Breast cancer: Difference between revisions
| [pending revision] | [pending revision] |
woman cancer |
|||
| Line 371: | Line 371: | ||
[[ur:سرطان پستان]] |
[[ur:سرطان پستان]] |
||
[[zh:乳癌]] |
[[zh:乳癌]] |
||
== |
|||
== Headline text == |
|||
== |
|||
cancer afect on woman |
|||
Revision as of 23:10, 20 October 2008
| Breast cancer | |
|---|---|
| Specialty | Oncology |
Breast cancer is a cancer that starts in the cells of the breast in women and men. Worldwide, breast cancer is the second most common type of cancer after lung cancer (10.4% of all cancer incidence, both sexes counted)[1] and the fifth most common cause of cancer death.[2] In 2005, breast cancer caused 502,000 deaths worldwide (7% of cancer deaths; almost 1% of all deaths).[2]
Because the breast is composed of identical tissues in males and females, breast cancer also occurs in males.[3][4] Incidences of breast cancer in men are approximately 100 times less common than in women, but men with breast cancer are considered to have the same statistical survival rates as women.[5]
Classification
Breast cancers are described along four different classification schemes, or groups, each based on different criteria and serving a different purpose:
- Pathology - Each tumor is classified by its histological (microscopic anatomy) appearance and other criteria.
- Grade of tumor - The histological grade of a tumor is determined by a pathologist under a microscope. A well-differentiated (low grade) tumor resembles normal tissue. A poorly differentiated (high grade) tumor is composed of disorganized cells and, therefore, does not look like normal tissue. Moderately differentiated (intermediate grade) tumors are somewhere in between.
- Protein & gene expression status - Currently, all breast cancers should be tested for expression, or detectable effect, of the estrogen receptor (ER), progesterone receptor (PR) and HER2/neu proteins. These tests are usually done by immunohistochemistry and are presented in a pathologist's report. The profile of expression of a given tumor helps predict its prognosis, or outlook, and helps an oncologist choose the most appropriate treatment. More genes and/or proteins may be tested in the future.
- Stage of a tumor - The currently accepted staging scheme for breast cancer is the TNM classification. This considers the Tumor itself, whether it has spread to lymph Nodes, and whether there are any Metastases to locations other than the breast and lymph nodes.
Breast cancer is usually, but not always, primarily classified by its histological appearance. Rare variants are defined on the basis of physical exam findings. For example, Inflammatory breast cancer (IBC), a form of ductal carcinoma or malignant cancer in the ducts, is distinguished from other carcinomas by the inflamed appearance of the affected breast.[6] In the future, some pathologic classifications may be changed. For example, a subset of ductal carcinomas may be re-named basal-like carcinoma (part of the "triple-negative" tumors).[citation needed]
Signs and symptoms
The first symptom, or subjective sign, of breast cancer is typically a lump that feels different than the surrounding breast tissue. According to the Merck Manual, more than 80% of breast cancer cases are discovered when the woman feels a lump.[7] According to the American Cancer Society (ACS), the first medical sign, or objective indication of breast cancer as detected by a physician, is discovered by mammogram.[8] Lumps found in lymph nodes located in the armpits[7] and/or collarbone[citation needed] can also indicate breast cancer.
Indications of breast cancer other than a lump may include changes in breast size or shape, skin dimpling, nipple inversion, or spontaneous single-nipple discharge. Pain is an unreliable tool in determining the presence of breast cancer, but may be indicative of other breast-related health issues such as mastodynia.[8][7][9]
When breast cancer cells invade the dermal lymphatics, small lymph vessels in the skin of the breast, its presentation can resemble skin inflammation and thus is known as inflammatory breast cancer (IBC). Symptoms of inflammatory breast cancer include pain, swelling, warmth and redness throughout the breast, as well as an orange peel texture to the skin referred to as peau d'orange.[7]
Another reported symptom complex of breast cancer is Paget's disease of the breast. This syndrome presents as eczematoid skin changes such as redness and mild flaking of the nipple skin. As Paget's advances, symptoms may include tingling, itching, increased sensitivity, burning, and pain. There may also be discharge from the nipple. Approximately half of women diagnosed with Paget's also have a lump in the breast.[10]
Occasionally, breast cancer presents as metastatic disease, that is, cancer that has spread beyond the original organ. Metastatic breast cancer will cause symptoms that depend on the location of metastasis. More common sites of metastasis include bone, liver, lung and brain. Unexplained weight loss can occasionally herald an occult breast cancer, as can symptoms of fevers or chills. Bone or joint pains can sometimes be manifestations of metastatic breast cancer, as can jaundice or neurological symptoms. These symptoms are "non-specific," meaning they can also be manifestations of many other illnesses.[11]
Most symptoms of breast disorder do not turn out to represent underlying breast cancer. Benign breast diseases such as mastitis and fibroadenoma of the breast are more common causes of breast disorder symptoms. The appearance of a new symptom should be taken seriously by both patients and their doctors, because of the possibility of an underlying breast cancer at almost any age.[12]
Epidemiology and etiology
Epidemiological risk factors for a disease can provide important clues as to the etiology, or cause, of a disease. The first case-controlled study on breast cancer epidemiology was done by Janet Lane-Claypon, who published a comparative study in 1926 of 500 breast cancer cases and 500 control patients of the same background and lifestyle for the British Ministry of Health.[13][verification needed][14]
Today, breast cancer, like other forms of cancer, is considered to be the final outcome of multiple environmental and hereditary factors. Some of these factors include:
- Lesions to DNA such as genetic mutations. Mutations that can lead to breast cancer have been experimentally linked to estrogen exposure.[15] Beyond the contribution of estrogen, research has implicated viral oncogenesis and the contribution of ionizing radiation in causing genetic mutations.[citation needed]
- Failure of immune surveillance, a theory in which the immune system removes malignant cells throughout one's life.[16]
- Abnormal growth factor signaling in the interaction between stromal cells and epithelial cells can facilitate malignant cell growth. For example, tumors can induce blood vessel growth (angiogenesis) by secreting various growth factors further facilitating cancer growth.[citation needed]
- Inherited defects in DNA repair genes, such as BRCA1, BRCA2[17] and p53.[citation needed]
Although many epidemiological risk factors have been identified, the cause of any individual breast cancer is often unknowable. In other words, epidemiological research informs the patterns of breast cancer incidence across certain populations, but not in a given individual. The primary risk factors that have been identified are sex,[18] age,[19] childbearing, hormones,[20] a high-fat diet,[21] alcohol intake,[22][23] obesity,[24] and environmental factors such as tobacco use, radiation[17] and shiftwork.[25]
