Osteoarthritis: Difference between revisions
→Alternative medicine: removed indepth discussion to subsection |
Reverted to revision 549216632 by Sthubbar: 5 reverts for Doc James in 24hrs, isn't that auto 24hr ban. Stop removing all added treatments. If you want to remove one or two, but justify the individual removals.. (TW) |
||
| Line 105: | Line 105: | ||
===Alternative medicine=== |
===Alternative medicine=== |
||
The following show promise as treatments for OA [[avocado]]/[[soybean]] [[unsaponifiables]]<ref>{{cite journal|last=Pirotta|first=M|title=Arthritis disease - the use of complementary therapies.|journal=Australian family physician|date=2010 Sep|volume=39|issue=9|pages=638-40|pmid=20877766}}</ref>, [[boswellic acid]]<ref>{{cite journal|last=Rosenbaum|first=CC|coauthors=O'Mathúna, DP; Chavez, M; Shields, K|title=Antioxidants and antiinflammatory dietary supplements for osteoarthritis and rheumatoid arthritis.|journal=Alternative therapies in health and medicine|date=2010 Mar-Apr|volume=16|issue=2|pages=32-40|pmid=21553931}}</ref>, [[Uncaria guianensis|cat's claw]]<ref>{{cite journal|pmid=20232616}}</ref>, [[curcumin]]<ref>{{cite journal|pmid=19836480}}</ref>, [[chondroitin]]<ref>{{cite journal|last=Pirotta|first=M|title=Arthritis disease - the use of complementary therapies.|journal=Australian family physician|date=2010 Sep|volume=39|issue=9|pages=638-40|pmid=20877766}}</ref><ref>{{cite journal|last=Schneider|first=Heinz|title=Symptom-Modifying Effect of Chondroitin Sulfate in Knee Osteoarthritis: A Meta-Analysis of Randomized Placebo-Controlled Trials Performed with Structum®|journal=The Open Rheumatology Journal|date=25 July 2012|volume=6|issue=1|pages=183–189|doi=10.2174/1874312901206010183}}</ref>, [[Harpagophytum|Devil's claw]]<ref>{{cite journal|last=Rosenbaum|first=CC|coauthors=O'Mathúna, DP; Chavez, M; Shields, K|title=Antioxidants and antiinflammatory dietary supplements for osteoarthritis and rheumatoid arthritis.|journal=Alternative therapies in health and medicine|date=2010 Mar-Apr|volume=16|issue=2|pages=32-40|pmid=17627199}}</ref>, [[glucosamine sulfate]]<ref>{{cite journal|last=Rovati|first=L. C.|coauthors=Girolami, F.; Persiani, S.|title=Crystalline glucosamine sulfate in the management of knee osteoarthritis: efficacy, safety, and pharmacokinetic properties|journal=Therapeutic Advances in Musculoskeletal Disease|date=8 March 2012|volume=4|issue=3|pages=167–180|doi=10.1177/1759720X12437753}}</ref> , [[S-Adenosyl methionine]]<ref name=Hard2003>{{cite journal |author=Hardy ML |title=S-adenosyl-L-methionine for treatment of depression, osteoarthritis, and liver disease |journal=Evid Rep Technol Assess (Summ) |issue=64 |pages=1–3 |year=2003 |month=August |pmid=12899148 |author-separator=, |author2=Coulter I |author3=Morton SC |display-authors=3 |last4=Favreau |first4=J |last5=Venuturupalli |first5=S |last6=Chiappelli |first6=F |last7=Rossi |first7=F |last8=Orshansky |first8=G |last9=Jungvig |first9=LK}}</ref><ref>{{cite journal|last=De Silva|first=V|coauthors=El-Metwally, A, Ernst, E, Lewith, G, Macfarlane, GJ, Arthritis Research UK Working Group on Complementary and Alternative, Medicines|title=Evidence for the efficacy of complementary and alternative medicines in the management of osteoarthritis: a systematic review|journal=Rheumatology |date=May 2011 |volume=50|issue=5|pages=911–20|pmid=21169345|doi=10.1093/rheumatology/keq379}}</ref> and [[Transcutaneous electrical nerve stimulation|TENS]].<ref>{{cite journal|last=Ying|first=KN|coauthors=While, A|title=Pain relief in osteoarthritis and rheumatoid arthritis: TENS.|journal=British journal of community nursing|date=2007 Aug|volume=12|issue=8|pages=364-71|pmid=17851302}}</ref> |
|||
;Acupuncture |
;Acupuncture |
||
A [[Cochrane review]] found that while acupuncture leads to a [[statistically significant]] improvement in pain relief, this improvement is small and may be of questionable [[clinical significance]]. Waiting list-controlled trials for peripheral joint |
A [[Cochrane review]] found that while acupuncture leads to a [[statistically significant]] improvement in pain relief, this improvement is small and may be of questionable [[clinical significance]]. Waiting list-controlled trials for peripheral joint OA do show clinically relevant benefits, but these may be due to placebo effects.<ref>{{cite journal |author=Manheimer E |title=Acupuncture for peripheral joint osteoarthritis |journal=Cochrane Database Syst Rev |issue=1 |pages=CD001977 |year=2010 |pmid=20091527 |doi=10.1002/14651858.CD001977.pub2 |editor1-last=Manheimer |editor1-first=Eric |pmc=3169099 |author-separator=, |author2=Cheng K |author3=Linde K |display-authors=3 |last4=Lao |first4=L |last5=Yoo |first5=J |last6=Wieland |first6=S |last7=Van Der Windt |first7=DA |last8=Berman |first8=BM |last9=Bouter |first9=LM}}</ref> Acupuncture does not seem to produce long-term benefits.<ref>{{cite journal | last = Wang | first = S | coauthors = Kain ZN; White PF | year = 2008 | journal = Anesth Analg | doi = 10.1213/ane.0b013e318160644d | url = http://www.thecochranelibrary.com/.../file/Acupuncture.../CD001977.pdf | title = Acupuncture Analgesia: II. Clinical Considerations | volume = 106 | pages = 611–21 | pmid = 18227323 | issue = 2 }}</ref> |
||
;Glucosamine |
