Dapagliflozin: Difference between revisions
No edit summary |
|||
| Line 152: | Line 152: | ||
==Mechanism of action== |
==Mechanism of action== |
||
Dapagliflozin inhibits subtype 2 of the [[sodium-glucose transport proteins]] ([[SGLT2]]) which are responsible for at least 90% of the glucose [[reabsorption]] in the kidney. Blocking this transporter mechanism causes blood glucose to be eliminated through the urine.<ref>{{cite web|url=http://www.prous.com/molecules/default.asp?ID=165|archive-url=https://web.archive.org/web/20071105072914/http://www.prous.com/molecules/default.asp?ID=165|url-status=dead|archive-date=2007-11-05|title=Life Sciences - Clarivate|website=Clarivate}}</ref> In combination with metformin, dapagliflozin at standard treatment dose of 10mg daily lowered HbA1c by 0.54-0.84 percentage points when compared to metformin monotherapy in patients with inadequately controlled type 2 diabetes and normal renal function.<ref>Bailey |
Dapagliflozin inhibits subtype 2 of the [[sodium-glucose transport proteins]] ([[SGLT2]]) which are responsible for at least 90% of the glucose [[reabsorption]] in the kidney. Blocking this transporter mechanism causes blood glucose to be eliminated through the urine.<ref>{{cite web|url=http://www.prous.com/molecules/default.asp?ID=165|archive-url=https://web.archive.org/web/20071105072914/http://www.prous.com/molecules/default.asp?ID=165|url-status=dead|archive-date=2007-11-05|title=Life Sciences - Clarivate|website=Clarivate}}</ref> In combination with metformin, dapagliflozin at standard treatment dose of 10mg daily lowered HbA1c by 0.54-0.84 percentage points when compared to metformin monotherapy in patients with inadequately controlled type 2 diabetes and normal renal function.<ref>{{cite journal |last1=Bailey |first1=Clifford J |last2=Gross |first2=Jorge L |last3=Pieters |first3=Anne |last4=Bastien |first4=Arnaud |last5=List |first5=James F |title=Effect of dapagliflozin in patients with type 2 diabetes who have inadequate glycaemic control with metformin: a randomised, double-blind, placebo-controlled trial |journal=The Lancet |date=June 2010 |volume=375 |issue=9733 |pages=2223–2233 |doi=10.1016/S0140-6736(10)60407-2 }}</ref><ref>{{cite journal |last1=Bailey |first1=Clifford J |last2=Gross |first2=Jorge L |last3=Hennicken |first3=Delphine |last4=Iqbal |first4=Nayyar |last5=Mansfield |first5=Traci A |last6=List |first6=James F |title=Dapagliflozin add-on to metformin in type 2 diabetes inadequately controlled with metformin: a randomized, double-blind, placebo-controlled 102-week trial |journal=BMC Medicine |date=December 2013 |volume=11 |issue=1 |pages=43 |doi=10.1186/1741-7015-11-43 |pmid=23425012 }}</ref><ref>{{cite journal |last1=Henry |first1=R. R. |last2=Murray |first2=A. V. |last3=Marmolejo |first3=M. H. |last4=Hennicken |first4=D. |last5=Ptaszynska |first5=A. |last6=List |first6=J. F. |title=Dapagliflozin, metformin XR, or both: initial pharmacotherapy for type 2 diabetes, a randomised controlled trial: T2DM: dapagliflozin, metformin XR, or both |journal=International Journal of Clinical Practice |date=May 2012 |volume=66 |issue=5 |pages=446–456 |doi=10.1111/j.1742-1241.2012.02911.x |pmid=22413962 }}</ref> |
||
</ref> |
|||
Regarding its protective effects in heart failure, this is attributed primarily to haemodynamic effects, where SGLT2 inhibitors potently reduce intravascular volume through osmotic diuresis and natriuresis. This consequently may lead to a reduction in preload and afterload, thereby alleviating cardiac workload and improving left ventricular function.<ref>{{cite journal |vauthors=Lan NS, Fegan PG, Yeap BB, Dwivedi G |title=The effects of sodium-glucose cotransporter 2 inhibitors on left ventricular function: current evidence and future directions |journal=ESC Heart Fail |volume=6 |issue=5 |pages=927–935 |date=October 2019 |pmid=31400090 |pmc=6816235 |doi=10.1002/ehf2.12505 }}</ref> |
Regarding its protective effects in heart failure, this is attributed primarily to haemodynamic effects, where SGLT2 inhibitors potently reduce intravascular volume through osmotic diuresis and natriuresis. This consequently may lead to a reduction in preload and afterload, thereby alleviating cardiac workload and improving left ventricular function.<ref>{{cite journal |vauthors=Lan NS, Fegan PG, Yeap BB, Dwivedi G |title=The effects of sodium-glucose cotransporter 2 inhibitors on left ventricular function: current evidence and future directions |journal=ESC Heart Fail |volume=6 |issue=5 |pages=927–935 |date=October 2019 |pmid=31400090 |pmc=6816235 |doi=10.1002/ehf2.12505 }}</ref> |