No etiology is known for 95% of breast cancer cases, while approximately 5% of new breast cancers are attributable to hereditary syndromes.[26] In particular, carriers of the breast cancer susceptibility genes, BRCA1 and BRCA2, are at a 30-40% increased risk for breast and ovarian cancer, depending on in which portion of the protein the mutation occurs.[27]
Worldwide, breast cancer is by far the most common cancer amongst women, with an incidence rate more than twice that of colorectal cancer and cervical cancer and about three times that of lung cancer. However breast cancer mortality worldwide is just 25% greater than that of lung cancer in women.[1] In 2005, breast cancer caused 502,000 deaths worldwide (7% of cancer deaths; almost 1% of all deaths).[2] The number of cases worldwide has significantly increased since the 1970s, a phenomenon partly blamed on modern lifestyles in the Western world.[28][29]
The incidence of breast cancer varies greatly around the world, being lower in less-developed countries and greatest in the more-developed countries. In the twelve world regions, the annual age-standardized incidence rates per 100,000 women are as follows: in Eastern Asia, 18; South Central Asia, 22; sub-Saharan Africa, 22; South-Eastern Asia, 26; North Africa and Western Asia, 28; South and Central America, 42; Eastern Europe, 49; Southern Europe, 56; Northern Europe, 73; Oceania, 74; Western Europe, 78; and in North America, 90.[30]
Women in the United States have the highest incidence rates of breast cancer in the world; 141 among white women and 122 among African American women.[31][32] Among women in the US, breast cancer is the most common cancer and the second-most common cause of cancer death (after lung cancer).[32] Women in the US have a 1 in 8 (12.5%) lifetime chance of developing invasive breast cancer and a 1 in 35 (3%) chance of breast cancer causing their death.[32] In 2007, breast cancer was expected to cause 40,910 deaths in the US (7% of cancer deaths; almost 2% of all deaths).[8]
In the US, both incidence and death rates for breast cancer have been declining in the last few years in Native Americans and Alaskan Natives.[33][8] Nevertheless, a US study conducted in 2005 by the Society for Women's Health Research indicated that breast cancer remains the most feared disease,[34] even though heart disease is a much more common cause of death among women.[35] Many doctors say that women exaggerate their risk of breast cancer.[36]
Prevention
Lower age of first childbirth (less than 24 years maternal age), having more children (about 7% lowered risk per child), and breastfeeding (4% per breastfeeding year, with an average relative risk around 0.7[37][38]) have all been correlated to lowered breast cancer risk in large studies.[39]
Phytoestrogens and soy
Phytoestrogens such as found in soybeans have been extensively studied in animal and human in-vitro and epidemiological studies. The literature support the following conclusions:
- Plant estrogen intake, such as from soy products, in early adolescence may protect against breast cancer later in life.[40]
- Plant estrogen intake later in life is not likely to influence breast cancer incidence either positively or negatively.[41]
Folic acid (folate)
This article's factual accuracy is disputed. (March 2008) |
Studies have found that "folate intake counteracts breast cancer risk associated with alcohol consumption"[42] and "women who drink alcohol and have a high folate intake are not at increased risk of cancer."[43][44][45] A prospective study of over 17,000 women found that those who consume 40 grams of alcohol (about 3-4 drinks) per day have a higher risk of breast cancer. However, in women who take 200 micrograms of folate (folic acid or Vitamin B9) every day, the risk of breast cancer drops below that of alcohol abstainers.[46]
Folate is involved in the synthesis, repair, and functioning of DNA, the body’s genetic map, and a deficiency of folate may result in damage to DNA that may lead to cancer.[47] In addition to breast cancer, studies have also associated diets low in folate with increased risk of pancreatic, and colon cancer.[48][49]
Foods rich in folate include citrus fruits, citrus juices, dark green leafy vegetables (such as spinach), dried beans, and peas.
Avoiding exposure to secondhand tobacco smoke
Breathing secondhand smoke increases breast cancer risk by 70% in younger, primarily pre-menopausal women. The California Environmental Protection Agency has concluded that passive smoking causes breast cancer[50] and the US Surgeon General[51] has concluded that the evidence is "suggestive," one step below causal. There is some evidence that exposure to tobacco smoke is most problematic between puberty and first childbirth. The reason that breast tissue appears most sensitive to chemical carcinogens in this phase is that breast cells are not fully differentiated until lactation.[52]
Oophorectomy and mastectomy
Prophylactic oophorectomy (removal of ovaries), in high-risk individuals, when child-bearing is complete, reduces the risk of developing breast cancer by 60%, as well as reducing the risk of developing ovarian cancer by 96%.[53]
Medications
Hormonal therapy has been used for chemoprevention in individuals at high risk for breast cancer. In 2002, a clinical practice guideline by the US Preventive Services Task Force (USPSTF) recommended that "clinicians discuss chemoprevention with women at high risk for breast cancer and at low risk for adverse effects of chemoprevention" with a grade B recommendation.[54][verification needed][55][56]
Selective estrogen receptor modulators (SERMs)
The guidelines[clarification needed] were based on studies of SERMs from the MORE, BCPT P-1, and Italian trials. In the MORE trial, the relative risk reduction for raloxifene was 76%.[57] The P-1 preventative study demonstrated that tamoxifen can prevent breast cancer in high-risk individuals. The relative risk reduction was up to 50% of new breast cancers, though the cancers prevented were more likely estrogen-receptor positive (this is analogous to the effect of finasteride on the prevention of prostate cancer, in which only low-grade prostate cancers were prevented).[58][59] The Italian trial showed benefit from tamoxifen.[60]
Additional randomized controlled trials have been published since the guidelines. The IBIS trial found benefit from tamoxifen.[61] In 2006, the NSABP STAR trial demonstrated that raloxifene had equal efficacy in preventing breast cancer compared with tamoxifen, but that there were fewer side effects with raloxifene.[62] The RUTH Trial concluded that "benefits of raloxifene in reducing the risks of invasive breast cancer and vertebral fracture should be weighed against the increased risks of venous thromboembolism and fatal stroke".[63] On September 14, 2007, the US Food and Drug Administration approved raloxifene (Evista) to prevent invasive breast cancer in postmenopausal women.[64]
Screening
Breast cancer screening is an attempt to find unsuspected cancers. The most common screening methods are self and clinical breast exams, x-ray mammography, and breast Magnetic Resonance Imaging (MRI). Genetic testing may also be used.
