User:HAL333/sandbox/viralvector: Difference between revisions
| Line 157: | Line 157: | ||
In 1977, the [[National Institutes of Health]] (NIH) issued formal guidelines confining viral DNA cloning to rigid [[BSL-4]] conditions, practically preventing such research. However, the NIH loosened these rules in 1979, permitting [[Bernard Moss]] to develop a viral vector utilizing [[vaccinia]].{{sfn|Moss|2014|pp=4220}} In 1982, Moss reported the first use of a viral vector for transient gene expression.{{sfn|Shimada|2014|pp=625}} The following year, Moss used the vaccinia vector to express a [[hepatitis B]] antigen, creating the first viral vector vaccine.{{sfn|McCann|2022|pp=1}} |
In 1977, the [[National Institutes of Health]] (NIH) issued formal guidelines confining viral DNA cloning to rigid [[BSL-4]] conditions, practically preventing such research. However, the NIH loosened these rules in 1979, permitting [[Bernard Moss]] to develop a viral vector utilizing [[vaccinia]].{{sfn|Moss|2014|pp=4220}} In 1982, Moss reported the first use of a viral vector for transient gene expression.{{sfn|Shimada|2014|pp=625}} The following year, Moss used the vaccinia vector to express a [[hepatitis B]] antigen, creating the first viral vector vaccine.{{sfn|McCann|2022|pp=1}} |
||
[[File:How viral vector COVID-19 Vaccines Work (English).pdf|thumb|upright|A 2021 [[U.S. Centers for Disease Control and Prevention]] poster explaining the COVID-19 viral vector vaccines]] |
|||
In the early 1990s, the first successful gene therapy was used to treat [[severe combined immunodeficiency]] in patient [[Ashanthi DeSilva]]: it employed a recombinant retrovirus.{{sfn|Bulcha|2022|pp=1}} |
In the early 1990s, the first successful gene therapy was used to treat [[severe combined immunodeficiency]] in patient [[Ashanthi DeSilva]]: it employed a recombinant retrovirus.{{sfn|Bulcha|2022|pp=1}} |
||
Revision as of 20:03, 29 April 2024

Viral vectors are tools used to deliver genetic material into cells. This process can be performed inside a living organism or in cell culture. They have widespread applications for use in basic research, therapies, and vaccines.
Viruses have evolved specialized molecular mechanisms to efficiently transport their genomes inside the cells they infect. Delivery of genes or other genetic material by a vector is termed transduction and the infected cells are described as transduced.
Molecular biologists first harnessed this machinery in the 1970s. Paul Berg used a modified SV40 virus containing DNA from the bacteriophage λ to infect monkey kidney cell maintained in culture.
In addition to their use in molecular biology research, viral vectors are used for gene therapy and the development of vaccines. Vectors can either integrate into a cell's genome or transiently express a gene with non-integrative vectors.[1]: 50
Characteristics

"Viruses are infectious agents composed of nucleic acids protected by a protein coat. These microbes cannot self-replicate, relying instead on the cells they infect to produce more copies of themselves by hijacking the host’s replication machinery [1]. Viruses are generally associated with disease, but genetic engineers have repurposed their biology to leverage their natural ability to modify or supplement the host cell genetic code, producing a new class of gene delivery tools known as viral vectors" [2]
A viral vector consists of three components:[3]
- A protein capsid and/or envelope that encapsidates the genetic payload. This determines the target tissue or antigen recognition.
- The genetic payload: the transgene that results in the desired effect when expressed.
- The "regulatory cassette" that allows for the expression of the trangene either as a chromosomal integrant or an episome. It comprises enhancer, promoter, and auxiliary elements.
The three viruses most commonly used as viral vectors are adenoviruses (Ads) or adeno-associated viruses (AAVs), and lentiviruses (a type of retrovirus).[4]
Viral Vectors are tailored to their specific applications but generally share a few key properties.[citation needed]
- Safety: Although viral vectors are occasionally created from pathogenic viruses, they are modified in such a way as to minimize the risk of handling them. This usually involves the deletion of a part of the viral genome critical for viral replication. Such a virus can efficiently infect cells but, once the infection has taken place, requires a helper virus to provide the missing proteins for production of new virions.
- Low toxicity: The viral vector should have a minimal effect on the physiology of the cell it infects.
- Stability: Some viruses are genetically unstable and can rapidly rearrange their genomes. This is detrimental to predictability and reproducibility of the work conducted using a viral vector and is avoided in their design.
- Cell type specificity: Most viral vectors are engineered to infect as wide a range of cell types as possible. However, sometimes the opposite is preferred. The viral vector can be modified to target the virus to a specific kind of cell. Viruses modified in this manner are said to be pseudotyped.
- Identification: Viral vectors are often given certain genes that help identify which cells took up the viral genes. These genes are called markers. A common marker is resistance to a certain antibiotic. The cells can then be isolated easily, as those that have not taken up the viral vector genes do not have antibiotic resistance, and so cannot grow in a culture with the relevant antibiotic present.
