of Neurology included high-dose riboflavin (400 mg) as "probably effective and should be considered for migraine prevention,"[14] a recommendation also provided by the UK National Migraine Centre.[15] A 2017 review reported that daily riboflavin taken at 400 mg per day for at least three months may reduce the frequency of migraine headaches in adults.[16]
Despite being safe, inexpensive, and well-tolerated, use of high-dose riboflavin for migraine prevention or treatment in children and adolescents is inconclusive and not recommended.[1][3][17]
Dietary recommendations
| United States | ||
| Age group (years) | RDA for riboflavin (mg/d)[6] | Tolerable upper intake level[6] |
|---|---|---|
| Infants 0–6 months | 0.3* | ND |
| Infants 6–12 months | 0.4* | |
| 1–3 | 0.5 | |
| 4–8 | 0.6 | |
| 9–13 | 0.9 | |
| Females 14–18 | 1.0 | |
| Males 14–18 | 1.3 | |
| Females 19+ | 1.1 | |
| Males 19+ | 1.3 | |
| Pregnant females 14–50 | 1.4 | |
| Lactating females 14–50 | 1.6 | |
| European Food Safety Authority | ||
| Age group (years) | Adequate Intake of riboflavin (mg/d)[18] | Tolerable upper limit[18] |
| 7–11 months | 0.4 | ND |
| 1–3 | 0.6 | |
| 4–6 | 0.7 | |
| 7–10 | 1.0 | |
| 11–14 | 1.4 | |
| 15–17 | 1.6 | |
| 18+ | ||
| Australia and New Zealand | ||
| Age group (years) | Adequate Intake of riboflavin (mg/d)[19] | Upper level of intake[19] |
| 0–6 months | 0.3* | ND |
| 7–12 months | 0.4* | |
| 1–3 | 0.5 | |
| 4–8 | 0.6 | |
| 9–13 | 0.9 | |
| Females 14–70 | 1.1 | |
| Males 14–70 | 1.3 | |
| Females >70 | 1.3 | |
| Males >70 | 1.6 | |
| Pregnant females 14–50 | 1.4 | |
| Lactating females 14–50 | 1.6 | |
| * Adequate intake for infants, no RDA/RDI yet established[6] | ||
The National Academy of Medicine (then the U.S. Institute of Medicine [IOM]) updated Estimated Average Requirements (EARs) and Recommended Dietary Allowances (RDAs) for riboflavin in 1998. The current EARs for riboflavin for women and men ages 14 and up are 0.9 mg/day and 1.1 mg/day, respectively; the RDAs are 1.1 and 1.3 mg/day, respectively. RDAs are higher than EARs so as to identify amounts that will cover people with higher than average requirements. RDA for pregnancy is 1.4 mg/day. RDA for lactation is 1.6 mg/day. For infants up to 12 months the Adequate Intake (AI) is 0.3–0.4 mg/day. and for children ages 1–13 years the RDA increases with age from 0.5 to 0.9 mg/day. As for safety, the IOM sets Tolerable upper intake levels (ULs) for vitamins and minerals when evidence is sufficient. In the case of riboflavin there is no UL, as there is no human data for adverse effects from high doses. Collectively the EARs, RDAs, AIs and ULs are referred to as Dietary Reference Intakes (DRIs).[6][20]
The European Food Safety Authority (EFSA) refers to the collective set of information as Dietary Reference Values, with Population Reference Intake (PRI) instead of RDA, and Average Requirement instead of EAR. AI and UL defined the same as in United States. For women and men ages 15 and older the PRI is set at 1.6 mg/day. PRI for pregnancy is 1.9 mg/day, for lactation 2.0 mg/day. For children ages 1–14 years the PRIs increase with age from 0.6 to 1.4 mg/day. These PRIs are higher than the U.S. RDAs.[21] The EFSA also reviewed the safety question and like the U.S., decided that there was not sufficient information to set an UL.[22]
Safety
In humans, there is no evidence for riboflavin toxicity produced by excessive intakes. Absorption becomes less efficient as doses increase, and what is absorbed in excess of requirements is excreted via the kidneys into urine (resulting in a bright yellow color).[20][6][7] When up to 400 mg of riboflavin per day for trial periods of 3-12 months was consumed orally for research on reducing frequency and severity of migraine headache, there were reports of abdominal pain and diarrhea in the treated subjects.[16]
Labeling
For U.S. food and dietary supplement labeling purposes the amount in a serving is expressed as a percent of Daily Value (%DV). For riboflavin labeling purposes 100% of the Daily Value was 1.7 mg, but as of May 27, 2016, it was revised to 1.3 mg to bring it into agreement with the RDA.[23][24] A table of the old and new adult daily values is provided at Reference Daily Intake.
