Trisomy X
| Trisomy X | |
|---|---|
| Other names | 47,XXX, triple X syndrome, triplo-X syndrome, XXX syndrome |
 | |
| Three girls with trisomy X | |
| Specialty | Medical genetics |
| Symptoms | Tall stature, skeletal anomalies, minor neurocognitive and behavioural difficulties |
| Usual onset | Conception |
| Duration | Lifelong |
| Causes | Nondisjunction |
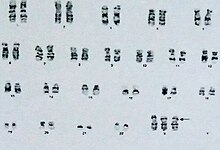
| Diagnostic method | Karyotype |
Trisomy X, also known as triple X syndrome and characterized by the karyotype[note 1] 47,XXX, is a chromosome disorder in which a female has an extra copy of the X chromosome. A relatively common disorder occurring in 1 in 1,000 women, trisomy X is rarely diagnosed; fewer than 10% of those with the condition know they have it. Diagnosis of trisomy X is complicated by its mild presentation; many girls and women with an extra X chromosome show no symptoms significant enough to inspire formal testing.
Symptoms of trisomy X include learning disabilities, mild dysmorphic features such as hypertelorism (wide-spaced eyes) and clinodactyly (incurved pinky fingers), early menopause, and increased height, with an average height around 172 cm (5 ft 7+1⁄2 in). The average IQ in trisomy X is 85–90, compared to 100 in the general population. As the symptoms of trisomy X are often not serious enough to inspire a karyotype test, many cases of trisomy X are diagnosed before birth via prenatal screening tests such as amniocentesis; research on girls and women with the disorder find that cases which were diagnosed postnatally, having been referred for karyotype by obvious symptoms, are generally more severe than those diagnosed prenatally. Most women with trisomy X live normal lives, although their socioeconomic status is reduced compared to the population as a whole.
Trisomy X occurs via a process called nondisjunction, where the normal process of cell division is interrupted and produces gametes with too many or too few chromosomes. Nondisjunction is a random occurrence, and most girls and women with trisomy X have no family histories of chromosome aneuploidy.[note 2] Advanced maternal age is mildly associated with trisomy X. Women with trisomy X can have children of their own, who in most cases do not have an increased risk of chromosome disorders; women with mosaic trisomy X, who have a mix of 46,XX and 47,XXX cells, may have an increased risk of chromosomally abnormal children.
First diagnosed in 1959, the early understanding of trisomy X was that of a debilitating disability observed in institutionalized disabled or mentally ill women. Beginning in the 1960s, cohort studies following people with sex chromosome aneuploidies from birth to adulthood found that people with these disorders are often mildly affected, fitting in with the general population, and that many cases never come to diagnostic attention.
Presentation
Trisomy X has a variable phenotype, ranging from asymptomatic cases to relatively significant disability, and the clinical portrait is not entirely clear. Nonetheless, a number of consistent physiological, psychological, and developmental traits associated with trisomy X have emerged in the medical literature.[3] Several factors can affect the presentation of trisomy X, including mosaicism,[4] and severity is known to vary between prenatally and postnatally diagnosed cases, with postnatal cases having more severe phenotypes on average.[5] Symptoms associated with trisomy X include tall stature, mild developmental delay, subtle physical and skeletal anomalies, increased rates of mental health concerns, and earlier age of menopause.[3][6]
Physiological
Trisomy X has a number of physical and physiological impacts, most of which are quite subtle.[3] Tall stature is one of the major physical associations of trisomy X, although its presentation varies throughout the lifespan. Prior to the age of four, most girls with trisomy X are of average height; growth picks up after this age, being particularly rapid between the ages of four and eight. 40% of girls with trisomy X aged six to thirteen are above the 90th percentile in height.[6] The average height in trisomy X is almost one standard deviation above the norm.[7][8] The height excess in trisomy X is primarily in the limbs, with long legs and a shorter sitting height.[3] Though head circumference is generally below the 50th percentile,[6] frank microcephaly with head circumference below the 5th percentile is rare.[3] The average adult height has been estimated as 172 cm (5 ft 7+1⁄2 in) and head circumference as 20th percentile.[9][note 3]
Minor skeletal and craniofacial anomalies are associated with trisomy X. One study found a tendency toward a shorter facial length and overall reduction in craniofacial growth.[12] Subtle dysmorphisms seen in some females with trisomy X include hypertelorism (wide-spaced eyes), epicanthic folds, and upslanting palpebral fissures. These differences are usually minor and do not have an impact on the daily lives of girls and women with the condition.[3] Dental abnormalities are associated with sex chromosome aneuploidy, including trisomy X; taurodontism, where the pulp of the teeth extends into the roots,[13] increased enamel thickness, and increased root length have all been connected to the condition.[14] Other skeletal anomalies associated with trisomy X include clinodactyly (incurved pinky fingers), radioulnar synostosis (the fusion of the long bones in the forearm),[15] flat feet, and hyper-extensible joints.[16] These findings are not unique to trisomy X, but rather are seen in sex chromosome aneuploidy disorders as a whole.[17]
Severe internal disease is rare in trisomy X; although heart defects are common in some more severe X-chromosome polysomy conditions,[18] they are no more frequent in trisomy X than the general population.[6] Nonetheless, some such conditions appear more frequent in the karyotype. Genitourinary conditions are more common than in the general population, particularly kidney malformations,[3] although severe malformations are uncommon.[19] Autoimmune disorders, particularly lupus, are more common in trisomy X than in the general population.[20][21] Conditions such as sleep apnea, asthma, scoliosis, and hip dysplasia have also been linked to sex chromosome aneuploidies as a whole, including trisomy X.[17]
Puberty starts around the expected age and progresses as normal.[22] Precocious puberty has been reported,[6][23] but is not considered a characteristic of the syndrome.[3] Endocrinological research in trisomy X is sparse, but implies a high luteinizing hormone response.[6][24] Fertility is thought to be normal when not complicated by early menopause;[3] a large population study found women with 47,XXX karyotypes to average 1.9 lifetime pregnancies, compared to 2.3 for women with 46,XX karyotypes, and to be no more likely to miscarry.[8] Premature ovarian failure (POF), or early menopause, is a known complication of trisomy X. Premature ovarian failure is defined as menopause before the age of 40; in the general population, 1 in 100 women experience menopause before this age, 1 in 1,000 before age 30, and 1 in 10,000 before age 20. Amongst women with POF, 3% have trisomy X, compared to 1 in 1,000 in the general population.[25] The average age of menopause for women with trisomy X is 45 years, compared to 50 years for women with 46,XX karyotypes.[8] POF is more common in women with trisomy X who also have autoimmune disorders.[3]
