Progesterone
 | |
 | |
| Clinical data | |
|---|---|
| Other names | 4-pregnene-3,20-dione |
| Pregnancy category |
|
| Routes of administration | oral, implant |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | prolonged absorption, half-life approx 25-50 hours |
| Protein binding | 96%-99% |
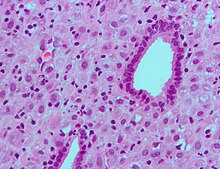
| Metabolism | hepatic to pregnanediols and pregnanolones |
| Elimination half-life | 34.8-55.13 hours |
| Excretion | renal |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.000.318 |
| Chemical and physical data | |
| Formula | C21H30O2 |
| Molar mass | 314.46 g·mol−1 |
| Specific rotation | [α]D |
| Melting point | 126 °C (259 °F) |
Progesterone is a C-21 steroid hormone involved in the female menstrual cycle, pregnancy (supports gestation) and embryogenesis of humans and other species. Progesterone belongs to a class of hormones called progestogens, and is the major naturally occurring human progestogen.
Progesterone should not be confused with progestins, which are synthetically produced progestogens.
Progesterone is commonly manufactured from the yam family, Dioscorea. Dioscorea produces large amounts of a steroid called diosgenin, which can be converted into progesterone in the laboratory. There is debate at how much if any conversion may occur between Dioscorea spp to progesterone in humans.[citation needed]
Sources
Plant
Outside progesterone-producing animals such as humans, progesterone-like steroids are found in Dioscorea mexicana. Dioscorea mexicana is a plant that is part of the yam family and resides in Mexico.[2] It contains a steroid called diosgenin that is taken from the plant and is converted into progesterone.[3] Diosgenin and progesterone are found in other Dioscorea species as well.
Another plant that has been discovered to indirectly contain progesterone is Dioscorea pseudojaponica that resides in Taiwan. Research has showed that the Taiwanese yam contained saponins, steroids, which are converted to diosgenin. From diosgenin, it can produce progesterone.[4]
Another plant that is found to contain these steroids that convert to progesterone is a wild yam called Dioscorea villosa. One study showed that the Dioscorea villosa contains 3.5% of diosgenin.[5] There are many other Dioscorea species of the yam family that contribute to the production of progesterone, but there is one new species found. Dioscorea polygonoides has been researched and found 2.64% of diosgenin that was recognized by testing it with gas chromatography-mass spectrometry.[6] Many of the Dioscorea species that originate from the yam family grow in countries that have tropical and subtropical climates.[7]
Animal
Progesterone is produced in the ovaries (specifically after ovulation in the corpus luteum), the brain, and, during pregnancy, in the placenta.
In humans, increasing amounts of progesterone are produced during pregnancy:
- Initially, the source is the corpus luteum that has been "rescued" by the presence of human chorionic gonadotropins (hCG) from the conceptus.
- However, after the 8th week production of progesterone shifts to the placenta. The placenta utilizes maternal cholesterol as the initial substrate, and most of the produced progesterone enters the maternal circulation, but some is picked up by the fetal circulation and used as substrate for fetal corticosteroids. At term the placenta produces about 250 mg progesterone per day.
- An additional source of progesterone is milk products. They contain much progesterone because on dairy farms cows are milked during pregnancy, when the progesterone content of the milk is high. After consumption of milk products the level of bioavailable progesterone goes up.[8] This observation has resulted in concern that diets high in dairy products might induce pet and human diseases.[9]
Chemistry
Progesterone was independently discovered by four research groups.[10][11][12][13]
Willard Myron Allen co-discovered progesterone with his anatomy professor George Washington Corner at the University of Rochester Medical School in 1933. Allen first determined its melting point, molecular weight, and partial molecular structure. He also gave it the name Progesterone derived from Progestational Steroidal ketone.[14]
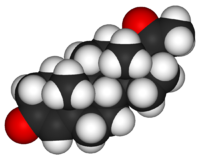
Like other steroids, progesterone consists of four interconnected cyclic hydrocarbons. Progesterone contains ketone and oxygenated functional groups, as well as two methyl branches. Like all steroid hormones, it is hydrophobic.
Synthesis
Biosynthesis

Bottom: progesterone is important for aldosterone (mineralocorticoid) synthesis, as 17-hydroxyprogesterone is for cortisol (glucocorticoid), and androstenedione for sex steroids.