Sources
Food and beverages that provide riboflavin without fortification are milk, cheese, eggs, leaf vegetables, liver, kidneys, lean meats, legumes, mushrooms, and almonds.[4][6]
The milling of cereals results in considerable loss (up to 60%) of vitamin B2, so white flour is enriched in some countries by addition of the vitamin. The enrichment of bread and ready-to-eat breakfast cereals contributes significantly to the dietary supply of vitamin B2. Polished rice is not usually enriched, because the vitamin's yellow color would make the rice visually unacceptable to the major rice-consuming populations. However, most of the flavin content of whole brown rice is retained if the rice is steamed (parboiled) prior to milling. This process drives the flavins in the germ and aleurone layers into the endosperm. Free riboflavin is naturally present in foods along with protein-bound FMN and FAD. Bovine milk contains mainly free riboflavin, with a minor contribution from FMN and FAD. In whole milk, 14% of the flavins are bound noncovalently to specific proteins.[25] Milk and yogurt contain some of the highest riboflavin content.[3]
Riboflavin is added to baby foods, breakfast cereals, pastas and vitamin-enriched meal replacement products.[3] It is difficult to incorporate riboflavin into liquid products because it has poor solubility in water, hence the requirement for riboflavin-5'-phosphate (E101a), a more soluble form of riboflavin.[9]
Riboflavin is also used as a food coloring and as such is designated in Europe as the E number E101.[26] It is also used in cosmetics products to dye hair.[9]
Absorption, metabolism, excretion
The maximum amount of riboflavin that an adult can normally absorb in a single dose is 27 mg.[3][27] When excess amounts are consumed, they are either not absorbed or the small[specify] amount that is absorbed is excreted in urine.[6] After a single oral dose, biologic half-life is about 66 to 84 minutes in healthy people.[27]
Deficiency
Signs and symptoms
Mild riboflavin deficiencies can exceed 50% of the population in developing countries and in refugee situations. Deficiency is uncommon in the United States and in other countries that have wheat flour, bread, pasta, corn meal or rice enrichment regulations. In the U.S., starting in the 1940s, flour, corn meal and rice have been fortified with B vitamins as a means of restoring some of what is lost in milling, bleaching and other processing. For adults 20 and older, average intake from food and beverages is 1.8 mg/day for women and 2.5 mg/day for men. An estimated 23% consume a riboflavin-containing dietary supplement that provides on average 10 mg. The U.S. Department of Health and Human Services conducts National Health and Nutrition Examination Survey every two years and reports food results in a series of reports referred to as "What We Eat In America." From NHANES 2011–2012, estimates were that 8% of women and 3% of men consumed less than the RDA. When compared to the lower Estimated Average Requirements, fewer than 3% did not achieve the EAR level.[citation needed]
Riboflavin deficiency (also called ariboflavinosis) results in stomatitis including painful red tongue with sore throat, chapped and fissured lips (cheilosis), and inflammation of the corners of the mouth (angular stomatitis). There can be oily scaly skin rashes on the scrotum, vulva, philtrum of the lip, or the nasolabial folds. The eyes can become itchy, watery, bloodshot and sensitive to light.[28] Due to interference with iron absorption, even mild to moderate riboflavin deficiency results in an anemia with normal cell size and normal hemoglobin content (i.e. normochromic normocytic anemia). This is distinct from anemia caused by deficiency of folic acid (B9) or cyanocobalamin (B12), which causes anemia with large blood cells (megaloblastic anemia).[29] Deficiency of riboflavin during pregnancy can result in birth defects including congenital heart defects[30] and limb deformities.[31] Prolonged riboflavin insufficiency is also known to cause degeneration of the liver and nervous system.[6]
The stomatitis symptoms are similar to those seen in pellagra, which is caused by niacin (B3) deficiency. Therefore, riboflavin deficiency is sometimes called "pellagra sine pellagra" (pellagra without pellagra), because it causes stomatitis but not widespread peripheral skin lesions characteristic of niacin deficiency.[28]
Riboflavin deficiency prolongs recovery from malaria,[32] despite preventing growth of plasmodium (the malaria parasite).[33]
Causes
Riboflavin deficiency is usually found together with other nutrient deficiencies, particularly of other water-soluble vitamins. A deficiency of riboflavin can be primary – poor vitamin sources in one's daily diet – or secondary, which may be a result of conditions that affect absorption in the intestine, the body not being able to use the vitamin, or an increase in the excretion of the vitamin from the body.