||
| Line 189: | Line 188: | ||
In 2020, the U.S. [[Food and Drug Administration]] (FDA) expanded the indications for dapagliflozin to include treatment for adults with heart failure with reduced ejection fraction to reduce the risk of cardiovascular death and hospitalization for heart failure.<ref name="FDA PR 20200505" /> It is the first in this particular drug class, sodium-glucose co-transporter 2 inhibitors, to be approved to treat adults with New York Heart Association's functional class II-IV heart failure with reduced ejection fraction.<ref name="FDA PR 20200505" /> |
In 2020, the U.S. [[Food and Drug Administration]] (FDA) expanded the indications for dapagliflozin to include treatment for adults with heart failure with reduced ejection fraction to reduce the risk of cardiovascular death and hospitalization for heart failure.<ref name="FDA PR 20200505" /> It is the first in this particular drug class, sodium-glucose co-transporter 2 inhibitors, to be approved to treat adults with New York Heart Association's functional class II-IV heart failure with reduced ejection fraction.<ref name="FDA PR 20200505" /> |
||
The results of the DAPA-HF and DECLARE-TIMI 58 clinical trials demonstrated the efficacy of dapagliflozin compared to placebo in improving survival in adults with heart failure with reduced ejection fraction by 17%. They both showed a reduction in the number of hospitalisations from worsening heart failure, cardiovascular death and all-cause mortality.<ref>McMurray |
The results of the DAPA-HF and DECLARE-TIMI 58 clinical trials demonstrated the efficacy of dapagliflozin compared to placebo in improving survival in adults with heart failure with reduced ejection fraction by 17%. They both showed a reduction in the number of hospitalisations from worsening heart failure, cardiovascular death and all-cause mortality.<ref>{{cite journal |last1=McMurray |first1=John J.V. |last2=Solomon |first2=Scott D. |last3=Inzucchi |first3=Silvio E. |last4=Køber |first4=Lars |last5=Kosiborod |first5=Mikhail N. |last6=Martinez |first6=Felipe A. |last7=Ponikowski |first7=Piotr |last8=Sabatine |first8=Marc S. |last9=Anand |first9=Inder S. |last10=Bělohlávek |first10=Jan |last11=Böhm |first11=Michael |last12=Chiang |first12=Chern-En |last13=Chopra |first13=Vijay K. |last14=de Boer |first14=Rudolf A. |last15=Desai |first15=Akshay S. |last16=Diez |first16=Mirta |last17=Drozdz |first17=Jaroslaw |last18=Dukát |first18=Andrej |last19=Ge |first19=Junbo |last20=Howlett |first20=Jonathan G. |last21=Katova |first21=Tzvetana |last22=Kitakaze |first22=Masafumi |last23=Ljungman |first23=Charlotta E.A. |last24=Merkely |first24=Béla |last25=Nicolau |first25=Jose C. |last26=O’Meara |first26=Eileen |last27=Petrie |first27=Mark C. |last28=Vinh |first28=Pham N. |last29=Schou |first29=Morten |last30=Tereshchenko |first30=Sergey |last31=Verma |first31=Subodh |last32=Held |first32=Claes |last33=DeMets |first33=David L. |last34=Docherty |first34=Kieran F. |last35=Jhund |first35=Pardeep S. |last36=Bengtsson |first36=Olof |last37=Sjöstrand |first37=Mikaela |last38=Langkilde |first38=Anna-Maria |title=Dapagliflozin in Patients with Heart Failure and Reduced Ejection Fraction |journal=New England Journal of Medicine |date=21 November 2019 |volume=381 |issue=21 |pages=1995–2008 |doi=10.1056/NEJMoa1911303 }}</ref><ref>{{cite journal |last1=Kato |first1=Eri T. |last2=Silverman |first2=Michael G. |last3=Mosenzon |first3=Ofri |last4=Zelniker |first4=Thomas A. |last5=Cahn |first5=Avivit |last6=Furtado |first6=Remo H.M. |last7=Kuder |first7=Julia |last8=Murphy |first8=Sabina A. |last9=Bhatt |first9=Deepak L. |last10=Leiter |first10=Lawrence A. |last11=McGuire |first11=Darren K. |last12=Wilding |first12=John P.H. |last13=Bonaca |first13=Marc P. |last14=Ruff |first14=Christian T. |last15=Desai |first15=Akshay S. |last16=Goto |first16=Shinya |last17=Johansson |first17=Peter A. |last18=Gause-Nilsson |first18=Ingrid |last19=Johanson |first19=Per |last20=Langkilde |first20=Anna Maria |last21=Raz |first21=Itamar |last22=Sabatine |first22=Marc S. |last23=Wiviott |first23=Stephen D. |title=Effect of Dapagliflozin on Heart Failure and Mortality in Type 2 Diabetes Mellitus |journal=Circulation |date=28 May 2019 |volume=139 |issue=22 |pages=2528–2536 |doi=10.1161/CIRCULATIONAHA.119.040130 }}</ref> |
||
