Acne
| Acne | |
|---|---|
| Specialty | Dermatology, family medicine |

Acne vulgaris is an inflammatory disease of the skin, caused by changes in the pilosebaceous units (skin structures consisting of a hair follicle and its associated sebaceous gland). Acne lesions are commonly referred to as pimples, spots or zits.
The condition is common in puberty among Western societies. It is considered an abnormal response to normal levels of the male hormone testosterone. The response for most people diminishes over time and acne thus tends to disappear, or at least decrease, after one reaches their early twenties. There is, however, no way to predict how long it will take for it to disappear entirely, and some individuals will continue to suffer from acne decades later, into their thirties and forties and even beyond. Acne affects a large percentage of humans at some stage in life.
The term acne comes from a corruption of the Greek άκμή (acme in the sense of a skin eruption) in the writings of Aëtius Amidenus.
Symptoms
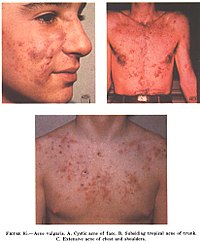
The most common form of acne is known as "acne vulgaris", meaning "common acne." Excessive secretion of oils from the glands combines with naturally occurring dead skin cells to block the hair follicles. Oil secretions build up beneath the blocked pore, providing a perfect environment for the skin bacteria Propionibacterium acnes to multiply uncontrolled. In response, the skin inflames, producing the visible lesion. The face, chest, back, shoulders and upper arms are especially affected.
The typical acne lesions are: comedones, papules, pustules, nodules and inflammatory cysts. These are the more inflamed form of pus-filled or reddish bumps, even boil-like tender swellings. Non-inflamed 'sebaceous cysts', more properly called epidermoid cysts, occur either in association with acne or alone but are not a constant feature. After resolution of acne lesions, prominent unsightly scars may remain.
Aside from scarring, its main effects are psychological, such as reduced self-esteem and depression. Acne usually appears during adolescence, when people already tend to be most socially insecure.
Causes of acne
Exactly why some people get acne and some do not is not fully known. It is known to be partly hereditary. Several factors are known to be linked to acne:
- Hormonal activity, such as menstrual cycles and puberty
- Stress, through increased output of hormones from the adrenal (stress) glands.
- Hyperactive sebaceous glands, secondary to the three hormone sources above.
- Accumulation of dead skin cells.
- Bacteria in the pores, to which the body becomes 'allergic'.
- Skin irritation or scratching of any sort will activate inflammation.
- Use of anabolic steroids.
- Any medication containing halogens (iodides, chlorides, bromides), lithium, barbiturates, or androgens.
- Exposure to high levels of chlorine compounds, particularly chlorinated dioxins, can cause severe, long-lasting acne, known as Chloracne.
Traditionally, attention has focused mostly on hormone-driven over-production of sebum as the main contributing factor of acne. More recently, more attention has been given to narrowing of the follicle channel as a second main contributing factor. Abnormal shedding of the cells lining the follicle, abnormal cell binding ("hyperkeratinization") within the follicle, and water retention in the skin (swelling the skin and so pressing the follicles shut) have all been put forward as mechanisms involved.
Several hormones have been linked to acne: the male hormones testosterone, dihydrotestosterone (DHT) and dehydroepiandrosterone sulfate (DHEAS), as well as insulin-like growth factor 1 (IGF-I). In addition, acne-prone skin has been shown to be insulin resistant.
Development of acne vulgaris in latter years is uncommon, although this is the age group for Rosacea which may have similar appearances. True acne vulgaris in older adults may be a feature of an underlying condition such as pregnancy and disorders such as polycystic ovary syndrome or the rare Cushing's syndrome.