Neurodevelopmental

General cognitive functioning is reduced in trisomy X, with an average intelligence quotient of 85–90 compared to 100 in the general population.[3] Performance IQ tends to be higher than verbal IQ.[26] Though intellectual disability is rare, it is more prevalent than in the general population, occurring in about 5–10% of females with trisomy X[3] compared to approximately 1% of the broader population.[27] Although the average is depressed, some women with trisomy X are highly intelligent,[28] and some patients in the medical literature have acquired advanced degrees or worked in cognitive fields.[26]
Infant milestones are normal to slightly delayed. A patient support organization reports crawling around the age of ten months and walking around sixteen to eighteen months, with first words acquired shortly after one year of age and fluent speech around age two.[22] Speech therapy is indicated for between 40% and 90% of girls with trisomy X.[26] Expressive language skills tend to be more affected than receptive skills.[29]
Neuroimaging in trisomy X demonstrates decreased whole brain volumes, correlated with overall intellectual functioning. Amygdala volume may also be smaller than expected after controlling for whole brain size. White matter abnormalities have been reported, although their significance is unknown. These findings are common to X-chromosome polysomy syndromes, being seen in males with Klinefelter syndrome.[3][26] A minority[6] of patients have epilepsy or electroencephalogram abnormalities,[30] particularly partial seizures; these findings may be more common in intellectually disabled patients.[3][31] Epilepsy in sex chromosome aneuploidies generally is mild, amenable to treatment, and often attenuates or disappears with time. Tremor is reported in approximately a quarter of women with trisomy X and responds to the same treatments as in the general population.[32]
Autism spectrum disorders are more common in trisomy X, occurring in approximately 15% of patients[29] compared to less than 1% of girls in the general population.[33] Adult women with trisomy X appear to have higher rates of autistic symptomatology than control women.[34] Executive dysfunction is more prevalent amongst those with trisomy X than the general population.[26][29]
Psychological
The psychological portrait of trisomy X is not entirely clear, and appears to be complicated by a more severe phenotype in postnatally than prenatally diagnosed groups.[22] Studies indicate a generally shy and placid personality tendency with low self-esteem,[35][36] which is also observed in other X-chromosome polysomies.[37] These traits vary in severity; though some women with trisomy X are significantly impaired, many are within the normal range of variance, and some are high-functioning and high-achieving.[28]
Some mental health diagnoses are more frequent in women with trisomy X. Dysthymia and cyclothymia are more common than in the general population.[3][6] Compared to control women, women with trisomy X average higher schizotypy, reporting higher levels of introversion, magical thinking, and impulsivity.[26] Approximately one-fifth of women with trisomy X report clinically significant levels of anxiety.[29] Women with trisomy X are often "late bloomers", experiencing high rates of psychological distress into early adulthood, but by their mid-thirties having stronger interpersonal bonds and healthy relationships.[26]
Sex chromosome aneuploidies are associated with psychosis, and schizophrenic women are more likely to have trisomy X than the general female population.[38] The prevalence of trisomy X in women with adult-onset schizophrenia is estimated to be around 1 in 400, compared to 1 in 1,000 in women as a whole; the prevalence in childhood onset schizophrenia is unclear, but may be as high as 1 in 40.[39] Schizophrenia in trisomy X may be associated with intellectual disability.[40][41]
The study of mental health in trisomy X is impacted by an apparent gap in severity between prenatal and postnatal diagnosis. For instance, psychogenic stomach pains are reported in a disproportionate number of postnatally diagnosed patients, but fewer prenatally diagnosed ones.[22] Studies comparing prenatally and postnatally diagnosed cases of trisomy X find differences in severity on a number of medical, neurological, and psychological features, including verbal intelligence and adaptive functioning.[5]
The psychosocial adaptation of girls and women with trisomy X is dependent on environmental factors. Girls growing up in stable environments with healthy home lives tend to have relatively high adaptive and social functioning, while significant behavioural and psychological issues are predominantly seen in cases from troubled social environments.[6] Though girls with trisomy X usually have good relationships with peers, they trend towards immaturity;[26] behavioural issues in children with trisomy X are thought to be a consequence of the disconnect between apparent age, as understood via increased height, and cognitive and emotional maturity encouraging hard-to-reach expectations.[6]
Mosaic forms
The most common karyotype in trisomy X is 47,XXX, where all cells have an additional copy of the X chromosome. Mosaicism, where both 47,XXX and other cell lines are present, occurs in approximately 10% of cases. Mosaic trisomy X has different outcomes to the non-mosaic condition, depending on the exact cell lines involved. Common mosaic forms observed include 46,XX/47,XXX, 45,X0/47,XXX (with a Turner syndrome cell line), and 47,XXX/48,XXXX (with a tetrasomy X cell line). Complex mosaicism, with cell lines such as 45,X0/46,XX/47,XXX, can also be seen.[3]
46,XX/47,XXX
The simplest form of mosaic trisomy X, with a 46,XX/47,XXX karyotype, has an attenuated presentation compared to full trisomy X. Cognitive development is more typical, with improved long-term life outcomes. Although the general profile is milder than that of a non-mosaic 47,XXX karyotype, 46,XX/47,XXX mosaicism is associated with a higher risk of chromosome anomalies in offspring than full trisomy X; some writers have recommended screening during pregnancy. The increased risk of abnormal offspring in mosaicism has been hypothesized to be a consequence of oocyte abnormality in 46,XX/47,XXX women not seen in full 47,XXX.[3][42][43]
45,X0/47,XXX
Between 3% and 15% of females with Turner syndrome, defined by a karyotype with a single copy of the X chromosome, have a 47,XXX cell line.[3][44] Mosaic karyotypes with both 45,X0 and 47,XXX cells are considered cases of Turner syndrome rather than trisomy X, but trisomy X mosaicism has a significant impact on the Turner syndrome phenotype. Non-mosaic Turner syndrome is characterized by failure to begin or complete puberty and primary amenorrhea, while 80–90% of women with 45,X0/47,XXX mosaicism begin puberty naturally and approximately 60–80% have spontaneous menses.[44][45] Around two-thirds of 45,X0/47,XXX mosaics have clinically significant short stature, compared with virtually all women with non-mosaic Turner syndrome.[45]
