Chronic granulomatous disease
This article needs additional citations for verification. (January 2010) |
| Chronic granulomatous disease | |
|---|---|
| Specialty | Immunology |
Chronic granulomatous disease (CGD) (also known as Bridges–Good syndrome, Chronic granulomatous disorder, and Quie syndrome[1]) is a diverse group of hereditary diseases in which certain cells of the immune system have difficulty forming the reactive oxygen compounds (most importantly the superoxide radical due to defective phagocyte NADPH oxidase) used to kill certain ingested pathogens.[2] This leads to the formation of granulomata in many organs.[3] CGD affects about 1 in 200,000 people in the United States, with about 20 new cases diagnosed each year.[4][5]
This condition was first discovered in 1950 in a series of 4 boys from Minnesota, and in 1957 was named "a fatal granulomatosus of childhood" in a publication describing their disease.[6][7] The underlying cellular mechanism that causes chronic granulomatous disease was discovered in 1967, and research since that time has further elucidated the molecular mechanisms underlying the disease.[8] Bernard Babior made key contributions in linking the defect of superoxide production of white blood cells, to the etiology of the disease. In 1986, the X-linked form of CGD was the first disease for which positional cloning was used to identify the underlying genetic mutation.
Classification
This section needs expansion. You can help by adding to it. (May 2009) |
Chronic granulomatous disease is the name for a genetically heterogeneous group of immunodeficiencies. The core defect is a failure of phagocytic cells to kill organisms that they have engulfed because of defects in a system of enzymes that produce free radicals and other toxic small molecules. There are several types, including:[9]
- X-linked chronic granulomatous disease]] (CGD)
- autosomal recessive cytochrome b-negative CGD
- autosomal recessive cytochrome b-positive CGD type I
- autosomal recessive cytochrome b-positive CGD type II
- atypical granulomatous disease
Symptoms
Classically, patients with chronic granulomatous disease will suffer from recurrent bouts of infection due to the decreased capacity of their immune system to fight off disease-causing organisms. The recurrent infections they acquire are specific and are, in decreasing order of frequency:
- pneumonia
- abscesses of the skin, tissues, and organs
- suppurative arthritis
- osteomyelitis
- bacteremia/fungemia
- superficial skin infections such as cellulitis or impetigo
Most people with CGD are diagnosed in childhood, usually before age 5.[10] Early diagnosis is important since these people can be placed on antibiotics to ward off infections before they occur. Small groups of CGD patients may also be affected by McLeod syndrome because of the proximity of the two genes on the same X-chromosome.[citation needed]
Atypical infections
People with CGD are sometimes infected with organisms that usually do not cause disease in people with normal immune systems. Among the most common organisms that cause disease in CGD patients are:
- bacteria (particularly those that are catalase-positive)[11]
- Staphylococcus aureus.
- Serratia marcescens.
- Listeria species.
- E. coli.
- Klebsiella species.
- Pseudomonas cepacia, a.k.a. Burkholderia cepacia.[12]
- Nocardia.[13]
- fungi
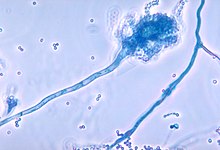
- Aspergillus species. Aspergillus has a propensity to cause infection in people with CGD and of the Aspergillus species, Aspergillus fumigatus seems to be most common in CGD.
- Candida species.
Patients with CGD can usually resist infections of catalase-negative bacteria. Catalase is an enzyme that catalyzes the breakdown of hydrogen peroxide in many organisms. In organisms that lack catalase (catalase-negative), normal metabolic functions will cause an accumulation of hydrogen peroxide which the host's immune system can use to fight off the infection. In organisms that have catalase (catalase-positive), the enzyme breaks down any hydrogen peroxide that was produced through normal metabolism. Therefore hydrogen peroxide will not accumulate, leaving the patient vulnerable to catalase-positive bacteria.