The safety and effectiveness of dapagliflozin were evaluated in a randomized, double-blind, placebo-controlled study of 4,744 participants.<ref name="FDA PR 20200505" /> The average age of participants was 66 years and more participants were male (77%) than female.<ref name="FDA PR 20200505" /> To determine the drug's effectiveness, investigators examined the occurrence of cardiovascular death, hospitalization for heart failure, and urgent heart failure visits.<ref name="FDA PR 20200505" /> Participants were randomly assigned to receive a once-daily dose of either 10 milligrams of dapagliflozin or a placebo (inactive treatment).<ref name="FDA PR 20200505" /> After about 18 months, people who received dapagliflozin had fewer cardiovascular deaths, hospitalizations for heart failure, and urgent heart failure visits than those receiving the placebo.<ref name="FDA PR 20200505" /> |
The safety and effectiveness of dapagliflozin were evaluated in a randomized, double-blind, placebo-controlled study of 4,744 participants.<ref name="FDA PR 20200505" /> The average age of participants was 66 years and more participants were male (77%) than female.<ref name="FDA PR 20200505" /> To determine the drug's effectiveness, investigators examined the occurrence of cardiovascular death, hospitalization for heart failure, and urgent heart failure visits.<ref name="FDA PR 20200505" /> Participants were randomly assigned to receive a once-daily dose of either 10 milligrams of dapagliflozin or a placebo (inactive treatment).<ref name="FDA PR 20200505" /> After about 18 months, people who received dapagliflozin had fewer cardiovascular deaths, hospitalizations for heart failure, and urgent heart failure visits than those receiving the placebo.<ref name="FDA PR 20200505" /> |
||
Revision as of 14:50, 15 June 2022
 | |||
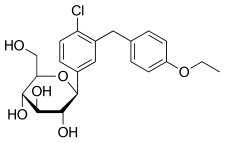 Haworth projection (bottom) | |||
| |||
| Clinical data | |||
|---|---|---|---|
| Pronunciation | /ˌdæpəɡlɪˈfloʊzɪn/ DAP-ə-glif-LOH-zin | ||
| Trade names | Forxiga, Farxiga, Edistride, others | ||
| Other names | BMS-512148; (1S)-1,5-anhydro-1-C-{4-chloro-3-[(4-ethoxyphenyl)methyl]phenyl}-D-glucitol | ||
| AHFS/Drugs.com | Monograph | ||
| License data |
| ||
| Pregnancy category |
| ||
| Routes of administration | By mouth (tablets) | ||
| Drug class | Sodium-glucose co-transporter 2 (SGLT2) inhibitor | ||
| ATC code | |||
| Legal status | |||
| Legal status | |||
| Pharmacokinetic data | |||
| Bioavailability | 78% (after 10 mg dose) | ||
| Protein binding | ~91% | ||
| Metabolism | UGT1A9 (major), CYP (minor) | ||
| Metabolites | Dapagliflozin 3-O-glucuronide (inactive) | ||
| Elimination half-life | ~12.9 hours | ||
| Excretion | Urine (75%), feces (21%)[2] | ||
| Identifiers | |||
| |||
| CAS Number | |||
| PubChem CID | |||
| IUPHAR/BPS | |||
| DrugBank | |||
| ChemSpider | |||
| UNII | |||
| KEGG | |||
| ChEBI | |||
| ChEMBL | |||
| CompTox Dashboard (EPA) | |||
| ECHA InfoCard | 100.167.331 | ||
| Chemical and physical data | |||
| Formula | C21H25ClO6 | ||
| Molar mass | 408.88 g·mol−1 | ||
| 3D model (JSmol) | |||
| |||
| |||
| | |||
Dapagliflozin, sold under the brand names Farxiga (US) and Forxiga (EU) among others, is a medication used to treat type 2 diabetes.[2][3][4] It is also used to treat adults with certain kinds of heart failure and chronic kidney disease.[5][6][3]
Common side effects include hypoglycaemia (low blood sugar), urinary tract infections, genital infections, and volume depletion (reduced amount of water in the body).[7] Diabetic ketoacidosis is a common side effect in type 1 diabetic patients.[8] Serious but rare side effects include Fournier gangrene.[9] Dapagliflozin is a sodium-glucose co-transporter-2 (SGLT-2) inhibitor and works by removing sugar from the body with the urine.[10]
It was developed by Bristol-Myers Squibb in partnership with AstraZeneca. It is on the World Health Organization's List of Essential Medicines.[11] In 2019, it was the 310th most commonly prescribed medication in the United States, with more than 1 million prescriptions.[12]
Medical uses