Turner syndrome is characteristically associated with sterility, and only 2% of women with Turner's, including mosaic cases, are capable of becoming pregnant. Turner's women with 47,XXX cell lines are more likely to be fertile than the condition as a whole, more likely to have live births, and more likely to have children with normal karyotypes; in one exceptional case, a woman with a 45,X0/46,XX/47,XXX karyotype had fourteen pregnancies with six live children, including a daughter with Turner syndrome.[46] The proportion of patients with this mosaicism who are capable of having children is unclear, as the medical literature is thought to overrepresent women with reproductive potential due to their clinical exceptionality. Women with the mosaicism experience premature ovarian failure; a literature review found the average age of menopause to be 28, with the onset of likely perimenopausal irregular menses occurring around age 22.[45]
Outside of sexual development and fertility, the impact of a 47,XXX cell line in Turner syndrome is little understood. Although women with trisomy X have lower IQs than the general population and women with Turner syndrome do not, intellectual disability does not appear to be more common in the mosaicism than for non-mosaic Turner's.[47] Mosaic patients tend to have similar dysmorphic features to those observed in non-mosaic Turner's patients, but less marked, and some have none of the traditional Turner's stigmata.[48]
47,XXX/48,XXXX
Mosaicism with a tetrasomy X cell line generally presents closer to the phenotype of tetrasomy than trisomy X.[49] Like trisomy X, tetrasomy X has a variable phenotype muddled by underdiagnosis. The tetrasomy is generally more severe than the trisomy; intellectual disability is characteristic, dysmorphic features more visible, and puberty often altered.[3][18][50]
Causes
Trisomy X, like other aneuploidy disorders, is caused by a process called nondisjunction. Nondisjunction occurs when homologous chromosomes or sister chromatids fail to separate properly during meiosis, the process that produces gametes (eggs or sperm), and result in gametes with too many or too few chromosomes.[51] Nondisjunction can occur during gametogenesis, where the trisomy is present from conception, or zygote development, where it occurs after conception.[3] When nondisjunction occurs after conception, the resulting karyotype is generally mosaic, with both 47,XXX and other cell lines.[52]
The majority of trisomy X occurs through maternal nondisjunction, with around 90% of cases being traced to errors in oogenesis.[53] The vast majority of cases of trisomy X occur randomly; they have nothing to do with the chromosomes of the parents and little chance of recurring in the family.[22] Nondisjunction is related to advanced maternal age, and trisomy X specifically appears to have a small but significant maternal age effect. In a cohort of women with trisomy X born in the 1960s, the average maternal age was 33.[3] Compared to other disorders such as Down syndrome or Klinefelter syndrome, the effect of maternal age in trisomy X is less understood.[6][54][55]
The risk of women with full trisomy X having chromosomally abnormal children is low, likely below 1%. However, mosaic trisomy X is associated with a higher rate of offspring with chromosomal disorders.[3] In the vast majority of cases, trisomy X occurs randomly and has nothing to do with the chromosomes of the parents, and little chance of recurring in the family. Recurrence may occur if the mother has mosaicism for trisomy X, particularly in ovarian cells, but this makes up a small fraction of cases.[22]
Diagnosis and differential diagnosis
Chromosome aneuploidies such as trisomy X are diagnosed via karyotype,[56] the process in which chromosomes are tested from blood, bone marrow, amniotic fluid, or placental cells.[57] As trisomy X generally has a mild or asymptomatic phenotype, most cases are never diagnosed. It is estimated that around 10% of cases of trisomy X are diagnosed in their lifetimes; many cases are ascertained coincidentally during prenatal testing via amniocentesis or chorionic villi sampling, which is routinely performed for advanced maternal age.[3] Indications for postnatal testing for trisomy X include tall stature,[58] hypotonia, developmental disability or neurodivergence, mild dysmorphic features such as hypertelorism or clinodactyly, and premature ovarian failure.[3] As postnatal karyotyping generally occurs in the setting of clinical concern, postnatally diagnosed trisomy X tends to have a more severe phenotype than prenatal.[5][22]
Cases of trisomy X with more severe phenotypes can pose a problem for differential diagnosis. Tetrasomy X, characterized by four copies of the X chromosome, is a particular differential diagnosis of trisomy X. Intellectual disability, generally mild, is more frequently seen in the tetrasomy than the trisomy. There is more of a tendency towards noticeable dysmorphic features such as hypertelorism, clinodactyly, and epicanthic folds. Unlike trisomy X, approximately half of women with tetrasomy X have no or incomplete pubertal development. Although in most cases tetrasomy X is significantly more severe than trisomy X, some cases of tetrasomy X have mild phenotypes, and some cases of trisomy X severe ones. Like trisomy X, the full phenotypic range of tetrasomy X is unknown due to underdiagnosis.[15][59] Pentasomy X, with five X chromosomes, may rarely be a differential diagnosis for trisomy X. The phenotype of pentasomy X is more severe than the trisomy or tetrasomy, with significant intellectual disability, heart defects, microcephaly, and short stature.[7][15]
Due to overlapping dysmorphic features, such as epicanthic folds and upslanting palpebral fissures, some cases of trisomy X may be ascertained due to suspicion of Down syndrome.[3] A phenotype with some similarities to Down syndrome is more frequent in tetrasomy than trisomy X.[60]
When the primary presenting symptom is tall stature, trisomy X may be considered alongside other conditions depending on the rest of the phenotype. Marfan syndrome may be considered due to the disproportion between limb and torso length observed in both syndromes, as well as the joint issues. Beckwith-Wiedemann syndrome, another disproportionate tall stature syndrome, can be associated with developmental disability similar to that seen in some cases of trisomy X.[58]
As karyotypic diagnosis is conclusive, differential diagnosis can be abandoned after karyotype in most cases of trisomy X. However, due to the relatively high prevalence of trisomy X, other congenital disorders may occur comorbid with a 47,XXX karyotype. Differential diagnosis remains indicated when the phenotype is particularly severe for what a 47,XXX karyotype alone explains, such as in the setting of severe intellectual disability or significant malformation.[3]
Prognosis
"My doctor told us that if our unborn daughter had to have a genetic issue, Trisomy X is the one to have, so to speak. He said that many girls with this condition are completely normal, and that it is not physically noticeable. The issues that we could have might be with speech and motor delays, or learning disabilities. [...] The doctor did have us speak with a genetic counselor, but no one encouraged us to terminate and we did not consider it."