Cholesterol undergoes oxidation by NADPH twice to make 2. It then again undergoes oxidation by NADPH to produce pregnenolone 3 which is then reduced by NAD+ to form 4. Afterwards, keto-enol tautomerism turns 4 into 5. Lastly, it tautomerizes by enol-keto to produce progesterone.[15] A study has proven that pregenolone and progesterone can also be biosynthesized by yeast.[16]
Progesterone, like all other steroid hormones, is synthesized from pregnenolone, a derivative of cholesterol. This conversion takes place in two steps. The 3-hydroxyl group is converted to a keto group and the double bond is moved to C-4, from C-5.
Progesterone is the precursor of the mineralocorticoid aldosterone, and after conversion to 17-hydroxyprogesterone (another natural progestogen) of cortisol and androstenedione. Androstenedione can be converted to testosterone, estrone and estradiol.
Laboratory

A total synthesis of progesterone was reported in 1971 by W.S. Johnson (see figure to the right).[17] The synthesis begins with reacting the phosphonium salt 7 with phenyl lithium in tetrahydrofuran to produce the phosphonium ylide 8. The ylide 8 is reacted with an aldehyde to produce the alkene 9. The ketal protecting groups of 9 are hydrolyzed to produce the diketone 10 which in turn is cyclized to from the cyclopentenone 11. The ketone of 11 is reacted with methyl lithium to yield the tertiary alcohol 12 which in turn is treated with acid to produce the tertiary cation 13. The key step of the synthesis is the π-cation cyclization of 13 in which the B-, C-, and D-rings of the steroid are simultaneously formed to produce 14. This step resembles the cationic cyclization reaction used in the biosynthesis of steroids and hence is referred to as biomimetic. In the next step the enol orthoester is hydrolyzed to produce the ketone 15. The cyclopentene A-ring is then opened by oxidizing with ozone to produce 16. Finally, the diketone 16 undergoes an intramolecular aldol condensation by treating with aqueous potassium hydroxide to produce progesterone.[17]
A semisynthesis of progesterone is much simpler than the previous one because it will only focus on the regioselectivity. In this semi-synthesis, there are two ways to produce progesterone, but each way ends with a different yield. For the first semi-synthesis, desoxycorticosterone reacts with Me3SiI in CHCl3 to lose a hydroxyl group and produce progesterone. Using CHCl3 as a solvent, it gives the product at lower yield, but it produces progesterone at a greater amount of 90%. As for the second semi-synthesis, descoxycorticosterone reacts with Me3SiI in MeCN to make progesterone as a result of losing a hydroxyl group. MeCN as a solvent produces progesterone at a higher yield, but at a lower production amount of 78%.[18]
Levels
In women, progesterone levels are relatively low during the preovulatory phase of the menstrual cycle, rise after ovulation, and are elevated during the luteal phase. Progesterone levels tend to be < 2 ng/ml prior to ovulation, and > 5 ng/ml after ovulation. If pregnancy occurs, progesterone levels are initially maintained at luteal levels. With the onset of the luteal-placental shift in progesterone support of the pregnancy, levels start to rise further and may reach 100-200 ng/ml at term. Whether a decrease in progesterone levels is critical for the initiation of labor has been argued and may be species-specific. After delivery of the placenta and during lactation, progesterone levels are very low.
Progesterone levels are relatively low in children and postmenopausal women.[19] Adult males have levels similar to those in women during the follicular phase of the menstrual cycle.
Effects
Progesterone exerts its primary action through the intracellular progesterone receptor although a distinct, membrane bound progesterone receptor has also been postulated.[20][21]. Additionally, progesterone is a highly potent antagonist of the mineralocorticoid receptor (MR, the receptor for aldosterone and other mineralocorticosteroids). It prevents MR activation by binding to this receptor with an affinity exceeding even those of aldosterone and other corticosteroids such as cortisol and corticosterone [22].
Progesterone has a number of physiological effects which are amplified in the presence of estrogen. Estrogen through estrogen receptors upregulates the expression of progesterone receptors. [23]. Also, elevated levels of progesterone potently reduce the sodium-retaining activity of aldosterone, resulting in natriuresis and a reduction in extracellular fluid volume. Progesterone withdrawal, on the other hand, is associated with a temporary increase in sodium retention (reduced natriuresis, with an increase in extracellular fluid volume) due to the compensatory increase in aldosterone production which combats the blockade of the mineralocorticoid receptor by the previously elevated level of progesterone[24].
