Eltrombopag
 | |
| Clinical data | |
|---|---|
| Trade names | Promacta, Revolade, Alvaiz |
| Other names | SB-497115-GR |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a609011 |
| License data |
|
| Pregnancy category |
|
| Routes of administration | By mouth |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | ~52%[3] |
| Protein binding | >99% |
| Metabolism | extensive liver (through CYP1A2 and CYP2C8) |
| Elimination half-life | 21–35 hours |
| Excretion | feces (59%), urine (31%) |
| Identifiers | |
| |
| CAS Number |
|
| PubChem CID | |
| DrugBank |
|
| ChemSpider | |
| UNII |
|
| KEGG | |
| ChEBI | |
| ChEMBL |
|
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.128.125 |
| Chemical and physical data | |
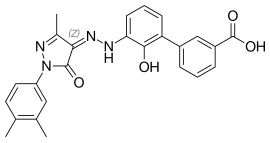
| Formula | C25H22N4O4 |
| Molar mass | 442.475 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| | |
Eltrombopag, sold under the brand name Promacta among others, is a medication used to treat thrombocytopenia (abnormally low platelet counts) and severe aplastic anemia.[3][4] Eltrombopag is sold under the brand name Revolade outside the US and is marketed by Novartis.[5] It is a thrombopoietin receptor agonist.[3] It is taken by mouth.[3][4]
Eltrombopag was discovered as a result of research collaboration between GlaxoSmithKline and Ligand Pharmaceuticals and is transferred to Novartis Pharmaceuticals.[5][6][7]
Medical uses
[edit]Eltrombopag was initially approved by the U.S. Food and Drug Administration (FDA) on 20 November 2008, for the treatment of thrombocytopenia in people with chronic immune (idiopathic) thrombocytopenic purpura who have had an insufficient response to corticosteroids, immunoglobulin therapy, or splenectomy.[8][9][10]
On 24 August 2015, the FDA approved eltrombopag (Promacta for oral suspension) for the treatment of thrombocytopenia in children one year and older with idiopathic thrombocytopenia who have had an insufficient response to corticosteroids, immunoglobulins, or splenectomy.[11]
Development
[edit]In preclinical studies, the compound was shown to interact selectively with the thrombopoietin receptor, leading to activation of the JAK-STAT signaling pathway and increased proliferation and differentiation of megakaryocytes. Animal studies confirmed that it increased platelet counts. In 73 healthy volunteers, higher doses of eltrombopag caused larger increases in the number of circulating platelets without tolerability problems.[12]
Clinical trials
[edit]Eltrombopag has been shown to be effective in two major clinical syndromes: idiopathic thrombocytopenic purpura (ITP)[13] and cirrhosis due to hepatitis C (in which low platelet counts may be a contraindication for interferon treatment).[14]
After six weeks of therapy in a phase III trial, eltrombopag 50 mg/day was associated with a significantly higher response rate than placebo in adult patients with chronic idiopathic thrombocytopenic purpura (ITP).[15]
History
[edit]Eltrombopag received breakthrough therapy designation from the U.S. Food and Drug Administration (FDA) in February 2014, for people with aplastic anemia for which immunosuppression has not been successful.[16] In 2017, the NIH made Eltrombopag a standard of care in aplastic anemia.[17]
Research
[edit]It has been shown to produce a trilineage hematopoiesis in some people with aplastic anemia, resulting in increased platelet counts, along with red and white blood cell counts.[18]
References
[edit]- ^ a b "Revolade Product Information". Therapeutic Goods Administration (TGA). Archived from the original on 23 May 2021. Retrieved 23 May 2021.
- ^ "Revolade 25 mg film-coated tablets - Summary of Product Characteristics (SmPC)". (emc). 17 August 2020. Archived from the original on 23 May 2021. Retrieved 22 May 2021.
- ^ a b c d e "Promacta- eltrombopag olamine tablet, film coated Promacta- eltrombopag olamine powder, for suspension". DailyMed. Archived from the original on 23 May 2021. Retrieved 22 May 2021.
- ^ a b c "Revolade EPAR". European Medicines Agency (EMA). 17 September 2018. Archived from the original on 23 May 2021. Retrieved 22 May 2021.
- ^ a b "Ligand Sells Promacta Assets and Royalty for $827 Million" (Press release). Ligand Pharmaceuticals. 5 March 2019. Archived from the original on 24 June 2021. Retrieved 17 June 2021 – via Business Wire.
- ^ "Revolade". GSK Canada. Archived from the original on 28 June 2021. Retrieved 17 June 2021.
- ^ "Novartis announces completion of transactions with GSK". Sandoz (Press release). Archived from the original on 24 June 2021. Retrieved 17 June 2021.
- ^ "Approval Letter" (PDF). U.S. Food and Drug Administration (FDA). Archived (PDF) from the original on 28 February 2017. Retrieved 18 March 2016.