Applications
Basic research
Viral vectors were originally developed as an alternative to transfection of naked DNA for molecular genetics experiments. Compared to traditional methods of transfection (like calcium phosphate precipitation), transduction can ensure that nearly 100% of cells are infected without severely affecting cell viability.[citation needed] Furthermore, some viruses integrate into the cell genome facilitating stable expression.[citation needed]
Protein coding genes can be expressed using viral vectors, commonly to study the function of the particular protein. Viral vectors, especially retroviruses, stably expressing marker genes such as GFP are widely used to permanently label cells to track them and their progeny, for example in xenotransplantation experiments, when cells infected in vitro are implanted into a host animal.[citation needed]
Gene insertion, which can be done with viral vectors, is cheaper to carry out than gene knockout. But as gene silencing, an effect that may be intended with gene insertion, is sometimes non-specific and has off-target effects on other genes, it hence provides less reliable results. Animal host vectors also play an important role[clarification needed].
Gene therapy

Gene therapy is a technique for correcting defective genes responsible for disease development. In the future, gene therapy may provide a way to cure genetic disorders, such as severe combined immunodeficiency, cystic fibrosis or even haemophilia A. Because these diseases result from mutations in the DNA sequence for specific genes, gene therapy trials have used viruses to deliver unmutated copies of these genes to the cells of the patient's body. There have been a huge number of laboratory successes with gene therapy. However, several problems of viral gene therapy must be overcome before it gains widespread use. Immune response to viruses not only impedes the delivery of genes to target cells but can cause severe complications for the patient. In one of the early gene therapy trials in 1999 this led to the death of Jesse Gelsinger, who was treated using an adenoviral vector.[5]
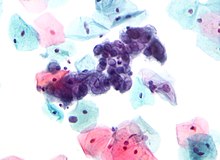
Some viral vectors, for instance gamma-retroviruses, insert their genomes at a seemingly random location on one of the host chromosomes, which can disturb the function of cellular genes and lead to cancer. In a severe combined immunodeficiency retroviral gene therapy trial conducted in 2002, four of the patients developed leukemia as a consequence of the treatment;[6] three of the patients recovered after chemotherapy.[7] Adeno-associated virus-based vectors are much safer in this respect as they always integrate at the same site in the human genome, with applications in various disorders, such as Alzheimer's disease.[8]
Vaccines

A live vector vaccine is a vaccine that uses an organism (typically virus or bacterium) that does not cause disease to transport the pathogen genes into the body in order to stimulate an immune response.[9] Viruses expressing pathogen proteins are currently being developed as vaccines against these pathogens, based on the same rationale as DNA vaccines. The genes used in such vaccines are usually antigen coding surface proteins from the pathogenic organism. They are then inserted into the genome of a non-pathogenic organism, where they are expressed on the organism's surface and can elicit an immune response.[clarification needed]
Unlike attenuated vaccines, viral vector vaccines lack other pathogen genes required for replication, so infection by the pathogen is impossible. Adenoviruses are being actively developed as vaccine vectors.
In comparison to other vaccine types, viral vectors offer efficient gene transduction and can target specific cell types. Further, they are able to induce more robust immune responses and enhanced cellular immunity.[10]
Medicine delivery
A strain of canarypox virus modified to carry feline interleukin-2 is used to treat cats with fibrosarcoma.[11]
Oncolytic viruses
"Oncolytic viruses selectively repli-cate in tumor cells, resulting in direct lysis of tumor cells2. During this death process, damage-associated molecular pat-terns (DAMPs) and tumor-associated antigens are released into the tumor micro-environment, which promotes the recruit-ment and activation of dendritic cells (DCs). As the activated DCs uptake, process and present the released tumor-associated antigens, tumor-specific effectors T lymphocytes are conse-quently stimulated to kill the tumor cells, including those unin-fected. Thus, the oncolytic virus-induced tumor death is also coined as immunogenic cell death (ICD) because it triggers an inflammatory response capable of changing the tumor micro- environment from “cold” to “warm”. "
-Zhang 2021
Types
Retroviruses
Retroviruses—enveloped RNA viruses—are popular viral vector platforms due to their ability to integrate genetic material into the host genome.[2] Retroviral vectors comprise two general classes: gamma retroviral and lentiviral vectors. The fundamental difference between the two are that gamma retroviral vectors can only infect dividing cells, while lentiviral vectors can infect both dividing and resting cells.[12]
Gamma retroviral vectors
Retroviruses are one of the mainstays of current gene therapy approaches. The recombinant retroviruses such as the Moloney murine leukemia virus have the ability to integrate into the host genome in a stable fashion. They contain a reverse transcriptase to make a DNA copy of the RNA genome, and an integrase that allows integration into the host genome. They have been used in a number of FDA-approved clinical trials such as the SCID-X1 trial.[13]
Retroviral vectors can either be replication-competent or replication-defective. Replication-defective vectors are the most common choice in studies because the viruses have had the coding regions for the genes necessary for additional rounds of virion replication and packaging replaced with other genes, or deleted. These virus are capable of infecting their target cells and delivering their viral payload, but then fail to continue the typical lytic pathway that leads to cell lysis and death.
