Diabetes: Difference between revisions
| [pending revision] | [pending revision] |
UCSFrb1983 (talk | contribs) →Pathophysiology: Reformatted and simplified pathophysiology section |
UCSFrb1983 (talk | contribs) →Pathophysiology: Added references to pathophysiology section |
||
| Line 157: | Line 157: | ||
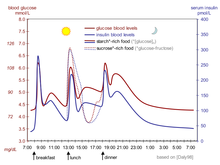
[[File:Suckale08 fig3 glucose insulin day.png|thumb|The fluctuation of blood sugar (red) and the sugar-lowering hormone [[insulin]] (blue) in humans during the course of a day with three meals - one of the effects of a [[sucrose|sugar]]-rich vs a [[starch]]-rich meal is highlighted.]] |
[[File:Suckale08 fig3 glucose insulin day.png|thumb|The fluctuation of blood sugar (red) and the sugar-lowering hormone [[insulin]] (blue) in humans during the course of a day with three meals - one of the effects of a [[sucrose|sugar]]-rich vs a [[starch]]-rich meal is highlighted.]] |
||
[[File:Glucose-insulin-release.png|thumb|Mechanism of insulin release in normal pancreatic beta cells - insulin production is more or less constant within the beta cells. Its release is triggered by food, chiefly food containing absorbable glucose.]] |
[[File:Glucose-insulin-release.png|thumb|Mechanism of insulin release in normal pancreatic beta cells - insulin production is more or less constant within the beta cells. Its release is triggered by food, chiefly food containing absorbable glucose.]] |
||
[[Insulin]] is the principal hormone that regulates the uptake of [[glucose]] from the blood into most cells of the body, especially liver, muscle, and adipose tissue. Therefore, deficiency of insulin or the insensitivity of its [[Receptor (biochemistry)|receptors]] plays a central role in all forms of diabetes mellitus. |
[[Insulin]] is the principal hormone that regulates the uptake of [[glucose]] from the blood into most cells of the body, especially liver, muscle, and adipose tissue. Therefore, deficiency of insulin or the insensitivity of its [[Receptor (biochemistry)|receptors]] plays a central role in all forms of diabetes mellitus.<ref name=":0">Mantzoros C, Serdy, S. Insulin Action. In: UpToDate, Nathan D (Ed), UpToDate, Waltham, MA. (Accessed on April 23, 2014).</ref> |
||
The body obtains [[glucose]] from three main places: the intestinal absorption of food, the breakdown of [[glycogen]], the storage form of glucose found in the liver, and [[gluconeogenesis]], the generation of glucose from non-carbohydrate substrates in the body. Insulin plays a critical role in balancing glucose levels in the body. Insulin can inhibit the breakdown of [[glycogen]] or the process of [[gluconeogenesis]], it can transport glucose into fat and muscle cells, and it can stimulate the storage of glucose in the form of [[glycogen]]. |
The body obtains [[glucose]] from three main places: the intestinal absorption of food, the breakdown of [[glycogen]], the storage form of glucose found in the liver, and [[gluconeogenesis]], the generation of glucose from non-carbohydrate substrates in the body.<ref name=":0" /> Insulin plays a critical role in balancing glucose levels in the body. Insulin can inhibit the breakdown of [[glycogen]] or the process of [[gluconeogenesis]], it can transport glucose into fat and muscle cells, and it can stimulate the storage of glucose in the form of [[glycogen]].<ref name=":0" /> |
||
[[Insulin]] is released into the blood by [[beta cells]] (β-cells), found in the [[islets of Langerhans]] in the pancreas, in response to rising levels of blood glucose, typically after eating. Insulin is used by about two-thirds of the body's cells to absorb glucose from the blood for use as fuel, for conversion to other needed molecules, or for storage. Lower glucose levels result in decreased insulin release from the [[beta cells]] and in the breakdown of [[glycogen]] to [[glucose]]. This process is mainly controlled by the hormone [[glucagon]], which acts in the opposite manner to insulin. |
[[Insulin]] is released into the blood by [[beta cells]] (β-cells), found in the [[islets of Langerhans]] in the pancreas, in response to rising levels of blood glucose, typically after eating.<ref name=":0" /> Insulin is used by about two-thirds of the body's cells to absorb glucose from the blood for use as fuel, for conversion to other needed molecules, or for storage. Lower glucose levels result in decreased insulin release from the [[beta cells]] and in the breakdown of [[glycogen]] to [[glucose]]. This process is mainly controlled by the hormone [[glucagon]], which acts in the opposite manner to insulin.<ref>Chapter 24. Endocrine Functions of the Pancreas & Regulation of Carbohydrate Metabolism. In: Barrett KE, Boitano S, Barman SM, Brooks HL. eds. ''<em>Ganong's Review of Medical Physiology, 24e</em>. ''New York, NY: McGraw-Hill; 2012.http://accessmedicine.mhmedical.com/content.aspx?bookid=393&Sectionid=39736766. Accessed April 23, 2014.</ref> |
||
If the amount of [[insulin]] available is insufficient, if cells respond poorly to the effects of insulin ([[insulin insensitivity]] or [[insulin resistance]]), or if the insulin itself is defective, then glucose will not be absorbed properly by the body cells that require it, and it will not be stored appropriately in the liver and muscles. The net effect is persistently high levels of blood glucose, poor protein synthesis, and other metabolic derangements, such as [[acidosis]]. |
If the amount of [[insulin]] available is insufficient, if cells respond poorly to the effects of insulin ([[insulin insensitivity]] or [[insulin resistance]]), or if the insulin itself is defective, then glucose will not be absorbed properly by the body cells that require it, and it will not be stored appropriately in the liver and muscles. The net effect is persistently high levels of blood glucose, poor protein synthesis, and other metabolic derangements, such as [[acidosis]].<ref name=":0" /> |
||
When the glucose concentration in the blood remains high over time, the [[kidneys]] will reach a threshold of [[reabsorption]], and glucose will be excreted in the [[urine]] ([[glycosuria]]). This increases the [[osmotic pressure]] of the urine and inhibits reabsorption of water by the kidney, resulting in increased urine production ([[polyuria]]) and increased fluid loss. Lost blood volume will be replaced osmotically from water held in body cells and other body compartments, causing [[dehydration]] and increased thirst ([[polydipsia]]). |