;Glucosamine |
||
Controversy surrounding glucosamine may be due to including the ineffective hydrochloride and the effective sulfate preperations of glucosamine as well as different treatment protocols and preperations.<ref>[http://www.bestbets.org/bets/bet.php?id=979 The effects of Glucosamine Sulphate on OA of the knee joint]. BestBets.</ref>.<ref name=pmid17599746>{{cite journal |author=Vlad SC, Lavalley MP, McAlindon TE, Felson DT |title=Glucosamine for pain in osteoarthritis: Why do trial results differ? |journal= Arthritis & Rheumatism|volume=56 |issue=7 |pages=2267–77 |year=2007 |pmid=17599746 |doi=10.1002/art.22728}}</ref> A 2010 meta-analysis has found that it is no better than [[placebo]].<ref name="pmid20847017">{{cite journal |author=Wandel S, Jüni P, Tendal B, ''et al.'' |title=Effects of glucosamine, chondroitin, or placebo in patients with [http://www.acumio.com/dealing-osteoarthritis-guide-afflicted-individuals-485.html osteoarthritis] of hip or knee: network meta-analysis |journal=BMJ |volume=341 |pages=c4675 |year=2010 |pmid=20847017 |pmc=2941572 |doi=10.1136/bmj.c4675}}</ref> [[Glucosamine sulfate]] is an effective treatment<ref>{{cite journal|last=Pirotta|first=M|title=Arthritis disease - the use of complementary therapies.|journal=Australian family physician|date=2010 Sep|volume=39|issue=9|pages=638-40|pmid=20877766}}</ref><ref name=pmid15855241>{{cite journal |author=Poolsup N, Suthisisang C, Channark P, Kittikulsuth W |title=Glucosamine long-term treatment and the progression of knee osteoarthritis: systematic review of randomized controlled trials |journal=The Annals of pharmacotherapy |volume=39 |issue=6 |pages=1080–7 |year=2005 |pmid=15855241 |doi=10.1345/aph.1E576}}</ref><ref>{{cite journal |author=Black C |title=The clinical effectiveness of glucosamine and chondroitin supplements in slowing or arresting progression of osteoarthritis of the knee: a systematic review and economic evaluation |journal=Health Technol Assess |volume=13 |issue=52 |pages=1–148 |year=2009 |month=November |pmid=19903416 |url=http://www.hta.ac.uk/execsumm/summ1352.htm |author-separator=, |author2=Clar C |author3=Henderson R |display-authors=3 |last4=MacEachern |first4=C |last5=McNamee |first5=P |last6=Quayyum |first6=Z |last7=Royle |first7=P |last8=Thomas |first8=S |doi=10.3310/hta13520}}</ref> The [[Osteoarthritis Research Society International]] (OARSI) recommends that glucosamine be discontinued if no effect is observed after six months.<ref>{{cite journal |author=Zhang W |title=OARSI recommendations for the management of hip and knee osteoarthritis, Part II: OARSI evidence-based, expert consensus guidelines |journal=Osteoarthr. Cartil. |volume=16 |issue=2 |pages=137–62 |year=2008 |month=February |pmid=18279766 |doi=10.1016/j.joca.2007.12.013 |url=http://www.oarsi.org/pdfs/part_II_OARSI_recommendations_for_management_of_hipknee_OA_2007.pdf |author-separator=, |author2=Moskowitz RW |author3=Nuki G |display-authors=3 |last4=Abramson |first4=S. |last5=Altman |first5=R.D. |last6=Arden |first6=N. |last7=Bierma-Zeinstra |first7=S. |last8=Brandt |first8=K.D. |last9=Croft |first9=P.}}</ref> |
|||
==Epidemiology== |
==Epidemiology== |
||
Revision as of 23:51, 7 April 2013
| Osteoarthritis | |
|---|---|
| Specialty | Family medicine, orthopedic surgery, rheumatology |
Osteoarthritis (OA) also known as degenerative arthritis or degenerative joint disease or osteoarthrosis, is a group of mechanical abnormalities involving degradation of joints,[1] including articular cartilage and subchondral bone. Symptoms may include joint pain, tenderness, stiffness, locking, and sometimes an effusion. A variety of causes—hereditary, developmental, metabolic, and mechanical deficits—may initiate processes leading to loss of cartilage. When bone surfaces become less well protected by cartilage, bone may be exposed and damaged. As a result of decreased movement secondary to pain, regional muscles may atrophy, and ligaments may become more lax.[2]
Treatment generally involves a combination of exercise, lifestyle modification, and analgesics. If pain becomes debilitating, joint replacement surgery may be used to improve the quality of life. OA is the most common form of arthritis,[2] and the leading cause of chronic disability in the United States.[3] It affects about 8 million people in the United Kingdom and nearly 27 million people in the United States.[4]
Signs and symptoms

The main symptom is pain, causing loss of ability and often stiffness. "Pain" is generally described as a sharp ache, or a burning sensation in the associate muscles and tendons. OA can cause a crackling noise (called "crepitus") when the affected joint is moved or touched, and patients may experience muscle spasm and contractions in the tendons. Occasionally, the joints may also be filled with fluid. Humid and cold weather increases the pain in many patients.[5][6]
OA commonly affects the hands, feet, spine, and the large weight bearing joints, such as the hips and knees, although in theory, any joint in the body can be affected. As OA progresses, the affected joints appear larger, are stiff and painful, and usually feel better with gentle use but worse with excessive or prolonged use, thus distinguishing it from rheumatoid arthritis.