Conversely, replication-competent viral vectors contain all necessary genes for virion synthesis, and continue to propagate themselves once infection occurs. Because the viral genome for these vectors is much lengthier, the length of the actual inserted gene of interest is limited compared to the possible length of the insert for replication-defective vectors. Depending on the viral vector, the typical maximum length of an allowable DNA insert in a replication-defective viral vector is usually about 8–10 kB.[verification needed][14] While this limits the introduction of many genomic sequences, most cDNA sequences can still be accommodated.
The primary drawback to use of retroviruses such as the Moloney retrovirus involves the requirement for cells to be actively dividing for transduction. As a result, cells such as neurons are very resistant to infection and transduction by retroviruses.
There is concern that insertional mutagenesis due to integration into the host genome might lead to cancer or leukemia. This concern remained theoretical until gene therapy for ten SCID-X1 patients using Moloney murine leukemia virus[15] resulted in two cases of leukemia caused by activation of the LMO2 oncogene due to nearby integration of the vector.[16]
Lentiviral vectors

The most commonly used lentiviral vector is human immunodeficiency virus type 1 (HIV-1), although simian immunodeficiency virus (SIV), the feline immunodeficiency virus (FIV), and the equine infectious anaemia virus (EIAV) have also been utilized.[12]
Lentiviral vectors have been used as In vivo therapies, such as directly treating genetic diseases like haemophilia B, and for ex vivo therapies like the the transduction of immune cells in CAR T cell therapy.[12]
Lentiviral vectors are able to carry up to 10 kb of foreign DNA.[12]
Lentiviruses are a subclass of retroviruses. They are sometimes used as vectors for gene therapy thanks to their ability to integrate into the genome of non-dividing cells, which is a unique feature of lentiviruses, as other retroviruses can infect only dividing cells. The viral genome in the form of RNA is reverse-transcribed when the virus enters the cell to produce DNA, which is then inserted into the genome at a random position (although recent findings suggest that the insertion of viral DNA is not random but directed to specific active genes and related to genome organisation[17]) by the viral integrase enzyme. The vector, now called a provirus, remains in the genome and is passed on to the progeny of the cell when it divides. There are, as yet, no techniques for determining the site of integration, which can pose a problem. The provirus can disturb the function of cellular genes and lead to activation of oncogenes promoting the development of cancer, which raises concerns for possible applications of lentiviruses in gene therapy. However, studies have shown that lentivirus vectors have a lower tendency to integrate in places that potentially cause cancer than gamma-retroviral vectors.[18] More specifically, one study found that lentiviral vectors did not cause either an increase in tumor incidence or an earlier onset of tumors in a mouse strain prone to tumors.[19] Moreover, clinical trials that utilized lentiviral vectors to deliver gene therapy for the treatment of HIV experienced no increase in mutagenic or oncologic events.[20] Versions of the lentiviral vector have been developed that do not integrate their genetic material into the cell's genome but only transiently express genes.[21]: 50
For safety reasons, lentiviral vectors never carry the genes required for their replication. To produce a lentivirus, several plasmids are transfected into a so-called packaging cell line, commonly HEK 293. One or more plasmids, generally referred to as packaging plasmids, encode the virion proteins, such as the capsid and the reverse transcriptase. Another plasmid contains the genetic material to be delivered by the vector. It is transcribed to produce the single-stranded RNA viral genome and is marked by the presence of the ψ (psi) sequence. This sequence is used to package the genome into the virion.