Subclinical deficiency has also been observed in women taking oral contraceptives, in the elderly, in people with eating disorders, chronic alcoholism and in diseases such as HIV, inflammatory bowel disease, diabetes and chronic heart disease. The Celiac Disease Foundation points out that a gluten-free diet may be low in riboflavin (and other nutrients) as enriched wheat flour and wheat foods (bread, pasta, cereals, etc.) are a major dietary contribution to total riboflavin intake.[citation needed]
There are rare genetic defects that compromise riboflavin absorption, transport, metabolism or utilization by flavoproteins. One of these is riboflavin transporter deficiency, previously known as Brown-Vialetto-Van Laere syndrome. Variants of the genes SLC52A2 and SLC52A3 which code respectively, for transporter proteins RDVT2 and RDVT3 are defective. Infants and young children present with muscle weakness, cranial nerve deficits including hearing loss, sensory symptoms including sensory ataxia, feeding difficulties and respiratory difficulties which are caused by a sensorimotor axonal neuropathy and cranial neuropathy. When untreated, most infants with riboflavin transporter deficiency rapidly become ventilator dependent and die in the first decade of life. Treatment with oral supplementation of high amounts of riboflavin is lifesaving.[34][35]
Diagnosis
Riboflavin deficiency is also known as ariboflavinosis. The assessment of riboflavin status is essential for confirming cases with non-specific symptoms whenever deficiency is suspected. Indicators that have been used in humans are erythrocyte glutathione reductase, erythrocyte flavin concentration and urinary excretion, the last with either a normal urine sample or after a vitamin load test.[6][7] Erythrocyte glutathione reductase (EGR) is a flavin-adenine dinucleotide (FAD)-dependent enzyme, and the major flavoprotein in erythrocytes. Measurement of the activity coefficient of EGR is the preferred method for assessing riboflavin status. It provides a measure of tissue saturation and long-term riboflavin status. Fresh red blood cells are washed, lysed and assayed. Results are expressed as an activity coefficient (AC), a ratio, determined by enzyme activity with and without the addition of FAD) to the culture medium. An AC of 1.0 to 1,2 indicates that adequate amounts of riboflavin were present; 1.2 to 1.4 is considered low, greater than 1.4 indicates deficient.[7] With the erythrocyte flavin method, values greater than 400 nmol/L are considered adequate and values below 270 nmol/l deficient. This is not considered as sensitive as the EGR method.[6] Urinary excretion is expressed as nmol of riboflavin per gram of creatinine. Low is in range of 50 to 72 nmol/g and deficient is below 50 nmol/g. Load tests provided evidence for determining dietary requirements. For adult men, as oral doses were increased from 0.5 mg to 1.1 mg, there was a modest linear increase in urinary riboflavin, reaching 100 micrograms in a subsequent 24-hour urine collection. Beyond a load dose of 1.1 mg, urinary excretion increased rapidly, so that with a dose of 2.5 mg, urinary content was 800 micrograms.[6]
History
The name "riboflavin" comes from "ribose" (the sugar whose reduced form, ribitol, forms part of its structure) and "flavin", the ring-moiety which imparts the yellow color to the oxidized molecule (from Latin flavus, "yellow").[4] The reduced form, which occurs in metabolism along with the oxidized form, appears as orange-yellow needles or crystals.[9]
"Vitamin B" was originally considered to have two components, a heat-labile vitamin B1 and a heat-stable vitamin B2.[2] In the 1920s, vitamin B2 was initially thought to be the factor necessary for preventing pellagra.[2] In 1923, Paul Gyorgy in Heidelberg was investigating egg-white injury in rats;[2] the curative factor for this condition was called vitamin H, which is now called biotin. Since both pellagra and vitamin H deficiency were associated with dermatitis, Gyorgy decided to test the effect of vitamin B2 on vitamin H deficiency in rats. He enlisted the service of Wagner-Jauregg in Kuhn's laboratory.[2] In 1933, Kuhn, Gyorgy, and Wagner found that thiamin-free extracts of yeast, liver, or rice bran prevented the growth failure of rats fed a thiamin-supplemented diet.[2]
Further, the researchers noted that a yellow-green fluorescence in each extract promoted rat growth, and that the intensity of fluorescence was proportional to the effect on growth.[2] This observation enabled them to develop a rapid chemical and bioassay to isolate the factor from egg white in 1933.[2] The same group then isolated the same preparation (a growth-promoting compound with yellow-green fluorescence) from whey using the same procedure (lactoflavin). In 1934, Kuhn's group identified the structure of so-called flavin and synthesized vitamin B2, leading to evidence in 1939 that riboflavin was essential for human health.[2]
In the early years, the vitamin had also been referred to as "Vitamin G."[36]
See also
References
- ^ a b c d "Riboflavin". Drugs.com. 1 July 2021. Retrieved 8 October 2021.