In smaller joints, such as at the fingers, hard bony enlargements, called Heberden's nodes (on the distal interphalangeal joints) and/or Bouchard's nodes (on the proximal interphalangeal joints), may form, and though they are not necessarily painful, they do limit the movement of the fingers significantly. OA at the toes leads to the formation of bunions, rendering them red or swollen. Some people notice these physical changes before they experience any pain.
OA is the most common cause of joint effusion, sometimes called water on the knee in lay terms, an accumulation of excess fluid in or around the knee joint.[7]
Causes
Some investigators believe that mechanical stress on joints underlies all OA, with many and varied sources of mechanical stress, including misalignments of bones caused by congenital or pathogenic causes; mechanical injury; overweight; loss of strength in muscles supporting joints; and impairment of peripheral nerves, leading to sudden or uncoordinated movements that overstress joints.[8] However exercise, including running in the absence of injury, has not been found to increase one's risk of developing OA.[9] Nor has cracking one's knuckles been found to play a role.[10]
Primary

Primary OA is a chronic degenerative disorder related to but not caused by aging, as there are people well into their nineties who have no clinical or functional signs of the disease. As a person ages, the water content of the cartilage decreases[11][better source needed][ as a result of a reduced proteoglycan content, thus causing the cartilage to be less resilient. The water content of healthy cartilage is finely balanced by compressive force driving water out & swelling pressure drawing water in.[12] Collagen fibres exert the compressive force, whereas the Gibbs-Donnan effect & cartilage proteoglycans create osmotic pressure which tends to draw water in.[12] However during onset of OA there is an increase in cartilage water content. [13][14][15][16][17] This increase occurs because whilst there is an overall loss of proteoglycans,[14][18] it is outweighed by a loss of collagen.[12][18] Without the protective effects of the proteoglycans, the collagen fibers of the cartilage can become susceptible to degradation and thus exacerbate the degeneration. Inflammation of the surrounding joint capsule can also occur, though often mild (compared to what occurs in rheumatoid arthritis). This can happen as breakdown products from the cartilage are released into the synovial space, and the cells lining the joint attempt to remove them. New bone outgrowths, called "spurs" or osteophytes, can form on the margins of the joints, possibly in an attempt to improve the congruence of the articular cartilage surfaces. These bone changes, together with the inflammation, can be both painful and debilitating.
A number of studies have shown that there is a greater prevalence of the disease among siblings and especially identical twins, indicating a hereditary basis.[19] Although a single factor is not generally sufficient to cause the disease, about half of the variation in susceptibility has been assigned to genetic factors.[20]
The development of OA is correlated with a history of previous joint injury and with obesity, especially with respect to knees.[21] Since the correlation with obesity has been observed not only for knees but also for non-weight bearing joints and the loss of body fat is more closely related to symptom relief than the loss of body weight, it has been suggested that there may be a metabolic link to body fat as opposed to just mechanical loading.[22]
Changes in sex hormone levels may play a role in the development of OA as it is more prevalent among post-menopausal women than among men of the same age.[23][24] A study of mice found natural female hormones to be protective while injections of the male hormone Dihydrotestosterone reduced protection.[25]
Secondary
This type of OA is caused by other factors but the resulting pathology is the same as for primary OA:
- Alkaptonuria
- Congenital disorders of joints
- Diabetes
- Ehlers-Danlos Syndrome
- Hemochromatosis and Wilson's disease
- Inflammatory diseases (such as Perthes' disease), (Lyme disease), and all chronic forms of arthritis (e.g. costochondritis, gout, and rheumatoid arthritis). In gout, uric acid crystals cause the cartilage to degenerate at a faster pace.