Adenoviruses
As opposed to lentiviruses, adenoviral DNA does not integrate into the genome and is not replicated during cell division.[22]: 5 This limits their use in basic research, although adenoviral vectors are still used in in vitro and also in vivo experiments.[23] Their primary applications are in gene therapy and vaccination. Since humans commonly come in contact with adenoviruses, which cause respiratory, gastrointestinal and eye infections, majority of patients have already developed neutralizing antibodies which can inactivate the virus before it can reach the target cell. To overcome this problem scientists are currently investigating adenoviruses that infect different species to which humans do not have immunity, for example, the chimpanzee adenovirus used as a vector to transport SARS-CoV-2 spike gene in Oxford AstraZeneca COVID vaccine. PEGylation of adenoviruses for gene therapy can help prevent adverse reactions due to pre-existing adenovirus immunity.[24]
Among 50 human adenovirus serotypes, serotype 5 is the most widely investigated.[25]
Adenovirus vectors possess a number of benefits: "high transduction efficiency, high level of transgene expression, and broad range of viral tropism". They can also infect dividing and non-dividing cells.[26]
One disadvantage is that pre-existing immunity to adenovirus serotypes is common, reducing efficacy.[26]
Adeno-associated viruses

Adeno-associated virus (AAV) is a small virus that infects humans and some other primate species. AAV is not currently known to cause disease, and causes a very mild immune response. AAV can infect both dividing and non-dividing cells and may incorporate its genome into that of the host cell. Moreover, AAV mostly stays as episomal (replicating without incorporation into the chromosome); performing long and stable expression.[27] These features make AAV a very attractive candidate for creating viral vectors for gene therapy.[28] However, AAV can only bring up to 5kb which is considerably small compared to AAV's original capacity.[27]
Adeno-associated viral vectors have been engineered to evade virus recognition by TLR9 receptors by incorporating TLR9-inhibiting genes into the vector.[29]
Furthermore, because of its potential use as a gene therapy vector, researchers have created an altered AAV called self-complementary adeno-associated virus (scAAV). Whereas AAV packages a single strand of DNA and requires the process of second-strand synthesis, scAAV packages both strands which anneal together to form double stranded DNA. By skipping second strand synthesis scAAV allows for rapid expression in the cell.[30] Otherwise, scAAV carries many characteristics of its AAV counterpart.
Plant viruses
Plant viruses can be used to engineer viral vectors, tools commonly used to deliver genetic material into plant cells; they are also sources of biomaterials and nanotechnology devices.[31][32] Tobacco mosaic virus (TMV) is the first virus to be discovered. Viral vectors based on TMV include those of the magnICON[33] and TRBO plant expression technologies.[31]
Vaccinia

Vaccinia virus, a poxvirus, is another promising candidate for viral vector development.[34] Its use as the smallpox vaccine—first reported by Edward Jenner in 1798—led to the eradication of smallpox and demonstrated vaccinia as safe and effective in humans.[35][34][note 1] Moreover, manufacturing procedures developed to mass-produce smallpox vaccine stockpiles may expedite vaccinia viral vector production.[25]
Vaccinia possesses a large DNA genome and can consequently carry up to 40 kb of foreign DNA.[35][37][38][37] Further, vaccinia are unlikely to integrate into the host genome, decreasing the chance of carcinogenesis.[37] Attenuated strains—replicating and non-replicating—have been developed.[35] Although widely characterized due to its use against smallpox, as of 2019 the function of 50 percent of the vaccinia genome was unknown. This may lead to unpredictable effects.[38]
As a vaccine, vaccinia vectors display highly effective transgene expression and create a robust immune response.[25] Vaccinia is also fast-acting: its life cycle produces mature progeny virus within 6 hours, and has three viral spread mechanisms.[38] Vaccinia also has an adjuvant effect, activating a strong innate response via toll-like receptors.[25] A significant disadvantage that can reduce its efficacy as a viral vector, however, is pre-existing immunity against vaccinia for those who received the smallpox vaccine.[25]
Herpesviruses
Of the nine herpesviruses that infect humans, herpes simplex virus 1 (HSV-1) is the most well characterized and most commonly used as a viral vector.[39] HSV-1 offers several advtanges: it can target multiple cell-types and deliver therapeutics via specialized expression systems.[40] Moreover, HSV-1 can cross the blood brain barrier if medically-disrupted, enabling it to target neurological diseases. Also, HSV-1 does not integrate into the host genome and can carry large amounts of foreign DNA. The former feature prevents harmful mutagenesis, as can occur with retroviral and adeno-associated vectors. Replication-deficient strains have been developed.[41]
In 2015, talimogene laherparepvec—an HSV-1 vector that triggers an anti-tumor immune response—was approved by the US Food and Drug Administration to treat melanoma.[42] As of 2020, HSV-1 vectors have been experimentally applied against sarcomas and cancers of the brain, colon, prostate, and skin.[43]
Cytomegalovirus (CMV), a herpesvirus, has also been employed as a viral vector.[44] CMV can infect most cell types and can thus proliferate throughout the body. Although a CMV-based vaccine provided significant immunity against SIV—closely related to HIV—in macaques, development of CMV as a reliable vector was reported to still be in early stages as of 2020.[45][46]
Hybrids