Parent of a daughter with trisomy X[61]
The prognosis of trisomy X is, broadly speaking, good, and adult independence, while oft-delayed, is generally achieved. The majority of adults are able to achieve normal life outcomes, pursuing education, employment, or homemaking.[61] Adult employment is generally in lower-skill pink-collar occupations,[6][62] with reduced household income compared to women as a whole,[8] and unemployment or underemployment is more common than expected amongst women with trisomy X who hold higher education qualifications.[63]
Childhood and adolescence, particularly in compulsory education, tends to be more difficult for those with trisomy X than adult life. Parents report their daughters struggling both academically and socially at school,[64] particularly during secondary education,[61] while adults report better adaptation after leaving education and entering the workforce.[6] Of the women in the cohort studies followed to early adulthood, seven of 37 dropped out of high school, while three attended university.[6] A literature review found that compared to age-matched women in the general population, women with trisomy X are 68% as likely to live with a partner, 64% as likely to have children, 36% as likely to hold higher education qualifications, and almost twice as likely to be retired from the workforce.[65]
Physical health is generally good, with many women with trisomy X living into old age.[22] Little data exists on aging in trisomy X.[6] Data from the Danish Cytogenetic Central Register, which covers 13% of women with trisomy X in Denmark,[66] suggests a life expectancy of 71 for women with full trisomy X and 78 for mosaics.[67] The limited sample, composed only of women with trisomy X who have come to medical attention, has led to speculation this number is an underestimate.[65]
Women with trisomy X who were diagnosed prenatally have better outcomes as a group than those diagnosed postnatally, and 46,XX/47,XXX mosaics better than those with full trisomy X.[3] Some of the improved outcome in prenatal diagnosis appears to be a function of higher socioeconomic status amongst parents.[6]
Epidemiology
Trisomy X is a relatively common genetic disorder, occurring in around 1 in 1,000 female births. Despite this prevalence, only around 10% of cases are diagnosed during their lifetime.[3] Large cytogenetic studies in Denmark find a diagnosed prevalence of 6 in 100,000 females, around 7% of the actual number of girls and women with trisomy X expected to exist in the general population.[66] Diagnosis in the United Kingdom is particularly low, with an estimated 2% of cases medically recognized.[65] Amongst the 244,000 women in the UK Biobank research sample, 110 were found to have 47,XXX karyotypes, corresponding to approximately half the number expected in the population. The fact this number is still reduced compared to the broader population is thought to be an effect of UK Biobank participants being less likely to be of low IQ and low socioeconomic status than the general population, both of which are more frequent in trisomy X.[8] Trisomy X's severe underdiagnosis makes it problematic to determine the condition's phenotype, as diagnosed cases are likely more severe than the general 47,XXX population.[65]
Trisomy X only occurs in females, as the Y chromosome is in most cases necessary for male sexual development.[22][note 4]
-
Expected and observed number of people diagnosed with trisomy X and Turner syndrome in Denmark
-
Age at diagnosis for trisomy X, Klinefelter syndrome, and XYY syndrome
History
The first known case of trisomy X, in a 176 cm (5 ft 9+1⁄2 in) woman who experienced premature ovarian failure at the age of 19, was diagnosed in 1959 by a team led by Patricia Jacobs.[71] The late 1950s and early 1960s were a period of frequent ascertainment of previously unknown sex chromosome aneuploidies, with the 47,XXX karyotype discovered alongside 45,X0 and 47,XXY the same year.[72][73] Early studies on sex chromosome aneuploidy screened patients residing in institutions, giving an image of the karyotypes as incapacitating; even at the time, this research was criticized for giving an inaccurate portrait of sex chromosome aneuploidy.[74] Early reports of women with trisomy X have since been criticized for a dehumanizing ableist perspective, showing nude photographs of institutionalized women described as "mental deficiency patients".[63]
In response to the biased early studies, a newborn screening program for sex chromosome aneuploidy disorders was implemented in the 1960s.[75] Almost 200,000 neonates were screened in Aarhus, Toronto, New Haven, Denver, Edinburgh, and Winnipeg; those found to have sex chromosome aneuploidies were followed up for twenty years for most of the cohorts, and longer (until the death of one of the researchers, for Denver[76]) for the Edinburgh and Denver cohorts.[6] The children with trisomy X and Klinefelter's had their karyotypes disclosed to their parents, but due to the then-present perception that XYY syndrome was associated with violent criminality, the diagnosis in that case was hidden from the family.[75]
These cohort studies served to dispell the burgeoning idea that sex chromosome aneuploidies were "tantamount to a life of serious handicaps" and reveal the high prevalence of them in the population.[77] They provided extensive information on the outcomes of trisomy X and other sex chromosome aneuploidies, forming much of the medical literature on the topic to this day. However, the small sample sizes of the long-term follow-ups in particular stymies extrapolation; by 1999, only 16 women in Edinburgh were still being followed.[22] In 2007, rare chromosome disorder organization Unique collaborated with Jacobs and University of Reading pediatrics professor Gary Butler to hold a study day on trisomy X.[78] That same year, Nicole Tartaglia founded the eXtraordinarY Kids Clinic in Denver to study children with sex chromosome aneuploidies; around one-fifth of patients at the clinic have trisomy X as of 2015[update].[17] In 2020, she introduced the eXtraordinarY Babies Study, a planned new cohort study on people prenatally diagnosed with sex chromosome aneuploidies.[79]
The first description of trisomy X used the term 'superfemale' to describe the karyotype by analogy to Drosophilia flies, a term that was immediately disputed. Curt Stern proposed the use of 'metafemale', which Jacobs criticized as both medically inaccurate and an "illegitimate product of a Graeco-Roman alliance". Bernard Lennon, opposing the use of 'superfemale' as misleading and possessed of an inappropriate "emotional element", suggested 'XXX syndrome'.[80][81] For some years, the disorder was predominantly known as 'triple X syndrome' or 'triple X', though the latter in particular is now discouraged.[22]
Society and culture
Diagnosis of sex chromosome aneuploidies is increasing,[17] as is the amount of support available for families.[82] Awareness of these conditions is growing; in the late 2010s, several state governments across the United States declared May to be National X & Y Chromosome Variation Awareness Month.[83][84] The parents and caregivers of children with sex chromosome aneuploidies have created campaigns to raise awareness and increase available support. These campaigns made significant strides over the course of the 2010s to increase awareness,[82] decrease stigma, and improve the state of research.[85]
The literature on trisomy X overwhelmingly considers the karyotype from a medical perspective. Little sociological or educational research exists on trisomy X, a state of affairs criticized by both families and academics.[64] Women with trisomy X discussing their experiences express optimism about the karyotype[76] and hope for other people with it.[86]
In other animals
Trisomy X has been observed in other species that use the XY sex-determination system. Six cases of trisomy X have been recorded in dogs, for which the karyotype is 79,XXX compared to 78,XX for an euploid female dog.[87] Unlike in humans, trisomy X in dogs is strongly linked to infertility, either primary anestrus or infertility with an otherwise normal estrous cycle. Canine trisomy X is thought to be underascertained, as most pet dogs are desexed and so underlying infertility will not be discovered.[88] Three of the six known cases of canine trisomy X demonstrated behavioural issues such as fearfulness, inciting speculation about a link between the karyotype and psychological concerns as seen in humans with the condition. An additional dog with normal fertility and no reported behavioural issues was found to have a mosaic 78,XX/79,XXX karyotype. The canine X chromosome has a particularly large pseudoautosomal region, and dogs accordingly have a lower rate of monosomy X than observed in other species; however, a large pseudoautosomal region is not considered a contraindication for trisomy X, and canine trisomy X may have a comparable prevalence to the human form.[87]
Trisomy X is also observed in cattle, where it corresponds to a 61,XXX karyotype. A survey of 71 heifers who failed to become pregnant after two breeding seasons found two cases of trisomy X.[89] A heifer in another case series of 12 found to have trisomy X was found, on investigation, to have a prepubertal internal reproductive system.[90] In addition to domesticated cattle, trisomy X has been observed in river buffalo, where it is also associated with infertility.[91]
Notes
- ^ 'Karyotype' as a term has multiple meanings, all of which are used here. It may refer to a person's chromosome complement, to the test used to discern said chromosome complement, or to an image of chromosomes ascertained via such a test.[1]
- ^ Aneuploidy is the presence of too many or too few chromosomes in a cell.[2]
- ^ As comparison, the average adult height for women in the Anglosphere is around 162 cm (5 ft 4 in).[10][11]
- ^ Male phenotypes, innate or induced, with forms of X chromosome polysomy that are usually phenotypically female do occur. For trisomy X, a trans man and several men with sex reversal have been recorded.[68][69][70]
References
- ^ Biesecker BB. "Genetics Glossary: Karyotype". National Human Genome Research Institute. Retrieved 24 May 2021.
- ^ Mandrioli D, Belpoggi F, Silbergeld EK, Perry MJ (12 October 2016). "Aneuploidy: a common and early evidence-based biomarker for carcinogens and reproductive toxicants". Environmental Health. 15 (97): 97. doi:10.1186/s12940-016-0180-6. PMC 5059969. PMID 27729050.