Reproductive system
Progesterone is sometimes called the "hormone of pregnancy",[25] and it has many roles relating to the development of the fetus:
- Progesterone converts the endometrium to its secretory stage to prepare the uterus for implantation. At the same time progesterone affects the vaginal epithelium and cervical mucus, making the mucus thick and impermeable to sperm. If pregnancy does not occur, progesterone levels will decrease, leading, in the human, to menstruation. Normal menstrual bleeding is progesterone withdrawal bleeding.
- During implantation and gestation, progesterone appears to decrease the maternal immune response to allow for the acceptance of the pregnancy.
- Progesterone decreases contractility of the uterine smooth muscle.[25]
- In addition progesterone inhibits lactation during pregnancy. The fall in progesterone levels following delivery is one of the triggers for milk production.
- A drop in progesterone levels is possibly one step that facilitates the onset of labor.
The fetus metabolizes placental progesterone in the production of adrenal mineralo- and glucosteroids.
Nervous system
Progesterone, like pregnenolone and dehydroepiandrosterone, belongs to the group of neurosteroids that are found in high concentrations in certain areas in the brain and are synthesized there.
Neurosteroids affect synaptic functioning, are neuroprotective, and affect myelination.[26] They are investigated for their potential to improve memory and cognitive ability.
Progesterone as neuroprotectant affects regulation of apoptotic genes.
Its effect as a neurosteroid works predominantly through the GSK-3 beta pathway, as an inhibitor. (Other GSK-3 beta inhibitors include bipolar mood stabilizers, lithium and valproic acid.)
Other systems
- It raises epidermal growth factor-1 levels, a factor often used to induce proliferation, and used to sustain cultures, of stem cells.
- It increases core temperature (thermogenic function) during ovulation.[27]
- It reduces spasm and relaxes smooth muscle. Bronchi are widened and mucus regulated. (Progesterone receptors are widely present in submucosal tissue.)
- It acts as an antiinflammatory agent and regulates the immune response.
- It reduces gall-bladder activity.[28]
- It normalizes blood clotting and vascular tone, zinc and copper levels, cell oxygen levels, and use of fat stores for energy.
- It may affect gum health, increasing risk of gingivitis (gum inflammation) and tooth decay.
- It appears to prevent endometrial cancer (involving the uterine lining) by regulating the effects of estrogen.
Medical applications
The use of progesterone and its analogues have many medical applications -- both to address acute situations, and to address the long-term decline of natural progesterone levels. Because of the poor bioavailability of progesterone when taken orally, many synthetic progestins have been designed. However, the roles of progesterone may not be fulfilled by the synthetic progestins which in some cases were designed solely to mimic progesterone's uterine effects.
Bioavailability
Progesterone is poorly absorbed by oral ingestion unless micronised and in oil, or with fatty foods; it does not dissolve in water. Products such as Prometrium, Utrogestan, Minagest and Microgest are therefore capsules containing micronised progesterone in oil - in all three mentioned the oil is peanut oil, which may cause serious allergic reactions in some people, but compounding pharmacies, which have the facilities and licenses to make their own products, can use alternatives. Vaginal and rectal application is also effective, with products such as ENDOMETRIN (progesterone) Vaginal Insert 100 mg, approved by the FDA in June 2007 to support embryo implantation and early pregnancy. Other products are CRINONE and PROCHIEVE bioadhesive progesterone vaginal gels (the first progesterone products FDA-approved for use in infertility and during pregnancy) and Cyclogest, which is progesterone in cocoa butter in the form of pessaries. Progesterone can be given by injection, but because it has a short half-life they need to be daily. Marketing of progesterone phamaceutical products, country to country, varies considerably, with many countries having no oral progesterone products marketed, but they can usually be specially imported by pharmacies through international wholesalers.