Dapagliflozin is used along with diet, exercise and usually with other glucose lowering medications, to improve glycaemic control in adults with type 2 diabetes and to reduce the risk of hospitalisation for heart failure among adults with type 2 diabetes and known cardiovascular disease or other cardiovascular risk factors (including high blood pressure, high cholesterol and smokers). Dapagliflozin was also shown to reduce the rate of decline in kidney function and kidney failure in adults with type 2 diabetes, a finding that has recently been confirmed in both diabetic and non-diabetic populations. Dapagliflozin is also an important treatment option in patients with comorbid type 2 diabetes and heart failure with a reduced ejection fraction (on top of standard medical and/or device therapy), and lowers the risk of hospitalisation for heart failure and cardiovascular deaths in this group (as well as non-diabetic patients with HFrEF).[13][14][15] All SGLT-2 inhibitors are useful to reduce the risk of hospitalisation for heart failure in people with atherosclerotic cardiovascular disease, however a small number of meta-analyses and cohort studies have shown that dapagliflozin is superior to others such as empagliflozin.[16][17][18][verification needed]
In addition, dapagliflozin is indicated for the treatment of adults with heart failure with reduced ejection fraction to reduce the risk of cardiovascular death and hospitalization for heart failure.[5][6][3] It is also indicated to reduce the risk of kidney function decline, kidney failure, cardiovascular death and hospitalization for heart failure in adults with chronic kidney disease who are at risk of disease progression.[19]
In the European Union it is indicated in adults:
- for the treatment of insufficiently controlled type 2 diabetes mellitus as an adjunct to diet and exercise:[3][20][21][22]
- for the treatment of heart failure with reduced ejection fraction.[3]
In November 2021, the European Medicines Agency (EMA) stated that dapagliflozin should no longer be used to treat type 1 diabetes.[4]
Adverse effects
Since dapagliflozin leads to heavy glycosuria (sometimes up to about 70 grams per day) it can lead to rapid weight loss and tiredness. The glucose acts as an osmotic diuretic (this effect is the cause of polyuria in diabetes) which can lead to dehydration. The increased amount of glucose in the urine can also worsen the infections already associated with diabetes, particularly urinary tract infections and thrush (candidiasis). Rarely, use of an SGLT2 drug, including dapagliflozin, is associated with necrotizing fasciitis of the perineum, also called Fournier gangrene.[26]
Dapagliflozin is also associated with hypotensive reactions. There are concerns it may increase the risk of diabetic ketoacidosis.[27]
Dapagliflozin can cause dehydration, serious urinary tract infections and genital yeast infections.[5] Elderly people, people with kidney problems, those with low blood pressure, and people on diuretics should be assessed for their volume status and kidney function.[5] People with signs and symptoms of metabolic acidosis or ketoacidosis (acid buildup in the blood) should also be assessed.[5] Dapagliflozin can cause serious cases of necrotizing fasciitis of the perineum (Fournier gangrene) in people with diabetes and low blood sugar when combined with insulin.[5]
To lessen the risk of developing ketoacidosis (a serious condition in which the body produces high levels of blood acids called ketones) after surgery, the FDA has approved changes to the prescribing information for SGLT2 inhibitor diabetes medicines to recommend they be stopped temporarily before scheduled surgery. Canagliflozin, dapagliflozin, and empagliflozin should each be stopped at least three days before, and ertugliflozin should be stopped at least four days before scheduled surgery.[28]
Symptoms of ketoacidosis include nausea, vomiting, abdominal pain, tiredness, and trouble breathing.[28]
The glucose lowering effect of dapagliflozin diminishes in CKD patients with an eGFR <45mL/min and is therefore not recommended for use to lower glucose levels in patients with diabetes. However, recent evidence found improved safety and efficacy data in the reduction of renal failure risks in CKD patients with or without diabetes using dapagliflozin.[29][30][31]
Mechanism of action
Dapagliflozin inhibits subtype 2 of the sodium-glucose transport proteins (SGLT2) which are responsible for at least 90% of the glucose reabsorption in the kidney. Blocking this transporter mechanism causes blood glucose to be eliminated through the urine.[32] In combination with metformin, dapagliflozin at standard treatment dose of 10mg daily lowered HbA1c by 0.54-0.84 percentage points when compared to metformin monotherapy in patients with inadequately controlled type 2 diabetes and normal renal function.[33][34][35]
