Tubo-ovarian abscess
| Tubo-ovarian abscess | |
|---|---|
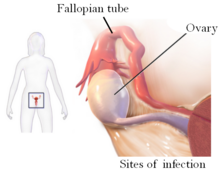 | |
| Drawing showing the sites of a tubo-ovarian abscess | |
| Specialty | Urology, gynaecology |
A tubo-ovarian abscess (TOA) is one of the late complications of pelvic inflammatory disease (PID) and can be life-threatening if the abscess ruptures and results in sepsis. It consists of an encapsulated or confined pocket of pus with defined boundaries that forms during an infection of a fallopian tube and ovary. These abscesses are found most commonly in reproductive age women and typically result from upper genital tract infection.[1][2] It is an inflammatory mass involving the fallopian tube, ovary and, occasionally, other adjacent pelvic organs. A TOA can also develop as a complication of a hysterectomy.[3]: 103
Symptoms typically include fever, an elevated white blood cell count, lower abdominal-pelvic pain, and/or vaginal discharge. Fever and leukocytosis may be absent. TOAs are often polymicrobial with a high percentage of anaerobic bacteria. The cost of treatment in the United States is approximately $2,000 per patient, which equals about $1.5 billion annually.[1] Though rare, TOA can occur without a preceding episode of PID or sexual activity.[4][5]
Signs and symptoms

The signs and symptoms of tubo-ovarian abscess (TOA) are the same as with pelvic inflammatory disease (PID) with the exception that the abscess can be found with magnetic resonance imaging (MRI), sonography and x-ray.[1] It also differs from PID in that it can create symptoms of acute-onset pelvic pain.[6] Typically this disease is found in sexually active women.[4][7] Tubo-ovarian abscess can mimic abdominal tumours.[8]
Complications
Complications of TOA are related to the possible removal of one or both ovaries and fallopian tubes. Without these reproductive structures, fertility can be affected. Surgical complications can develop and include:[citation needed]
- Allergic shock due to anesthetics
- A paradoxical reaction to a drug
- Infection
Cause
The development of TOA is thought to begin with the pathogens spreading from the cervix to the endometrium, through the salpinx, into the peritoneal cavity and forming the tubo-ovarian abscess with (in some cases) pelvic peritonitis. TOA can develop from the lymphatic system with infection of the parametrium from an intrauterine device (IUD).[1] Bacteria recovered from TOAs are Escherichia coli, Bacteroides fragilis, other Bacteroides species, Peptostreptococcus, Peptococcus, and aerobic streptococci.[9] Long term IUD use is associated with TOA.[10] Actinomyces is also recovered from TOA.[10]
| Genus | species | Gram stain | form | genome sequenced | reference |
|---|---|---|---|---|---|
| Neisseria gonorrhoeae | spp. | + | cocci | [1][11] | |
| Chlamydia trachomatis | spp. | + | intracellular | [1][11] | |
| Mycoplasma genitalium | spp. | + | bacillus | [11] | |
| Mycoplasma hominis | [11] | ||||
| Ureaplasma urealyticum | + | bacillus | [11] | ||
| Escherichia coli | + | bacillus | X | [4][9][11] | |
| Corynebacterium jeikeium | + | bacillus | X | [11] | |
| Bacteroides fragilis | + | bacillus | X | [9][11] | |
| Lactobacillus | jensenii | + | bacillus | [11] | |
| Cutibacterium acnes | + | bacillus | [11] | ||
| Haemophilus influenzae | + | bacillus | [11] | ||
| Streptococcus pneumoniae | + | cocci | [11] | ||
| Streptococcus constellatus | + | cocci | [9][11] | ||
| Prevotella bivia | + | bacillus | [11] | ||
| Fusobacterium nucleatum | + | bacillus | [11] | ||
| Enterococcus faecium | + | cocci | [11] | ||
| Actinomyces neuii | + | bacillus | X | [11] | |
| Lactobacillus | delbrueckii | + | bacillus | [11] | |
| Streptococcus intermedius | + | cocci | [9][11] | ||
| Eikenella corrodens | + | bacillus | X | [11] | |
| Abiotrophia | + | bacillus | X | [4] | |
| Granulicatella | + | bacillus | X | [4] |
Diagnosis
Laparoscopy and other imaging tools can visualize the abscess. Physicians are able to make the diagnosis if the abscess ruptures when the woman begins to have lower abdominal pain that then begins to spread. The symptoms then become the same as the symptoms for peritonitis. Sepsis occurs, if left untreated.[3]: 103 Ultrasonography is a sensitive enough imaging tool that it can accurately differentiate between pregnancy, hemorrhagic ovarian cysts, endometriosis, ovarian torsion, and tubo-ovarian abscess. Its availability, the relative advancement in the training of its use, its low cost, and because it does not expose the woman (or fetus) to ionizing radiation, ultrasonography an ideal imaging procedure for women of reproductive age.[6]
Prevention
Risk factors have been identified which indicate what women will be more likely to develop TOA. These are: increased age, IUD insertion, chlamydia infection, and increased levels of certain proteins (CRP and CA-125) and will alert clinicians to follow up on unresolved symptoms of PID.[12]
Treatment
Treatment for TOA differs from PID in that some clinicians recommend patients with tubo-ovarian abscesses have at least 24 hours of inpatient parenteral treatment with antibiotics, and that they may require surgery.[1][13] If surgery becomes necessary, pre-operative administration of broad-spectrum antibiotics is started and removal of the abscess, the affected ovary and fallopian tube is done. After discharge from the hospital, oral antibiotics are continued for the length of time prescribed by the physician.[3]: 103
Treatment is different if the TOA is discovered before it ruptures and can be treated with IV antibiotics. During this treatment, IV antibiotics are usually replaced with oral antibiotics on an outpatient basis. Patients are usually seen three days after hospital discharge and then again one to two weeks later to confirm that the infection has cleared.[3]: 103 Ampicillin/sulbactam plus doxycycline is effective against C. trachomatis, N. gonorrhoeae, and anaerobes in women with tubo-ovarian abscess. Parenteral Regimens described by the Centers for Disease Control and prevention are Ampicillin/Sulbactam 3 g IV every 6 hours and Doxycycline 200 mg orally or IV every 24 hours, though other regiments that are used for pelvic inflammatory disease have been effective.[14]
Epidemiology
The epidemiology of TOA is closely related to that of pelvic inflammatory disease which is estimated to one million people yearly.[15]
References
- ^ a b c d e f g Pelvic inflammatory disease. American Family Physician, Vol. 85, No. 8. (15 April 2012), pp. 791-796 by Margaret Gradison
- ^ "CDC - Pelvic Inflammatory Disease - 2010 STD Treatment Guidelines". Retrieved 2015-05-16.