When the glucose concentration in the blood remains high over time, the [[kidneys]] will reach a threshold of [[reabsorption]], and glucose will be excreted in the [[urine]] ([[glycosuria]]).<ref>Bender DA, Mayes PA. Chapter 20. Gluconeogenesis & the Control of Blood Glucose. In: Murray RK, Bender DA, Botham KM, Kennelly PJ, Rodwell VW, Weil P. eds. ''<em>Harper's Illustrated Biochemistry, 29e</em>. ''New York, NY: McGraw-Hill; 2012.http://accessmedicine.mhmedical.com/content.aspx?bookid=389&Sectionid=40142496. Accessed April 23, 2014.</ref> This increases the [[osmotic pressure]] of the urine and inhibits reabsorption of water by the kidney, resulting in increased urine production ([[polyuria]]) and increased fluid loss. Lost blood volume will be replaced osmotically from water held in body cells and other body compartments, causing [[dehydration]] and increased thirst ([[polydipsia]]).<ref>Masharani U, German MS. Chapter 17. Pancreatic Hormones and Diabetes Mellitus. In: Gardner DG, Shoback D. eds. ''<em>Greenspan’s Basic & Clinical Endocrinology, 9e</em>. ''New York, NY: McGraw-Hill; 2011.http://accessmedicine.mhmedical.com/content.aspx?bookid=380&Sectionid=39744057. Accessed April 23, 2014.</ref> |
||
==Diagnosis== |
==Diagnosis== |
||
Revision as of 21:28, 23 April 2014
| Diabetes | |
|---|---|
| Specialty | Diabetology, endocrinology |
Diabetes mellitus (DM) or simply diabetes, is a group of metabolic diseases in which a person has high blood sugar.[2] This high blood sugar produces the symptoms of frequent urination, increased thirst, and increased hunger. Untreated, diabetes can cause many complications. Acute complications include diabetic ketoacidosis and nonketotic hyperosmolar coma. Serious long-term complications include heart disease, kidney failure, and damage to the eyes.
Diabetes is due to either the pancreas not producing enough insulin, or because cells of the body do not respond properly to the insulin that is produced.[3] There are three main types of diabetes mellitus:[4]
- Type 1 DM results from the body's failure to produce insulin. This form was previously referred to as "insulin-dependent diabetes mellitus" (IDDM) or "juvenile diabetes".[4]
- Type 2 DM results from insulin resistance, a condition in which cells fail to use insulin properly, sometimes also with an absolute insulin deficiency. This form was previously referred to as non insulin-dependent diabetes mellitus (NIDDM) or "adult-onset diabetes".
- Gestational diabetes, is the third main form and occurs when pregnant women without a previous diagnosis of diabetes develop a high blood glucose level.
Prevention and treatment often involve a healthy diet, physical exercise, not using tobacco, and being a normal body weight.[4] Blood pressure control and proper foot care are also important for people with the disease.[4] Type 1 diabetes must be managed with insulin injections.[4] Type 2 diabetes may be treated with medications with or without insulin.[4] Insulin and some oral medications can cause low blood sugar, which can be dangerous. A pancreas transplant is occasionally considered for people with type 1 diabetes who have severe complications of their disease, including end stage renal disease requiring kidney transplantation.[5] Gestational diabetes usually resolves after the birth of the baby.
Globally, as of 2013, an estimated 382 million people have diabetes worldwide, with type 2 diabetes making up about 90% of the cases.[6][7] This is equal to 3.3% of the population, with equal rates in both women and men.[8] In 2011 diabetes resulted in 1.4 million deaths worldwide, making it the 8th leading cause of death.[4] The number of people with diabetes is expected to rise to 592 million by 2035.[7]
Signs and symptoms

The classic symptoms of untreated diabetes are weight loss, polyuria (frequent urination), polydipsia (increased thirst), and polyphagia (increased hunger).[9] Symptoms may develop rapidly (weeks or months) in type 1 diabetes, while they usually develop much more slowly and may be subtle or absent in type 2 diabetes.
Prolonged high blood glucose can cause glucose absorption in the lens of the eye, which leads to changes in its shape, resulting in vision changes. Blurred vision is a common complaint leading to a diabetes diagnosis. A number of skin rashes that can occur in diabetes are collectively known as diabetic dermadromes.
Diabetic emergencies
People (usually with type 1 diabetes) may also experience episodes of diabetic ketoacidosis, a type of metabolic problems characterized by nausea, vomiting and abdominal pain, the smell of acetone on the breath, deep breathing known as Kussmaul breathing, and in severe cases a decreased level of consciousness.[10]
A rare but equally severe possibility is hyperosmolar nonketotic state, which is more common in type 2 diabetes and is mainly the result of dehydration.[10]
Complications
All forms of diabetes increase the risk of long-term complications. These complications typically develop after many years (10–20), but may be the first signs or symptoms in those who have otherwise not received a diagnosis before that time.
The major long-term complications relate to damage to blood vessels. These complications can be grouped into microvascular disease (damage to small blood vessels) and macrovascular disease (damage to larger arteries).
The primary microvascular complications of diabetes include damage to the eyes, kidneys, and nerves.[11] Damage to the eyes, known as diabetic retinopathy, is caused by damage to the blood vessels in the retina of the eye, and can result in gradual vision loss and potentially blindness.[11] Damage to the kidneys, known as diabetic nephropathy, can lead to tissue scarring, urine protein loss, and eventually chronic kidney disease, sometimes requiring dialysis or kidney transplant.[11] Damage to the nerves of the body, known as diabetic neuropathy, is the most common complication of diabetes.[11] The symptoms can include numbness, tingling, pain, and altered pain sensation, which can lead to damage to the skin. Diabetes-related foot problems (such as diabetic foot ulcers) may occur, and can be difficult to treat, occasionally requiring amputation. Additionally, proximal diabetic neuropathy causes painful muscle wasting and weakness.