Breast self-examination involves examining one's own breasts using a specific palpation technique to detect any lumps in the breast tissue, which may be cancerous. Clinical exams are similar, except they are performed by a clinician or doctor.
X-ray mammography uses x-rays to examine the breast for any uncharacteristic masses or lumps. Regular mammograms -- the process of getting breast mammography -- is often recommended as a preventative measure, particularly for older women and at-risk individuals.
Finally, breast MRIs are another imaging technique that can be used to spot potentially cancerous masses.
Genetic testing for breast cancer typically involves testing for mutations in the BRCA genes. This is not generally a recommended technique except for those at elevated risk for breast cancer.
Diagnosis
Breast cancer is diagnosed by the examination of surgically removed breast tissue. A number of procedures can obtain tissue or cells prior to definitive treatment for histological or cytological examination. Such procedures include fine-needle aspiration, nipple aspirates, ductal lavage, core needle biopsy, and local surgical excision. These diagnostic steps, when coupled with radiographic imaging, are usually accurate in diagnosing a breast lesion as cancer. Occasionally, pre-surgical procedures such as fine needle aspirate may not yield enough tissue to make a diagnosis, or may miss the cancer entirely. Imaging tests are sometimes used to detect metastasis and include chest X-ray, bone scan, Cat scan, MRI, and PET scanning. While imaging studies are useful in determining the presence of metastatic disease, they are not in and of themselves diagnostic of cancer. Only microscopic evaluation of a biopsy specimen can yield a cancer diagnosis. Ca 15.3 (carbohydrate antigen 15.3, epithelial mucin) is a tumor marker determined in blood which can be used to follow disease activity over time after definitive treatment. Blood tumor marker testing is not routinely performed for the screening of breast cancer, and has poor performance characteristics for this purpose.
Staging
It has been suggested that this section be split out into another article titled Breast cancer staging. (Discuss) (June 2008) |
Breast cancer is staged according to the TNM system, updated in the AJCC Staging Manual, now on its sixth edition. Prognosis is closely linked to results of staging, and staging is also used to allocate patients to treatments both in clinical trials and clinical practice. The information for staging is as follows:
TX: Primary tumor cannot be assessed. T0: No evidence of tumor. Tis: Carcinoma in situ, no invasion T1: Tumor is 2 cm or less T2: Tumor is more than 2 cm but not more than 5 cm T3: Tumor is more than 5 cm T4: Tumor of any size growing into the chest wall or skin, or inflammatory breast cancer
NX: Nearby lymph nodes cannot be assessed N0: Cancer has not spread to regional lymph nodes. N1: Cancer has spread to 1 to 3 axillary or one internal mammary lymph node N2: Cancer has spread to 4 to 9 axillary lymph nodes or multiple internal mammary lymph nodes N3: One of the following applies:
Cancer has spread to 10 or more axillary lymph nodes, or Cancer has spread to the lymph nodes under the clavicle (collar bone), or Cancer has spread to the lymph nodes above the clavicle, or Cancer involves axillary lymph nodes and has enlarged the internal mammary lymph nodes, or Cancer involves 4 or more axillary lymph nodes, and tiny amounts of cancer are found in internal mammary lymph nodes on sentinel lymph node biopsy.
MX: Presence of distant spread (metastasis) cannot be assessed. M0: No distant spread. M1: Spread to distant organs, not including the supraclavicular lymph node, has occurred
Summary of stages:
- Stage 0 - Carcinoma in situ (DCIS)
- Stage I - Tumor (T) does not involve axillary lymph nodes (N).
- Stage IIA – T 2-5 cm, N negative, or T <2 cm and N positive.
- Stage IIB – T > 5 cm, N negative, or T 2-5 cm and N positive (< 4 axillary nodes).
- Stage IIIA – T > 5 cm, N positive, or T 2-5 cm with 4 or more axillary nodes
- Stage IIIB – T has penetrated chest wall or skin, and may have spread to < 10 axillary N
- Stage IIIC – T has > 10 axillary N, 1 or more supraclavicular or infraclavicular N, or internal mammary N.
- Stage IV – Distant metastasis (M)
Approximately 90% of new breast cancer cases in the US will be classified as "early-stage" cases (DCIS, Stage I,IIA, IIB or IIIA), due to early detection and prevention techniques. Early-stage treatment options are different from late-stage options.[65]
Hormone receptors
Breast lesions are examined for certain markers, notably sex steroid hormone receptors. About two thirds of postmenopausal breast cancers are estrogen receptor positive (ER+) and progesterone receptor positive (PR+).[66] Receptor status modifies the treatment as, for instance, only ER-positive tumors, not ER-negative tumors, are sensitive to hormonal therapy.