"Natural progesterone" products derived from yams, do not require a prescription. Wild yams contain a plant steroid called diosgenin, however there is no evidence that the human body can metabolize diosgenin into progesterone.[29][30] Diosgenin can however be chemically converted into progesterone in the lab.[31]
Specific uses
- Progesterone is used to support pregnancy in Assisted Reproductive Technology (ART) cycles such as In-vitro Fertilization (IVF). While daily intramuscular injections of progesterone-in-oil (PIO) have been the standard route of administration, PIO injections are not FDA-approved for use in pregnancy. A recent meta-analysis showed that the intravaginal route with an appropriate dose and dosing frequency is equivalent to daily intramuscular injections.[32] In addition, a recent case-matched study comparing vaginal progesterone with PIO injections showed that live birth rates were nearly identical with both methods. [33]
- Progesterone is used to control anovulatory bleeding. It is also used to prepare uterine lining in infertility therapy and to support early pregnancy. Patients with recurrent pregnancy loss due to inadequate progesterone production may receive progesterone.
- Progesterone is being investigated as potentially beneficial in treating multiple sclerosis, since the characteristic deterioration of nerve myelin insulation halts during pregnancy, when progesterone levels are raised; deterioration commences again when the levels drop.
- Vaginally dosed progesterone is being investigated as potentially beneficial in preventing preterm birth in women at risk for preterm birth. The initial study by Fonseca suggested that vaginal progesterone could prevent preterm birth in women with a history of preterm birth.[34]
A subsequent and larger study showed that vaginal progesterone was no better than placebo in preventing recurrent preterm birth in women with a history of a previous preterm birth,[35] but a planned secondary analysis of the data in this trial showed that women with a short cervix at baseline in the trial had benefit in two ways: a reduction in births less than 32 weeks and a reduction in both the frequency and the time their babies were in intensive care.[36] In another trial, vaginal progesterone was shown to be better than placebo in reducing preterm birth prior to 34 weeks in women with an extremely short cervix at baseline.[37] An editorial by Roberto Romero discusses the role of sonographic cervical length in identifying patients who may benefit from progesterone treatment.[38]
- Progesterone is used in hormone therapy for transsexual women and other women with intersex conditions - especially when synthetic progestins have been ineffective or caused side-effects - since normal breast tissue cannot develop except in the presence of both progestogen and estrogen. Mammary glandular tissue is otherwise fibrotic, the breast shape conical and the areola immature. Progesterone can correct those even after years of inadequate hormonal treatment. Research usually cited against such value was conducted using Provera, a synthetic progestin. Progesterone also has a role in skin elasticity and bone strength, in respiration, in nerve tissue and in female sexuality, and the presence of progesterone receptors in certain muscle and fat tissue may hint at a role in sexually-dimorphic proportions of those.
- Progesterone receptor antagonists, or selective progesterone receptor modulators (SPRM)s, such as RU-486 (Mifepristone), can be used to prevent conception or induce medical abortions.
Note that methods of hormonal contraception do not contain progesterone but a progestin.
Progesterone may affect male behavior.[39]
Progesterone is starting to be used in the treatment of the skin condition hidradenitis suppurativa.[citation needed]
Aging
Since most progesterone in males is created during testicular production of testosterone, and most in females by the ovaries, the shutting down (whether by natural or chemical means), or removal, of those inevitably causes a considerable reduction in progesterone levels. Previous concentration upon the role of progestagens (progesterone and molecules with similar effects) in female reproduction, when progesterone was simply considered a "female hormone", obscured the significance of progesterone elsewhere in both sexes.
The tendency for progesterone to have a regulatory effect, the presence of progesterone receptors in many types of body tissue, and the pattern of deterioration (or tumor formation) in many of those increasing in later years when progesterone levels have dropped, is prompting widespread research into the potential value of maintaining progesterone levels in both males and females.
Brain damage
It has been observed in animal models that females have reduced susceptibility to traumatic brain injury and this protective effect has been hypothesized to be caused by increased circulating levels of estrogen and progesterone in females.[40] A number of additional animal studies have confirmed that progesterone has neuroprotective effects when administered shortly after traumatic brain injury.[41] Encouraging results have also been reported in human clinical trials.[42][43]
The mechanism of progesterone protective effects may be the reduction of inflammation which follows brain trauma.[44]
See also
References
- ^ "FDA-sourced list of all drugs with black box warnings (Use Download Full Results and View Query links.)". nctr-crs.fda.gov. FDA. Retrieved 22 Oct 2023.