Hybrid vectors are vector viruses that are genetically engineered to have qualities of more than one vector. Viruses are altered to avoid the shortcomings of typical viral vectors, which may have limited loading capacity, immunogenicity, genotoxicity, and fail to support long-term adequate transgenic expression. Through the replacement of undesirable elements with desired abilities, hybrid vectors may in the future outperform standard transfection vectors in terms of safety and therapeutic efficiency.[47]
History
In 1972, Stanford University biochemist Paul Berg developed the first viral vector, incorporating DNA from E. coli into the polyomavirus SV40.[48][49][50] The implications of this research troubled scientists like Robert Pollack, who convinced Berg not to insert DNA from SV40 into E. coli via a bacteriophage vector. They feared that introducing the purportedly cancer-causing genes of SV40 may have created carcinogenic bacterial strains.[51] These concerns and others in the emerging field of recombinant DNA led to the Asilomar Conference of 1975, where attendees agreed to a voluntary moratorium on cloning DNA.[52]
In 1977, the National Institutes of Health (NIH) issued formal guidelines confining viral DNA cloning to rigid BSL-4 conditions, practically preventing such research. However, the NIH loosened these rules in 1979, permitting Bernard Moss to develop a viral vector utilizing vaccinia.[52] In 1982, Moss reported the first use of a viral vector for transient gene expression.[53] The following year, Moss used the vaccinia vector to express a hepatitis B antigen, creating the first viral vector vaccine.[54]
In the early 1990s, the first successful gene therapy was used to treat severe combined immunodeficiency in patient Ashanthi DeSilva: it employed a recombinant retrovirus.[55]
Gelsinger joined a clinical trial run by the University of Pennsylvania that aimed at developing a treatment for infants born with the severe form of the disease. On September 13, 1999, Gelsinger was injected with an adenoviral vector carrying a corrected gene to test the safety of the procedure. He died four days later at the age of 18, on September 17, apparently having suffered a massive immune response triggered by the use of the viral vector to transport the gene into his cells, leading to multiple organ failure and brain death.[56]
COVID-19
Future
Challenges
The choice of a viral vector to deliver genetic material to cells comes with some logistical problems. There are a limited number of viral vectors available for therapeutic use. Any of these few viral vectors can cause the body to develop an immune response if the vector is seen as a foreign invader.[57][58] Once used, the viral vector cannot be effectively used in the patient again because it will be recognized by the body. If the vaccine or gene therapy fails in clinical trials, the virus can't be used again in the patient for a different vaccine or gene therapy in the future.
Pre-existing immunity against the viral vector could also be present in the patient, rendering the therapy ineffective for that patient.[57][59] Because priming with a naked DNA vaccine and boosting with a viral vector results in a robust immune response via yet indefinite mechanism(s), despite pre-existing viral vector immunity, this vaccination strategy can counteract this problem.[60] However, this method may present another expense and obstacle in the vaccine distribution process. Pre-existing immunity may also be challenged by increasing vaccine dose or changing the vaccination route.[61]
Some shortcomings of viral vectors (such as genotoxicity and low transgenic expression) can be overcome through the use of hybrid vectors.
Potential
In popular culture

In film, viral vectors are often portrayed as unintentionally causing a pandemic and civilizational catastrophe.[62] The 2007 film I Am Legend depicts a cancer-targeting viral vector as unleashing a zombie apocalypse.[63][64] Similarly, a viral vector therapy for Alzheimer's in Rise of the Planet of the Apes (2011) becomes a deadly pathogen and causes an ape uprising.[65]
Notes and references
Notes
- ^ ADD MORE! COW/HORSEPOX Edward Jenner's use of material from cow blisters containing vaccinia was the basis for vaccinology and ultimately led to the eradication of smallpox from Earth.[36]
Citations
- ^ Nóbrega C (2020). A handbook of gene and cell therapy. Liliana Mendonça, Carlos A. Matos. Cham: Springer. ISBN 978-3-030-41333-0. OCLC 1163431307.
- ^ a b Labbé 2021, pp. 1.
- ^ Bulcha 2022, pp. 1–2.
- ^ Bulcha 2022, pp. 2.
- ^ Beardsley T (February 2000). "A tragic death clouds the future of an innovative treatment method". Scientific American.
- ^ McDowell N (15 January 2003). "New cancer case halts US gene therapy trials". New Scientist.
- ^ Hacein-Bey-Abina S, Hauer J, Lim A, Picard C, Wang GP, Berry CC, et al. (July 2010). "Efficacy of gene therapy for X-linked severe combined immunodeficiency". The New England Journal of Medicine. 363 (4): 355–64. doi:10.1056/NEJMoa1000164. PMC 2957288. PMID 20660403.
- ^ Sasmita AO (April 2019). "Current viral-mediated gene transfer research for treatment of Alzheimer's disease". Biotechnology & Genetic Engineering Reviews. 35 (1): 26–45. doi:10.1080/02648725.2018.1523521. PMID 30317930. S2CID 52978228.
- ^ "Live-Vector Vaccine". American Institute of Chemical Engineers. 17 December 2014. Archived from the original on 2021-02-03. Retrieved 2021-02-03.
- ^ Shimada 2014, pp. 624.
- ^ "EPAR summary for the public: Oncept IL-2 (Feline interleukin-2 recombinant canary pox virus) [EMA/151380/2013 EMEA/V/C/002562]" (PDF). European Medical Agency. 2013.
- ^ a b c d Labbé 2021, pp. 2.
- ^ Cavazzana-Calvo M, Hacein-Bey S, de Saint Basile G, Gross F, Yvon E, Nusbaum P, et al. (April 2000). "Gene therapy of human severe combined immunodeficiency (SCID)-X1 disease". Science. 288 (5466): 669–72. Bibcode:2000Sci...288..669C. doi:10.1126/science.288.5466.669. PMID 10784449.