HER2
The breast cancer is also usually tested for the presence of human epidermal growth factor receptor 2, a protein also known as HER2, neu or erbB2. HER2 is a cell-surface protein involved in cell development. In normal cells, HER2 controls aspects of cell growth and division. When activated in cancer cells, HER2 accelerates tumor formation. About 20-30% of breast cancers overexpress HER2. Those patients may be candidates for the drug trastuzumab, both in the postsurgical setting (so-called "adjuvant" therapy), and in the metastatic setting.[67]
Treatment
The mainstay of breast cancer treatment is surgery when the tumor is localized, with possible adjuvant hormonal therapy (with tamoxifen or an aromatase inhibitor), chemotherapy, and/or radiotherapy. At present, the treatment recommendations after surgery (adjuvant therapy) follow a pattern. This pattern is subject to change, as every two years, a worldwide conference takes place in St. Gallen, Switzerland, to discuss the actual results of worldwide multi-center studies. Depending on clinical criteria (age, type of cancer, size, metastasis) patients are roughly divided to high risk and low risk cases, with each risk category following different rules for therapy. Treatment possibilities include radiation therapy, chemotherapy, hormone therapy, and immune therapy.
In planning treatment, doctors can also use PCR tests like Oncotype DX or microarray tests like MammaPrint that predict breast cancer recurrence risk based on gene expression. In February 2007, the MammaPrint test became the first breast cancer predictor to win formal approval from the Food and Drug Administration. This is a new gene test to help predict whether women with early-stage breast cancer will relapse in 5 or 10 years, this could help influence how aggressively the initial tumor is treated.[68]
Interstitial laser thermotherapy (ILT) is an innovative method of treating breast cancer in a minimally invasive manner and without the need for surgical removal, and with the absence of any adverse effect on the health and survival of the patient during intermediate followup [69].
Radiation treatment is also used to help destroy cancer cells that may linger after surgery. Radiation can reduce the risk of recurrence by 50-66% (1/2 - 2/3rds reduction of risk) when delivered in the correct dose. [70]
Prognosis
A prognosis is the medical team's "best guess" in how cancer will affect a patient. There are many prognostic factors associated with breast cancer: staging, tumour size and location, grade, whether disease is systemic (has metastasized, or traveled to other parts of the body), recurrence of the disease, and age of patient.
Stage is the most important, as it takes into consideration size, local involvement, lymph node status and whether metastatic disease is present. The higher the stage at diagnosis, the worse the prognosis. Larger tumours, invasiveness of disease to lymph nodes, chest wall, skin or beyond, and aggressiveness of the cancer cells raise the stage, while smaller tumours, cancer-free zones, and close to normal cell behaviour (grading) lower it.
Grading is based on how cultured biopsied cells behave. The closer to normal cancer cells are, the slower their growth and a better prognosis. If cells are not well differentiated, they appear immature, divide more rapidly, and tend to spread. Well differentiated is given a grade of 1, moderate is grade 2, while poor or undifferentiated is given a higher grade of 3 or 4 (depending upon the scale used).
Younger women tend to have a poorer prognosis than post-menopausal women due to several factors. Their breasts are active with their cycles, they may be nursing infants, and may be unaware of changes in their breasts. Therefore, younger women are usually at a more advanced stage when diagnosed.
The presence of estrogen and progesterone receptors in the cancer cell, while not prognostic, is important in guiding treatment. Those who do not test positive for these specific receptors will not respond to hormone therapy.
Likewise, HER2/neu status directs the course of treatment. Patients whose cancer cells are positive for HER2/neu have more aggressive disease and may be treated with trastuzumab, a monoclonal antibody that targets this protein.
Psychological aspects of diagnosis and treatment
The emotional impact of cancer diagnosis, symptoms, treatment, and related issues can be severe. Most larger hospitals are associated with cancer support groups which can help patients cope with the many issues that come up in a supportive environment with other people with experience with similar issues. Online cancer support groups are also very beneficial to cancer patients, especially in dealing with uncertainty and body-image problems inherent in cancer treatment.
Not all breast cancer patients experience their illness in the same manner. Factors such as age can have a significant impact on the way a patient copes with a breast cancer diagnosis. For example, a recent study conducted by researchers at the College of Public Health of the University of Georgia showed that older women may face a more difficult recovery from breast cancer than their younger counterparts.[71] As the incidence of breast cancer in women over 50 rises and survival rates increase, breast cancer is increasingly becoming a geriatric issue that warrants both further research and the expansion of specialized cancer support services tailored for specific age groups.[71]
Racial disparities in diagnosis and treatment
It has been suggested that this article be merged with Epidemiology and etiology of Breast cancer and Breast cancer treatment. (Discuss) Proposed since October 2007. |
Several studies have found that black women in the U.S. are more likely to die from breast cancer even though white women are more likely to be diagnosed with the disease. Even after diagnosis, black women are less likely to get treatment compared to white women.[72][73][74] Scholars have advanced several theories for the disparities, including inadequate access to screening, reduced availability of the most advanced surgical and medical techniques, or some biological characteristic of the disease in the African American population.[75] Some studies suggest that the racial disparity in breast cancer outcomes may reflect cultural biases more than biological disease differences.[76] Research is currently ongoing to define the contribution of both biological and cultural factors.[77][73]
Metastasis
Most people understand breast cancer as something that happens in the breast. However it can metastasize (spread) via lymphatics to nearby lymph nodes, usually those under the arm. That is why surgery for breast cancer always involves some type of surgery for the glands under the arm — either axillary clearance, sampling, or sentinel node biopsy.
Breast cancer can also spread to other parts of the body via blood vessels or the lymphatic system. So it can spread to the lungs, pleura (the lining of the lungs), liver, brain, and most commonly to the bones.[78] Seventy percent of the time that breast cancer spreads to other locations, it spreads to bone, especially the vertebrae and the long bones of the arms, legs, and ribs. Breast cancer cells "set up house" in the bones and form tumors. Usually when breast cancer spreads to bone, it eats away healthy bone, causing weak spots, where the bones can break easily. That is why breast cancer patients are often seen wearing braces or using a wheelchair, and have aching bones.