- ^ Applezweig N (1969). "Steroids". Chem Week. 104: 57–72. PMID 12255132.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Noguchi E, Fujiwara Y, Matsushita S, Ikeda T, Ono M, Nohara T (2006). "Metabolism of tomato steroidal glycosides in humans" ([dead link] – Scholar search). Chem. Pharm. Bull. 54 (9): 1312–4. doi:10.1248/cpb.54.1312. PMID 16946542.
{{cite journal}}: External link in|format=|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Yang DJ, Lu TJ, Hwang LS (2003). "Isolation and identification of steroidal saponins in Taiwanese yam cultivar (Dioscorea pseudojaponica Yamamoto)". J. Agric. Food Chem. 51 (22): 6438–44. doi:10.1021/jf030390j. PMID 14558759.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Hooker E (2004). "Final report of the amended safety assessment of Dioscorea Villosa (Wild Yam) root extract". Int. J. Toxicol. 23 Suppl 2: 49–54. doi:10.1080/10915810490499055. PMID 15513824.
- ^ 5 Nino, J.; Jimenez, D. A.; Mosquera, O. M.; Correa, Y. M. Diosgenin Quantification by Hplc in a Dioscorea Polygonoides Tuber Collection from Columbian Flora. J. Braz. Chem. Soc. 2007, 18, 1073-1076.
- ^ 6 Myoda, T.; Nagai, T.; Nagashima, T. Properties of Starches in Yam (Dioscorea Spp.) Tuber. Curr. Top. Food. Sci. Technol. 2005, 105-114.
- ^ Goodson III WH, Handagama P, Moore II DH, Dairkee S (2007-12-13). "Milk products are a source of dietary progesterone". 30th Annual San Antonio Breast Cancer Symposium. pp. abstract # 2028. Retrieved 2008-03-12.
{{cite web}}: Cite has empty unknown parameter:|coauthors=(help)CS1 maint: multiple names: authors list (link) - ^ Elisabeth Rieping (2008-01-01). "Breast Cancer and Progesterone from the Milk of Pregnant Cows". Retrieved 2008-03-12.
{{cite web}}: Cite has empty unknown parameter:|coauthors=(help) - ^ Allen WM (1935). "The isolation of crystalline progestin". Science. 82 (2118): 89–93. doi:10.1126/science.82.2118.89. PMID 17747122.
- ^ Butenandt A, Westphal U (1934). "Zur Isolierung und Charakterisierung des Corpusluteum-Hormons". Berichte Deutsche chemische Gesellschaft. 67: 1440–1442. doi:10.1002/cber.19340670831.
- ^ Hartmann M, Wettstein A (1934). "Ein krystallisiertes Hormon aus Corpus luteum". Helvetica Chimica Acta. 17: 878–882. doi:10.1002/hlca.193401701111.
- ^ Slotta KH, Ruschig H, Fels E (1934). "Reindarstellung der Hormone aus dem Corpusluteum". Berichte Deutsche chemische Gesellschaft. 67: 1270–1273. doi:10.1002/cber.19340670729.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Allen WM (1970). "Progesterone: how did the name originate?". South. Med. J. 63 (10): 1151–5. PMID 4922128.
- ^ Dewick, Paul M. (2002). Medicinal natural products: a biosynthetic approach. New York: Wiley. pp. page 244. ISBN 0-471-49641-3.
{{cite book}}:|pages=has extra text (help) - ^ Duport C, Spagnoli R, Degryse E, Pompon D (1998). "Self-sufficient biosynthesis of pregnenolone and progesterone in engineered yeast". Nat. Biotechnol. 16 (2): 186–9. doi:10.1038/nbt0298-186. PMID 9487528.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ a b c Johnson WS, Gravestock MB, McCarry BE (1971). "Acetylenic bond participation in biogenetic-like olefinic cyclizations. II. Synthesis of dl-progesterone". J. Am. Chem. Soc. 93 (17): 4332–4. PMID 5131151.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Numazawa M, Nagaoka M, Kunitama Y (1986). "Regiospecific deoxygenation of the dihydroxyacetone moiety at C-17 of corticoid steroids with iodotrimethylsilane". Chem. Pharm. Bull. 34 (9): 3722–6. PMID 3815593.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ NIH Clinical Center (2004-08-16). "Progesterone Historical Reference Ranges". United States National Institutes of Health. Retrieved 2008-03-12.