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab Tartaglia NR, Howell S, Sutherland A, Wilson R, Wilson L (11 May 2010). "A review of trisomy X (47,XXX)". Orphanet Journal of Rare Diseases. 5 (8): 8. doi:10.1186/1750-1172-5-8. PMC 2883963. PMID 20459843.
- ^ Butnariu L, Rusu C, Caba L, Pânzaru M, Braha E, Grămescu M, Popescu R, Bujoranu C, Gorduza EV (2013). "Genotype-phenotype correlation in trisomy X: a retrospective study of a selected group of 36 patients and review of literature". Medical-Surgical Journal. 117 (3): 714–721. PMID 24502039.
- ^ a b c Wigby K, D'Epagnier C, Howell S, Reicks A, Wilson R, Cordeiro L, Tartaglia N (November 2016). "Expanding the phenotype of Triple X syndrome: A comparison of prenatal versus postnatal diagnosis". American Journal of Medical Genetics Part A. 170 (11): 2870–2881. doi:10.1002/ajmg.a.37688. PMC 6501572. PMID 27644018.
- ^ a b c d e f g h i j k l m n o p q Otter M, Schrander-Stumpel CTRM, Curfs LMG (1 July 2009). "Triple X syndrome: a review of the literature". European Journal of Human Genetics. 18 (3): 265–271. doi:10.1038/ejhg.2009.109. PMC 2987225. PMID 19568271.
- ^ a b Ottesen AM, Aksglaede L, Garn I, Tartaglia N, Tassone F, Gravholt CH, Bojesen A, Sørensen K, Jørgensen N, Rajpert-De Meyts E, Gerdes T, Lind AM, Kjaergaard S, Juul A (May 2010). "Increased number of sex chromosomes affects height in a nonlinear fashion: A study of 305 patients with sex chromosome aneuploidy". American Journal of Medical Genetics Part A. 152A (5): 1206–1212. doi:10.1002/ajmg.a.33334. PMC 5454803. PMID 20425825.
- ^ a b c d e Tuke MA, Ruth KS, Wood AR, Beaumont RN, Tyrrell J, Jones SE, Yaghootkar H, Turner CLS, Donohoe ME, Brooke AM, Collinson MN, Freathy RM, Weedon MN, Frayling TM, Murray A (2019). "Mosaic Turner syndrome shows reduced penetrance in an adult population study". Genetics in Medicine. 21 (4): 877–886. doi:10.1038/s41436-018-0271-6. PMC 6752315. PMID 30181606.
- ^ Jones, Kenneth Lyons; Jones, Marilyn Crandall; del Campo, Miguel (18 August 2013). "Chromosomal Abnormality Syndromes Identifiable on Routine Karyotype". Smith's Recognizable Patterns of Human Malformation (7 ed.). Amsterdam: Elsevier. p. 74. ISBN 9780323638821.
- ^ US Dept. of Health and Human Services; et al. (August 2016). "Anthropometric reference data for children and adults: United States, 2011–2014" (PDF). National Health Statistics Reports. 11. Archived (PDF) from the original on 2 February 2017. Retrieved 23 March 2021.
- ^ "Australian health survey: first results". Australian Bureau of Statistics. 29 October 2012. Archived from the original on 20 January 2017. Retrieved 23 March 2021.
- ^ Krušinskienė V, Alvesalo L, Šidlauskas A (1 August 2005). "The craniofacial complex in 47,XXX females". European Journal of Orthodontics. 27 (4): 396–401. doi:10.1093/ejo/cji016. PMID 16043476.
- ^ Feichtinger C, Rossiwell B (1977). "Taurodontism in human sex chromosome aneuploidy". Archives of Oral Biology. 22 (5): 327–329. doi:10.1016/0003-9969(77)90031-0. PMID 270328.
- ^ Lähdesmäki RE, Alvesalo LJ (23 June 2010). "Root length in the permanent teeth of women with an additional X chromosome (47,XXX females)". Acta Odontologica Scandinavica. 68 (4): 223–227. doi:10.3109/00016357.2010.490954. PMID 20568965. S2CID 19436534.
- ^ a b c NORD, Samango-Sprouse C (2020). "Trisomy X". National Organization for Rare Diseases. Retrieved 10 May 2021.
- ^ Wilson, Rebecca; Bennett, Elizabeth; Howell, Susan E; Tartaglia, Nicole (20 December 2012). "Sex Chromosome Aneuploidies". Psychopathology of Childhood and Adolescence: A Neuropsychological Approach. New York: Springer Publishing. pp. 594–596. ISBN 978-0826109200.
- ^ a b c d Tartaglia N, Howell S, Wilson R, Janusz J, Boada R, Martin S, Frazier JB, Pfeiffer M, Regan K, McSwegin S, Zeitler P (17 July 2015). "The eXtraordinarY Kids Clinic: an interdisciplinary model of care for children and adolescents with sex chromosome aneuploidy". Journal of Multidisciplinary Healthcare. 8 (1): 323–334. doi:10.2147/JMDH.S80242. PMC 4514383. PMID 26229481.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ a b Linden MG, Bender BG, Robinson A (October 1995). "Sex chromosome tetrasomy and pentasomy". Pediatrics. 96 (4): 672–682. PMID 7567329.
- ^ Lin HJ, Ndiforchu F, Patell S (15 March 1993). "Exstrophy of the cloaca in a 47,XXX child: Review of genitourinary malformations in triple‐X patients". American Journal of Medical Genetics. 45 (6): 761–763. doi:10.1002/ajmg.1320450619. PMID 8456857.
- ^ Slae M, Heshin-Bekenstein M, Simckes A, Heimer G, Engelhard D, Eisenstein EM (2014). "Female polysomy-X and systemic lupus erythematosus". Seminars in Arthritis and Rheumatism. 43 (4): 508–512. doi:10.1016/j.semarthrit.2013.07.014. PMID 24012046.
- ^ Liu K, Kurien BT, Zimmerman SL, Kaufman KM, Taft DH, Kottyan LC, Lazaro S, Weaver CA, Ice JA, Adler AJ, Chodosh J, Radfar L, Rasmussen A, Stone DU, Lewis DM, Li S, Koelsch KA, Igoe A, Talsania M, Kumar J, Maier-Moore JS, Harris VM, Gopalakrishnan R, Jonsson R, Lessard JA, Lu X, Gottenberg JE, Anaya JM, Cunninghame-Graham DS, Huang AJW, Brennan MT, Hughes P, Xie G, Ng WF, Nordmark G, Eriksson P, Omdal R, Rhodus NL, Rischmueller M, Rohrer M, Segal BM, Vyse TJ, Wahren-Herlenius M, Witte T, Pons-Estel B, Alarcón-Riquelme M, Guthridge JM, James JA, Lessard CJ, Kelly JA, Thompson SD, Gaffney PM, Montgomery CG, Edberg JC, Kimberly RP, Alarcón GS, Langefeld CL, Gilkeson GS, Kamen DL, Tsao BP, McCune WJ, Salmon JE, Merrill JT, Weisman MH, Wallace DJ, Utset TO, Bottinger EP, Amos CI, Siminovitch KA, Mariette X, Sivils KL, Harley JB, Scofield RH (29 December 2015). "X chromosome dose and sex bias in autoimmune diseases: increased prevalence of 47,XXX in systemic lupus erythematosus and Sjögren's syndrome". Arthritis & Rheumatology. 68 (5): 1290–1300. doi:10.1002/art.39560. PMC 5019501. PMID 26713507.