Misconceptions about causes
There are many misconceptions and rumors about what does and does not cause the condition:
- Diet. One flawed study purported that chocolate, french fries, potato chips and sugar, among others, affect acne.[1]A recent review of scientific literature cannot affirm either way.[2]The consensus among health professionals is that acne sufferers should experiment with their diets, and refrain from consuming such fare if they find such food affects the severity of their acne.[3]A recent study, based on a survey of 47,335 women, did find a positive epidemiological association between milk consumption and acne, particularly skimmed.[4]The researchers hypothesize that the association may be caused by hormones (such as bovine IGF-I) present in cow milk; but this has not been definitively shown. Seafood, on the other hand, may contain relatively high levels of iodine, but probably not enough to cause an acne outbreak. Still, people who are prone to acne may want to avoid excessive consumption of foods high in iodine. It has also been suggested that there is a link between a diet high in refined sugars and acne. According to this hypothesis, the startling absence of acne in non-westernized societies could be explained by the low glycemic index of these tribes' diets.[5]Further research is necessary to establish whether a reduced consumption of high-glycemic foods (such as soft drinks, sweets, white bread) can significantly alleviate acne, though consumption of high-glycemic foods should in any case be kept to a minimum, for general health reasons.[6]
- Deficient personal hygiene. Acne is not caused by dirt. This misconception probably comes from the fact that acne involves skin infections. In fact, the blockages that cause acne occur deep within the narrow follicle channel, where it is impossible to wash them away. These plugs are formed by the cells and sebum created there by the body. The bacteria involved are the same bacteria that are always present on the skin. Regular cleansing of the skin can reduce, but not prevent, acne for a particular individual and very little variation among individuals is due to hygiene. Anything beyond very gentle cleansing can actually worsen existing lesions and even encourage new ones by damaging or overdrying skin.
- Sex. Common myths state that either celibacy or masturbation cause acne and, conversely, that sexual intercourse can cure it. There is absolutely no scientific evidence suggesting that any of these are factual. It is true, though, that anger and stress affect hormone levels and thus bodily oil production, which can cause acne.
Treatments
Available treatments
There are many products sold for the treatment of acne, many of them without any scientifically-proven effects. Generally speaking successful treatments give little improvement within the first week or two; and then the acne decreases over approximately 3 months, after which the improvement starts to flatten out. Treatments that promise improvements within 2 weeks are likely to be largely disappointing.
A combination of treatments can greatly reduce the amount and severity of acne in many cases. Those treatments that are most effective tend to have greater potential for side effects and need a greater degree of monitoring, so a step-wise approach is often taken. Many people consult with doctors when deciding which treatments to use, especially when considering using any treatments in combination. There are a number of treatments that have been proven effective:

Exfoliating the skin
This can be done either mechanically, using an abrasive cloth or a liquid scrub, or chemically. Common chemical exfoliating agents include salicylic acid and glycolic acid, which encourage the peeling of the top layer of skin to prevent a build-up of dead skin cells which combine with skin oil to block pores. It also helps to unblock already clogged pores. Note that the word "peeling" is not meant in the visible sense of shedding, but rather as the destruction of the top layer of skin cells at the microscopic level. Depending on the type of exfoliation used, some visible flaking is possible. Moisturizers and anti-acne topicals containing chemical exfoliating agents are commonly available over-the-counter.
Topical Bactericidals
Widely available OTC bactericidal products containing Benzoyl peroxide may be used in mild to moderate acne. The gel or cream containing benzoyl peroxide is rubbed, twice daily, into the pores over the affected region and primarily prevents new lesions by killing P.acnes. Unlike antibiotics, Benzoyl peroxide has the advantage of being a strong oxidiser (essentially a mild bleach) and thus does not appear to generate resistance. However, it routinely causes dryness, local irritation and redness. A sensible regimen may include the use of suitable non-comedogenic moisturisers to help avoid overdrying the skin.[7]
Care must be taken when using Benzoyl peroxide, as it can very easily bleach any fabric or hair it comes in contact with.
Other antibacterials that have been used include triclosan, or chlorhexidine gluconate but these are often less effective.
Topical antibiotics
Externally applied antibiotics such as erythromycin, clindamycin, Stiemycin or tetracycline aim to kill the bacteria that are harbored in the blocked follicles. Whilst topical use of antibiotics is equally as effective as oral, this method avoids possible side effects of stomach upset or drug interactions (e.g. it will not affect the oral contraceptive pill), but may prove awkward to apply over larger areas than just the face alone.

Oral antibiotics
Oral antibiotics used to treat acne include erythromycin or one of the tetracycline antibiotics (tetracycline, the better absorbed oxytetracycline, or one of the once daily doxycycline, minocycline or lymecycline). Trimethoprim is also sometimes used (off-label use in UK). However, reducing the P. acnes bacteria will not, in itself, do anything to reduce the oil secretion and abnormal cell behaviour that is the initial cause of the blocked follicles. Additionally the antibiotics are becoming less and less useful as resistant P. acnes are becoming more common. Acne will generally reappear quite soon after the end of treatment—days later in the case of topical applications, and weeks later in the case of oral antibiotics.