- ^ a b c d Hoffman, Barbara (2012). Williams gynecology. New York: McGraw-Hill Medical. ISBN 9780071716727.
- ^ a b c d e Goodwin, K.; Fleming, N.; Dumont, T. (2013). "Tubo-ovarian Abscess in Virginal Adolescent Females: A Case Report and Review of the Literature". Journal of Pediatric and Adolescent Gynecology. 26 (4): e99–e102. doi:10.1016/j.jpag.2013.02.004. ISSN 1083-3188. PMID 23566794.
- ^ Ho, Jeh Wen; Angstetra, D.; Loong, R.; Fleming, T. (2014). "Tuboovarian Abscess as Primary Presentation for Imperforate Hymen". Case Reports in Obstetrics and Gynecology. 2014: 1–3. doi:10.1155/2014/142039. ISSN 2090-6684. PMC 4009186. PMID 24822139.
- ^ a b Dupuis, Carolyn S.; Kim, Young H. (2015). "Ultrasonography of adnexal causes of acute pelvic pain in pre-menopausal non-pregnant women". Ultrasonography. 34 (4): 258–267. doi:10.14366/usg.15013. ISSN 2288-5919. PMC 4603210. PMID 26062637.
- ^ Cho, Hyun-Woong; Koo, Yu-Jin; Min, Kyung-Jin; Hong, Jin-Hwa; Lee, Jae-Kwan (2015). "Pelvic Inflammatory Disease in Virgin Women with Tubo-ovarian Abscess: A Single-center Experience and Literature Review". Journal of Pediatric and Adolescent Gynecology. 30 (2): 203–208. doi:10.1016/j.jpag.2015.08.001. ISSN 1083-3188. PMID 26260586.
- ^ Lim, Andy; Pourya, Pouryahya; Lim, Alvin (2020). "Tubo-ovarian Abscess Masquerading as Dual Tumours". OSP Journal of Case Reports. 2 (2). doi:10.26180/5ed852773f47e. Retrieved 4 June 2020.
- ^ a b c d e Landers, D. V.; Sweet, R. L. (1983). "Tubo-ovarian Abscess: Contemporary Approach to Management". Clinical Infectious Diseases. 5 (5): 876–884. doi:10.1093/clinids/5.5.876. ISSN 1058-4838. PMID 6635426.
- ^ a b Lentz, Gretchen (2013). Comprehensive gynecology. Philadelphia: Mosby Elsevier. p. 558. ISBN 9780323069861.
- ^ a b c d e f g h i j k l m n o p q r s t Dessein, Rodrigue; Giraudet, Géraldine; Marceau, Laure; Kipnis, Eric; Galichet, Sébastien; Lucot, Jean-Philippe; Faure, Karine; Munson, E. (2015). "Identification of Sexually Transmitted Bacteria in Tubo-Ovarian Abscesses through Nucleic Acid Amplification: TABLE 1". Journal of Clinical Microbiology. 53 (1): 357–359. doi:10.1128/JCM.02575-14. ISSN 0095-1137. PMC 4290956. PMID 25355760.
- ^ Lee, Suk Woo; Rhim, Chae Chun; Kim, Jang Heub; Lee, Sung Jong; Yoo, Sie Hyeon; Kim, Shin Young; Hwang, Young Bin; Shin, So Young; Yoon, Joo Hee (2015). "Predictive Markers of Tubo-Ovarian Abscess in Pelvic Inflammatory Disease". Gynecologic and Obstetric Investigation. 81 (2): 97–104. doi:10.1159/000381772. ISSN 0378-7346. PMID 25926103. S2CID 27186672.
- ^ Lentz, Gretchen (2013). Comprehensive gynecology. Philadelphia: Mosby Elsevier. p. 584. ISBN 9780323069861.
- ^ "CDC - Pelvic Inflammatory Disease - 2010 STD Treatment Guidelines". www.cdc.gov. Archived from the original on 2011-02-09.
- ^ "PID Epidemiology". Center for Disease Control. Archived from the original on 2015-02-22. Retrieved 2015-05-21.
External links

