Diabetic nephropathy: Difference between revisions
Ozzie10aaaa (talk | contribs) |
Ozzie10aaaa (talk | contribs) |
||
| Line 68: | Line 68: | ||
* Clinical (overt) albuminuria: urinary albumin excretion ≥300 mg/24h. |
* Clinical (overt) albuminuria: urinary albumin excretion ≥300 mg/24h. |
||
Diabetic patients are suggested to control albumin excretion every year. |
Diabetic patients are suggested to control albumin excretion every year. |
||
Urinary albumin collection can also be timed (normal value <20 mg/min) or a random spot collection (normal value <30 μg/mg). Abnormal values correlate with nephropathy.Another diagnostic tool is glomerular filtration rate esteem ([[Estimated Glomerular Filtration Rate|eGFR]]) based on creatinine values and patient’s age.<ref>{{Cite web|title = glomerular filtration rate|url = http://medical-dictionary.thefreedictionary.com/glomerular+filtration+rate|accessdate = 2015-06-27}}</ref> Normal eGFR is above 90 mm/min/1.73 m<sup>2</sup>; different stages of renal damage can be identified by eGFR intervals. |
Urinary albumin collection can also be timed (normal value <20 mg/min) or a random spot collection (normal value <30 μg/mg). Abnormal values correlate with nephropathy.Another diagnostic tool is glomerular filtration rate esteem ([[Estimated Glomerular Filtration Rate|eGFR]]) based on creatinine values and patient’s age.<ref>{{Cite web|title = glomerular filtration rate|url = http://medical-dictionary.thefreedictionary.com/glomerular+filtration+rate|accessdate = 2015-06-27}}</ref> Normal eGFR is above 90 mm/min/1.73 m<sup>2</sup>;<ref>{{Cite web|title = Reporting Glomerular Filtration Rate (GFR) - National Kidney Disease Education Program (NKDEP)|url = http://nkdep.nih.gov/lab-evaluation/gfr/reporting.shtml|website = nkdep.nih.gov|accessdate = 2015-06-27}}</ref> different stages of renal damage can be identified by eGFR intervals. |
||
== Treatment == |
== Treatment == |
||
Revision as of 17:42, 27 June 2015
| Diabetic nephropathy | |
|---|---|
| Specialty | Nephrology, endocrinology |
Diabetic nephropathy (nephropatia diabetica), also known as Kimmelstiel–Wilson syndrome, or nodular diabetic glomerulosclerosis and intercapillary glomerulonephritis, is a progressive kidney disease caused by angiopathy of capillaries in the kidney glomeruli.[1] [2]It is characterized by nephrotic syndrome and diffuse glomerulosclerosis. It is due to longstanding diabetes mellitus, and is a prime indication for dialysis in many developed countries. It is classified as a small blood vessel complication of diabetes.[3]
Signs and symptoms
Throughout its early course, diabetic nephropathy has no symptoms. They develop in late stages and may be a result of excretion of high amounts of protein in the urine or due to renal failure:[4]
Possible symptoms include:
- edema: swelling, usually around the eyes
- foamy appearance or excessive frothing of the urine (caused by the proteinuria)
- unintentional weight gain (from fluid accumulation)
- anorexia (poor appetite)
- nausea and vomiting
- malaise (general ill feeling)
- fatigue
- headache
- frequent hiccups.
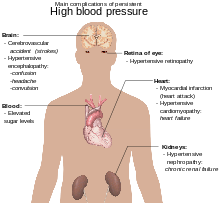
- hypertension
Cause
The word diabetes means "passing through", referring to the polyuria (abnormal increase of urine production), a symptom historically present in those affected by the disease. When the level of blood glucose rises beyond the kidney's capacity to reabsorb glucose from the renal ultrafiltrate, glucose remains diluted in the fluid, raising its osmotic pressure and causing more water to be carried out, thus, increasing the excreted urine volume. The increased volume dilutes the sodium chloride in the urine, signalling the macula densa to release more renin, causing vasoconstriction, a survival mechanism to retain water by passing less blood through the kidneys. Because the kidney is nurtured exclusively by the blood it filters, the vasoconstriction also reduces the nutrients supplied to it, causing infarct of its tissues and reduction of renal function.
Pathophysiology