Acunol® is an oral medication indicated for the treatment of mild to moderate acne. It is a new drug developed by a dermatologist.
Hormonal treatments
In females, acne can be improved with hormonal treatments. The normal combined oestrogen/progestogen contraceptive pills have some effect, but the anti-testosterone Cyproterone in combination with an oestrogen (Diane 35) is particularly effective at reducing androgenic hormone levels. Diane-35 is not available in the USA, but a newer oral contraceptive containing the progestin drospirenone is now available with fewer side effects than Diane 35 / Dianette. Both can be used where blood tests show abnormally high levels of androgens, but are effective even when this is not the case.
If a pimple is large and/or does not seem to be affected by other treatments, a dermatologist may administer an injection of cortisone directly into it, which will usually reduce redness and inflammation almost immediately. This has the effect of flattening the pimple, thereby making it easier to cover up with makeup, and can also aid in the healing process. Side effects are minimal, but may include a temporary whitening of the skin around the injection point. This method also carries a much smaller risk of scarring than surgical removal.
External retinoids
Normalizing the follicle cell lifecycle. A group of medications for this are topical retinoids such as tretinoin (brand name Retin-A), adapalene (brand name Differin) and tazarotene (brand name Tazorac). Like isotretinoin, they are related to vitamin A, but they are administered as topicals and generally have much milder side effects. They can, however, cause significant irritation of the skin. The retinoids appear to influence the cell creation and death lifecycle of cells in the follicle lining. This helps prevent the hyperkeratinization of these cells that can create a blockage. Retinol, a form of vitamin A, has similar but milder effects and is used in many over-the-counter moisturizers and other topical products. Effective topical retinoids have been in use over 30 years but are available only on prescription so are not as widely used as the other topical treatments. Topical retinoids often cause an initial flare up of acne within a month or so, which can be severe.
Oral retinoids
Reducing the secretion of oils from the glands. This is done by a daily oral intake of vitamin A derivatives like isotretinoin (marketed as Accutane, Sotret) over a period of 4-6 months. It is believed that isotretinoin works primarily by reducing the secretion of oils from the glands, however some studies suggest that it affect other acne-related factors as well. Isotretinoin has been shown to be very effective in treating severe acne and can either improve or clear well over 80% of patients. The drug has a much longer effect than anti-bacterial treatments and will often cure acne for good. The treatment requires close medical supervision by a dermatologist because the drug has many known side effects (which can be severe). About 25% of patients may relapse after one treatment. In those cases, a second treatment for another 4-6 months may be indicated to obtain desired results. It is often recommended that one lets a few months pass between the two treatments, because the condition can actually improve somewhat in the time after stopping the treatment and waiting a few months also give the body a chance to recover. Occasionally a third or even a fourth course is used, but the benefits are often less substantial. The most common side effects are dry skin and occasional nosebleeds (secondary to dry nasal mucosa). Oral retinoids also often cause an initial flare up of acne within a month or so, which can be severe. There are reports that the drug has damaged the liver of patients. For this reason, it is recommended that patients have blood samples taken and examined before and during treatment. In some cases, treatment is terminated due to changes in various levels of chemicals in the blood, which might be related to liver damage. Others claim that the reports of permanent damage to the liver are unsubstantiated, and routine testing is considered unnecessary by some dermatologists. Blood triglycerides also need to be monitored. However, routine testing are part of the official guidelines for the use of the drug in many countries. Some press reports suggest that isotretinoin may cause depression but as of September 2005 there is no agreement in the medical literature as to the risk. The drug also causes birth defects if women become pregnant while taking it or take it while pregnant. For this reason, female patients are required to use two separate forms of birth control or vow abstinence while on the drug. Because of this, the drug is supposed to be given as a last resort after milder treatments have proven insufficient. Restrictive rules (see iPledge Program) for use were put into force in the USA beginning in March 2006 to prevent misuse.[8] This has occasioned widespread editorial comment.[9]
Phototherapy
It has long been known that short term improvement can be achieved with sunlight. However studies have shown that sunlight worsens acne long-term, presumably due to UV damage. More recently, visible light has been successfully employed to treat acne (Phototherapy) - in particular intense blue light generated by purpose-built fluorescent lighting, dichroic bulbs, LEDs or lasers. Used twice weekly, this has been shown to reduce the number of acne lesions by about 64%;[10] and is even more effective when applied daily. The mechanism appears to be that porphyrins produced within P. acnes generate free radicals when irradiated by blue light.[11] Particularly when applied over several days, these free radicals ultimately kill the bacteria.[12] Since porphyrins are not otherwise present in skin, and no UV light is employed, it appears to be safe, and has been licensed by the U.S. FDA.[13] The treatment apparently works even better if used with red visible light (660 nanometer) resulting in a 76% reduction of lesions after 3 months of daily treatment;[14] and overall clearance was similar or better than benzoyl peroxide. Unlike most of the other treatments few if any negative side effects are typically experienced, and the development of bacterial resistance to the treatment seems very unlikely. After treatment, clearance can be longer lived than is typical with topical or oral antibiotic treatments, several months is not uncommon. However, the equipment or treatment is expensive, although portable home use equipment costs can be very much comparable to Benzoyl Peroxide/moisturiser/cleanser costs over a few years.