- ^ a b c d e f g h i j k Unique, Hultén M, Scerif G (2021). "Triple X syndrome, also called Trisomy X" (PDF). Unique. Retrieved 10 May 2021.
- ^ Grosso S, Berardi R, Pucci L, Balestri P (1999). "Precocious puberty in trisomy X syndrome". Obstetrics & Gynecology. 94S (5 Pt 2): 861. doi:10.1097/00006250-199911001-00039. PMID 10546772.
- ^ Stagi S, di Tommaso M, Scalini P, Lapi E, Losi S, Bencini E, Masoni F, Dosa L, Becciani S, de Martino M (4 March 2016). "Triple X syndrome and puberty: focus on the hypothalamus-hypophysis-gonad axis". Fertility and Sterility. 105 (6): 1547–1553. doi:10.1016/j.fertnstert.2016.02.019. PMID 26952785.
- ^ Cordts EB, Christofolini DM, dos Santos AA, Bianco B, Barbosa CP (2011). "Genetic aspects of premature ovarian failure: a literature review". Archives of Gynecology and Obstetrics. 283 (3): 635–643. doi:10.1007/s00404-010-1815-4. PMID 21188402. S2CID 10472263.
- ^ a b c d e f g h Leggett V, Jacobs P, Nation K, Scerif G, Bishop DVM (February 2010). "Neurocognitive outcomes of individuals with a sex chromosome trisomy: XXX, XYY, or XXY: a systematic review". Developmental Medicine and Child Neurology. 52 (2): 119–129. doi:10.1111/j.1469-8749.2009.03545.x. PMC 2820350. PMID 20059514.
- ^ Maulik PK, Mascarenhas MN, Mathers CD, Dua T, Saxena S (April 2011). "Prevalence of intellectual disability: a meta-analysis of population-based studies". Research in Developmental Disabilities. 32 (2): 419–436. doi:10.1016/j.ridd.2010.12.018. PMID 21236634.
- ^ a b Kliegman, Robert M; St. Geme, Joseph (19 April 2019). "Hypofunction of the Ovaries". Nelson Textbook of Pediatrics (21 ed.). Amsterdam: Elsevier. pp. 3005–3006. ISBN 9780323529501.
- ^ a b c d van Rijn S (15 July 2019). "A review of neurocognitive functioning and risk for psychopathology in sex chromosome trisomy (47,XXY, 47,XXX, 47,XYY)". Current Opinion in Psychiatry. 32 (2): 79–84. doi:10.1097/YCO.0000000000000471. PMC 6687415. PMID 30689602.
- ^ Grosso S, Farnetani MA, Di Bartolo RM, Berardi R, Pucci L, Mostardini R, Anichini C, Bartalini G, Galimberti D, Morgese G, Balestri P (2004). "Electroencephalographic and epileptic patterns in X chromosome anomalies". Journal of Clinical Neurophysiology. 21 (4): 249–253. doi:10.1097/00004691-200407000-00003. PMID 15509914. S2CID 23522441.
- ^ Roubertie A, Humbertclaude V, Leydet J, Lefort G, Echenne B (July 2006). "Partial epilepsy and 47,XXX karyotype: report of four cases". Pediatric Neurology. 35 (1): 69–74. doi:10.1016/j.pediatrneurol.2006.01.003. PMID 16814091.
- ^ AXYS, Berry Kravis E (December 2020). "Seizures and tremor in people with X & Y chromosome variations" (PDF). AXYS: Association for X and Y Chromosome Variations. Retrieved 11 May 2021.
- ^ Maenner MJ, Shaw KA, Baio J, Washington A, Patrick M, DiRienzo M, Christensen DL, Wiggins LD, Pettygrove S, Andrews JG, Lopez M, Hudson A, Baroud T, Schwenk Y, White T, Rosenberg CR, Lee LC, Harrington RA, Huston M, Hewitt A, Esler A, Hall-Lande J, Poynter JN, Hallas-Muchow L, Constantino JN, Fitzgerald RT, Zahorodny W, Shenouda J, Daniels JL, Warren Z, Vehorn A, Salinas A, Durkin MS, Dietz PM (27 March 2020). "Prevalence of autism spectrum disorder among children aged 8 years — Autism and Developmental Disabilities Monitoring Network, 11 sites, United States". Morbidity and Mortality Weekly Report: Surveillance Summaries. 69 (4): 1–12. doi:10.15585/mmwr.ss6904a1. PMC 7119644. PMID 32214087.
- ^ Otter M, Crins PML, Campforts BCM, Stumpel CTRM, van Amelsvoort T, Vingerhoets C (15 February 2021). "Social functioning and emotion recognition in adults with triple X syndrome". BJPsych Open. 7 (2): e51. doi:10.1192/bjo.2021.8. PMC 8058878. PMID 33583482.
- ^ Milunsky, Aubrey (2004). "Prenatal Diagnosis of Sex Chromosome Abnormalities". Genetic Disorders and the Fetus: Diagnosis, Prevention, and Treatment (5 ed.). Baltimore: JHU Press. pp. 312–314.
- ^ Tennes K, Puck M, Bryant K, Frankenburg W, Robinson A (1975). "A developmental study of girls with trisomy X". American Journal of Human Genetics. 27 (1): 71–80. PMC 1762786. PMID 1155452.
- ^ Visootsak J, Graham JM (24 October 2006). "Klinefelter syndrome and other sex chromosomal aneuploidies". Orphanet Journal of Rare Diseases. 1 (1): 42. doi:10.1186/1750-1172-1-42. PMC 1634840. PMID 17062147.
- ^ DeLisi LE, Friedrich U, Wahlstrom J, Boccio-Smith A, Forsman A, Eklund K, Crow TJ (1994). "Schizophrenia and sex chromosome anomalies". Schizophrenia Bulletin. 20 (3): 495–505. doi:10.1093/schbul/20.3.495. PMID 7973466.
- ^ Eckstrand K, Addington AM, Stromberg T, Merriman B, Miller R, Gochman P, Long R, Dutra A, Chen Z, Meltzer P, Nelson SF, Rapaport JL (18 September 2008). "Sex chromosome anomalies in childhood onset schizophrenia: an update". Molecular Psychiatry. 13 (10): 910–911. doi:10.1038/mp.2008.67. PMC 4316819. PMID 18800051.
- ^ Turan B, Akıncı MA, Dursun OB, Esin İB (July 2019). "Genetic syndromes as a cause of treatment resistance in schizophrenia: A case with triple X syndrome". İstanbul Tıp Fakültesi Dergisi. 82 (3): 162–163. doi:10.26650/IUITFD.2019.0011.