The primary macrovascular complications of diabetes include coronary artery disease (angina and myocardial infarction), stroke, and peripheral vascular disease. About 75% of deaths in diabetics are due to coronary artery disease.[12]
There is a link between cognitive deficit and diabetes. Compared to those without diabetes, those with the disease have a 1.2 to 1.5-fold greater rate of decline in cognitive function.[13]
Causes
| Feature | Type 1 diabetes | Type 2 diabetes |
|---|---|---|
| Onset | Sudden | Gradual |
| Age at onset | Mostly in children | Mostly in adults |
| Body size | Thin or normal[14] | Often obese |
| Ketoacidosis | Common | Rare |
| Autoantibodies | Usually present | Absent |
| Endogenous insulin | Low or absent | Normal, decreased or increased |
| Concordance in identical twins |
50% | 90% |
| Prevalence | ~10% | ~90% |
Diabetes mellitus is classified into four broad categories: type 1, type 2, gestational diabetes, and "other specific types".[3] The "other specific types" are a collection of a few dozen individual causes.[3] The term "diabetes", without qualification, usually refers to diabetes mellitus.
Type 1
Type 1 diabetes mellitus is characterized by loss of the insulin-producing beta cells of the islets of Langerhans in the pancreas, leading to insulin deficiency. This type can be further classified as immune-mediated or idiopathic. The majority of type 1 diabetes is of the immune-mediated nature, in which a T-cell-mediated autoimmune attack leads to the loss of beta cells and thus insulin.[15] It causes approximately 10% of diabetes mellitus cases in North America and Europe. Most affected people are otherwise healthy and of a healthy weight when onset occurs. Sensitivity and responsiveness to insulin are usually normal, especially in the early stages. Type 1 diabetes can affect children or adults, but was traditionally termed "juvenile diabetes" because a majority of these diabetes cases were in children.
"Brittle" diabetes, also known as unstable diabetes or labile diabetes, is a term that was traditionally used to describe the dramatic and recurrent swings in glucose levels, often occurring for no apparent reason in insulin-dependent diabetes. This term, however, has no biologic basis and should not be used.[16] Still, type 1 diabetes can be accompanied by irregular and unpredictable hyperglycemia, frequently with ketosis, and sometimes with serious hypoglycemia. Other complications include an impaired counterregulatory response to hypoglycemia, infection, gastroparesis (which leads to erratic absorption of dietary carbohydrates), and endocrinopathies (e.g., Addison's disease).[16] These phenomena are believed to occur no more frequently than in 1% to 2% of persons with type 1 diabetes.[17]
Type 1 diabetes is partly inherited, with multiple genes, including certain HLA genotypes, known to influence the risk of diabetes. In genetically susceptible people, the onset of diabetes can be triggered by one or more environmental factors, such as a viral infection or diet. There is some evidence that suggests an association between type 1 diabetes and Coxsackie B4 virus. Unlike type 2 diabetes, the onset of type 1 diabetes is unrelated to lifestyle.
Type 2
Type 2 diabetes mellitus is characterized by insulin resistance, which may be combined with relatively reduced insulin secretion.[3] The defective responsiveness of body tissues to insulin is believed to involve the insulin receptor. However, the specific defects are not known. Diabetes mellitus cases due to a known defect are classified separately. Type 2 diabetes is the most common type.
In the early stage of type 2, the predominant abnormality is reduced insulin sensitivity. At this stage, hyperglycemia can be reversed by a variety of measures and medications that improve insulin sensitivity or reduce glucose production by the liver.
Type 2 diabetes is due primarily to lifestyle factors and genetics.[18] A number of lifestyle factors are known to be important to the development of type 2 diabetes, including obesity (defined by a body mass index of greater than thirty), lack of physical activity, poor diet, stress, and urbanization.[6] Excess body fat is associated with 30% of cases in those of Chinese and Japanese descent, 60-80% of cases in those of European and African descent, and 100% of Pima Indians and Pacific Islanders.[3] Those who are not obese often have a high waist–hip ratio.[3]
Dietary factors also influence the risk of developing type 2 diabetes. Consumption of sugar-sweetened drinks in excess is associated with an increased risk.[19][20] The type of fats in the diet is also important, with saturated fats and trans fatty acids increasing the risk and polyunsaturated and monounsaturated fat decreasing the risk.[18] Eating lots of white rice appears to also play a role in increasing risk.[21] A lack of exercise is believed to cause 7% of cases.[22]
Gestational diabetes
Gestational diabetes mellitus (GDM) resembles type 2 diabetes in several respects, involving a combination of relatively inadequate insulin secretion and responsiveness. It occurs in about 2-10% of all pregnancies and may improve or disappear after delivery.[23] However, after pregnancy approximately 5-10% of women with gestational diabetes are found to have diabetes mellitus, most commonly type 2.[23] Gestational diabetes is fully treatable, but requires careful medical supervision throughout the pregnancy. Management may include dietary changes, blood glucose monitoring, and in some cases insulin may be required.
Though it may be transient, untreated gestational diabetes can damage the health of the fetus or mother. Risks to the baby include macrosomia (high birth weight), congenital cardiac and central nervous system anomalies, and skeletal muscle malformations. Increased fetal insulin may inhibit fetal surfactant production and cause respiratory distress syndrome. Hyperbilirubinemia may result from red blood cell destruction. In severe cases, perinatal death may occur, most commonly as a result of poor placental perfusion due to vascular impairment. Labor induction may be indicated with decreased placental function. A Caesarean section may be performed if there is marked fetal distress or an increased risk of injury associated with macrosomia, such as shoulder dystocia.
Other types
Prediabetes indicates a condition that occurs when a person's blood glucose levels are higher than normal but not high enough for a diagnosis of type 2 DM. Many people destined to develop type 2 DM spend many years in a state of prediabetes.
Latent autoimmune diabetes of adults (LADA) is a condition in which type 1 DM develops in adults. Adults with LADA are frequently initially misdiagnosed as having type 2 DM, based on age rather than etiology.