- ^ Coffin JM, Hughes SH, Varmus HE (1997). "Principles of Retroviral Vector Design". In Varmus, Harold, Coffin, John M., Hughes, Stephen H. (eds.). Retroviruses. Plainview, N.Y: Cold Spring Harbor Laboratory Press. ISBN 978-0-87969-571-2. PMID 21433340.
- ^ Hacein-Bey-Abina S, Le Deist F, Carlier F, Bouneaud C, Hue C, De Villartay JP, et al. (April 2002). "Sustained correction of X-linked severe combined immunodeficiency by ex vivo gene therapy". The New England Journal of Medicine. 346 (16): 1185–93. doi:10.1056/NEJMoa012616. PMID 11961146.
- ^ Hacein-Bey-Abina S, Von Kalle C, Schmidt M, McCormack MP, Wulffraat N, Leboulch P, et al. (October 2003). "LMO2-associated clonal T cell proliferation in two patients after gene therapy for SCID-X1". Science. 302 (5644): 415–9. Bibcode:2003Sci...302..415H. doi:10.1126/science.1088547. PMID 14564000. S2CID 9100335.
- ^ Marini B, Kertesz-Farkas A, Ali H, Lucic B, Lisek K, Manganaro L, et al. (May 2015). "Nuclear architecture dictates HIV-1 integration site selection" (PDF). Nature. 521 (7551): 227–31. Bibcode:2015Natur.521..227M. doi:10.1038/nature14226. hdl:11368/2844160. PMID 25731161. S2CID 974969.
- ^ Cattoglio C, Facchini G, Sartori D, Antonelli A, Miccio A, Cassani B, et al. (September 2007). "Hot spots of retroviral integration in human CD34+ hematopoietic cells". Blood. 110 (6): 1770–8. doi:10.1182/blood-2007-01-068759. PMID 17507662. S2CID 8715798.
- ^ Montini E, Cesana D, Schmidt M, Sanvito F, Ponzoni M, Bartholomae C, et al. (June 2006). "Hematopoietic stem cell gene transfer in a tumor-prone mouse model uncovers low genotoxicity of lentiviral vector integration". Nature Biotechnology. 24 (6): 687–96. doi:10.1038/nbt1216. PMID 16732270. S2CID 8966580.
- ^ Lidonnici MR, Paleari Y, Tiboni F, Mandelli G, Rossi C, Vezzoli M, et al. (December 2018). "Multiple Integrated Non-clinical Studies Predict the Safety of Lentivirus-Mediated Gene Therapy for β-Thalassemia". Molecular Therapy: Methods & Clinical Development. 11: 9–28. doi:10.1016/j.omtm.2018.09.001. PMC 6178212. PMID 30320151.
- ^ Nóbrega C (2020). A handbook of gene and cell therapy. Liliana Mendonça, Carlos A. Matos. Cham: Springer. ISBN 978-3-030-41333-0. OCLC 1163431307.
- ^ Bulcha JT, Wang Y, Ma H, Tai PW, Gao G (February 2021). "Viral vector platforms within the gene therapy landscape". Signal Transduction and Targeted Therapy. 6 (1): 53. doi:10.1038/s41392-021-00487-6. PMC 7868676. PMID 33558455.
- ^ Ramos-Kuri M, Rapti K, Mehel H, Zhang S, Dhandapany PS, Liang L, et al. (November 2015). "Dominant negative Ras attenuates pathological ventricular remodeling in pressure overload cardiac hypertrophy". Biochimica et Biophysica Acta (BBA) - Molecular Cell Research. 1853 (11 Pt A): 2870–84. doi:10.1016/j.bbamcr.2015.08.006. PMC 4715892. PMID 26260012.
- ^ Seregin SS, Amalfitano A (2009). "Overcoming pre-existing adenovirus immunity by genetic engineering of adenovirus-based vectors". Expert Opinion on Biological Therapy. 9 (12): 1521–1531. doi:10.1517/14712590903307388. PMID 19780714. S2CID 21927486.
- ^ a b c d e Ura 2014, pp. 627.
- ^ a b Ura 2014, pp. 628.
- ^ a b Nussbaum RL, McInnes RR, Willard HF (2015). Thompson & Thompson Genetics in Medicine. Canada: ELSEVIER. p. 278. ISBN 978-1-4377-0696-3.
- ^ Cite error: The named reference
:1was invoked but never defined (see the help page). - ^ Chan YK, Wang SK, Church GM (2021). "Engineering adeno-associated viral vectors to evade innate immune and inflammatory responses". Science Translational Medicine. 13 (588): eabd3438. doi:10.1126/scitranslmed.abd3438. PMC 8409505. PMID 33568518.