Regarding its protective effects in heart failure, this is attributed primarily to haemodynamic effects, where SGLT2 inhibitors potently reduce intravascular volume through osmotic diuresis and natriuresis. This consequently may lead to a reduction in preload and afterload, thereby alleviating cardiac workload and improving left ventricular function.[36]
Selectivity
The IC50 for SGLT2 is less than one thousandth of the IC50 for SGLT1 (1.1 versus 1390 nmol/L), so that the drug does not interfere with intestinal glucose absorption.[37]
Names
Dapagliflozin is the International nonproprietary name (INN),[38] and the United States Adopted Name (USAN).[39]
There is a fixed-dose combination product dapagliflozin/metformin extended-release, called Xigduo XR.[40][41][42]
In July 2016, the fixed-dose combination of saxagliptin and dapagliflozin was approved for medical use in the European Union and is sold under the brand name Qtern.[43] The combination drug was approved for medical use in the United States in February 2017, where it is sold under the brand name Qtern.[44][45]
In May 2019, the fixed-dose combination of dapagliflozin, saxagliptin, and metformin hydrochloride as extended-release tablets was approved in the United States to improve glycemic control in adults with type 2 diabetes when used in combination with diet and exercise. The FDA granted the approval of Qternmet XR to AstraZeneca.[46] The combination drug was approved for use in the European Union in November 2019, and is sold under the brand name Qtrilmet.[47]
History
In 2012, the Committee for Medicinal Products for Human Use (CHMP) of the European Medicines Agency (EMA) issued a positive opinion on the drug.[3]
Dapagliflozin was found effective in several studies in participants with type 2.[3] The main measure of effectiveness was the level of glycated haemoglobin (HbA1c), which gives an indication of how well blood glucose is controlled.[3]
In two studies involving 840 participants with type 2 diabetes, dapagliflozin when used alone decreased HbA1c levels by 0.66 percentage points more than placebo (a dummy treatment) after 24 weeks.[3] In four other studies involving 2,370 participants, adding dapagliflozin to other diabetes medicines decreased HbA1c levels by 0.54–0.68 percentage points more than adding placebo after 24 weeks.[3]
In a study involving 814 participants with type 2 diabetes, dapagliflozin used in combination with metformin was at least as effective as a sulphonylurea (another type of diabetes medicines) used with metformin.[3] Both combinations reduced HbA1c levels by 0.52 percentage points after 52 weeks.[3]
A long-term study, involving over 17,000 participants with type 2 diabetes, looked at the effects of dapagliflozin on cardiovascular (heart and circulation) disease.[3] The study indicated that dapagliflozin's effects were in line with those of other diabetes medicines that also work by blocking SGLT2.[3]
In two studies involving 1,648 participants with type 1 diabetes whose blood sugar was not controlled well enough on insulin alone, adding dapagliflozin 5 mg decreased HbA1c levels after 24 hours by 0.37% and by 0.42% more than adding placebo.[3]
Dapagliflozin was approved for medical use in the European Union in November 2012.[3] It is marketed in a number of European countries.[48]
Dapagliflozin was approved for medical use in the United States in January 2014.[49][19]
In 2020, the U.S. Food and Drug Administration (FDA) expanded the indications for dapagliflozin to include treatment for adults with heart failure with reduced ejection fraction to reduce the risk of cardiovascular death and hospitalization for heart failure.[5] It is the first in this particular drug class, sodium-glucose co-transporter 2 inhibitors, to be approved to treat adults with New York Heart Association's functional class II-IV heart failure with reduced ejection fraction.[5]
The results of the DAPA-HF and DECLARE-TIMI 58 clinical trials demonstrated the efficacy of dapagliflozin compared to placebo in improving survival in adults with heart failure with reduced ejection fraction by 17%. They both showed a reduction in the number of hospitalisations from worsening heart failure, cardiovascular death and all-cause mortality.[50][51]