Some cases of diabetes are caused by the body's tissue receptors not responding to insulin (even when insulin levels are normal, which is what separates it from type 2 diabetes); this form is very uncommon. Genetic mutations (autosomal or mitochondrial) can lead to defects in beta cell function. Abnormal insulin action may also have been genetically determined in some cases. Any disease that causes extensive damage to the pancreas may lead to diabetes (for example, chronic pancreatitis and cystic fibrosis). Diseases associated with excessive secretion of insulin-antagonistic hormones can cause diabetes (which is typically resolved once the hormone excess is removed). Many drugs impair insulin secretion and some toxins damage pancreatic beta cells. The ICD-10 (1992) diagnostic entity, malnutrition-related diabetes mellitus (MRDM or MMDM, ICD-10 code E12), was deprecated by the World Health Organization when the current taxonomy was introduced in 1999.[24]
Other forms of diabetes mellitus include congenital diabetes, which is due to genetic defects of insulin secretion, cystic fibrosis-related diabetes, steroid diabetes induced by high doses of glucocorticoids, and several forms of monogenic diabetes.
The following is a comprehensive list of other causes of diabetes:[25]
|
|
Pathophysiology

Insulin is the principal hormone that regulates the uptake of glucose from the blood into most cells of the body, especially liver, muscle, and adipose tissue. Therefore, deficiency of insulin or the insensitivity of its receptors plays a central role in all forms of diabetes mellitus.[27]
The body obtains glucose from three main places: the intestinal absorption of food, the breakdown of glycogen, the storage form of glucose found in the liver, and gluconeogenesis, the generation of glucose from non-carbohydrate substrates in the body.[27] Insulin plays a critical role in balancing glucose levels in the body. Insulin can inhibit the breakdown of glycogen or the process of gluconeogenesis, it can transport glucose into fat and muscle cells, and it can stimulate the storage of glucose in the form of glycogen.[27]
Insulin is released into the blood by beta cells (β-cells), found in the islets of Langerhans in the pancreas, in response to rising levels of blood glucose, typically after eating.[27] Insulin is used by about two-thirds of the body's cells to absorb glucose from the blood for use as fuel, for conversion to other needed molecules, or for storage. Lower glucose levels result in decreased insulin release from the beta cells and in the breakdown of glycogen to glucose. This process is mainly controlled by the hormone glucagon, which acts in the opposite manner to insulin.[28]
If the amount of insulin available is insufficient, if cells respond poorly to the effects of insulin (insulin insensitivity or insulin resistance), or if the insulin itself is defective, then glucose will not be absorbed properly by the body cells that require it, and it will not be stored appropriately in the liver and muscles. The net effect is persistently high levels of blood glucose, poor protein synthesis, and other metabolic derangements, such as acidosis.[27]
When the glucose concentration in the blood remains high over time, the kidneys will reach a threshold of reabsorption, and glucose will be excreted in the urine (glycosuria).[29] This increases the osmotic pressure of the urine and inhibits reabsorption of water by the kidney, resulting in increased urine production (polyuria) and increased fluid loss. Lost blood volume will be replaced osmotically from water held in body cells and other body compartments, causing dehydration and increased thirst (polydipsia).[30]
Diagnosis
| Condition | 2-hour glucose | Fasting glucose | HbA1c | |||
|---|---|---|---|---|---|---|
| Unit | mmol/L | mg/dL | mmol/L | mg/dL | mmol/mol | DCCT % |
| Normal | < 7.8 | < 140 | < 6.1 | < 110 | < 42 | < 6.0 |
| Impaired fasting glycaemia | < 7.8 | < 140 | 6.1–7.0 | 110–125 | 42–46 | 6.0–6.4 |
| Impaired glucose tolerance | ≥ 7.8 | ≥ 140 | < 7.0 | < 126 | 42–46 | 6.0–6.4 |
| Diabetes mellitus | ≥ 11.1 | ≥ 200 | ≥ 7.0 | ≥ 126 | ≥ 48 | ≥ 6.5 |
Diabetes mellitus is characterized by recurrent or persistent hyperglycemia, and is diagnosed by demonstrating any one of the following:[24]
- Fasting plasma glucose level ≥ 7.0 mmol/l (126 mg/dl)
- Plasma glucose ≥ 11.1 mmol/l (200 mg/dL) two hours after a 75 g oral glucose load as in a glucose tolerance test
- Symptoms of hyperglycemia and casual plasma glucose ≥ 11.1 mmol/l (200 mg/dl)
- Glycated hemoglobin (Hb A1C) ≥ 6.5%.[33]
A positive result, in the absence of unequivocal hyperglycemia, should be confirmed by a repeat of any of the above methods on a different day. It is preferable to measure a fasting glucose level because of the ease of measurement and the considerable time commitment of formal glucose tolerance testing, which takes two hours to complete and offers no prognostic advantage over the fasting test.[34] According to the current definition, two fasting glucose measurements above 126 mg/dl (7.0 mmol/l) is considered diagnostic for diabetes mellitus.
Per the World Health Organization people with fasting glucose levels from 6.1 to 6.9 mmol/l (110 to 125 mg/dl) are considered to have impaired fasting glucose.[35] people with plasma glucose at or above 7.8 mmol/L (140 mg/dL), but not over 11.1 mmol/L (200 mg/dL), two hours after a 75 g oral glucose load are considered to have impaired glucose tolerance. Of these two prediabetic states, the latter in particular is a major risk factor for progression to full-blown diabetes mellitus, as well as cardiovascular disease.[36] The American Diabetes Association since 2003 uses a slightly different range for impaired fasting glucose of 5.6 to 6.9 mmol/l (100 to 125 mg/dl).[37]
Glycated hemoglobin is better than fasting glucose for determining risks of cardiovascular disease and death from any cause.[38]
The rare disease diabetes insipidus has similar symptoms to diabetes mellitus, but without disturbances in the sugar metabolism (insipidus means "without taste" in Latin) and does not involve the same disease mechanisms.
Prevention
There is no known preventive measure for type 1 diabetes.[4] Type 2 diabetes can often be prevented by a person being a normal body weight and physical exercise.[4]
Management
Diabetes mellitus is a chronic disease, for which there is no known cure except in very specific situations. Management concentrates on keeping blood sugar levels as close to normal ("euglycemia") as possible, without causing hypoglycemia. This can usually be accomplished with diet, exercise, and use of appropriate medications (insulin in the case of type 1 diabetes; oral medications, as well as possibly insulin, in type 2 diabetes).