- ^ McCarty DM, Monahan PE, Samulski RJ (August 2001). "Self-complementary recombinant adeno-associated virus (scAAV) vectors promote efficient transduction independently of DNA synthesis". Gene Therapy. 8 (16): 1248–54. doi:10.1038/sj.gt.3301514. PMID 11509958.
- ^ a b Abrahamian P, Hammond RW, Hammond J (2020-06-10). "Plant Virus-Derived Vectors: Applications in Agricultural and Medical Biotechnology". Annual Review of Virology. 7 (1): 513–535. doi:10.1146/annurev-virology-010720-054958. ISSN 2327-0578. PMID 32520661. S2CID 219588089.
- ^ Pasin F, Menzel W, Daròs JA (June 2019). "Harnessed viruses in the age of metagenomics and synthetic biology: an update on infectious clone assembly and biotechnologies of plant viruses". Plant Biotechnology Journal. 17 (6): 1010–1026. doi:10.1111/pbi.13084. ISSN 1467-7652. PMC 6523588. PMID 30677208.
- ^ magnICON
- ^ a b Zhang 2021, pp. 1578.
- ^ a b c Ura 2014, pp. 626.
- ^ Kaynarcalidan 2021, pp. 1–3, 5.
- ^ a b c Kaynarcalidan 2021, pp. 1.
- ^ a b c Guo 2019, pp. 4.
- ^ Mody 2020, pp. 1.
- ^ Mody 2020, pp. 3–4.
- ^ Mody 2020, pp. 4.
- ^ Khushalani 2023, pp. 1.
- ^ Hromic-Jahjefendic 2020, p. 631.
- ^ Ura 2014, pp. 631.
- ^ Sasso 2020, pp. 10.
- ^ Schaefer, et al. (2005). "Divergent HIV and Simian Immunodeficiency Virus Surveillance, Zaire". Emerging Infectious Diseases. 11 (9).
- ^ Huang S, Kamihira M (2013). "Development of hybrid viral vectors for gene therapy". Biotechnology Advances. 31 (2): 208–23. doi:10.1016/j.biotechadv.2012.10.001. PMID 23070017.
- ^ "The use of viral vectors in vaccine development". npj Vaccines. 8: 62–73. 4 July 2022.
{{cite journal}}: Cite uses deprecated parameter|authors=(help) - ^ Lukiw WJ (18 May 2023). "Commentary: A tribute to Dr. Paul Berg (1926–2023) American biochemist, Nobel Laureate and discoverer of recombinant DNA technology, vaccine and genetic engineering". Frontiers in Cell and Developmental Biology. 11.
- ^ "BiochemicalMethodforInsertingNew GeneticInformationintoDNA of SimianVirus40:CircularSV40DNA MoleculesContainingLambda Phage Genes and the Galactose Operon of Escherichia coli". Proceedings of the National Academy of Sciences of the United States of America. 69 (10): 2904–2909. October 1972.
{{cite journal}}: Cite uses deprecated parameter|authors=(help) - ^ Carmen 1986, pp. 61–62.
- ^ a b Moss 2014, pp. 4220.
- ^ Shimada 2014, pp. 625.
- ^ McCann 2022, pp. 1.
- ^ Bulcha 2022, pp. 1.
- ^ Stolberg SG (November 28, 1999). "The Biotech Death of Jesse Gelsinger". The New York Times Magazine. Retrieved July 5, 2018.
- ^ a b Nayak S, Herzog RW (March 2010). "Progress and prospects: immune responses to viral vectors". Gene Therapy. 17 (3): 295–304. doi:10.1038/gt.2009.148. PMC 3044498. PMID 19907498.
- ^ Zhou HS, Liu DP, Liang CC (November 2004). "Challenges and strategies: the immune responses in gene therapy". Medicinal Research Reviews. 24 (6): 748–61. doi:10.1002/med.20009. PMID 15250039. S2CID 17622444.
- ^ Crommelin DJ, Sindelar RD, Meibohm B (2008). Pharmaceutical Biotechnology: Fundamentals and application. London: Taylor & Francis. ISBN 978-1420044379.
- ^ Yang ZY, Wyatt LS, Kong WP, Moodie Z, Moss B, Nabel GJ (January 2003). "Overcoming immunity to a viral vaccine by DNA priming before vector boosting". Journal of Virology. 77 (1): 799–803. doi:10.1128/JVI.77.1.799-803.2003. PMC 140625. PMID 12477888.
- ^ Pandey A, Singh N, Vemula SV, Couëtil L, Katz JM, Donis R, et al. (2012). Subbiah E (ed.). "Impact of preexisting adenovirus vector immunity on immunogenicity and protection conferred with an adenovirus-based H5N1 influenza vaccine". PLOS ONE. 7 (3): e33428. Bibcode:2012PLoSO...733428P. doi:10.1371/journal.pone.0033428. PMC 3303828. PMID 22432020.
- ^ Sánchez-Angulo M (6 December 2023). "Microbial pathogens in the movies". FEMS Microbiology Letters. 370.