The safety and effectiveness of dapagliflozin were evaluated in a randomized, double-blind, placebo-controlled study of 4,744 participants.[5] The average age of participants was 66 years and more participants were male (77%) than female.[5] To determine the drug's effectiveness, investigators examined the occurrence of cardiovascular death, hospitalization for heart failure, and urgent heart failure visits.[5] Participants were randomly assigned to receive a once-daily dose of either 10 milligrams of dapagliflozin or a placebo (inactive treatment).[5] After about 18 months, people who received dapagliflozin had fewer cardiovascular deaths, hospitalizations for heart failure, and urgent heart failure visits than those receiving the placebo.[5]
In July 2020, the FDA granted AstraZeneca a Fast Track Designation in the US for the development of dapagliflozin to reduce the risk of hospitalisation for heart failure or cardiovascular death in adults following a heart attack.[52]
In August 2020, it was reported that detailed results from the Phase III DAPA-CKD trial showed that dapagliflozin on top of standard of care reduced the composite measure of worsening of renal function or risk of cardiovascular or renal death by 39% compared to placebo (p<0.0001) in patients with chronic kidney disease stages 2–4 and elevated urinary albumin excretion. The results were consistent in patients both with and without type 2 diabetes.[53]
In April 2021, the FDA expanded the indications for dapagliflozin to include reducing the risk of kidney function decline, kidney failure, cardiovascular death and hospitalization for heart failure in adults with chronic kidney disease who are at risk of disease progression.[19] The efficacy of dapagliflozin to improve kidney outcomes and reduce cardiovascular death in people with chronic kidney disease was evaluated in a multicenter, double-blind study of 4,304 participants.[19]
Society and culture
Legal status
A generic version of dapagliflozin was approved by the US Food and Drug Administration (FDA) in February 2022,[54] but can't be sold until October 2025.[55][56]
Research
This section needs expansion with: Summary of meta-analyses and reviews of dapagliflozin research. You can help by adding to it. (May 2022) |
A study found that in heart failure with a reduced ejection fraction, dapagliflozin reduced the risk of worsening of heart failure or progression to death from cardiovascular causes, irrespective of diabetic status.[57]
A systematic review concluded that dapagliflozin reduced heart failure hospitalization, cardiovascular death, and all-cause mortality in patients with HFrEF and diabetes. [58]
References
- ^ "Dapagliflozin (Farxiga) Use During Pregnancy". Drugs.com. 30 August 2018. Archived from the original on 17 April 2021. Retrieved 5 May 2020.
- ^ a b c "Farxiga- dapagliflozin tablet, film coated". DailyMed. 3 February 2020. Archived from the original on 30 October 2020. Retrieved 5 May 2020.
- ^ a b c d e f g h i j k l m n o p q r s "Forxiga EPAR". European Medicines Agency (EMA). Archived from the original on 17 February 2020. Retrieved 17 February 2020. Text was copied from this source which is © European Medicines Agency. Reproduction is authorized provided the source is acknowledged.
- ^ a b "Forxiga (dapagliflozin) 5mg should no longer be used for the treatment of Type 1 Diabetes Mellitus". European Medicines Agency (EMA). 11 November 2021. Archived from the original on 11 November 2021. Retrieved 11 November 2021.
- ^ a b c d e f g h i j k l m "FDA approves new treatment for a type of heart failure". U.S. Food and Drug Administration (FDA) (Press release). 5 May 2020. Archived from the original on 6 May 2020. Retrieved 5 May 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ a b National Institute for Health and Care Excellence (24 February 2021). "Dapagliflozin for treating chronic heart failure with reduced ejection fraction". NICE Technology Appraisal Auidance [TA679]. NICE. Archived from the original on 9 May 2021. Retrieved 9 May 2021.
- ^ Ptaszynska, Agata; Johnsson, Kristina M.; Parikh, Shamik J.; De Bruin, Tjerk W. A.; Apanovitch, Anne Marie; List, James F. (2014). "Safety Profile of Dapagliflozin for Type 2 Diabetes: Pooled Analysis of Clinical Studies for Overall Safety and Rare Events". Drug Safety. 37 (10): 815–829. doi:10.1007/s40264-014-0213-4. PMID 25096959. S2CID 24064402.
- ^ Dandona, Paresh; Mathieu, Chantal; Phillip, Moshe; Hansen, Lars; Tschöpe, Diethelm; Thorén, Fredrik; Xu, John; Langkilde, Anna Maria; DEPICT-1 Investigators (2018). "Efficacy and Safety of Dapagliflozin in Patients with Inadequately Controlled Type 1 Diabetes: The DEPICT-1 52-Week Study". Diabetes Care. 41 (12): 2552–2559. doi:10.2337/dc18-1087. PMID 30352894. S2CID 53027785.