- ^ "Drug Approval Package: Promacta (Eltrombopag) NDA #022291". U.S. Food and Drug Administration (FDA). 14 January 2009. Archived from the original on 3 April 2021. Retrieved 22 May 2021.
- ^ "Summary Review" (PDF). U.S. Food and Drug Administration (FDA). 19 January 2008. Archived (PDF) from the original on 23 May 2021. Retrieved 22 May 2021.
- ^ "FDA extends use of Promacta in young children with rare blood disorder" (Press release). U.S. Food and Drug Administration (FDA). Archived from the original on 26 January 2018. Retrieved 18 March 2016.
- ^ Jenkins JM, Williams D, Deng Y, Uhl J, Kitchen V, Collins D, Erickson-Miller CL (June 2007). "Phase 1 clinical study of eltrombopag, an oral, nonpeptide thrombopoietin receptor agonist". Blood. 109 (11): 4739–4741. doi:10.1182/blood-2006-11-057968. PMID 17327409.
- ^ Bussel JB, Cheng G, Saleh MN, Psaila B, Kovaleva L, Meddeb B, et al. (November 2007). "Eltrombopag for the treatment of chronic idiopathic thrombocytopenic purpura". The New England Journal of Medicine. 357 (22): 2237–2247. doi:10.1056/NEJMoa073275. PMID 18046028.
- ^ McHutchison JG, Dusheiko G, Shiffman ML, Rodriguez-Torres M, Sigal S, Bourliere M, et al. (November 2007). "Eltrombopag for thrombocytopenia in patients with cirrhosis associated with hepatitis C". The New England Journal of Medicine. 357 (22): 2227–2236. doi:10.1056/NEJMoa073255. PMID 18046027. Archived from the original on 17 October 2021. Retrieved 12 December 2019.
- ^ Garnock-Jones KP, Keam SJ (2009). "Eltrombopag". Drugs. 69 (5): 567–576. doi:10.2165/00003495-200969050-00005. PMID 19368418. S2CID 265943270.
- ^ "Eltrombopag / Promacta". U.S. Food and Drug Administration (FDA). Archived from the original on 6 December 2016. Retrieved 18 March 2016.
- ^ Townsley DM, Scheinberg P, Winkler T, Desmond R, Dumitriu B, Rios O, et al. (April 2017). "Eltrombopag Added to Standard Immunosuppression for Aplastic Anemia". The New England Journal of Medicine. 376 (16): 1540–1550. doi:10.1056/NEJMoa1613878. PMC 5548296. PMID 28423296.
- ^ Desmond R, Townsley DM, Dumitriu B, Olnes MJ, Scheinberg P, Bevans M, et al. (March 2014). "Eltrombopag restores trilineage hematopoiesis in refractory severe aplastic anemia that can be sustained on discontinuation of drug". Blood. 123 (12): 1818–1825. doi:10.1182/blood-2013-10-534743. PMC 3962161. PMID 24345753.
External links
[edit]- "Eltrombopag". Drug Information Portal. U.S. National Library of Medicine.
- "Eltrombopag olamine". Drug Information Portal. U.S. National Library of Medicine.
- Clinical trial number NCT00102739 for "SB-497115 (Oral Thrombopoietin Receptor Agonist) Versus Placebo In Adults With Refractory Immune Thrombocytopenic Purpura (ITP)" at ClinicalTrials.gov
- Clinical trial number NCT00370331 for "RAISE: Randomized Placebo-Controlled Idiopathic Thrombocytopenic Purpura (ITP) Study With Eltrombopag (RAISE)" at ClinicalTrials.gov
- Clinical trial number NCT00351468 for "EXTEND (Eltrombopag Extended Dosing Study) (EXTEND)" at ClinicalTrials.gov
- Clinical trial number NCT01520909 for "Study of a New Medication for Childhood Chronic Immune Thrombocytopenia (ITP), a Blood Disorder of Low Platelet Counts That Can Lead to Bruising Easily, Bleeding Gums, and/or Bleeding Inside the Body. (PETIT2)" at ClinicalTrials.gov
- Clinical trial number NCT00908037 for "Efficacy and Safety Study of Eltrombopag in Pediatric Patients With Thrombocytopenia From Chronic Idiopathic Thrombocytopenic Purpura (ITP) (PETIT)" at ClinicalTrials.gov
- Clinical trial number NCT00516321 for "Eltrombopag To Initiate And Maintain Interferon Antiviral Treatment To Subjects With Hepatitis C Related Liver Disease" at ClinicalTrials.gov
- Clinical trial number NCT00529568 for "Eltrombopag To Initiate And Maintain Interferon Antiviral Treatment To Benefit Subjects With Hepatitis C Liver Disease" at ClinicalTrials.gov
- Clinical trial number NCT01623167 for "Eltrombopag With Standard Immunosuppression for Severe Aplastic Anemia" at ClinicalTrials.gov
- Clinical trial number NCT00922883 for "A Pilot Study of the Thrombopoietin-Receptor Agonist Eltrombopag in Refractory Aplastic Anemia Patients" at ClinicalTrials.gov