Genetics
Most cases of chronic granulomatous disease are transmitted as a mutation on the X chromosome and are thus called an "X-linked trait".[10] The affected gene on the X chromosome codes for the gp91 protein p91-PHOX (p is the weight of the protein in kDa; the g means glycoprotein). CGD can also be transmitted in an autosomal recessive fashion (via CYBA and NCF1) and affects other PHOX proteins. The type of mutation that causes both types of CGD are varied and may be deletions, frame-shift, nonsense, and missense.[14][15]
A low level of NADPH, the cofactor required for superoxide synthesis, can lead to CGD. This has been reported in women who are homozygous for the genetic defect causing glucose-6-phosphate dehydrogenase deficiency (G6PD), which is characterised by reduced NADPH levels.[citation needed]
Pathophysiology

Phagocytes (i.e., neutrophils and macrophages) require an enzyme to produce reactive oxygen species to destroy bacteria after they are ingested (phagocytosis), a process known as the respiratory burst. This enzyme is termed "phagocyte NADPH oxidase" (PHOX). This enzyme oxidizes NADPH and reduces molecular oxygen to produce superoxide anions, a reactive oxygen species. Superoxide is then disproportionated into peroxide and molecular oxygen by superoxide dismutase. Finally, peroxide is used by myeloperoxidase to oxidize chloride ions into hypochlorite (the active component of bleach), which is toxic to bacteria. Thus, NADPH oxidase is critical for phagocyte killing of bacteria through reactive oxygen species.
(Two other mechanisms are used by phagocytes to kill bacteria: nitric oxide and proteases, but the loss of ROS-mediated killing alone is sufficient to cause chronic granulomatous disease.)
Defects in one of the four essential subunits of phagocyte NADPH oxidase (PHOX) can all cause CGD of varying severity, dependent on the defect. There are over 410 known possible defects in the PHOX enzyme complex that can lead to chronic granulomatous disease.[3]
Diagnosis
The nitroblue-tetrazolium (NBT) test is the original and most widely known test for chronic granulomatous disease.[16][17] It is negative in CGD, meaning that it does not turn blue. The higher the blue score, the better the cell is at producing reactive oxygen species. This test depends upon the direct reduction of NBT to the insoluble blue compound formazan by NADPH oxidase; NADPH is oxidized in the same reaction. This test is simple to perform and gives rapid results, but only tells whether or not there is a problem with the PHOX enzymes, not how much they are affected. A similar test uses dihydrorhodamine (DHR) where whole blood is stained with DHR, incubated, and stimulated to produce superoxide radicals which oxidize DHR to rhodamin in cells with normal function. An advanced test called the cytochrome C reduction assay tells physicians how much superoxide a patient's phagocytes can produce. Once the diagnosis of CGD is established, a genetic analysis may be used to determine exactly which mutation is the underlying cause.[citation needed]
Treatment
Management of chronic granulomatous disease revolves around two goals: 1) diagnose the disease early so that antibiotic prophylaxis can be given to keep an infection from occurring, and 2) educate the patient about his or her condition so that prompt treatment can be given if an infection occurs.[citation needed]
Antibiotics
Physicians often prescribe the antibiotic trimethoprim-sulfamethoxazole to prevent bacterial infections.[18] This drug also has the benefit of sparing the normal bacteria of the digestive tract. Fungal infection is commonly prevented with itraconazole,[19] although a newer drug of the same type called voriconazole may be more effective.[20] The use of this drug for this purpose is still under scientific investigation.
Immunomodulation
Interferon, in the form of interferon gamma-1b (Actimmune) is approved by the Food and Drug Administration for the prevention of infection in CGD. It has been shown to reduce infections in CGD patients by 70% and to decrease their severity. Although its exact mechanism is still not entirely understood, it has the ability to give CGD patients more immune function and therefore, greater ability to fight off infections. This therapy has been standard treatment for CGD for several years.[21]
Hematopoietic stem cell transplantation (HSCT)
Hematopoietic stem cell transplantation from a matched donor is curative although not without significant risk.[22][23]
Prognosis
There are currently no studies detailing the long term outcome of chronic granulomatous disease with modern treatment. Without treatment, children often die in the first decade of life. The increased severity of X-linked CGD results in a decreased survival rate of patients, as 20% of X-linked patients die of CGD-related causes by the age of 10, whereas 20% of autosomal recessive patients die by the age of 35.[24]
Recent experience from centers specializing in the care of patients with CGD suggests that the current mortality has fallen to under 3% and 1% respectively.[25]
CGD was initially termed "fatal granulomatous disease of childhood" because patients rarely survived past their first decade in the time before routine use of prophylactic antimicrobial agents. The average patient now survives at least 40 years.[26]
Epidemiology
CGD affects about 1 in 200,000 people in the United States, with about 20 new cases diagnosed each year.[4][5]
Chronic granulomatous disease affects all people of all races, however, there is limited information on prevalence outside of the United States. One survey in Sweden reported an incidence of 1 in 220,000 people,[27] while a larger review of studies in Europe suggested a lower rate: 1 in 250,000 people.[24]
History
This section needs expansion. You can help by adding to it. (May 2009) |
This condition was first described in 1954 by Janeway, who reported five cases of the disease in children.[28] In 1957 it was further characterized as "a fatal granulomatosus of childhood".[6][7] The underlying cellular mechanism that causes chronic granulomatous disease was discovered in 1967, and research since that time has further elucidated the molecular mechanisms underlying the disease.[8] Use of antibiotic prophylaxis, surgical abscess drainage, and vaccination led to the term "fatal" being dropped from the name of the disease as children survived into adulthood.