{{cite journal}}: CS1 maint: numeric names: authors list (link) - ^ Hu, Yang; Bai, Ziyu; Tang, Yan; Liu, Rongji; Zhao, Bin; Gong, Jian; Mei, Dan (2020). "Fournier Gangrene Associated with Sodium-Glucose Cotransporter-2 Inhibitors: A Pharmacovigilance Study with Data from the U.S. FDA Adverse Event Reporting System". Journal of Diabetes Research. 2020: 1–8. doi:10.1155/2020/3695101. PMC 7368210. PMID 32695827.
- ^ FARXIGA- dapagliflozin tablet, film coated. Archived 30 October 2020 at the Wayback Machine DailyMed. Retrieved 6 May 2021.
- ^ World Health Organization (2021). World Health Organization model list of essential medicines: 22nd list (2021). Geneva: World Health Organization. hdl:10665/345533. WHO/MHP/HPS/EML/2021.02.
- ^ "Dapagliflozin - Drug Usage Statistics". ClinCalc. Archived from the original on 13 April 2020. Retrieved 16 October 2021.
- ^ McMurray JJ, Solomon SD, Inzucchi SE, Køber L, Kosiborod MN, Martinez FA, Ponikowski P, Sabatine MS, Anand IS, Bělohlávek J, Böhm M. Dapagliflozin in patients with heart failure and reduced ejection fraction. New England Journal of Medicine. 2019 Nov 21;381(21):1995-2008.
- ^ Wiviott SD, Raz I, Bonaca MP, Mosenzon O, Kato ET, Cahn A, Silverman MG, Zelniker TA, Kuder JF, Murphy SA, Bhatt DL. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. New England Journal of Medicine. 2019 Jan 24;380(4):347-57.
- ^ Heerspink HJ, Stefánsson BV, Correa-Rotter R, Chertow GM, Greene T, Hou FF, Mann JF, McMurray JJ, Lindberg M, Rossing P, Sjöström CD. Dapagliflozin in patients with chronic kidney disease. New England Journal of Medicine. 2020 Oct 8;383(15):1436-46.
- ^ Shi Z, Gao F, Liu W, He X. Comparative Efficacy of Dapagliflozin and Empagliflozin of a Fixed Dose in Heart Failure: A Network Meta-Analysis. Frontiers in Cardiovascular Medicine. 2022;9.
- ^ McGuire DK, Shih WJ, Cosentino F, Charbonnel B, Cherney DZI, Dagogo-Jack S, et al. Association of SGLT2 Inhibitors With Cardiovascular and Kidney Outcomes in Patients With Type 2 Diabetes: A Meta-analysis. JAMA Cardiology. 2021;6(2):148-58
- ^ Zelniker TA, Wiviott SD, Raz I, et al. (January 2019). "SGLT2 inhibitors for primary and secondary prevention of cardiovascular and renal outcomes in type 2 diabetes: a systematic review and meta-analysis of cardiovascular outcome trials". Lancet. 393 (10166): 31–9. doi:10.1016/S0140-6736(18)32590-X. PMID 30424892. S2CID 53277899.
However, in patients with atherosclerotic cardiovascular disease, the effect of empagliflozin on cardiovascular death was more pro-nounced than that of canagliflozin or dapagliflozin
- ^ a b c d "FDA Approves Treatment for Chronic Kidney Disease". U.S. Food and Drug Administration (FDA) (Press release). 30 April 2021. Archived from the original on 30 April 2021. Retrieved 30 April 2021.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ Cefalu WT, Leiter LA, De Bruin TW., Gause-Nilsson I, Sugg J, Parikh SJ. Dapagliflozin's effects on glycemia and cardiovascular risk factors in high-risk patients with type 2 diabetes: A 24-week, multicenter, randomized, double-blind, placebo-controlled study with a 28-week extension. Diabetes care. 2015;38(7):1218–27. Available from: https://diabetesjournals.org/care/article/38/7/1218/30814/Dapagliflozin-s-Effects-on-Glycemia-and Archived 4 March 2022 at the Wayback Machine
- ^ Ferrannini E, Ramos SJ, Salsali A, Tang W, List JF. Dapagliflozin monotherapy in type 2 diabetic patients with inadequate glycemic control by diet and exercise: A randomized, double-blind, placebo-controlled, phase 3 trial. Diabetes care. 2010;33(10):2217–24. Available from: https://www.proquest.com/docview/759542603/fulltextPDF/376EB22F644E45FBPQ/1?accountid=14723 Archived 10 June 2022 at the Wayback Machine
- ^ Rossing P, Inzucchi SE, Vart P, Jongs N, Docherty KF, Jhund PS, et al. Dapagliflozin and new-onset type 2 diabetes in patients with chronic kidney disease or heart failure: pooled analysis of the DAPA-CKD and DAPA-HF trials. The Lancet Diabetes & endocrinology. 2022;10(1):24–34.