Glomerular hyperfiltration is the basic pathophysiology in diabetic nephropathy. This leads to intraglomerular hypertension. ACE inhibitor drugs help prevent diabetic nephropathy by preventing this step. Progression from glomerular hyperfilteration leads to the stage of basement membrane thickening. This is the earliest detectable change in the course of diabetic nephropathy.[5] This is followed by expansion of mesangium and finally by nodular sclerosis. At this stage, the kidney may leak more serum albumin (plasma protein) than normal in the urine (albuminuria), and this can be detected by sensitive medical tests for albumin. This stage is called "microalbuminuria". As diabetic nephropathy progresses, increasing numbers of glomeruli are destroyed by progressive nodular glomerulosclerosis. Consequently, urine albumin increases to the point that it may be detected by ordinary urinalysis techniques. At this stage, a kidney biopsy generally clearly shows diabetic nephropathy.
Diagnosis
| CKD Stage | eGFR level (mL/min/1.73 m2) |
|---|---|
| Stage 1 | ≥ 90 |
| Stage 2 | 60 – 89 |
| Stage 3 | 30 – 59 |
| Stage 4 | 15 – 29 |
| Stage 5 | < 15 |
Diagnosis is based on the measurement of urinary albumin. We can define:[6]
- Normoalbuminuria: urinary albumin excretion <30 mg/24h, it is the physiological state;
- Microalbuminuria: urinary albumin excretion in the range of 30–299 mg/24h;
- Clinical (overt) albuminuria: urinary albumin excretion ≥300 mg/24h.
Diabetic patients are suggested to control albumin excretion every year. Urinary albumin collection can also be timed (normal value <20 mg/min) or a random spot collection (normal value <30 μg/mg). Abnormal values correlate with nephropathy.Another diagnostic tool is glomerular filtration rate esteem (eGFR) based on creatinine values and patient’s age.[7] Normal eGFR is above 90 mm/min/1.73 m2;[8] different stages of renal damage can be identified by eGFR intervals.
Treatment

The goals of treatment are to slow the progression of kidney damage and control related complications. The main treatment, once proteinuria is established, is ACE inhibitor drugs, which usually reduces proteinuria levels and slows the progression of diabetic nephropathy. [9] Several effects of the ACEIs that may contribute to renal protection have been related to the association of rise in Kinins which is also responsible for some of the side effects associated with ACEIs therapy such as dry cough. The renal protection effect is related to the antihypertensive effects in normal and hypertensive patients, renal vasodilatation resulting in increased renal blood flow and dilatation of the efferent arterioles. Many studies have shown that related drugs, angiotensin receptor blockers (ARBs), have a similar benefit.
Patients with diabetic nephropathy should avoid taking the following drugs:
- Contrast agents containing iodine
- Commonly used non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and naproxen, or COX-2 inhibitors like celecoxib, because they may injure the weakened kidney.
Prognosis

Diabetic nephropathy , in type 2 diabetes can be more difficult to predict, because the date of onset is not usually established. Without intervention 20 - 40 percent of patients with type 2 diabetes/microalbuminuria, will evolve to macroalbuminuria.[10]
Possible complications include:
- hypoglycemia (due to decreased renal clearance of insulin)
- rapidly progressing chronic kidney failure
- end-stage kidney disease
- hyperkalemia
- severe hypertension
- complications of hemodialysis
- complications of kidney transplant
- coexistence of other diabetes complications
- peritonitis (if peritoneal dialysis used)
- increased infections
Epidemiology
In the U.S. Diabetic nephropathy affected 6.9 million (2005-2008).[11] The number of people with diabetes is expected to rise by the year 2050, therefore so will Diabetic nephropathy ( and equal rise in end-stage renal disease).[12]
See also
References
- ^ "diabetic nephropathy". Retrieved 2015-06-27.
- ^ "Diabetes and kidney disease: MedlinePlus Medical Encyclopedia". www.nlm.nih.gov. Retrieved 2015-06-27.
- ^ Longo et al., Harrison's Principles of Internal Medicine, 18th ed., p.2982
- ^ "Diabetic nephropathy: MedlinePlus Medical Encyclopedia Image". www.nlm.nih.gov. Retrieved 2015-06-27.
- ^ Press, Dove. "Diabetic nephropathy – complications and treatment | IJNRD". www.dovepress.com. Retrieved 2015-06-27.
- ^ Martin, Helen (2011). "Laboratory Measurement of Urine Albumin and Urine Total Protein in Screening for Proteinuria in Chronic Kidney Disease". The Clinical Biochemist Reviews. 32 (2): 97–102. ISSN 0159-8090. PMC 3100287. PMID 21611083.
- ^ "glomerular filtration rate". Retrieved 2015-06-27.
- ^ "Reporting Glomerular Filtration Rate (GFR) - National Kidney Disease Education Program (NKDEP)". nkdep.nih.gov. Retrieved 2015-06-27.
- ^ Lim, Andy KH (2014-10-15). "Diabetic nephropathy – complications and treatment". International Journal of Nephrology and Renovascular Disease. 7: 361–381. doi:10.2147/IJNRD.S40172. ISSN 1178-7058. PMC 4206379. PMID 25342915.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Shlipak, Michael. "Clinical Evidence Handbook: Diabetic Nephropathy: Preventing Progression - American Family Physician". www.aafp.org. Retrieved 2015-06-27.
- ^ Lerma, Edgar V. (2014-01-01). Diabetes and Kidney Disease. Springer. ISBN 9781493907939.
- ^ Lai, K. N.; Tang, S. C. W. (2011-06-08). Diabetes and the Kidney. Karger Medical and Scientific Publishers. ISBN 9783805597432.
Further reading
- Gross, Jorge L.; Azevedo, Mirela J. de; Silveiro, Sandra P.; Canani, Luís Henrique; Caramori, Maria Luiza; Zelmanovitz, Themis (2005). "Diabetic Nephropathy: Diagnosis, Prevention, and Treatment". Diabetes Care. 28 (1): 164–176. doi:10.2337/diacare.28.1.164. ISSN 0149-5992. PMID 15616252.
This template is no longer used; please see Template:Endocrine pathology for a suitable replacement