- ^ a b c d e f g h i j Northrop-Clewes CA, Thurnham DI (2012). "The discovery and characterization of riboflavin". Annals of Nutrition & Metabolism. 61 (3): 224–30. doi:10.1159/000343111. PMID 23183293. S2CID 7331172.
- ^ a b c d e f g h i j "Riboflavin: Fact Sheet for Health Professionals". Office of Dietary Supplements, US National Institutes of Health. 20 August 2018. Retrieved 7 November 2018.
- ^ a b c d e f g "Riboflavin". Micronutrient Information Center, Linus Pauling Institute, Oregon State University. 2013. Retrieved 8 October 2021.
- ^ "What nutrients are added to flour and rice in fortification?". Food Fortification Initiative. 2021. Retrieved 8 October 2021.
- ^ a b c d e f g h i j k l Institute of Medicine (1998). "Riboflavin". Dietary Reference Intakes for Thiamin, Riboflavin, Niacin, Vitamin B6, Folate, Vitamin B12, Pantothenic Acid, Biotin, and Choline. Washington, DC: The National Academies Press. pp. 87–122. ISBN 978-0-309-06554-2. Archived from the original on 17 July 2015. Retrieved 29 August 2017.
- ^ a b c d e Merrill AH, McCormick DB (2020). "Riboflavin". In Marriott BP, Birt DF, Stallings VA, Yates AA (eds.). Present Knowledge in Nutrition (Eleventh ed.). London, United Kingdom: Academic Press (Elsevier). pp. 189–208. ISBN 978-0-323-66162-1.
- ^ "Map: Count of Nutrients In Fortification Standards". Global Fortification Data Exchange. Retrieved 1 August 2020.
- ^ a b c d e f "Riboflavin". PubChem, US National Library of Medicine. 2 October 2021. Retrieved 8 October 2021.
- ^ a b Sims GK, O'loughlin EJ (October 1992). "Riboflavin Production during Growth of Micrococcus luteus on Pyridine". Applied and Environmental Microbiology. 58 (10): 3423–5. Bibcode:1992ApEnM..58.3423S. doi:10.1128/AEM.58.10.3423-3425.1992. PMC 183117. PMID 16348793.
- ^ Stahmann KP, Revuelta JL, Seulberger H (May 2000). "Three biotechnical processes using Ashbya gossypii, Candida famata, or Bacillus subtilis compete with chemical riboflavin production". Applied Microbiology and Biotechnology. 53 (5): 509–16. doi:10.1007/s002530051649. PMID 10855708. S2CID 2471994.
- ^ Mastropasqua L (2015). "Collagen cross-linking: when and how? A review of the state of the art of the technique and new perspectives". Eye and Vision. 2: 19. doi:10.1186/s40662-015-0030-6. PMC 4675057. PMID 26665102.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Sorkin N, Varssano D (June 2014). "Corneal collagen crosslinking: a systematic review". Ophthalmologica. Journal International d'Ophtalmologie. International Journal of Ophthalmology. Zeitschrift Fur Augenheilkunde. 232 (1): 10–27. doi:10.1159/000357979. PMID 24751584. S2CID 32696531.
- ^ Holland S, Silberstein SD, Freitag F, Dodick DW, Argoff C, Ashman E (April 2012). "Evidence-based guideline update: NSAIDs and other complementary treatments for episodic migraine prevention in adults: report of the Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society". Neurology. 78 (17): 1346–53. doi:10.1212/wnl.0b013e3182535d0c. PMC 3335449. PMID 22529203.
- ^ ""Natural" remedies for migraine – should I try them?". UK National Migraine Centre. 2021. Retrieved 8 October 2021.
- ^ a b Thompson DF, Saluja HS (August 2017). "Prophylaxis of migraine headaches with riboflavin: A systematic review". Journal of Clinical Pharmacy and Therapeutics. 42 (4): 394–403. doi:10.1111/jcpt.12548. PMID 28485121. S2CID 29848028.
- ^ Sherwood M, Goldman RD (March 2014). "Effectiveness of riboflavin in pediatric migraine prevention". Canadian Family Physician Medecin de Famille Canadien. 60 (3): 244–6. PMC 3952759. PMID 24627379.