Learning about the disease and actively participating in the treatment is vital for people with diabetes, since the complications of diabetes are far less common and less severe in people who have well-managed blood sugar levels.[39][40] The goal of treatment is an HbA1C level of 6.5%, but should not be lower than that, and may be set higher.[41] Attention is also paid to other health problems that may accelerate the deleterious effects of diabetes. These include smoking, elevated cholesterol levels, obesity, high blood pressure, and lack of regular exercise.[41] Specialised footwear is widely used to reduce the risk of ulceration, or re-ulceration, in at-risk diabetic feet. Evidence for the efficacy of this remains equivocal, however.[42]
Lifestyle
People with diabetes can benefit from education about the disease and treatment, good nutrition to achieve a normal body weight, and sensible exercise, with the goal of keeping both short-term and long-term blood glucose levels within acceptable bounds. In addition, given the associated higher risks of cardiovascular disease, lifestyle modifications are recommended to control blood pressure.[43]
Medications
Metformin is generally recommended as a first line treatment for type 2 diabetes, as there is good evidence that it decreases mortality.[44] Routine use of aspirin, however, has not been found to improve outcomes in uncomplicated diabetes.[45] Angiotensin converting enzyme inhibitors (ACEIs) improve outcomes in those with DM while the similar medications angiotensin receptor blockers (ARBs) do not.[46]
Type 1 diabetes is typically treated with a combinations of regular and NPH insulin, or synthetic insulin analogs. When insulin is used in type 2 diabetes, a long-acting formulation is usually added initially, while continuing oral medications.[44] Doses of insulin are then increased to effect.[44]
Pancreatic transplantation
A pancreas transplant is occasionally considered for people with type 1 diabetes who have severe complications of their disease, including end stage renal disease requiring kidney transplantation.[47]
Support
In countries using a general practitioner system, such as the United Kingdom, care may take place mainly outside hospitals, with hospital-based specialist care used only in case of complications, difficult blood sugar control, or research projects. In other circumstances, general practitioners and specialists share care in a team approach. Home telehealth support can be an effective management technique.[48]
Epidemiology


Globally, as of 2010[update], an estimated 227 to 285 million people had diabetes, with type 2 making up about 90% of the cases.[6][8] This is equal to 3.3% of the population with equal rates in both women and men.[8] In 2011 it resulted in 1.4 million deaths worldwide making it the 8th leading cause of death.[4] This is an increase from 1 million deaths in 2000.[4]
Its rate has increased, and by 2030, this number is estimated to almost double.[49] Diabetes mellitus occurs throughout the world, but is more common (especially type 2) in more developed countries. The greatest increase in rates is, however, expected to occur in Asia and Africa, where most people with diabetes will probably be found by 2030.[49] The increase in rates in developing countries follows the trend of urbanization and lifestyle changes, perhaps most importantly a "Western-style" diet. This has suggested an environmental (i.e., dietary) effect, but there is little understanding of the mechanism(s) at present, though there is much speculation, some of it most compellingly presented.[49]
History
Diabetes was one of the first diseases described,[50] with an Egyptian manuscript from c. 1500 BCE mentioning "too great emptying of the urine".[51] The first described cases are believed to be of type 1 diabetes.[51] Indian physicians around the same time identified the disease and classified it as madhumeha or "honey urine", noting the urine would attract ants.[51] The term "diabetes" or "to pass through" was first used in 230 BCE by the Greek Appollonius of Memphis.[51] The disease was considered rare during the time of the Roman empire, with Galen commenting he had only seen two cases during his career.[51] This is possibly due the diet and life-style of the ancient people, or because the clinical symptoms were observed during the advanced stage of the disease. Galen named the disease "diarrhea of the urine" (diarrhea urinosa). The earliest surviving work with a detailed reference to diabetes is that of Aretaeus of Cappadocia (2nd or early 3rd century CE). He described the symptoms and the course of the disease, which he attributed to the moisture and coldness, reflecting the beliefs of the "Pneumatic School". He hypothesized a correlation of diabetes with other diseases and he discussed differential diagnosis from the snakebite which also provokes excessive thirst. His work remained unknown in the West until the middle of the 16th century when, in 1552, the first Latin edition was published in Venice.[52]
Type 1 and type 2 diabetes were identified as separate conditions for the first time by the Indian physicians Sushruta and Charaka in 400-500 CE with type 1 associated with youth and type 2 with being overweight.[51] The term "mellitus" or "from honey" was added by the Briton John Rolle in the late 1700s to separate the condition from diabetes insipidus, which is also associated with frequent urination.[51] Effective treatment was not developed until the early part of the 20th century, when Canadians Frederick Banting and Charles Herbert Best isolated and purified insulin in 1921 and 1922.[51] This was followed by the development of the long-acting insulin NPH in the 1940s.[51]
Etymology
The word diabetes (/ˌdaɪ.əˈbiːtiːz/ or /ˌdaɪ.əˈbiːt[invalid input: 'ɨ']s/) comes from Latin diabētēs, which in turn comes from Ancient Greek διαβήτης (diabētēs) which literally means "a passer through; a siphon."[53] Ancient Greek physician Aretaeus of Cappadocia (fl. 1st century CE) used that word, with the intended meaning "excessive discharge of urine", as the name for the disease.[54][55] Ultimately, the word comes from Greek διαβαίνειν (diabainein), meaning "to pass through,"[53] which is composed of δια- (dia-), meaning "through" and βαίνειν (bainein), meaning "to go".[54] The word "diabetes" is first recorded in English, in the form diabete, in a medical text written around 1425.
The word mellitus (/m[invalid input: 'ɨ']ˈlaɪtəs/ or /ˈmɛl[invalid input: 'ɨ']təs/) comes from the classical Latin word mellītus, meaning "mellite"[56] (i.e. sweetened with honey;[56] honey-sweet[57]). The Latin word comes from mell-, which comes from mel, meaning "honey";[56][57] sweetness;[57] pleasant thing,[57] and the suffix -ītus,[56] whose meaning is the same as that of the English suffix "-ite".[58] It was Thomas Willis who in 1675 added "mellitus" to the word "diabetes" as a designation for the disease, when he noticed the urine of a diabetic had a sweet taste (glycosuria).[55] This sweet taste had been noticed in urine by the ancient Greeks, Chinese, Egyptians, Indians, and Persians.