In addition, basic science and clinical work by dermatologists Yoram Harth and Alan Shalita and others have shown that intense blue/violet light (405-425 nanometer) can decrease the number of inflammatory acne lesion by 60-70% in 4 weeks of therapy, particularly when the P.acnes is pretreated with delta-aminolevulinic acid (ALA), which increases the production of porphyrins.
Less widely used treatments
- Azelaic acid (brand names Azelex, Finevin, Skinoren) is suitable for mild, comedonal acne.[15]
- Zinc. Orally administered zinc gluconate has been shown to be effective in the treatment of inflammatory acne, although less so than tetracyclines.[16][17]
Alternative treatments
- Nicholas Perricone's controversial book The Acne Prescription proposes an alternative treatment for adult acne, including a strict diet (dairy is totally avoided in all but two recipes) and topicals containing lipoic acid. Perricone's claims did not seem to be backed up by strong scientific evidence until the publication of the acne / milk link in early 2005. There are no double-blind studies proving the effectiveness of fatty acids against acne.
- Popping a pimple or any physical acne treatment creates the risk of irritating the skin and spreading the infection deeper into the skin, which may cause permanent scarring.
- Home remedies: Some people claim that several things in an average kitchen like nutmeg, honey, cinnamon, garlic, orange peel, sandalwood, etc can cure acne. None of these methods have been scientifically proven.
The following treatments are based on a theory that acne is often caused by an imbalance or shortage of certain essential elements (most commonly sulfur, magnesium, and zinc).
- Sulphur - MSM
- Magnesium supplements
- Special electrolyte (salt) solutions
- Chromium - Chromium supplementation appeared to work in a small study.[citation needed]
- Insulin treatment - insulin treatment has been reported to work, although no big studies have been performed
Future treatments
Laser surgery has been in use for some time to reduce the scars left behind by acne, but research is now being done on lasers for prevention of acne formation itself. The laser is used to produce one of the following effects:
- to burn away the follicle sac from which the hair grows
- to burn away the sebaceous gland which produces the oil
- to induce formation of oxygen in the bacteria, killing them
Since lasers and intense pulsed light sources cause thermal damage to the skin there are concerns that laser or intense pulsed light treatments for acne will induce hyperpigmented macules (spots) or cause long term dryness of the skin. As of 2005, this is still mostly at the stage of medical research rather than established treatment.
Because acne appears to have a significant hereditary link, there is some expectation that cheap whole-genome DNA sequencing may help isolate the body mechanisms involved in acne more precisely, possibly leading to a more satisfactory treatment. (Crudely put, take the DNA of large samples of people with significant acne and of people without, and let a computer search for statistically strong differences in genes between the two groups). However, as of 2005 DNA sequencing is not yet cheap and all this may still be decades off. It is also possible that gene therapy could be used to alter the skin's DNA.
Phage therapy has been proposed to kill P.Acnes.
Preferred treatments by types of acne vulgaris
- Comedonal (non-inflammatory) acne: local treatment with azelaic acid, salicylic acid, topical retinoids, benzoyl peroxide.