When breast cancer is found in bones, it has usually spread to more than one site. At this stage, it is treatable, often for many years, but it is not curable. Like normal breast cells, these tumors in the bone often thrive on female hormones, especially estrogen. Therefore treatment with medicines that lower estrogen levels may be prescribed.
History
Breast cancer may be one of the oldest known forms of cancer tumors in humans. The oldest description of cancer was discovered in Egypt and dates back to approximately 1600 BC. The Edwin Smith Papyrus describes 8 cases of tumors or ulcers of the breast that were treated by cauterization.The writing says about the disease, "There is no treatment."[79] For centuries, physicians described similar cases in their practises, with the same sad conclusion. It wasn't until doctors achieved greater understanding of the circulatory system in the 17th century that they could establish a link between breast cancer and the lymph nodes in the armpit. The French surgeon Jean Louis Petit (1674-1750) and later the Scottish surgeon Benjamin Bell (1749-1806) were the first to remove the lymph nodes, breast tissue, and underlying chest muscle. Their successful work was carried on by William Stewart Halsted who started performing mastectomies in 1882. The Halsted radical mastectomy often involved removing both breasts, associated lymph nodes, and the underlying pectoral muscles. This often led to long-term pain and disability, but was seen as necessary in order to prevent the cancer from recurring.[80] Radical mastectomies remained the standard until the 1970s, when a new understanding of metastasis led to perceiving cancer as a systemic illness as well as a localized one, and more sparing procedures were developed that proved equally effective.
Prominent women who lost their lives because of breast cancer include Empress Theodora, wife of Justinian; Anne of Austria, mother of Louis XIV of France; Mary Washington, mother of George and the environmentalist Rachel Carson.[81]
Cultural references

In the month of October, breast cancer is recognized by survivors, family and friends of survivors and/or victims of the disease.[82] A pink ribbon is worn to recognize the struggle that sufferers face when battling the cancer.[83]
Pink for October is an initiative started by Matthew Oliphant, which asks that any sites willing to help make people aware of breast cancer, change their template or layout to include the color pink, so that when visitors view the site, they see that the majority of the site is pink. Then after reading a short amount of information about breast cancer, or being redirected to another site, they are aware of the disease itself.[84]
The patron saint of breast cancer is Saint Agatha of Sicily.[85]
The pink and blue ribbon was designed in 1996 by Nancy Nick, President and Founder of the John W. Nick Foundation to bring awareness that "Men Get Breast Cancer Too!"[86]
Gallery
-
Breast self exam
-
Illustration of the early warning signs of breast cancer (click for larger image)
-
Woman undergoing mammogram
-
Mammography pictures, normal (left) and cancerous (right)
-
Mammogram displaying breast cancer, indicated with an arrow (click for larger view)
-
Mastectomy patient
-
Breast prostheses used by some mastectomy patients
-
Drawing of inflammatory breast cancer
-
Patient with advanced local-regional recurrence of breast cancer with an ulcerating axillary mass
-
Mastectomy specimen containing a very large cancer of the breast (in this case, an invasive ductal carcinoma)
-
Typical macroscopic (gross) appearance of the cut surface of a mastectomy specimen containing a cancer, in this case, an invasive ductal carcinoma of the breast, pale area at the center
-
Excised human breast tissue, showing a stellate area of cancer 2cm in diameter. The lesion could be felt clinically as a hard mobile lump, not attached to skin or chest wall.
-
Benign granular cell tumor removed from a woman's breast. Granular cell tumors of the breast represent one of the few lesions that can impersonate an invasive breast cancer on gross examination.
-
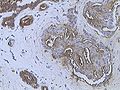
Infiltrating ductal carcinoma of the breast
-
Infiltrating ductal carcinoma of the Breast assayed with anti Mucin 1 antibody
-
Breast cancer (Infiltrating ductal carcinoma of the breast) assayed with anti HER-2 (ErbB2) antibody
-
Invasive lobular carcinoma of the breast demonstrating a predominantly lobular growth pattern
-
Metaplastic (sarcomatoid) carcinoma of the breast.
-
Histopathologic image from ductal cell carcinoma in situ (DCIS) of breast. Hematoxylin-eosin stain.
-
Histopathology of invasive ductal carcinoma of the breast representing a scirrhous growth. Core needle biopsy. HER-2/neu oncoprotein expression by Ventana immunostaining system.
See also
- List of notable breast cancer patients according to occupation
- List of notable breast cancer patients according to survival status
- List of breast carcinogenic substances
- Mammary tumor for breast cancer in other animals
- Breast reconstruction
- Alcohol and cancer
- Mammography Quality Standards Act
- National Breast Cancer Coalition
- National Comprehensive Cancer Network
- Breast Cancer Action
- Breakthrough Breast Cancer
- Living Beyond Breast Cancer
- Barron Lerner (Physician)
- International Agency for Research on Cancer
- The Hormone Foundation
- Susan G. Komen for the Cure
References
- ^ a b World Health Organization International Agency for Research on Cancer (2003). "World Cancer Report". Retrieved 2008-02-03.
{{cite web}}: Unknown parameter|month=ignored (help) - ^ a b c World Health Organization (2006). "Fact sheet No. 297: Cancer". Retrieved 2007-04-26.
{{cite web}}: Unknown parameter|month=ignored (help) - ^ "Male Breast Cancer Treatment - National Cancer Institute". National Cancer Institute. 2006. Retrieved 2006-10-16.
{{cite web}}: External link in|work= - ^ "Breast Cancer in Men: Cancer Research UK". Cancer Research UK. 2007. Retrieved 2007-11-06.
{{cite web}}: External link in|work= - ^ American Cancer Society (2007). "What Are the Key Statistics About Breast Cancer in Men?". Retrieved 2008-02-03.