- Injury to joints or ligaments (such as the ACL), as a result of an accident or orthopedic operations.
- Ligamentous deterioration or instability may be a factor.
- Marfan syndrome
- Obesity
- Septic arthritis (infection of a joint)
Diagnosis
Diagnosis is made with reasonable certainty based on history and clinical examination.[26][27] X-rays may confirm the diagnosis. The typical changes seen on X-ray include: joint space narrowing, subchondral sclerosis (increased bone formation around the joint), subchondral cyst formation, and osteophytes.[28] Plain films may not correlate with the findings on physical examination or with the degree of pain.[29] Usually other imaging techniques are not necessary to clinically diagnose OA.
In 1990, the American College of Rheumatology, using data from a multi-center study, developed a set of criteria for the diagnosis of hand OA based on hard tissue enlargement and swelling of certain joints.[30] These criteria were found to be 92% sensitive and 98% specific for hand OA versus other entities such as rheumatoid arthritis and spondyloarthropathies.[31]
Related pathologies whose names may be confused with OA include pseudo-arthrosis. This is derived from the Greek words pseudo, meaning "false", and arthrosis, meaning "joint." Radiographic diagnosis results in diagnosis of a fracture within a joint, which is not to be confused with OA which is a degenerative pathology affecting a high incidence of distal phalangeal joints of female patients. A polished ivory-like appearance may also develop on the bones of the affected joints, reflecting a change called eburnation.[32]
-
Damaged cartilage in gross pathological specimen from sows. (a) cartilage erosion (b)cartilage ulceration (c)cartilage repair (d)osteophyte (bone spur) formation.
-
Histopathology of osteoarthrosis of a knee joint in an elderly female.
-
Severe osteoarthritis and osteopenia of the carpal joint and 1st carpometacarpel joint.
Classification
OA can be classified into either primary or secondary depending on whether or not there is an identifiable underlying cause.
Both primary generalized nodal OA and erosive OA (EOA. also called inflammatory OA) are sub-sets of primary OA. EOA is a much less common, and more aggressive inflammatory form of OA which often affects the distal interphalangeal joints and has characteristic changes on x-ray.
Management
Lifestyle modification (such as weight loss and exercise) and analgesics are the mainstay of treatment. Acetaminophen / paracetamol is used first line and NSAIDs are only recommended as add on therapy if pain relief is not sufficient.[33] This is due to the relative greater safety of acetaminophen.[33]
Lifestyle modification
For overweight people, weight loss may be an important factor. Patient education has been shown to be helpful in the self-management of arthritis. It decreases pain, improves function, reduces stiffness and fatigue, and reduces medical usage.[34] A meta-analysis has shown patient education can provide on average 20% more pain relief when compared to NSAIDs alone in patients with hip OA.[34]
Physical measures
For most people with OA, graded exercise should be the mainstay of their self-management. Moderate exercise leads to improved functioning and decreased pain in people with OA of the knee.[9][34] While there is some evidence for certain physical therapies evidence for the combined program is limited.[35]
There is sufficient evidence to indicate that physical interventions can reduce pain and improve function.[36] There is some evidence that manual therapy is more effective than exercise for the treatment of hip OA, however this evidence could be considered to be inconclusive.[37] Functional, gait, and balance training has been recommended to address impairments of proprioception, balance, and strength in individuals with lower extremity arthritis as these can contribute to higher falls in older individuals.[38]
Orthotics
The use of orthoses (commonly referred to as splints, braces or insoles as applicable) can reduce the symptoms of OA at various joints. In the lower limb, orthoses are used for the foot and ankle[39] and knee.[40] In the upper limb, splinting of the base of the thumb leads to improvements after one year.[41]
Medication
- Analgesics
Paracetamol (INN; acetaminophen is the USAN) is the first line treatment for OA.[33][42] For mild to moderate symptoms effectiveness is similar to non-steroidal anti-inflammatory drugs (NSAIDs), though for more severe symptoms NSAIDs may be more effective.[33] NSAIDs such as ibuprofen while more effective in severe cases are associated with greater side effects such as gastrointestinal bleeding.[33] Another class of NSAIDs, COX-2 selective inhibitors (such as celecoxib) are equally effective to NSAIDs with lower rates of adverse gastrointestinal effects but higher rates of cardiovascular disease such as myocardial infarction.[43] They are also much more expensive. There are several NSAIDs available for topical use including diclofenac. They have fewer systemic side-effects and at least some therapeutic effect.[44] While opioid analgesics such as morphine and fentanyl improve pain, this benefit is outweighed by frequent adverse events and thus they should not routinely be used.[45]
- Other
Oral steroids are not recommended in the treatment of OA because of their modest benefit and high rate of adverse effects. Injection of glucocorticoids (such as hydrocortisone) leads to short term pain relief that may last between a few weeks and a few months.[46] Topical capsaicin and joint injections of hyaluronic acid have not been found to lead to significant improvement.[44][47] Hyaluronic acid injects have been associated with significant harm.[47]