- Mild papulo-pustular (inflammatory) acne: benzoyl peroxide or topical retinoids, topical antibiotics (such as erythromycin).
- Moderate inflammatory acne: benzoyl peroxide or topical retinoids combined with oral antibiotics (tetracyclines). Isotretinoin is an option.
- Severe inflammatory acne, nodular acne, acne resistant to the above treatments: isotretinoin, or contraceptive pills with cyproterone for females with virilization or drospirenone.
Preferred treatment by location
Acne occurring on the upper back, often referred to by the portmanteau bacne, may prove harder to treat than acne on the face. The greater thickness of the skin over the back may require the use of stronger topical agents. Sometimes oral medication is preferred because an individual may not be able to apply a topical cream to their own back.
Acne scars
Severe acne often leaves small scars where the skin gets a "volcanic" shape. Acne scars are very difficult (and expensive) to treat and it is unusual for the scars to be successfully removed completely. In those cases, scar treatment may be appropriate. The most commonly used forms of scar treatments are:
- Dermabrasion. The top layer of the skin is removed with a high-speed rotary wire brush or diamond-coated fraise (a grinding wheel) to make the scar look less pitted. It makes the scar less visible but does not remove it completely. Multiple treatments may be necessary to get the desired results. This procedure is usually performed by a dermatologist or cosmetic surgeon and is less commonly done now because of the risk of blood-borne diseases.
- Microdermabrasion is a newer technique that has a similar effect to traditional dermabrasion, but is less radical. While dermabrasion is a surgical procedure, microdermabrasion is performed by blasting tiny crystals at the skin or rubbing the skin with a rough tool under suction. Many dermatologists and cosmetic surgeons offer this procedure.
- Laser resurfacing. A laser is used to burn off the top layer of the skin. This procedure is commonly known by the brand names of the machines used to perform it, including SmoothBeam. Many dermatologists and cosmetic surgeons offer this procedure.
- Punch excision. The scar is excised with a punch tool and the edges are sutured together. This procedure is usually performed by a dermatologist or cosmetic surgeon.
- Chemical peels (also known as acid peels). A type of organic acid, most commonly glycolic, salicylic, or lactic, is applied to the skin so that a smoother layer can surface. Despite its unpleasant name, superficial peels are painless if performed properly and require no anaesthetic. Peels are typically performed several times over a period of weeks or months. The procedure can also be beneficial for active acne. Many dermatologists and cosmetologists offer this procedure, although the peels given by dermatologists are generally of a higher concentration and therefore potentially more effective. Deep peels are more aggressive and painful and require significant expertise.
- Subcision. The scar is detached from deeper tissue, allowing a pool of blood to form under the scar which helps form a connective tissue under the scar, levelling it with the surface. This procedure is usually performed by a dermatologist or cosmetic surgeon.
- Dermal filler. The scar is filled with an injectable dermal filler. There are several trade names.
Similar conditions
- Keratosis pilaris is a skin condition that is often confused with acne.
- Rosacea (ro-ZAY-she-ah) sometimes called "Adult Acne" occurs in people of all ages, especially older women when they go through the menopause. Two famous men with the affliction are W.C. Fields and former United States President Bill Clinton. The disorder is characterized by redness, pimples, and, in advanced stages, thickened skin. People who suffer from flushing or blush easily are most at risk of developing rosacea.
Timeline of acne treatment
The history of acne reaches back to the dawn of recorded history. In Anceint Egypt, it is recorded that several pharaohs were acne sufferers. From Ancient Greece, comes the English word 'acne' (meaning 'point' or 'peak'). Acne treatments are also of considerable antiquity:
- Ancient Rome : bathing in hot, and often sulfurous, mineral water was one of the few available acne treatments. One of the earliest texts to mention skin problems is De Medicina by the Roman writer Celsus.
- 1800s: Nineteenth century dermatologists used sulfur in the treatment of acne. It was believed to dry the skin.
- 1930s: laxatives were used as a cure for what were known as 'chastity pimples'
- 1950s When antibiotics became available, it was discovered that they had beneficial effects on acne. They were taken orally to begin with. Topical antibiotics became available later.
- 1960s Vitamin A acid and Retin A were found effective for acne. This led to the development of isotretinoin sold as Accutane and Roaccutane in the 1980's.