- ^ a b European Food Safety Authority (February 2006). "Tolerable Upper Intake Levels for Vitamins and Minerals" (PDF). EFSA. Retrieved 18 June 2018.
- ^ a b "Nutrient reference values for Australia and New Zealand" (PDF). National Health and Medical Research Council. 9 September 2005. Archived from the original (PDF) on 21 January 2017. Retrieved 19 June 2018.
- ^ a b Gropper SS, Smith JL, Groff JL (2009). "Ch. 9: Riboflavin". Advanced Nutrition and Human Metabolism (5th ed.). Wadsworth: CENGAG Learning. pp. 329–33. ISBN 9780495116578.
- ^ "Overview on Dietary Reference Values for the EU population as derived by the EFSA Panel on Dietetic Products, Nutrition and Allergies" (PDF). 2017. Archived (PDF) from the original on 28 August 2017.
- ^ "Tolerable Upper Intake Levels For Vitamins And Minerals" (PDF). European Food Safety Authority. 2006. Archived (PDF) from the original on 16 March 2016.
- ^ "Federal Register May 27, 2016 Food Labeling: Revision of the Nutrition and Supplement Facts Labels. FR page 33982" (PDF). Archived (PDF) from the original on 8 August 2016.
- ^ "Daily Value Reference of the Dietary Supplement Label Database (DSLD)". Dietary Supplement Label Database (DSLD). Retrieved 16 May 2020.
- ^ Kanno C, Kanehara N, Shirafuji K, Tanji R, Imai T (February 1991). "Binding form of vitamin B2 in bovine milk: its concentration, distribution and binding linkage". Journal of Nutritional Science and Vitaminology. 37 (1): 15–27. doi:10.3177/jnsv.37.15. PMID 1880629.
- ^ "Current EU approved additives and their E Numbers". UK Food Standards Agency. 27 July 2007. Archived from the original on 7 October 2010. Retrieved 3 December 2009.
- ^ a b Zempleni J, Galloway JR, McCormick DB (January 1996). "Pharmacokinetics of orally and intravenously administered riboflavin in healthy humans". The American Journal of Clinical Nutrition. 63 (1): 54–66. doi:10.1093/ajcn/63.1.54. PMID 8604671.
- ^ a b Sebrell WH, Butler RE (1939). "Riboflavin Deficiency in Man (Ariboflavinosis)". Public Health Reports. 54 (48): 2121–31. doi:10.2307/4583104. JSTOR 4583104.
- ^ Lane M, Alfrey CP (April 1965). "The Anemia of Human Riboflavin Deficiency". Blood. 25 (4): 432–42. doi:10.1182/blood.V25.4.432.432. PMID 14284333.
- ^ Smedts HP, Rakhshandehroo M, Verkleij-Hagoort AC, de Vries JH, Ottenkamp J, Steegers EA, Steegers-Theunissen RP (October 2008). "Maternal intake of fat, riboflavin and nicotinamide and the risk of having offspring with congenital heart defects". European Journal of Nutrition. 47 (7): 357–65. doi:10.1007/s00394-008-0735-6. PMID 18779918. S2CID 25548935.
- ^ Robitaille J, Carmichael SL, Shaw GM, Olney RS (September 2009). "Maternal nutrient intake and risks for transverse and longitudinal limb deficiencies: data from the National Birth Defects Prevention Study, 1997-2003". Birth Defects Research. Part A, Clinical and Molecular Teratology. 85 (9): 773–9. doi:10.1002/bdra.20587. PMID 19350655.
- ^ Das BS, Das DB, Satpathy RN, Patnaik JK, Bose TK (April 1988). "Riboflavin deficiency and severity of malaria". European Journal of Clinical Nutrition. 42 (4): 277–83. PMID 3293996.
- ^ Dutta P, Pinto J, Rivlin R (November 1985). "Antimalarial effects of riboflavin deficiency". Lancet. 2 (8463): 1040–3. doi:10.1016/S0140-6736(85)90909-2. PMID 2865519. S2CID 35542771.
- ^ Jaeger B, Bosch AM (July 2016). "Clinical presentation and outcome of riboflavin transporter deficiency: mini review after five years of experience". J Inherit Metab Dis. 39 (4): 559–64. doi:10.1007/s10545-016-9924-2. PMC 4920840. PMID 26973221.
- ^ Cali E, Dominik N, Manole A, Houlden H (2021). "Riboflavin Transporter Deficiency". GeneReviews [Internet]. PMID 26072523.
- ^ Levine H, Remington RE (May 1937). "The Vitamin G Content of Some Foods". J Nutr. 13 (5): 525–42. doi:10.1093/jn/13.5.525.