Surgery
If disability is significant and the above management is ineffective, joint replacement surgery or resurfacing may be recommended. Evidence supports joint replacement for both knees and hips.[48] For the knee it improves both pain and functioning.[49] Arthroscopic surgical intervention for OA of the knee however has been found to be no better than placebo at relieving symptoms.[50]
Alternative medicine
The following show promise as treatments for OA avocado/soybean unsaponifiables[51], boswellic acid[52], cat's claw[53], curcumin[54], chondroitin[55][56], Devil's claw[57], glucosamine sulfate[58] , S-Adenosyl methionine[59][60] and TENS.[61]
- Acupuncture
A Cochrane review found that while acupuncture leads to a statistically significant improvement in pain relief, this improvement is small and may be of questionable clinical significance. Waiting list-controlled trials for peripheral joint OA do show clinically relevant benefits, but these may be due to placebo effects.[62] Acupuncture does not seem to produce long-term benefits.[63]
- Glucosamine
Controversy surrounding glucosamine may be due to including the ineffective hydrochloride and the effective sulfate preperations of glucosamine as well as different treatment protocols and preperations.[64].[65] A 2010 meta-analysis has found that it is no better than placebo.[66] Glucosamine sulfate is an effective treatment[67][68][69] The Osteoarthritis Research Society International (OARSI) recommends that glucosamine be discontinued if no effect is observed after six months.[70]
Epidemiology
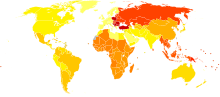
OA affects nearly 27 million people in the United States, accounting for 25% of visits to primary care physicians, and half of all NSAID prescriptions. It is estimated that 80% of the population have radiographic evidence of OA by age 65, although only 60% of those will have symptoms.[72] In the United States, hospitalizations for OA increased from 322,000 in 1993 to 735,000 in 2006.[73]
Globally OA causes moderate to severe disability in 43.4 million people as of 2004.[74]
Etymology
OA is derived from the Greek word part osteo-, meaning "of the bone", combined with arthritis: arthr-, meaning "joint", and -itis, the meaning of which has come to be associated with inflammation. The -itis of OA could be considered misleading as inflammation is not a conspicuous feature. Some clinicians refer to this condition as osteoarthosis to signify the lack of inflammatory response.
History
Evidence for OA found in the fossil record is studied by paleopathologists, specialists in ancient disease and injury. OA has been reported in fossils of the large carnivorous dinosaur Allosaurus fragilis.[75]
Research
There are ongoing efforts to determine if there are agents that modify outcomes in OA. Sprifermin is one candidate drug. There is also tentative evidence that strontium ranelate may decrease degeneration in OA and improve outcomes.[76][77]
References
- ^ "osteoarthritis" at Dorland's Medical Dictionary
- ^ a b Conaghan, Phillip. "Osteoarthritis — National clinical guideline for care and management in adults" (PDF). Retrieved 2008-04-29.
- ^ Centers for Disease Control and Prevention (CDC) (2001). "Prevalence of disabilities and associated health conditions among adults—United States, 1999". MMWR Morb Mortal Wkly Rep. 50 (7): 120–5. PMID 11393491.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Van Manen, MD; Nace, J; Mont, MA (2012). "Management of primary knee osteoarthritis and indications for total knee arthroplasty for general practitioners". The Journal of the American Osteopathic Association. 112 (11): 709–715. PMID 23139341.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ McAlindon T., Formica M., Schmid C.H., Fletcher J. (2007). "Changes in barometric pressure and ambient temperature influence osteoarthritis pain". The American Journal of Medicine. 120 (5): 429–434. doi:10.1016/j.amjmed.2006.07.036. PMID 17466654.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ MedlinePlus Encyclopedia: Osteoarthritis
- ^ Water on the knee, MayoClinic.com
- ^ Brandt KD, Dieppe P, Radin E (2009). "Etiopathogenesis of osteoarthritis". Med. Clin. North Am. 93 (1): 1–24, xv. doi:10.1016/j.mcna.2008.08.009. PMID 19059018.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ a b Bosomworth NJ (2009). "Exercise and knee osteoarthritis: benefit or hazard?". Can Fam Physician. 55 (9): 871–8. PMC 2743580. PMID 19752252.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Deweber, K (Mar–Apr 2011). "Knuckle cracking and hand osteoarthritis". Journal of the American Board of Family Medicine : JABFM. 24 (2): 169–74. doi:10.3122/jabfm.2011.02.100156. PMID 21383216.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help)CS1 maint: date format (link) - ^ Simon, H (2005-05-08). "Osteoarthritis". University of Maryland Medical Center. Retrieved 2009-04-25.
{{cite web}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ a b c Template:Cite DOI
- ^ Template:Cite DOI
- ^ a b Template:Cite PMID
- ^ Template:Cite DOI
- ^ Template:Cite PMID
- ^ Template:Cite PMID
- ^ a b Template:Cite DOI
- ^ Valdes AM, Spector TD (2008). "The contribution of genes to osteoarthritis". Rheum Dis Clin North Am. 34 (3): 581–603. doi:10.1016/j.rdc.2008.04.008. PMID 18687274.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Spector TD, MacGregor AJ (2004). "Risk factors for osteoarthritis: genetics". OsteoArthritis and Cartilage. 12: S39–44. doi:10.1016/j.joca.2003.09.005. PMID 14698640.