Society and culture
The 1989 "St. Vincent Declaration"[59][60] was the result of international efforts to improve the care accorded to those with diabetes. Doing so is important not only in terms of quality of life and life expectancy, but also economically—expenses due to diabetes have been shown to be a major drain on health—and productivity-related resources for healthcare systems and governments.
Several countries established more and less successful national diabetes programmes to improve treatment of the disease.[61]
People with diabetes who have neuropathic symptoms such as numbness or tingling in feet or hands are twice as likely to be unemployed as those without the symptoms.[62]
In 2010, diabetes-related emergency department (ED) visit rates in the United States were higher among people from the lowest income communities (526 per 10,000 population) than from the highest income communities (236 per 10,000 population). Approximately 9.4% of diabetes-related ED visits were for the uninsured.[63]
Naming
The term "type 1 diabetes" has replaced several former terms, including childhood-onset diabetes, juvenile diabetes, and insulin-dependent diabetes mellitus (IDDM). Likewise, the term "type 2 diabetes" has replaced several former terms, including adult-onset diabetes, obesity-related diabetes, and noninsulin-dependent diabetes mellitus (NIDDM). Beyond these two types, there is no agreed-upon standard nomenclature.
Other animals
In animals, diabetes is most commonly encountered in dogs and cats. Middle-aged animals are most commonly affected. Female dogs are twice as likely to be affected as males, while according to some sources, male cats are also more prone than females. In both species, all breeds may be affected, but some small dog breeds are particularly likely to develop diabetes, such as Miniature Poodles.[64] The symptoms may relate to fluid loss and polyuria, but the course may also be insidious. Diabetic animals are more prone to infections. The long-term complications recognised in humans are much rarer in animals. The principles of treatment (weight loss, oral antidiabetics, subcutaneous insulin) and management of emergencies (e.g. ketoacidosis) are similar to those in humans.[64]
Research
Inhaled insulin has been developed.[65] It was however withdrawn due to side effects.[65] There has been further efforts to develop further versions which may soon be FDA approved.[66]
References
- ^ "Diabetes Blue Circle Symbol". International Diabetes Federation. 17 March 2006.
- ^ "Diabetes". World Health Organization. Retrieved 4 April 2014.
- ^ a b c d e f Shoback, edited by David G. Gardner, Dolores (2011). Greenspan's basic & clinical endocrinology (9th ed.). New York: McGraw-Hill Medical. pp. Chapter 17. ISBN 0-07-162243-8.
{{cite book}}:|first=has generic name (help)CS1 maint: multiple names: authors list (link) - ^ a b c d e f g h i j k "Diabetes Fact sheet N°312". WHO. October 2013. Retrieved 25 March 2014. Cite error: The named reference "WHO2013" was defined multiple times with different content (see the help page).
- ^ "Pancreas Transplantation". American Diabetes Association. Retrieved 9 April 2014.
- ^ a b c d Williams textbook of endocrinology (12th ed.). Philadelphia: Elsevier/Saunders. pp. 1371–1435. ISBN 978-1-4377-0324-5.
- ^ a b "International Diabetes Foundation: Diabetes Atlas". Retrieved 4 April 2014. Cite error: The named reference "IDF" was defined multiple times with different content (see the help page).
- ^ a b c Vos, T (Dec 15, 2012). "Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010". Lancet. 380 (9859): 2163–96. PMID 23245607.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Cooke DW, Plotnick L (November 2008). "Type 1 diabetes mellitus in pediatrics". Pediatr Rev. 29 (11): 374–84, quiz 385. doi:10.1542/pir.29-11-374. PMID 18977856.
- ^ a b Kitabchi AE, Umpierrez GE, Miles JM, Fisher JN (July 2009). "Hyperglycemic crises in adult patients with diabetes". Diabetes Care. 32 (7): 1335–43. doi:10.2337/dc09-9032. PMC 2699725. PMID 19564476.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b c d "Diabetes Programme". World Health Organization. Retrieved 22 April 2014.
- ^ O'Gara, PT (Jan 29, 2013). "2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines". Circulation. 127 (4): e362-425. doi:10.1161/CIR.0b013e3182742cf6. PMID 23247304.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Cukierman, T (8 Nov 2005). "Cognitive decline and dementia in diabetes—systematic overview of prospective observational studies". Springer-Verlag. Retrieved 28 Apr 2013.
- ^ Attention: This template ({{cite doi}}) is deprecated. To cite the publication identified by doi:10.1383/medc.30.1.1.28264, please use {{cite journal}} (if it was published in a bona fide academic journal, otherwise {{cite report}} with
|doi=10.1383/medc.30.1.1.28264instead. - ^ Rother KI (April 2007). "Diabetes treatment—bridging the divide". The New England Journal of Medicine. 356 (15): 1499–501. doi:10.1056/NEJMp078030. PMID 17429082.
- ^ a b "Diabetes Mellitus (DM): Diabetes Mellitus and Disorders of Carbohydrate Metabolism: Merck Manual Professional". Merck Publishing. April 2010. Retrieved 2010-07-30.
- ^ Dorner M, Pinget M, Brogard JM (May 1977). "Essential labile diabetes". MMW Munch Med Wochenschr (in German). 119 (19): 671–4. PMID 406527.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Risérus U, Willet W (January 2009). "Dietary fats and prevention of type 2 diabetes". Progress in Lipid Research. 48 (1): 44–51. doi:10.1016/j.plipres.2008.10.002. PMC 2654180. PMID 19032965.
- ^ Malik, VS (2010-03-23). "Sugar Sweetened Beverages, Obesity, Type 2 Diabetes and Cardiovascular Disease risk". Circulation. 121 (11): 1356–64. doi:10.1161/CIRCULATIONAHA.109.876185. PMC 2862465. PMID 20308626.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Malik, VS (November 2010). "Sugar-Sweetened Beverages and Risk of Metabolic Syndrome and Type 2 Diabetes: A meta-analysis". Diabetes Care. 33 (11): 2477–83. doi:10.2337/dc10-1079. PMC 2963518. PMID 20693348.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Hu, EA; Pan, A; Malik, V; Sun, Q (2012-03-15). "White rice consumption and risk of type 2 diabetes: meta-analysis and systematic review". BMJ (Clinical research ed.). 344: e1454. doi:10.1136/bmj.e1454. PMC 3307808. PMID 22422870.