- ^ "Fact check: A vaccine did not turn characters in the movie 'I Am Legend' into zombies". Reuters. Reuters. December 18, 2020. Retrieved 27 April 2024.
- ^ Feldman ZB, Clayton J (20 December 2022). "Genetics and Ethics in the "I am Legend" Corpus". Journal of Literary Science. 14 (1–2): 94–107.
- ^ Sánchez-Angulo M (6 December 2023). "Microbial pathogens in the movies". FEMS Microbiology Letters. 370.
Works cited
XXX = mine further
Journal articles
- Bulcha JT, Wang Y, Ma H, Tai PW, Gao G (8 February 2021). "Viral vector platforms within the gene therapy landscape" (PDF). Signal Transduction and Targeted Therapy. 6 (1). doi:10.1038/s41392-021-00487-6. PMC 7868676. PMID 33558455.
{{cite journal}}: CS1 maint: PMC format (link)XXX - Ura T, Okuda K, Shimada M (29 July 2014). "Developments in Viral Vector-Based Vaccines". Vaccines. 2: 624–641. doi:10.3390/vaccines2030624.
{{cite journal}}: CS1 maint: unflagged free DOI (link)XXX - Moss B (6 September 2013). "Reflections on the Early Development of Poxvirus Vectors" (PDF). Vaccine. 31 (39): 4220–4222. doi:10.1016/j.vaccine.2013.03.042.
{{cite journal}}: Check|doi=value (help) - McCann N, O'Connor D, Lambe T, Pollard AJ (August 2022). "Viral vector vaccines". Current Opinion in Immunology. 77.
- Smith GL, Mackett M, Moss B (7 April 1983). "Infectious vaccinia virus recombinants that express hepatitis B virus surface antigen". Nature. 302 (5908): 490–495. doi:10.1038/302490a0.
- Li X, Le Y, Zhang Z, Nian X, Liu B, Yang X (May 2023). "Viral Vector-Based Gene Therapy" (PDF). International Journal of Molecular Science. 24 (9).XXX
- Mody PH, Pathak S, Hanson LK, Spencer JV (2020). "Herpes Simplex Virus: A Versatile Tool for Insights Into Evolution, Gene Delivery, and Tumor Immunotherapy" (PDF). Virology. 11. XXX
- Khushalani NI, Harrington KJ, Melcher A, Bommareddy PK, Zamarin D (December 2023). "Breaking the barriers in cancer care: The next generation of herpes simplex virus-based oncolytic immunotherapies for cancer treatment" (PDF). Molecular Therapy: Oncolytics. 11. PMID 37841530.XXX
- Kaynarcalidan O, Mascaraque SM, Drexler I (2021). "Vaccinia Virus: From Crude Smallpox Vaccines to Elaborate Viral Vector Vaccine Design". Biomedicines. 9 (11).XXX
- Guo ZS, et al. (2019). "Vaccinia virus-mediated cancer immunotherapy: cancer vaccines and oncolytics" (PDF). Journal of Immunotherapy of Cancer. 9 (7).
- Zhang Z, Donga L, Zhaoa C, Zhengb P, Zhanga X, Xu J (2021). "Vaccinia virus-based vector against infectious diseases and tumors" (PDF). Human Vaccines and Immunotherapeutics. 17 (6). doi:10.1080/21645515.2020.1840887.XXX
- Hromic-Jahjefendic A, Lundstrom K (2020). "Viral Vector-Based Melanoma Gene Therapy" (PDF). Biomedicines. 8 (60).
- Glorioso JC, et al. (2020). "Oncolytic HSV Vectors and Anti-Tumor Immunity". Current Issues in Molecular Biology. 41: 381–468. PMID 32938804.
- Sasso E, D’Alise AM, Zambrano N, Scarselli E, Folgori A, Nicosia A (2020). "New viral vectors for infectious diseases and cancer". Seminars in Immunology. 50.
{{cite journal}}: Vancouver style error: non-Latin character in name 2 (help) X - Labbé RP, Vessillier S, Rafiq QA (2021). "Lentiviral Vectors for T Cell Engineering: Clinical Applications, Bioprocessing and Future Perspectives" (PDF). Viruses. 13 (152).
Books
- Carmen I (1985). Cloning and the Constitution: An Inquiry into Governmental Policymaking and Genetic Experimentation. University of Wisconsin Press. ISBN 9780299103408.
Further reading
- Torashima T, Koyama C, Higashida H, Hirai H (2007). "Production of neuron-preferential lentiviral vectors". Protocol Exchange. doi:10.1038/nprot.2007.89.
- Okada Y, Ikawa M (2007). "Placenta specific gene manipulation by transducing zona-free blastocyst using lentiviral vector". Protocol Exchange. doi:10.1038/nprot.2007.62.
- Fry JW, Wood KJ (8 June 1999). "A comparison of vectors in use for clinical gene transfer". Expert Reviews in Molecular Medicine.