{{cite web}}: Unknown parameter|month=ignored (help) - ^ Giordano SH, Hortobagyi GN (2003). "Inflammatory breast cancer: clinical progress and the main problems that must be addressed". Breast Cancer Res. 5 (6): 284–8. doi:10.1186/bcr608. PMID 14580242.
{{cite journal}}: CS1 maint: unflagged free DOI (link) Free Full Text. - ^ a b c d Merck Manual of Diagnosis and Therapy (2003). "Breast Disorders: Cancer". Retrieved 2008-02-05.
{{cite web}}: Unknown parameter|month=ignored (help) - ^ a b c d American Cancer Society (2007). "Cancer Facts & Figures 2007" (PDF). Retrieved 2007-04-26.
- ^ eMedicine (2006). "Breast Cancer Evaluation". Retrieved 2008-02-05.
{{cite web}}: Unknown parameter|month=ignored (help) - ^ National Cancer Institute (2005). "Paget's Disease of the Nipple: Questions and Answers". Retrieved 2008-02-06.
{{cite web}}: Unknown parameter|month=ignored (help) - ^ National Cancer Institute (2004). "Metastatic Cancer: Questions and Answers". Retrieved 2008-02-06.
{{cite web}}: Unknown parameter|month=ignored (help) - ^ Merk Manual of Diagnosis and Therapy (2003). "Breast Disorders: Introduction". Retrieved 2008-02-05.
{{cite web}}: Unknown parameter|month=ignored (help) - ^ Lane-Claypon, Janet Elizabeth (1926). A further report on cancer of the breast, with special reference to its associated antecedent conditions. London, Greater London: Her Majesty’s Stationery Office (HMSO). OCLC 14713036.
{{cite book}}: Cite has empty unknown parameter:|coauthors=(help) - ^ Alfredo Morabia (2004). A History of Epidemiologic Methods and Concepts. Boston: Birkhauser. pp. 301–302. ISBN 3-7643-6818-7. Retrieved 2007-12-31.
- ^ Cavalieri E, Chakravarti D, Guttenplan J; et al. (2006). "Catechol estrogen quinones as initiators of breast and other human cancers: implications for biomarkers of susceptibility and cancer prevention". Biochim. Biophys. Acta. 1766 (1): 63–78. doi:10.1016/j.bbcan.2006.03.001. PMID 16675129.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Farlex (2005). ">immunological surveillance "The Free Dictionary: Immunological Surveilliance". Retrieved 2008-02-10.
{{cite web}}: Check|url=value (help) - ^ a b American Cancer Society (2005). "Breast Cancer Facts & Figures 2005-2006" (PDF). Retrieved 2007-04-26.
- ^ Giordano, Sharon H (2004). "Breast carcinoma in men". Cancer. 101 (1). American Cancer Society: 51–57.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ^ "Individual Risk Factors". BreastCancer.org. Retrieved 2007-03-11.
- ^ Yager JD (2006). "Estrogen carcinogenesis in breast cancer". New Engl J Med. 354 (3): 270–82. doi:10.1056/NEJMra050776. PMID 16421368.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Chlebowski RT, Blackburn GL, Thomson CA, Nixon DW, Shapiro A, Hoy MK; et al. "Dietary fat reduction and breast cancer outcome: interim efficacy results from the Women's Intervention Nutrition Study (WINS)". J Natl Cancer Inst. 98 (24): 1767–1776. PMID 17179478.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Boffetta, Paolo (2006-03-23). "The burden of cancer attributable to alcohol drinking". International Journal of Cancer. 119 (4). Wiley-Liss, Inc: 884–887. doi:10.1002/ijc.21903. PMID 16557583. Retrieved 2006-10-09.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ [1]
- ^ BBC report Weight link to breast cancer risk
- ^ WHO international Agency for Research on Cancer Press Release No. 180, December 2007.
- ^ Madigan MP, Ziegler RG, Benichou J, Byrne C, Hoover RN (1995). "Proportion of breast cancer cases in the United States explained by well-established risk factors". J. Natl. Cancer Inst. 87 (22): 1681–5. doi:10.1093/jnci/87.22.1681. PMID 7473816.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Venkitaraman, AR (2002). "cancer susceptibility and the functions of BRCA1 and BRCA2". Cell. 108 (2): 171–82. doi:10.1016/S0092-8674(02)00615-3.
- ^ Laurance, Jeremy (2006-09-29). "Breast cancer cases rise 80% since Seventies". The Independent. Retrieved 2006-10-09.
- ^ "Breast Cancer: Statistics on Incidence, Survival, and Screening". Imaginis Corporation. 2006. Retrieved 2006-10-09.
{{cite web}}: External link in|work= - ^ Stewart B. W. and Kleihues P. (Eds): World Cancer Report. IARCPress. Lyon 2003
- ^ Ries LAG, Eisner MP, Kosary CL, et al. SEER Cancer Statistics Review, 1975–2000. Bethesda, MD: National Cancer Institute, 2003.
- ^ a b c American Cancer Society (2007). "What Are the Key Statistics for Breast Cancer?". Retrieved 2008-02-03.
{{cite web}}: Unknown parameter|month=ignored (help) - ^ Espey DK, Wu XC, Swan J; et al. (2007). "Annual report to the nation on the status of cancer, 1975-2004, featuring cancer in American Indians and Alaska Natives". Cancer. 110 (10): 2119–52. doi:10.1002/cncr.23044. PMID 17939129.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ "Women's Fear of Heart Disease Has Almost Doubled in Three Years, But Breast Cancer Remains Most Feared Disease" (Press release). Society for Women's Health Research. 2005-07-07. Retrieved 2007-10-15.
- ^ "Leading Causes of Death for American Women 2004" (PDF). National Heart Lung and Blood Institute. Retrieved 2007-10-15.
- ^ In Breast Cancer Data, Hope, Fear and Confusion, By DENISE GRADY, New York Times, January 26, 1999.