{{cite web}}: Cite has empty unknown parameter:|coauthors=(help) - ^ Luconi M, Bonaccorsi L, Maggi M, Pecchioli P, Krausz C, Forti G, Baldi E (1998). "Identification and characterization of functional nongenomic progesterone receptors on human sperm membrane". J. Clin. Endocrinol. Metab. 83 (3): 877–85. doi:10.1210/jc.83.3.877. PMID 9506743.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Jang S, Yi LS (2005). "Identification of a 71 kDa protein as a putative non-genomic membrane progesterone receptor in boar spermatozoa". J. Endocrinol. 184 (2): 417–25. doi:10.1677/joe.1.05607. PMID 15684349.
- ^ ">Rupprecht R, Reul JM, van Steensel B, Spengler D, Söder M, Berning B, Holsboer F, Damm K (1993). "Pharmacological and functional characterization of human mineralocorticoid and glucocorticoid receptor ligands". Eur J Pharmacol. 247 (2): 145–54. doi:10.1016/0922-4106(93)90072-H. PMID 8282004.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Kastner P, Krust A, Turcotte B, Stropp U, Tora L, Gronemeyer H, Chambon P (1990). "Two distinct estrogen-regulated promoters generate transcripts encoding the two functionally different human progesterone receptor forms A and B". Embo J. 9 (5): 1603–14. PMID 2328727.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Landau RL, Bergenstal DM, Lugibihl K, Kascht ME. (1955). "The metabolic effects of progesterone in man". J Clin Endocrinol Metab. 15 (10): 1194–215. PMID 13263410.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Bowen R (2000-08-06). "Placental Hormones". Retrieved 2008-03-12.
{{cite web}}: Cite has empty unknown parameter:|coauthors=(help) - ^ Schumacher M, Guennoun R, Robert F; et al. (2004). "Local synthesis and dual actions of progesterone in the nervous system: neuroprotection and myelination". Growth Horm. IGF Res. 14 Suppl A: S18–33. doi:10.1016/j.ghir.2004.03.007. PMID 15135772.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Template:GeorgiaPhysiology
- ^ Hould FS, Fried GM, Fazekas AG, Tremblay S, Mersereau WA (1988). "Progesterone receptors regulate gallbladder motility". J. Surg. Res. 45 (6): 505–12. doi:10.1016/0022-4804(88)90137-0. PMID 3184927.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Zava DT, Dollbaum CM, Blen M (1998). "Estrogen and progestin bioactivity of foods, herbs, and spices". Proc. Soc. Exp. Biol. Med. 217 (3): 369–78. PMID 9492350.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Komesaroff PA, Black CV, Cable V, Sudhir K (2001). "Effects of wild yam extract on menopausal symptoms, lipids and sex hormones in healthy menopausal women". Climacteric. 4 (2): 144–50. doi:10.1080/713605087. PMID 11428178.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Marker RE, Krueger J (1940). "Sterols. CXII. Sapogenins. XLI. The Preparation of Trillin and its Conversion to Progesterone". J. Am. Chem. Soc. 62 (12): 3349–3350. doi:10.1021/ja01869a023.
- ^ Zarutskiea PW, Phillips JA (2007). "Re-analysis of vaginal progesterone as luteal phase support (LPS) in assisted reproduction (ART) cycles". Fertility and Sterility. 88 (supplement 1): S113. doi:10.1016/j.fertnstert.2007.07.365.
- ^ Khan N, Richter KS, Blake EJ, et al. Case-matched comparison of intramuscular versus vaginal progesterone for luteal phase support after in vitro fertilization and embryo transfer. Presented at: 55th Annual Meeting of the Pacific Coast Reproductive Society; April 18-22, 2007; Rancho Mirage, CA.