- ^ Lee, I-Min (1 July 2012). "Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy". The Lancet. 380 (9838): 219–29. doi:10.1016/S0140-6736(12)61031-9. PMC 3645500. PMID 22818936.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ a b "National Diabetes Clearinghouse (NDIC): National Diabetes Statistics 2011". U.S. Department of Health and Human Services. Retrieved 22 April 2014.
- ^ a b "Definition, Diagnosis and Classification of Diabetes Mellitus and its Complications" (PDF). World Health Organisation. 1999.
- ^ Unless otherwise specified, reference is: Table 20-5 in Mitchell, Richard Sheppard; Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson. Robbins Basic Pathology. Philadelphia: Saunders. ISBN 1-4160-2973-7.
{{cite book}}: CS1 maint: multiple names: authors list (link) 8th edition. - ^ Sattar N, Preiss, D, Murray, HM, Welsh, P, Buckley, BM, de Craen, AJ, Seshasai, SR, McMurray, JJ, Freeman, DJ (February 2010). "Statins and risk of incident diabetes: a collaborative meta-analysis of randomised statin trials". The Lancet. 375 (9716): 735–42. doi:10.1016/S0140-6736(09)61965-6. PMID 20167359.
{{cite journal}}: Unknown parameter|displayauthors=ignored (|display-authors=suggested) (help)CS1 maint: multiple names: authors list (link) - ^ a b c d e Mantzoros C, Serdy, S. Insulin Action. In: UpToDate, Nathan D (Ed), UpToDate, Waltham, MA. (Accessed on April 23, 2014).
- ^ Chapter 24. Endocrine Functions of the Pancreas & Regulation of Carbohydrate Metabolism. In: Barrett KE, Boitano S, Barman SM, Brooks HL. eds. Ganong's Review of Medical Physiology, 24e. New York, NY: McGraw-Hill; 2012.http://accessmedicine.mhmedical.com/content.aspx?bookid=393&Sectionid=39736766. Accessed April 23, 2014.
- ^ Bender DA, Mayes PA. Chapter 20. Gluconeogenesis & the Control of Blood Glucose. In: Murray RK, Bender DA, Botham KM, Kennelly PJ, Rodwell VW, Weil P. eds. Harper's Illustrated Biochemistry, 29e. New York, NY: McGraw-Hill; 2012.http://accessmedicine.mhmedical.com/content.aspx?bookid=389&Sectionid=40142496. Accessed April 23, 2014.
- ^ Masharani U, German MS. Chapter 17. Pancreatic Hormones and Diabetes Mellitus. In: Gardner DG, Shoback D. eds. Greenspan’s Basic & Clinical Endocrinology, 9e. New York, NY: McGraw-Hill; 2011.http://accessmedicine.mhmedical.com/content.aspx?bookid=380&Sectionid=39744057. Accessed April 23, 2014.
- ^ Definition and diagnosis of diabetes mellitus and intermediate hyperglycemia: Report of a WHO/IDF consultation (PDF). Geneva: World Health Organization. 2006. p. 21. ISBN 978-92-4-159493-6.
- ^ Vijan S (March 2010). "In the clinic. Type 2 diabetes". Annals of Internal Medicine. 152 (5): ITC31-15, quiz ITC316. doi:10.7326/0003-4819-152-5-201003020-01003. PMID 20194231.
- ^ ""Diabetes Care" January 2010". American Diabetes Association. Retrieved 2010-01-29.
- ^ Saydah SH, Miret M, Sung J, Varas C, Gause D, Brancati FL (August 2001). "Postchallenge hyperglycemia and mortality in a national sample of U.S. adults". Diabetes Care. 24 (8): 1397–402. doi:10.2337/diacare.24.8.1397. PMID 11473076.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Definition and diagnosis of diabetes mellitus and intermediate hyperglycemia : report of a WHO/IDF consultation (PDF). World Health Organization. 2006. p. 21. ISBN 978-92-4-159493-6.
- ^ Santaguida PL, Balion C, Hunt D, Morrison K, Gerstein H, Raina P, Booker L, Yazdi H. "Diagnosis, Prognosis, and Treatment of Impaired Glucose Tolerance and Impaired Fasting Glucose". Summary of Evidence Report/Technology Assessment, No. 128. Agency for Healthcare Research and Quality. Retrieved 2008-07-20.
{{cite web}}: CS1 maint: multiple names: authors list (link) - ^ Bartoli, E (Feb 2011). "The oral glucose tolerance test (OGTT) revisited". European journal of internal medicine. 22 (1): 8–12. doi:10.1016/j.ejim.2010.07.008. PMID 21238885.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Selvin E, Steffes MW, Zhu H, Matsushita K, Wagenknecht L, Pankow J, Coresh J, Brancati FL (2010). "Glycated hemoglobin, diabetes, and cardiovascular risk in nondiabetic adults". N. Engl. J. Med. 362 (9): 800–11. doi:10.1056/NEJMoa0908359. PMC 2872990. PMID 20200384.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Nathan DM, Cleary PA, Backlund JY, Genuth SM, Lachin JM, Orchard TJ, Raskin P, Zinman B; Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications (DCCT/EDIC) Study Research Group (December 2005). "Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes". The New England Journal of Medicine. 353 (25): 2643–53. doi:10.1056/NEJMoa052187. PMC 2637991. PMID 16371630.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ The Diabetes Control and Complications Trial Research Group (April 1995). "The effect of intensive diabetes therapy on the development and progression of neuropathy". Annals of Internal Medicine. 122 (8): 561–8. doi:10.1059/0003-4819-122-8-199504150-00001. PMID 7887548.
- ^ a b National Institute for Health and Clinical Excellence. Clinical guideline 66: Type 2 diabetes. London, 2008.