- ^ McTiernan A, Thomas DB (1986). "Evidence for a protective effect of lactation on risk of breast cancer in young women. Results from a case-control study". Am. J. Epidemiol. 124 (3): 353–8. PMID 3740036.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Byers T, Graham S, Rzepka T, Marshall J (1985). "Lactation and breast cancer. Evidence for a negative association in premenopausal women". Am. J. Epidemiol. 121 (5): 664–74. PMID 4014158.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ "Breast cancer and hormone replacement therapy: collaborative reanalysis of data from 51 epidemiological studies of 52,705 women with breast cancer and 108,411 women without breast cancer". Lancet. 350 (9084): 1047–59. 1997. doi:10.1016/S0140-6736(97)08233-0. PMID 10213546. Retrieved 2008-04-08.
{{cite journal}}: Cite has empty unknown parameter:|month=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Rice S, Whitehead SA (2006). "Phytoestrogens and breast cancer--promoters or protectors?". Endocr. Relat. Cancer. 13 (4): 995–1015. doi:10.1677/erc.1.01159. PMID 17158751.
- ^ Gikas PD, Mokbel K (2005). "Phytoestrogens and the risk of breast cancer: a review of the literature". Int J Fertil Womens Med. 50 (6): 250–8. PMID 16526415.
- ^ Mayo Clinic news release June 26 2001 "Folate Intake Counteracts Breast Cancer Risk Associated with Alcohol Consumption"
- ^ Boston University,Folate, Alcohol, and Cancer Risk
- ^ Bailey LB (2003). "Folate, methyl-related nutrients, alcohol, and the MTHFR 677C-->T polymorphism affect cancer risk: intake recommendations". J. Nutr. 133 (11 Suppl 1): 3748S–3753S. PMID 14608109.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Zhang S, Hunter D, Hankinson S, Giovannucci E, Rosner B, Colditz G, Speizer F, Willett W (1999). "A prospective study of folate intake and the risk of breast cancer". JAMA. 281 (17): 1632–7. doi:10.1001/jama.281.17.1632. PMID 10235158.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Baglietto, Laura, et al. Does dietary folate intake modify effect of alcohol consumption on breast cancer risk? Prospective cohort study. British Medical Journal, August 8, 2005
- ^ Jennings E. (1995). "Folic acid as a cancer preventing agent". Medical Hypotheses. 45 (3): 297–303. doi:10.1016/0306-9877(95)90121-3. PMID 8569555.
- ^ Giovannucci E, Stampfer MJ, Colditz GA, Hunter DJ, Fuchs C, Rosner BA, Speizer FE, Willett WC. (1998). "Multivitamin use, folate, and colon cancer in women in the Nurses' Health Study". Annals of Internal Medicine. 129 (7): 517–524. PMID 9758570.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ name="Oldref_42">Freudenheim JL, Grahm S, Marshall JR, Haughey BP, Cholewinski S, Wilkinson G (1991). "Folate intake and carcinogenesis of the colon and rectum". International Journal of Epidemiology. 20 (2): 368–374. doi:10.1093/ije/20.2.368. PMID 1917236.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ California Environmental Protection Agency: Air Resources Board, "Proposed Identification of Environmental Tobacco Smoke as a Toxic Air Contaminant" (June 24, 2005); on January 26, 2006, the Air Resources Board, following a lengthy review and public outreach process, determined ETS to be a Toxic Air Contaminant (TAC).
- ^ U.S. Department of Health and Human Services. "The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General", 2006
- ^ J. Russo, I. Russo. "Molecular Basis of Breast Cancer: Prevention and Treatment," Springer, 2003
- ^ Kauff N, Satagopan J, Robson M, Scheuer L, Hensley M, Hudis C, Ellis N, Boyd J, Borgen P, Barakat R, Norton L, Castiel M, Nafa K, Offit K (2002). "Risk-reducing salpingo-oophorectomy in women with a BRCA1 or BRCA2 mutation". N Engl J Med. 346 (21): 1609–15. doi:10.1056/NEJMoa020119. PMID 12023992.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ "Guide to Clinical Preventive Services, Third Edition: Periodic Updates, 2000-2003". Agency for Healthcare Research and Quality. US Preventive Services Task Force. Retrieved 2007-10-07.
- ^ "Chemoprevention of breast cancer: recommendations and rationale". Ann. Intern. Med. 137 (1): 56–8. 2002. PMID 12093249.
- ^ Kinsinger LS, Harris R, Woolf SH, Sox HC, Lohr KN (2002). "Chemoprevention of breast cancer: a summary of the evidence for the U.S. Preventive Services Task Force". Ann. Intern. Med. 137 (1): 59–69. PMID 12093250.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Cummings SR, Eckert S, Krueger KA; et al. (1999). "The effect of raloxifene on risk of breast cancer in postmenopausal women: results from the MORE randomized trial. Multiple Outcomes of Raloxifene Evaluation". JAMA. 281 (23): 2189–97. doi:10.1001/jama.281.23.2189. PMID 10376571.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Fisher B, Costantino JP, Wickerham DL; et al. (2005). "Tamoxifen for the prevention of breast cancer: current status of the National Surgical Adjuvant Breast and Bowel Project P-1 study". J. Natl. Cancer Inst. 97 (22): 1652–62. doi:10.1093/jnci/dji372. PMID 16288118.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Fisher B, Costantino JP, Wickerham DL; et al. (1998). "Tamoxifen for prevention of breast cancer: report of the National Surgical Adjuvant Breast and Bowel Project P-1 Study". J. Natl. Cancer Inst. 90 (18): 1371–88. doi:10.1093/jnci/90.18.1371. PMID 9747868.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Veronesi U, Maisonneuve P, Rotmensz N; et al. (2007). "Tamoxifen for the prevention of breast cancer: late results of the Italian Randomized Tamoxifen Prevention Trial among women with hysterectomy". J. Natl. Cancer Inst. 99 (9): 727–37. doi:10.1093/jnci/djk154. PMID 17470740.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Cuzick J, Forbes JF, Sestak I; et al. (2007). "Long-term results of tamoxifen prophylaxis for breast cancer--96-month follow-up of the randomized IBIS-I trial". J. Natl. Cancer Inst. 99 (4): 272–82. doi:10.1093/jnci/djk049. PMID 17312304.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Vogel VG, Costantino JP, Wickerham DL; et al. (2006). "Effects of tamoxifen vs raloxifene on the risk of developing invasive breast cancer and other disease outcomes: the NSABP Study of Tamoxifen and Raloxifene (STAR) P-2 trial". JAMA. 295 (23): 2727–41. doi:10.1001/jama.295.23.joc60074. PMID 16754727.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Barrett-Connor E, Mosca L, Collins P, et al Raloxifene Use for The Heart (RUTH) Trial Investigators. (2006). "Effects of raloxifene on cardiovascular events and breast cancer in postmenopausal women". N. Engl. J. Med. 355 (2): 125–37. doi:10.1056/NEJMoa062462. PMID 16837676.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ AFP.google.com, US approves Lilly's Evista for breast cancer prevention
- ^ Zuckerman, Diana, "Treatment Options for Early-Stage Breast Cancer: Information for Primary Care Providers", Medscape Continuing Medical Education. National Research Center for Women and Families.