- ^ da Fonseca EB, Bittar RE, Carvalho MH, Zugaib M (2003). "Prophylactic administration of progesterone by vaginal suppository to reduce the incidence of spontaneous preterm birth in women at increased risk: a randomized placebo-controlled double-blind study". Am. J. Obstet. Gynecol. 188 (2): 419–24. doi:10.1067/mob.2003.41. PMID 12592250.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ O'Brien JM, Adair CD, Lewis DF, Hall DR, Defranco EA, Fusey S, Soma-Pillay P, Porter K, How H, Schackis R, Eller D, Trivedi Y, Vanburen G, Khandelwal M, Trofatter K, Vidyadhari D, Vijayaraghavan J, Weeks J, Dattel B, Newton E, Chazotte C, Valenzuela G, Calda P, Bsharat M, Creasy GW (2007). "Progesterone vaginal gel for the reduction of recurrent preterm birth: primary results from a randomized, double-blind, placebo-controlled trial". Ultrasound Obstet Gynecol. 30 (5): 687–96. doi:10.1002/uog.5158. PMID 17899572.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ DeFranco EA, O'Brien JM, Adair CD, Lewis DF, Hall DR, Fusey S, Soma-Pillay P, Porter K, How H, Schakis R, Eller D, Trivedi Y, Vanburen G, Khandelwal M, Trofatter K, Vidyadhari D, Vijayaraghavan J, Weeks J, Dattel B, Newton E, Chazotte C, Valenzuela G, Calda P, Bsharat M, Creasy GW (2007). "Vaginal progesterone is associated with a decrease in risk for early preterm birth and improved neonatal outcome in women with a short cervix: a secondary analysis from a randomized, double-blind, placebo-controlled trial". Ultrasound Obstet Gynecol. 30 (5): 697–705. doi:10.1002/uog.5159. PMID 17899571.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Fonseca EB, Celik E, Parra M, Singh M, Nicolaides KH (2007). "Progesterone and the risk of preterm birth among women with a short cervix". N. Engl. J. Med. 357 (5): 462–9. doi:10.1056/NEJMoa067815. PMID 17671254.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Romero R (2007). "Prevention of spontaneous preterm birth: the role of sonographic cervical length in identifying patients who may benefit from progesterone treatment". Ultrasound Obstet Gynecol. 30 (5): 675–86. doi:10.1002/uog.5174. PMID 17899585.
- ^ Schneider JS, Stone MK, Wynne-Edwards KE, Horton TH, Lydon J, O'Malley B, Levine JE (2003). "Progesterone receptors mediate male aggression toward infants". Proc. Natl. Acad. Sci. U.S.A. 100 (5): 2951–6. doi:10.1073/pnas.0130100100. PMID 12601162.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Roof RL, Hall ED (2000). "Gender differences in acute CNS trauma and stroke: neuroprotective effects of estrogen and progesterone". J. Neurotrauma. 17 (5): 367–88. doi:10.1089/neu.2000.17.367. PMID 10833057.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Gibson CL, Gray LJ, Bath PM, Murphy SP (2008). "Progesterone for the treatment of experimental brain injury; a systematic review". Brain. 131 (Pt 2): 318–28. doi:10.1093/brain/awm183. PMID 17715141.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Wright DW, Kellermann AL, Hertzberg VS, Clark PL, Frankel M, Goldstein FC, Salomone JP, Dent LL, Harris OA, Ander DS, Lowery DW, Patel MM, Denson DD, Gordon AB, Wald MM, Gupta S, Hoffman SW, Stein DG (2007). "ProTECT: a randomized clinical trial of progesterone for acute traumatic brain injury". Ann Emerg Med. 49 (4): 391–402, 402.e1–2. doi:10.1016/j.annemergmed.2006.07.932. PMID 17011666.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Xiao G, Wei J, Yan W, Wang W, Lu Z (2008). "Improved outcomes from the administration of progesterone for patients with acute severe traumatic brain injury: a randomized controlled trial". Crit Care. 12 (2): R61. doi:10.1186/cc6887. PMID 18447940.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - ^ Pan DS, Liu WG, Yang XF, Cao F (2007). "Inhibitory effect of progesterone on inflammatory factors after experimental traumatic brain injury". Biomed. Environ. Sci. 20 (5): 432–8. PMID 18188998.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link)
Additional images

External links
- Progesterone at the U.S. National Library of Medicine Medical Subject Headings (MeSH)
- Kimball JW (2007-05-27). "Progesterone". Kimball's Biology Pages. Retrieved 2008-06-18.
{{cite web}}: Cite has empty unknown parameter:|coauthors=(help) - "Progesterone Resource Center". PMS, Menopause, and Progesterone Resource Center. Oasis Advanced Wellness, Inc. Retrieved 2008-06-18.
{{cite web}}: Cite has empty unknown parameter:|coauthors=(help) - Infertility - possible Treatments and Causes
- Ovulation and How it happens, Triggers and How to Help it Occur
- General discussion document on Progesterone, it's uses and applications