Research
Gene therapy is currently being studied as a possible treatment for chronic granulomatous disease. CGD is well-suited for gene therapy since it is caused by a mutation in single gene which only affects one body system (the hematopoietic system). Viruses have been used to deliver a normal gp91 gene to rats with a mutation in this gene, and subsequently the phagocytes in these rats were able to produce oxygen radicals.[29]
In 2006, two human patients with X-linked chronic granulomatous disease underwent gene therapy and blood cell precursor stem cell transplantation to their bone marrow. Both patients recovered from their CGD, clearing pre-existing infections and demonstrating increased oxidase activity in their neutrophils. However, long-term complications and efficacy of this therapy were unknown.[30]
In 2012, a 16 year old boy with CGD was treated at the Great Ormond Street Hospital, London with an experimental gene therapy which temporarily reversed the CGD and allowed him to overcome a life-threatening lung disease.[31]
References
- ^ Rapini, Ronald P.; Bolognia, Jean L.; Jorizzo, Joseph L. (2007). Dermatology: 2-Volume Set. St. Louis: Mosby. ISBN 1-4160-2999-0.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ^ "Chronic Granulomatous Disease: Immunodeficiency Disorders: Merck Manual Professional". Retrieved 2008-03-01.
- ^ a b Heyworth P, Cross A, Curnutte J (2003). "Chronic granulomatous disease". Curr Opin Immunol. 15 (5): 578–84. doi:10.1016/S0952-7915(03)00109-2. PMID 14499268.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Pao M, Wiggs EA, Anastacio MM; et al. (2004). "Cognitive function in patients with chronic granulomatous disease: a preliminary report". Psychosomatics. 45 (3): 230–4. doi:10.1176/appi.psy.45.3.230. PMID 15123849.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b James, William D.; Berger, Timothy G.; et al. (2006). Andrews' Diseases of the Skin: clinical Dermatology. Saunders Elsevier. ISBN 0-7216-2921-0.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ^ a b Berendes H, Bridges RA, Good RA (1957). "A fatal granulomatosus of childhood: the clinical study of a new syndrome". Minn Med. 40 (5): 309–12. PMID 13430573.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Bridges RA, Berendes H, Good RA (1959). "A fatal granulomatous disease of childhood; the clinical, pathological, and laboratory features of a new syndrome". AMA J Dis Child. 97 (4): 387–408. doi:10.1001/archpedi.1959.02070010389004. PMID 13636694.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Baehner RL, Nathan DG (1967). "Leukocyte oxidase: defective activity in chronic granulomatous disease". Science. 155 (3764): 835–6. doi:10.1126/science.155.3764.835. PMID 6018195.
- ^ Online Mendelian Inheritance in Man (OMIM): Granulomatous disease, Chronic, X-linked; CGD - 306400
- ^ a b Winkelstein J, Marino M, Johnston R, Boyle J, Curnutte J, Gallin J, Malech H, Holland S, Ochs H, Quie P, Buckley R, Foster C, Chanock S, Dickler H (2000). "Chronic granulomatous disease. Report on a national registry of 368 patients". Medicine (Baltimore). 79 (3): 155–69. doi:10.1097/00005792-200005000-00003. PMID 10844935.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Soler-Palacín P, Margareto C, Llobet P; et al. (2007). "Chronic granulomatous disease in pediatric patients: 25 years of experience". Allergol Immunopathol (Madr). 35 (3): 83–9. doi:10.1157/13106774. PMID 17594870. Retrieved 2009-04-08.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Lacy DE, Spencer DA, Goldstein A, Weller PH, Darbyshire P (November 1993). "Chronic granulomatous disease presenting in childhood with Pseudomonas cepacia septicaemia". J. Infect. 27 (3): 301–4. doi:10.1016/0163-4453(93)92271-W. PMID 7508484. Retrieved 2009-04-08.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Dorman SE, Guide SV, Conville PS; et al. (August 2002). "Nocardia infection in chronic granulomatous disease". Clin. Infect. Dis. 35 (4): 390–4. doi:10.1086/341416. PMID 12145721.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Heyworth P, Curnutte J, Rae J, Noack D, Roos D, van Koppen E, Cross A (2001). "Hematologically important mutations: X-linked chronic granulomatous disease (second update)". Blood Cells Mol Dis. 27 (1): 16–26. doi:10.1006/bcmd.2000.0347. PMID 11162142.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Cross A, Noack D, Rae J, Curnutte J, Heyworth P (2000). "Hematologically important mutations: the autosomal recessive forms of chronic granulomatous disease (first update)". Blood Cells Mol Dis. 26 (5): 561–5. doi:10.1006/bcmd.2000.0333. PMID 11112388.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Kasper, DL, Fauci, AS, Longo, DL, Braunwald, E, Hauser, SL, and Jameson, JL. Harrison's Principles of Internal Medicine, 16th edition 2005;357. ISBN 0-07-139140-1.