{{cite journal}}: Cite has empty unknown parameter:|month=(help) - ^ Coggon D, Reading I (2001). "Knee osteoarthritis and obesity". International Journal of Obesity Related Metabolic Disorders. 25 (5): 622–627. doi:10.1038/sj.ijo.0801585. PMID 11360143.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ P Pottie, N Presle (2006). "Obesity and osteoarthritis: more complex than predicted!". Annals of the Rheumatic Diseases. 65 (11): 1403–1405. doi:10.1136/ard.2006.061994. PMC 1798356. PMID 17038451.
{{cite journal}}: Cite has empty unknown parameter:|month=(help) - ^ Linn, Sarah; Murtaugh, Bryan; Casey, Ellen (2012). "Role of Sex Hormones in the Development of Osteoarthritis". Physical Medicine and Rehabilitation. 4 (5): 169–173. doi:10.1016/j.pmrj.2012.01.013.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Tanamas, SK; Wijethilake, Pushpika; Wluka, Anita E.; Davies-Tuck, Miranda L.; Urquhart, Donna M.; Wang, Yuanyuan; Cicuttini, Flavia M. (2011). "Sex hormones and structural changes in osteoarthritis: a systematic review". Maturitas. 69 (2): 141–156. doi:10.1016/j.maturitas.2011.03.019. PMID 21481553.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Ma, H.L.; Blanchet, T.J.; Peluso, D.; Hopkins, B.; Morris, E.A.; Glasson, S.S. (2007). "Osteoarthritis severity is sex dependent in a surgical mouse model". OsteoArthritis and Cartilage. 15 (6): 695–700. doi:10.1016/j.joca.2006.11.005. PMID 17207643.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Zhang W; Doherty M; Peat G; et al. (2010). "EULAR evidence-based recommendations for the diagnosis of knee osteoarthritis". Ann. Rheum. Dis. 69 (3): 483–9. doi:10.1136/ard.2009.113100. PMID 19762361.
{{cite journal}}: Unknown parameter|author-separator=ignored (help); Unknown parameter|month=ignored (help) - ^ Bierma-Zeinstra SM, Oster JD, Bernsen RM, Verhaar JA, Ginai AZ, Bohnen AM (2002). "Joint space narrowing and relationship with symptoms and signs in adults consulting for hip pain in primary care". J. Rheumatol. 29 (8): 1713–8. PMID 12180735.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Osteoarthritis (OA): Joint Disorders at The Merck Manual of Diagnosis and Therapy Professional Edition
- ^ Phillips CR, Brasington RD (2010). "Osteoarthritis treatment update: Are NSAIDs still in the picture?". Journal of Musculoskeletal Medicine. 27 (2).
- ^ Kalunian, Kenneth C (2013). "Patient information: Osteoarthritis symptoms and diagnosis (Beyond the Basics)". UpToDate. Retrieved 15 February 2013.
- ^ Altman R; Alarcón G; Appelrouth D; et al. (1990). "The American College of Rheumatology criteria for the classification and reporting of osteoarthritis of the hand". Arthritis Rheum. 33 (11): 1601–10. doi:10.1002/art.1780331101. PMID 2242058.
{{cite journal}}: Unknown parameter|author-separator=ignored (help) - ^ Neil Vasan; Le, Tao; Bhushan, Vikas (2010). First Aid for the USMLE Step 1, 2010 (First Aid USMLE). McGraw-Hill Medical. p. 378. ISBN 0-07-163340-5.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ^ a b c d e Flood J (2010). "The role of acetaminophen in the treatment of osteoarthritis". Am J Manag Care. 16 (Suppl Management): S48–54. PMID 20297877.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ a b c Cibulka MT, White DM, Woehrle J; et al. (2009). "Hip pain and mobility deficits—hip osteoarthritis: clinical practice guidelines linked to the international classification of functioning, disability, and health from the orthopaedic section of the American Physical Therapy Association". J Orthop Sports Phys Ther. 39 (4): A1–25. doi:10.2519/jospt.2009.0301. PMID 19352008.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Wang, SY (2012 Nov 6). "Physical therapy interventions for knee pain secondary to osteoarthritis: a systematic review". Annals of internal medicine. 157 (9): 632–44. doi:10.7326/0003-4819-157-9-201211060-00007. PMID 23128863.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Page CJ, Hinman RS, Bennell KL (2011). "Physiotherapy management of knee osteoarthritis". Int J Rheum Dis. 14 (2): 145–152. doi:10.1111/j.1756-185X.2011.01612.x. PMID 21518313.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ French HP, Brennan A, White B, Cusack T (2011). "Manual therapy for osteoarthritis of the hip or knee — a systematic review". Man Ther. 16 (2): 109–117. doi:10.1016/j.math.2010.10.011. PMID 21146444.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Sturnieks DL, Tiedemann A, Chapman K, Munro B, Murray SM, Lord SR (2004). "Physiological risk factors for falls in older people with lower limb arthritis". J. Rheumatol. 31 (11): 2272–9. PMID 15517643.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ http://www.japmaonline.org/content/82/3/136.short
- ^ http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD004020.pub2/pdf/standard
- ^ Rannou F, Dimet J, Boutron I; et al. (2009). "Splint for base-of-thumb osteoarthritis: a randomized trial". Ann. Intern. Med. 150 (10): 661–9. doi:10.7326/0003-4819-150-10-200905190-00003. PMID 19451573.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Zhang W; Moskowitz RW; Nuki G; et al. (2007). "OARSI recommendations for the management of hip and knee osteoarthritis, part I: critical appraisal of existing treatment guidelines and systematic review of current research evidence". Osteoarthr. Cartil. 15 (9): 981–1000. doi:10.1016/j.joca.2007.06.014. PMID 17719803.