- ^ Doody GA, Johnstone EC, Sanderson TL, Owens DG, Muir WJ (1998). "'Pfropfschizophrenie' revisited: Schizophrenia in people with mild learning disability". British Journal of Psychiatry. 173 (2): 145–153. doi:10.1192/bjp.173.2.145. PMID 9850227.
- ^ Milunsky, Aubrey (2004). "Prenatal Diagnosis of Sex Chromosome Abnormalities". Genetic Disorders and the Fetus: Diagnosis, Prevention, and Treatment (5 ed.). Baltimore: JHU Press. pp. 313–314.
- ^ Neri G, Opitz JM (1984). "A possible explanation for the low incidence of gonosomal aneuploidy among the offspring of triplo-X individuals". American Journal of Medical Genetics. 18 (2): 357–364. doi:10.1002/ajmg.1320180220. PMID 6465205.
- ^ a b Lim HH, Kil HR, Koo SH (July 2017). "Incidence, puberty, and fertility in 45,X/47,XXX mosaicism: Report of a patient and a literature review". American Journal of Medical Genetics Part A. 173 (7): 1961–1964. doi:10.1002/ajmg.a.38276. PMID 28485514. S2CID 32472061.
- ^ a b c Tang R, Lin L, Guo Z, Hou H, Yu Q (July 2019). "Ovarian reserve evaluation in a woman with 45,X/47,XXX mosaicism: A case report and a review of literature". Molecular Genetics & Genomic Medicine. 7 (7): e00732. doi:10.1002/mgg3.732. PMC 6625135. PMID 31070017.
- ^ Tarani L, Lampariello S, Raguso G, Colloridi F, Pucarelli I, Pasquino AM, Bruni LA (April 1998). "Pregnancy in patients with Turner's syndrome: six new cases and review of literature". Gynecological Endocrinology. 12 (2): 83–87. doi:10.3109/09513599809024955. PMID 9610420.
- ^ Sybert VP (March 2002). "Phenotypic effects of mosaicism for a 47,XXX cell line in Turner syndrome". Journal of Medical Genetics. 39 (3): 217–220. doi:10.1136/jmg.39.3.217. PMC 1735059. PMID 11897829.
- ^ Blair J, Tolmie J, Hollman AS, Donaldson MDC (November 2001). "Phenotype, ovarian function, and growth in patients with 45,X/47,XXX Turner mosaicism: Implications for prenatal counseling and estrogen therapy at puberty". Journal of Pediatrics. 139 (5): 724–728. doi:10.1067/mpd.2001.118571. PMID 11713453.
- ^ Rerrick EG (1970). "Mosaic XXX/XXXX sex chromosome complement case report and review of literature". Journal of Mental Deficiency Research. 14 (2): 141–148. doi:10.1111/j.1365-2788.1970.tb01108.x. PMID 5512214.
- ^ Milunsky, Aubrey (2004). "Prenatal Diagnosis of Sex Chromosome Abnormalities". Genetic Disorders and the Fetus: Diagnosis, Prevention, and Treatment (5 ed.). Baltimore: JHU Press. p. 314.
- ^ Mikwar M, MacFarlane AJ, Marchetti F (4 July 2020). "Mechanisms of oocyte aneuploidy associated with advanced maternal age". Mutation Research/Reviews in Mutation Research. 785: 108320. doi:10.1016/j.mrrev.2020.108320. PMID 32800274.
- ^ Kuliev A, Verlinsky Y (1 October 2004). "Meiotic and mitotic nondisjunction: lessons from preimplantation genetic diagnosis". Human Reproduction Update. 10 (5): 401–407. doi:10.1093/humupd/dmh036. PMID 15319376.
- ^ May KM, Jacobs PA, Lee M, Ratcliffe S, Robinson A, Nielsen J, Hassold TJ (April 1990). "The parental origin of the extra X chromosome in 47,XXX females". American Journal of Human Genetics. 46 (4): 754–761. PMC 1683670. PMID 2316522.
- ^ Dey, Subrata Kumar; Ghosh, Sujoy (29 August 2011). "Etiology of Down Syndrome: Risk of Advanced Maternal Age and Altered Meiotic Recombination for Chromosome 21 Nondisjunction". Genetics and Etiology of Down Syndrome. London: IntechOpen. pp. 23–31. ISBN 978-953-307-631-7.
- ^ Bojesen A, Juul S, Gravholt GH (1 February 2003). "Prenatal and Postnatal Prevalence of Klinefelter Syndrome: A National Registry Study". Journal of Clinical Endocrinology & Metabolism. 88 (2): 622–626. doi:10.1210/jc.2002-021491. PMID 12574191.
- ^ O'Connor C (2008). "Chromosomal abnormalities: aneuploidies". Nature Education. Archived from the original on 3 November 2020. Retrieved 16 May 2021.
- ^ Edens Hurst AC, Zieve D, Conaway B (2 April 2021). "Karyotyping". MedlinePlus. Retrieved 16 May 2021.
- ^ a b Corredor B, Dattani M, Gertosio C, Bozzola M (February 2019). "Tall stature: a challenge for clinicians". Current Pediatric Reviews. 15 (1): 10–21. doi:10.2174/1573396314666181105092917. PMC 6696825. PMID 30394212.
- ^ Unique, Rooman R, Hultén M (2005). "Tetrasomy X" (PDF). Unique. Archived (PDF) from the original on 18 March 2021. Retrieved 16 May 2021.
- ^ Telfer MA, Richardson CE, Helmken J, Smith GF (May 1970). "Divergent phenotypes among 48,XXXX and 47,XXX females". American Journal of Human Genetics. 22 (3): 326–335. PMC 1706538. PMID 4392739.
- ^ a b c Isaacs Cover, Virginia (2012). "Trisomy X, Tetrasomy X and Pentasomy X". Living with Klinefelter Syndrome (47,XXY) Trisomy X (47, XXX) and 47, XYY: A Guide for Families and Individuals Affected by Extra X and Y Chromosome Variations. Altona, Manitoba: Friesens. pp. 107–114. ISBN 978-0-615-57400-4.
- ^ Bender BG, Harmon RJ, Linden MG, Bucher-Bartelson B, Robinson A (16 April 1999). "Psychosocial competence of unselected young adults with sex chromosome abnormalities". American Journal of Medical Genetics. 88 (2): 200–206. doi:10.1002/(sici)1096-8628(19990416)88:2<200::aid-ajmg18>3.0.co;2-3. PMID 10206242.
- ^ a b Attfield K (25 January 2021). "Triple X superwomen: their post-compulsory education and employability". Journal of Education and Work. 34 (1): 81–94. doi:10.1080/13639080.2021.1875126. S2CID 231990866.
- ^ a b Attfield K (25 May 2020). "Triple X supergirls: Their special educational needs and social experience". International Journal of Educational Research. 102 (1): 101588. doi:10.1016/j.ijer.2020.101588.