- ^ Baehner RL, Nathan DG (May 1968). "Quantitative nitroblue tetrazolium test in chronic granulomatous disease". N. Engl. J. Med. 278 (18): 971–6. doi:10.1056/NEJM196805022781801. PMID 4384563.
- ^ Weening R, Kabel P, Pijman P, Roos D (1983). "Continuous therapy with sulfamethoxazole-trimethoprim in patients with chronic granulomatous disease". J Pediatr. 103 (1): 127–30. doi:10.1016/S0022-3476(83)80798-7. PMID 6408232.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Cale C, Jones A, Goldblatt D (2000). "Follow up of patients with chronic granulomatous disease diagnosed since 1990". Clin Exp Immunol. 120 (2): 351–5. doi:10.1046/j.1365-2249.2000.01234.x. PMC 1905649. PMID 10792387.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Sabo J, Abdel-Rahman S (2000). "Voriconazole: a new triazole antifungal". Ann Pharmacother. 34 (9): 1032–43. doi:10.1345/aph.19237. PMID 10981251.
- ^ "A controlled trial of interferon gamma to prevent infection in chronic granulomatous disease. The International Chronic Granulomatous Disease Cooperative Study Group". N Engl J Med. 324 (8): 509–16. 1991. doi:10.1056/NEJM199102213240801. PMID 1846940.
- ^ Jones LB, McGrogan P, Flood TJ; et al. (May 2008). "Special article: chronic granulomatous disease in the United Kingdom and Ireland: a comprehensive national patient-based registry". Clin. Exp. Immunol. 152 (2): 211–8. doi:10.1111/j.1365-2249.2008.03644.x. PMC 2384093. PMID 18410635.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Soncini E, Slatter MA, Jones LB; et al. (April 2009). "Unrelated donor and HLA-identical sibling haematopoietic stem cell transplantation cure chronic granulomatous disease with good long-term outcome and growth". Br. J. Haematol. 145 (1): 73–83. doi:10.1111/j.1365-2141.2009.07614.x. PMID 19222467.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b van den Berg MJ, Van Koppen E, Ahlin A; et al. (2009). Alspaugh, Andy (ed.). "Chronic Granulomatous Disease: The European Experience". PLoS ONE. 4 (4): e5234. doi:10.1371/journal.pone.0005234. PMC 2668749. PMID 19381301.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - ^ Modern Management of Chronic Granulomatous Disease by Reinhard Segar, Division of Immunology/Hematology, University Children’s Hospital of Zurich, Zurich, Switzerland
- ^ http://www.uptodate.com/contents/chronic-granulomatous-disease-treatment-and-prognosis
- ^ Pediatric Chronic Granulomatous Disease at eMedicine
- ^ Assari T (2006). "Chronic Granulomatous Disease; fundamental stages in our understanding of CGD". Med Immunol. 5: 4. doi:10.1186/1476-9433-5-4. PMC 1592097. PMID 16989665.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Dinauer M, Gifford M, Pech N, Li L, Emshwiller P (2001). "Variable correction of host defense following gene transfer and bone marrow transplantation in murine X-linked chronic granulomatous disease". Blood. 97 (12): 3738–45. doi:10.1182/blood.V97.12.3738. PMID 11389011.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Ott M, Schmidt M, Schwarzwaelder K; et al. (2006). "Correction of X-linked chronic granulomatous disease by gene therapy, augmented by insertional activation of MDS1-EVI1, PRDM16 or SETBP1". Nat Med. 12 (4): 401–9. doi:10.1038/nm1393. PMID 16582916.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Sample, Iian (29 February 2012). "Gene therapy cures life-threatening lung infection in teenage boy". The Guardian. Retrieved 6 November 2015.