- ^ Attention: This template ({{cite doi}}) is deprecated. To cite the publication identified by doi: 10.1002/dmrr.435, please use {{cite journal}} (if it was published in a bona fide academic journal, otherwise {{cite report}} with
|doi= 10.1002/dmrr.435instead. - ^ Adler AI, Stratton IM, Neil HA, Yudkin JS, Matthews DR, Cull CA, Wright AD, Turner RC, Holman RR (August 2000). "Association of systolic blood pressure with macrovascular and microvascular complications of type 2 diabetes (UKPDS 36): prospective observational study". BMJ. 321 (7258): 412–9. doi:10.1136/bmj.321.7258.412. PMC 27455. PMID 10938049.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b c Ripsin CM, Kang, H, Urban, RJ (2009). "Management of blood glucose in type 2 diabetes mellitus" (PDF). American family physician. 79 (1): 29–36. PMID 19145963.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Pignone M, Alberts MJ, Colwell JA, Cushman M, Inzucchi SE, Mukherjee D, Rosenson RS, Williams CD, Wilson PW, Kirkman MS; American Diabetes Association; American Heart Association; American College of Cardiology Foundation (June 2010). "Aspirin for primary prevention of cardiovascular events in people with diabetes: a position statement of the American Diabetes Association, a scientific statement of the American Heart Association, and an expert consensus document of the American College of Cardiology Foundation". Diabetes Care. 33 (6): 1395–402. doi:10.2337/dc10-0555. PMC 2875463. PMID 20508233.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Cheng, J (Mar 31, 2014). "Effect of Angiotensin-Converting Enzyme Inhibitors and Angiotensin II Receptor Blockers on All-Cause Mortality, Cardiovascular Deaths, and Cardiovascular Events in Patients With Diabetes Mellitus: A Meta-analysis". JAMA internal medicine. PMID 24687000.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ "Pancreas Transplantation". American Diabetes Association. Retrieved 9 April 2014.
- ^ Polisena J, Tran K, Cimon K, Hutton B, McGill S, Palmer K (2009). "Home telehealth for diabetes management: a systematic review and meta-analysis". Diabetes Obes Metab. 11 (10): 913–30. doi:10.1111/j.1463-1326.2009.01057.x. PMID 19531058.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b c Wild S, Roglic G, Green A, Sicree R, King H (2004). "Global prevalence of diabetes: Estimates for the year 2000 and projections for 2030". Diabetes Care. 27 (5): 1047–53. doi:10.2337/diacare.27.5.1047. PMID 15111519.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Ripoll, Brian C. Leutholtz, Ignacio (2011-04-25). Exercise and disease management (2nd ed.). Boca Raton: CRC Press. p. 25. ISBN 978-1-4398-2759-8.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ^ a b c d e f g h i editor, Leonid Poretsky, (2009). Principles of diabetes mellitus (2nd ed.). New York: Springer. p. 3. ISBN 978-0-387-09840-1.
{{cite book}}:|last=has generic name (help)CS1 maint: extra punctuation (link) CS1 maint: multiple names: authors list (link) - ^ Konstantinos Laios; Karamanou, M; Saridaki, Z; Androutsos, G; et al. (2012). "Aretaeus of Cappadocia and the first description of diabetes". Hormones. 11 (1): 109–113. PMID 22450352.
{{cite journal}}: Explicit use of et al. in:|author=(help) - ^ a b Oxford English Dictionary. diabetes. Retrieved 2011-06-10.
- ^ a b Harper, Douglas (2001–2010). "Online Etymology Dictionary. diabetes.". Retrieved 2011-06-10.
- ^ a b Dallas, John (2011). "Royal College of Physicians of Edinburgh. Diabetes, Doctors and Dogs: An exhibition on Diabetes and Endocrinology by the College Library for the 43rd St. Andrew's Day Festival Symposium".
- ^ a b c d Oxford English Dictionary. mellite. Retrieved 2011-06-10.
- ^ a b c d "MyEtimology. mellitus.". Retrieved 2011-06-10.
- ^ Oxford English Dictionary. -ite. Retrieved 2011-06-10.
- ^ Theodore H. Tulchinsky, Elena A. Varavikova (2008). The New Public Health, Second Edition. New York: Academic Press. p. 200. ISBN 0-12-370890-7.
- ^ Piwernetz K, Home PD, Snorgaard O, Antsiferov M, Staehr-Johansen K, Krans M (May 1993). "Monitoring the targets of the St Vincent Declaration and the implementation of quality management in diabetes care: the DIABCARE initiative. The DIABCARE Monitoring Group of the St Vincent Declaration Steering Committee". Diabetic Medicine. 10 (4): 371–7. doi:10.1111/j.1464-5491.1993.tb00083.x. PMID 8508624.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Dubois, HFW and Bankauskaite, V (2005). "Type 2 diabetes programmes in Europe" (PDF). Euro Observer. 7 (2): 5–6.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Stewart WF, Ricci JA, Chee E, Hirsch AG, Brandenburg NA (June 2007). "Lost productive time and costs due to diabetes and diabetic neuropathic pain in the US workforce". J. Occup. Environ. Med. 49 (6): 672–9. doi:10.1097/JOM.0b013e318065b83a. PMID 17563611.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Washington R.E., Andrews R.M., Mutter R.L. Emergency Department Visits for Adults with Diabetes, 2010. HCUP Statistical Brief #167. November 2013. Agency for Healthcare Research and Quality, Rockville, MD. [1].
- ^ a b "Diabetes mellitus". Merck Veterinary Manual, 9th edition (online version). 2005. Retrieved 2011-10-23.
- ^ a b Maria Rotella, C (Summer 2013). "Role of Insulin in the Type 2 Diabetes Therapy: Past, Present and Future". International journal of endocrinology and metabolism. 11 (3): 137–144. PMID 24348585.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ "Inhaled Insulin Clears Hurdle Toward F.D.A. Approval". New York Times. Retrieved 12 April 2014.
Further reading
- Attention: This template ({{cite doi}}) is deprecated. To cite the publication identified by doi:10.1056/NEJMra1110560, please use {{cite journal}} (if it was published in a bona fide academic journal, otherwise {{cite report}} with
|doi=10.1056/NEJMra1110560instead.
External links
- Diabetes at the Open Directory Project
- American Diabetes Association
- IDF Diabetes Atlas
- National Diabetes Education Program
This template is no longer used; please see Template:Endocrine pathology for a suitable replacement
Template:Link FA Template:Link FA Template:Link FA Template:Link FA Template:Link GA