- ^ Rusiecki JA, Holford TR, Zahm SH, Zheng T (2005). "Breast cancer risk factors according to joint estrogen receptor and progesterone receptor status". Cancer Detect. Prev. 29 (5): 419–26. doi:10.1016/j.cdp.2005.07.004. PMID 16185815.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ accessed 1/30/07 cancer.gov
- ^ "FDA Approves New Breast Cancer Test". Associated Press, February 6, 2007.
- ^ Dowlatshahi, Kambiz; Dieschbourg, Janice J.; Bloom, Kenneth J. (2004). "Laser Therapy of Breast Cancer with 3-Year follow up". The Breast Journal. 10 (3). Blackwell Publishing: 240–243. doi:10.1111/j.1075-122X.2004.21436.x.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Breastcancer.org Treatment Options
- ^ a b Robb C, Haley WE, Balducci L; et al. (2007). "Impact of breast cancer survivorship on quality of life in older women". Crit. Rev. Oncol. Hematol. 62 (1): 84–91. doi:10.1016/j.critrevonc.2006.11.003. PMID 17188505.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Wisconsin Cancer Incidence and Mortality, 2000-2004 Wisconsin Department of Health and Family Services
- ^ a b Tammemagi CM (2007). "Racial/ethnic disparities in breast and gynecologic cancer treatment and outcomes". Curr. Opin. Obstet. Gynecol. 19 (1): 31–6. doi:10.1097/GCO.0b013e3280117cf8. PMID 17218849.
- ^ Hirschman J, Whitman S, Ansell D (2007). "The black:white disparity in breast cancer mortality: the example of Chicago". Cancer Causes Control. 18 (3): 323–33. doi:10.1007/s10552-006-0102-y. PMID 17285262.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Breast cancer rates differ in races by Amanda Villa Wednesday, October 24, 2007. Badger Herald
- ^ Benjamin M, Reddy S, Brawley OW (2003). "Myeloma and race: a review of the literature". Cancer Metastasis Rev. 22 (1): 87–93. doi:10.1023/A:1022268103136. PMID 12716040.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Demicheli R, Retsky MW, Hrushesky WJ, Baum M, Gukas ID, Jatoi I (2007). "Racial disparities in breast cancer outcome: insights into host-tumor interactions". Cancer. 110 (9): 1880–8. doi:10.1002/cncr.22998. PMID 17876835.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Lacroix M (2006). "Significance, detection and markers of disseminated breast cancer cells". Endocr Relat Cancer. 13 (4): 1033–67. doi:10.1677/ERC-06-0001. PMID 17158753.
- ^ "The History of Cancer". American Cancer Society. 2002-03-25. Retrieved 2006-10-09.
- ^ [2]
- ^ James S. Olson. "Bathsheba's Breast: Women, Cancer, and History", 1st edition, The Johns Hopkins University Press, 2005 [ISBN-10: 0801880645. ISBN-13: 978-0801880643]
- ^ "Breast Cancer Awareness Month". Retrieved 2008-01-04.
- ^ "Pink Ribbon". Retrieved 2008-01-04.
- ^ "Pink for October". Retrieved 2008-01-04.
- ^ "Index of Saints". Catholic Forum. Retrieved 2008-01-04.
- ^ cite web | title = About Our Ribbon | url = http://www.johnwnickfoundation.org/pinkandblueribbon.html | accessdate = 2008-09-17 }}</
- Arthur, Joyce (2002-03). "Abortion and Breast Cancer — A Forged Link". The Humanist. Retrieved 2007-11-03.
{{cite web}}: Check date values in:|date=(help) - Ressler, Kelly-Anne (2002-08). "Information for GPs – Alcohol and cancer risk" (PDF). Cancer Control Program. South Eastern Sydney and Illawarra Area Health Service. Retrieved 2007-11-03.
{{cite web}}: Check date values in:|date=(help) - "Surgery choices for women with early-stage Breast cancer" (PDF). National Cancer Institute. United States Department of Health and Human Services. Retrieved 2007-11-03.
- Napieralski, Julie A. (1988-03). "Alcohol and the Risk of Breast Cancer". Program on Breast Cancer and Environmental Risk Factors in New York State. Cornell University. Retrieved 2007-11-03.
{{cite web}}: Check date values in:|date=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - "Breast cancer incidence (most recent) by country". NationMaster.com. Retrieved 2007-11-03.
- "Radiology Info - Breast Cancer". Radiological Society of North America. Radiological Society of North America. Retrieved 2007-11-03.
- Zuckerman, Diana. "Mastectomy v. Lumpectomy: Who Decides?". National Research Center for Women & Families. National Research Center. Retrieved 2007-11-03.
External links
Template:Link FA Template:Link FA Template:Link FA
==
Headline text
==
cancer afect on woman