- 1990s Laser treatment introduced
Some old treatments, like laxatives, have fallen into disuse but others, like spas, are recovering their popularity.
References
- James W (2005). "Clinical practice. Acne". N Engl J Med. 352 (14): 1463–72. PMID 15814882.
{{cite journal}}: Unknown parameter|month=ignored (help) - Webster G (2002). "Acne vulgaris". BMJ. 325 (7362): 475–9. PMID 12202330.
{{cite journal}}: Unknown parameter|month=ignored (help)
Footnotes
- ^ CHOICE - Citizens for Healthy Options In Children's Education (2003). "Acne Has Nothing to Do with Diet - Wrong!".
{{cite web}}: Unknown parameter|month=ignored (help) - ^ Magin P, Pond D, Smith W, Watson A (2005). "A systematic review of the evidence for 'myths and misconceptions' in acne management: diet, face-washing and sunlight". Fam Pract. 22 (1): 62–70. PMID 15644386.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Fries JH (1978). "Chocolate: a review of published reports of allergic and other deleterious effects, real or presumed". Ann Allergy. 41 (4): 195–207. PMID 152075.
- ^ Adebamowo CA, Spiegelman D, Danby FW, Frazier AL, Willett WC, Holmes MD (2005). "High school dietary dairy intake and teenage acne". J Am Acad Dermatol. 52 (2): 207–14. PMID 15692464.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Loren Cordain, et al. "Acne Vulgaris - A Disease of Western Civilization" Arch Dermatol. 2002;138:1584-1590. Observation
- ^ Smith R, Mann N, Makelainen H, Braue A, Varigos G (2004). "The effect of short-term altered macronutrient status on acne vulgaris and biochemical markers of insulin sensitivity". Asia Pac J Clin Nutr. 13 (Suppl): S67. PMID 15294556.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ 'Clear skin regimen' - How to use benzoyl peroxide to treat acne). Acne. Org instructions
- ^ "The iPLEDGE Program - Guide to Best Practices for Isotretinoin - "The resource to help the prescriber prepare, plan treatments, and prevent pregnancies during the course of isotretinoin therapy"" (PDF). 2005.
- ^ Bernadine Healy (2005-05-09). "Pledging for Accutane". US News Best Health.
{{cite news}}: Check date values in:|date=(help) - ^ Kawada A, Aragane Y, Kameyama H, Sangen Y, Tezuka T (2002). "Acne phototherapy with a high-intensity, enhanced, narrow-band, blue light source: an open study and in vitro investigation". J Dermatol Sci. 30 (2): 129–35. PMID 12413768.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Kjeldstad B (1984). "Photoinactivation of Propionibacterium acnes by near-ultraviolet light". Z Naturforsch [C]. 39 (3–4): 300–2. PMID 6730638.
- ^ Ashkenazi H, Malik Z, Harth Y, Nitzan Y (2003). "Eradication of Propionibacterium acnes by its endogenic porphyrins after illumination with high intensity blue light". FEMS Immunol Med Microbiol. 35 (1): 17–24. PMID 12589953.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ "New Light Therapy for Acne" U.S. Food and Drug Administration, FDA Consumer magazine, November-December 2002 Notice
- ^ Papageorgiou P, Katsambas A, Chu A (2000). "Phototherapy with blue (415 nm) and red (660 nm) light in the treatment of acne vulgaris" (PDF). Br J Dermatol. 142 (5): 973–8. PMID 10809858.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ "Azelaic Acid (Topical)" MedlinePlus, Revised: 07/24/2001 web entry
- ^ Dreno B, Amblard P, Agache P, Sirot S, Litoux P (1989). "Low doses of zinc gluconate for inflammatory acne". Acta Derm Venereol. 69 (6): 541–3. PMID 2575335.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Dreno B, Moyse D, Alirezai M, Amblard P, Auffret N, Beylot C, Bodokh I, Chivot M, Daniel F, Humbert P, Meynadier J, Poli F (2001). "Multicenter randomized comparative double-blind controlled clinical trial of the safety and efficacy of zinc gluconate versus minocycline hydrochloride in the treatment of inflammatory acne vulgaris". Dermatology. 203 (2): 135–40. PMID 11586012.
{{cite journal}}: CS1 maint: multiple names: authors list (link)
See also
External links
- Acne vulgaris: more than skin deep (on the psychological effects of acne)