- ^ a b c d Berglund A, Stochholm K, Gravholt CH (2020). "The epidemiology of sex chromosome abnormalities". American Journal of Medical Genetics Part C: Seminars in Medical Genetics. 184 (2): 202–215. doi:10.1002/ajmg.c.31805. PMID 32506765. S2CID 219537282.
- ^ a b Berglund A, Viuff MN, Skakkebæk A, Chang S, Stochholm K, Gravholt CH (2019). "Changes in the cohort composition of Turner syndrome and severe non-diagnosis of Klinefelter, 47,XXX and 47,XYY syndrome: a nationwide cohort study". Orphanet Journal of Rare Diseases. 14 (1): 16. doi:10.1186/s13023-018-0976-2. PMC 6332849. PMID 30642344.
- ^ Stochholm K, Juul S, Gravholt CH (2010). "Mortality and incidence in women with 47,XXX and variants". American Journal of Medical Genetics Part A. 152A (2): 367–372. doi:10.1002/ajmg.a.33214. PMID 20101696. S2CID 12004487.
- ^ Turan MT, Eşel E, Dündar M, Candemir Z, Baştürk M, Sofuoğlu S, Özkul Y (1 December 2000). "Female-to-male transsexual with 47,XXX karyotype". Biological Psychiatry. 48 (1): 1116–1117. doi:10.1016/S0006-3223(00)00954-9. PMID 11094147. S2CID 16396520.
- ^ Ogata T, Matsuo M, Muroya K, Koyama Y, Fukutani K (1 February 2001). "47,XXX male: A clinical and molecular study". American Journal of Medical Genetics. 98 (4): 353–356. doi:10.1002/1096-8628(20010201)98:4<353::AID-AJMG1110>3.0.CO;2-D. PMID 11170081.
- ^ Müller U, Latt SA, Donlon T, Opitz JM (October 1987). "Y‐specific DNA sequences in male patients with 46,XX and 47,XXX karyotypes". American Journal of Medical Genetics. 28 (2): 393–401. doi:10.1002/ajmg.1320280218. PMID 2827475.
- ^ Jacobs PA, Baikie AG, Court Brown WM, MacGregor TN, Harnden DG (26 September 1959). "Evidence for the existence of the human 'super female'". Lancet. 274 (7100): 423–425. doi:10.1016/S0140-6736(59)90415-5. PMID 14406377.
- ^ Ford CE, Jones KW, Polani PE, de Almeida JCC, Briggs JH (1959). "A sex-chromosome anomaly in a case of gonadal dysgenesis (Turner's syndrome)". Lancet. 273 (7075): 711–713. doi:10.1016/S0140-6736(59)91893-8. PMID 13642858.
- ^ Jacobs PA, Strong JA (31 January 1959). "A case of human intersexuality having a possible XXY sex-determining mechanism". Nature. 183 (4657): 302–303. Bibcode:1959Natur.183..302J. doi:10.1038/183302a0. PMID 13632697. S2CID 38349997.
- ^ Barr ML, Sergovich FR, Carr DH, Saver EL (6 September 1969). "The triplo-X female: an appraisal based on a study of 12 cases and a review of the literature". Canadian Medical Association Journal. 101 (5): 247–258. PMC 1946229. PMID 5812107.
- ^ a b Ratcliffe S (1999). "Long term outcome in children of sex chromosome abnormalities". Archives of Disease in Childhood. 80 (2): 192–195. doi:10.1136/adc.80.2.192. PMC 1717826. PMID 10325742.
- ^ a b Odle, Christine. "The story of Christine, born in 1967, dx shortly after birth". Triple-X Syndroom. Retrieved 23 May 2021.
- ^ Cohen FL, Durham JD (March 1985). "Sex chromosome variations in school-age children". Journal of School Health. 55 (3): 99–102. doi:10.1111/j.1746-1561.1985.tb04089.x. PMID 3845264.
- ^ "XXX Study Day Report" (PDF). Unique. September 2007. Retrieved 23 May 2021.
- ^ Tartaglia N, Howell S, Davis S, Kowal K, Tanda T, Brown M, Boada C, Alston A, Crawford L, Thompson T, van Rijn S, Wilson R, Janusz J, Ross J (June 2020). "Early neurodevelopmental and medical profile in children with sex chromosome trisomies: Background for the prospective eXtraordinarY Babies Study to identify early risk factors and targets for intervention". American Journal of Medical Genetics Part C: Seminars in Medical Genetics. 184 (2): 428–443. doi:10.1002/ajmg.c.31807. PMC 7413625. PMID 32506668.
- ^ Jacobs PA, Baikie AG, Court Brown WM, Harnden DG, MacGregor TN, MacLean N (19 December 1959). "Use of the term "superfemale"". The Lancet. 274 (7112): 1145. doi:10.1016/S0140-6736(59)90132-1.
- ^ Lennox B (2 January 1960). "Use of the term "superfemale"". The Lancet. 275 (7114): 55. doi:10.1016/S0140-6736(60)92744-6.
- ^ a b Auchmutey, Pam (2018). "Extraordinary Care". Emory Health Digest. Archived from the original on 6 August 2020. Retrieved 23 May 2021.
- ^ "National X & Y Chromosome Variation Awareness Month". AXYS: Association for X and Y Chromosome Variations. Retrieved 23 May 2021.
- ^ Auchmutey, Pam (2018). "Hiding in Plain Sight". Emory Health Digest. Retrieved 23 May 2021.
- ^ Snyder, Lia (9 June 2017). "Engagement Project Yields Unexpected Dividends". Patient-Centered Outcomes Research Institute. Retrieved 23 May 2021.
- ^ MacLean-Cerasoli, Katie. "The story of Katie, born in 1968, dx by amnio". Triple-X Syndroom. Retrieved 23 May 2021.
- ^ a b Szczerbal I, Switonski M (27 March 2021). "Clinical cytogenetics of the dog: a review". Animals. 11 (4): 947. doi:10.3390/ani11040947. PMC 8066086. PMID 33801756.
- ^ O'Connor CL, Schweizer C, Gradil C, Schlafer D, Lopate C, Prociuk U, Meyers-Wallen VN, Casal ML (15 July 2011). "Trisomy-X with estrous cycle anomalies in two female dogs". Theriogenology. 76 (2): 374–380. doi:10.1016/j.theriogenology.2011.02.017. PMC 3115384. PMID 21550105.
- ^ Swartz HA, Vogt DW (September 1983). "Chromosome abnormalities as a cause of reproductive inefficiency in heifers". Journal of Heredity. 74 (5): 320–324. doi:10.1093/oxfordjournals.jhered.a109802.
- ^ Pinheiro LEL, Almeida IL, Garcia JM, Basrur PK (December 1987). "Trisomy X and 129 translocation in infertile heifers". Theriogenology. 28 (6): 891–898. doi:10.1016/0093-691X(87)90039-2.
- ^ Prakash B, Balain DS, Lathwal SS, Malik RK (5 March 1994). "Trisomy-X in a sterile river buffalo". Veterinary Record. 134 (10): 241–242. doi:10.1136/vr.134.10.241. PMID 8197685. S2CID 361471.
External links
- NLM (2008). Triple X syndrome Genetics Home Reference