{{cite journal}}: Unknown parameter|author-separator=ignored (help); Unknown parameter|month=ignored (help) - ^ Chen, YF (April 2008). "Cyclooxygenase-2 selective non-steroidal anti-inflammatory drugs (etodolac, meloxicam, celecoxib, rofecoxib, etoricoxib, valdecoxib and lumiracoxib) for osteoarthritis and rheumatoid arthritis: a systematic review and economic evaluation". Health technology assessment. 12 (11): 1–278, iii. PMID 18405470.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ a b Altman R, Barkin RL (2009). "Topical therapy for osteoarthritis: clinical and pharmacologic perspectives". Postgrad Med. 121 (2): 139–47. doi:10.3810/pgm.2009.03.1986. PMID 19332972.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Nüesch E, Rutjes AW, Husni E, Welch V, Jüni P (2009). Nüesch, Eveline (ed.). "Oral or transdermal opioids for osteoarthritis of the knee or hip". Cochrane Database Syst Rev (4): CD003115. doi:10.1002/14651858.CD003115.pub3. PMID 19821302.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Arroll B, Goodyear-Smith F (2004). "Corticosteroid injections for osteoarthritis of the knee: meta-analysis". BMJ. 328 (7444): 869. doi:10.1136/bmj.38039.573970.7C. PMC 387479. PMID 15039276.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ a b Rutjes AW, Jüni P, da Costa BR, Trelle S, Nüesch E, Reichenbach S (2012). "Viscosupplementation for osteoarthritis of the knee: a systematic review and meta-analysis". Ann. Intern. Med. 157 (3): 180–91. doi:10.7326/0003-4819-157-3-201208070-00473. PMID 22868835.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Santaguida, PL (December 2008). "Patient characteristics affecting the prognosis of total hip and knee joint arthroplasty: a systematic review". Canadian journal of surgery. Journal canadien de chirurgie. 51 (6): 428–36. PMC 2592576. PMID 19057730.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Carr, AJ (7 April 2012). "Knee replacement". Lancet. 379 (9823): 1331–40. doi:10.1016/S0140-6736(11)60752-6. PMID 22398175.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Moseley JB; O'Malley K; Petersen NJ; et al. (2002). "A controlled trial of arthroscopic surgery for osteoarthritis of the knee is proven to bring an improvement lasting for about two years". The New England Journal of Medicine. 347 (2): 81–8. doi:10.1056/NEJMoa013259. PMID 12110735.
{{cite journal}}: Unknown parameter|author-separator=ignored (help) - ^ Pirotta, M (2010 Sep). "Arthritis disease - the use of complementary therapies". Australian family physician. 39 (9): 638–40. PMID 20877766.
{{cite journal}}: Check date values in:|date=(help) - ^ Rosenbaum, CC (2010 Mar-Apr). "Antioxidants and antiinflammatory dietary supplements for osteoarthritis and rheumatoid arthritis". Alternative therapies in health and medicine. 16 (2): 32–40. PMID 21553931.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ . PMID 20232616.
{{cite journal}}: Cite journal requires|journal=(help); Missing or empty|title=(help) - ^ . PMID 19836480.
{{cite journal}}: Cite journal requires|journal=(help); Missing or empty|title=(help) - ^ Pirotta, M (2010 Sep). "Arthritis disease - the use of complementary therapies". Australian family physician. 39 (9): 638–40. PMID 20877766.
{{cite journal}}: Check date values in:|date=(help) - ^ Schneider, Heinz (25 July 2012). "Symptom-Modifying Effect of Chondroitin Sulfate in Knee Osteoarthritis: A Meta-Analysis of Randomized Placebo-Controlled Trials Performed with Structum®". The Open Rheumatology Journal. 6 (1): 183–189. doi:10.2174/1874312901206010183.
- ^ Rosenbaum, CC (2010 Mar-Apr). "Antioxidants and antiinflammatory dietary supplements for osteoarthritis and rheumatoid arthritis". Alternative therapies in health and medicine. 16 (2): 32–40. PMID 17627199.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Rovati, L. C. (8 March 2012). "Crystalline glucosamine sulfate in the management of knee osteoarthritis: efficacy, safety, and pharmacokinetic properties". Therapeutic Advances in Musculoskeletal Disease. 4 (3): 167–180. doi:10.1177/1759720X12437753.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Hardy ML; Coulter I; Morton SC; et al. (2003). "S-adenosyl-L-methionine for treatment of depression, osteoarthritis, and liver disease". Evid Rep Technol Assess (Summ) (64): 1–3. PMID 12899148.
{{cite journal}}: Unknown parameter|author-separator=ignored (help); Unknown parameter|month=ignored (help) - ^ De Silva, V (May 2011). "Evidence for the efficacy of complementary and alternative medicines in the management of osteoarthritis: a systematic review". Rheumatology. 50 (5): 911–20. doi:10.1093/rheumatology/keq379. PMID 21169345.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Ying, KN (2007 Aug). "Pain relief in osteoarthritis and rheumatoid arthritis: TENS". British journal of community nursing. 12 (8): 364–71. PMID 17851302.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Manheimer E; Cheng K; Linde K; et al. (2010). Manheimer, Eric (ed.). "Acupuncture for peripheral joint osteoarthritis". Cochrane Database Syst Rev (1): CD001977. doi:10.1002/14651858.CD001977.pub2. PMC 3169099. PMID 20091527.
{{cite journal}}: Unknown parameter|author-separator=ignored (help) - ^ Wang, S (2008). "Acupuncture Analgesia: II. Clinical Considerations" (PDF). Anesth Analg. 106 (2): 611–21. doi:10.1213/ane.0b013e318160644d. PMID 18227323.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ The effects of Glucosamine Sulphate on OA of the knee joint. BestBets.
- ^ Vlad SC, Lavalley MP, McAlindon TE, Felson DT (2007). "Glucosamine for pain in osteoarthritis: Why do trial results differ?". Arthritis & Rheumatism. 56 (7): 2267–77. doi:10.1002/art.22728. PMID 17599746.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Wandel S, Jüni P, Tendal B; et al. (2010). "Effects of glucosamine, chondroitin, or placebo in patients with [http://www.acumio.com/dealing-osteoarthritis-guide-afflicted-individuals-485.html osteoarthritis] of hip or knee: network meta-analysis". BMJ. 341: c4675. doi:10.1136/bmj.c4675. PMC 2941572. PMID 20847017.
{{cite journal}}: Explicit use of et al. in:|author=(help); External link in|title= - ^ Pirotta, M (2010 Sep). "Arthritis disease - the use of complementary therapies". Australian family physician. 39 (9): 638–40. PMID 20877766.
{{cite journal}}: Check date values in:|date=(help) - ^ Poolsup N, Suthisisang C, Channark P, Kittikulsuth W (2005). "Glucosamine long-term treatment and the progression of knee osteoarthritis: systematic review of randomized controlled trials". The Annals of pharmacotherapy. 39 (6): 1080–7. doi:10.1345/aph.1E576. PMID 15855241.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Black C; Clar C; Henderson R; et al. (2009). "The clinical effectiveness of glucosamine and chondroitin supplements in slowing or arresting progression of osteoarthritis of the knee: a systematic review and economic evaluation". Health Technol Assess. 13 (52): 1–148. doi:10.3310/hta13520. PMID 19903416.
{{cite journal}}: Unknown parameter|author-separator=ignored (help); Unknown parameter|month=ignored (help) - ^ Zhang W; Moskowitz RW; Nuki G; et al. (2008). "OARSI recommendations for the management of hip and knee osteoarthritis, Part II: OARSI evidence-based, expert consensus guidelines" (PDF). Osteoarthr. Cartil. 16 (2): 137–62. doi:10.1016/j.joca.2007.12.013. PMID 18279766.
{{cite journal}}: Unknown parameter|author-separator=ignored (help); Unknown parameter|month=ignored (help) - ^ "WHO Disease and injury country estimates". World Health Organization. 2009. Retrieved Nov. 11, 2009.
{{cite web}}: Check date values in:|accessdate=(help) - ^ Green GA (2001). "Understanding NSAIDs: from aspirin to COX-2". Clin Cornerstone. 3 (5): 50–60. doi:10.1016/S1098-3597(01)90069-9. PMID 11464731.
- ^ Hospitalizations for Osteoarthritis Rising Sharply Newswise, Retrieved on September 4, 2008.
- ^ The global burden of disease : 2004 update.. [Online-Ausg.] ed. Geneva, Switzerland: World Health Organization; 2008. ISBN 9789241563710. p. 35.
- ^ Molnar, R. E., 2001, Theropod paleopathology: a literature survey: In: Mesozoic Vertebrate Life, edited by Tanke, D. H., and Carpenter, K., Indiana University Press, p. 337-363.
- ^ Civjan, Natanya (2012). Chemical Biology: Approaches to Drug Discovery and Development to Targeting Disease. John Wiley & Sons. p. 313. ISBN 9781118437674.
- ^ Bruyère, O (16 December 2008). "Evaluation of symptomatic slow-acting drugs in osteoarthritis using the GRADE system". BMC musculoskeletal disorders. 9: 165. doi:10.1186/1471-2474-9-165. PMC 2627841. PMID 19087296.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help)CS1 maint: unflagged free DOI (link)
External links
- American College of Rheumatology Factsheet on OA
- Osteoarthritis The Arthritis Foundation