- ^ Cefalu WT, Leiter LA, De Bruin TW., Gause-Nilsson I, Sugg J, Parikh SJ. Dapagliflozin's effects on glycemia and cardiovascular risk factors in high-risk patients with type 2 diabetes: A 24-week, multicenter, randomized, double-blind, placebo-controlled study with a 28-week extension. Diabetes care. 2015;38(7):1218–27. Available from: https://diabetesjournals.org/care/article/38/7/1218/30814/Dapagliflozin-s-Effects-on-Glycemia-and Archived 4 March 2022 at the Wayback Machine
- ^ Ferrannini E, Ramos SJ, Salsali A, Tang W, List JF. Dapagliflozin monotherapy in type 2 diabetic patients with inadequate glycemic control by diet and exercise: A randomized, double-blind, placebo-controlled, phase 3 trial. Diabetes care. 2010;33(10):2217–24. Available from: https://www.proquest.com/docview/759542603/fulltextPDF/376EB22F644E45FBPQ/1?accountid=14723 Archived 10 June 2022 at the Wayback Machine
- ^ Rossing P, Inzucchi SE, Vart P, Jongs N, Docherty KF, Jhund PS, et al. Dapagliflozin and new-onset type 2 diabetes in patients with chronic kidney disease or heart failure: pooled analysis of the DAPA-CKD and DAPA-HF trials. The Lancet Diabetes & endocrinology. 2022;10(1):24–34.
- ^ "FDA warns about rare occurrences of a serious infection of the genital area with SGLT2 inhibitors for diabetes". U.S. Food and Drug Administration (FDA). 9 February 2019. Archived from the original on 13 December 2019. Retrieved 16 December 2019.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ "SGLT2 inhibitors: Drug Safety Communication - FDA Warns Medicines May Result in a Serious Condition of Too Much Acid in the Blood". U.S. Food and Drug Administration (FDA). 15 May 2015. Archived from the original on 27 October 2016. Retrieved 15 November 2016.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ a b "FDA revises labels of SGLT2 inhibitors for diabetes to include warning". U.S. Food and Drug Administration. 19 March 2020. Archived from the original on 7 June 2020. Retrieved 6 June 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ Heerspink HJ, Stefánsson BV, Correa-Rotter R, Chertow GM, Greene T, Hou FF, Mann JF, McMurray JJ, Lindberg M, Rossing P, Sjöström CD. Dapagliflozin in patients with chronic kidney disease. New England Journal of Medicine. 2020 Oct 8;383(15):1436-46.
- ^ Cefalu WT, Leiter LA, De Bruin TW., Gause-Nilsson I, Sugg J, Parikh SJ. Dapagliflozin's effects on glycemia and cardiovascular risk factors in high-risk patients with type 2 diabetes: A 24-week, multicenter, randomized, double-blind, placebo-controlled study with a 28-week extension. Diabetes care. 2015;38(7):1218–27. Available from: https://diabetesjournals.org/care/article/38/7/1218/30814/Dapagliflozin-s-Effects-on-Glycemia-and Archived 4 March 2022 at the Wayback Machine
- ^ Kohan DE, Fioretto P, Tang W, List JF. Long-term study of patients with type 2 diabetes and moderate renal impairment shows that dapagliflozin reduces weight and blood pressure but does not improve glycemic control. Kidney international. 2014 Apr 1;85(4):962-71.
- ^ "Life Sciences - Clarivate". Clarivate. Archived from the original on 5 November 2007.
- ^ Bailey, Clifford J; Gross, Jorge L; Pieters, Anne; Bastien, Arnaud; List, James F (June 2010). "Effect of dapagliflozin in patients with type 2 diabetes who have inadequate glycaemic control with metformin: a randomised, double-blind, placebo-controlled trial". The Lancet. 375 (9733): 2223–2233. doi:10.1016/S0140-6736(10)60407-2.
- ^ Bailey, Clifford J; Gross, Jorge L; Hennicken, Delphine; Iqbal, Nayyar; Mansfield, Traci A; List, James F (December 2013). "Dapagliflozin add-on to metformin in type 2 diabetes inadequately controlled with metformin: a randomized, double-blind, placebo-controlled 102-week trial". BMC Medicine. 11 (1): 43. doi:10.1186/1741-7015-11-43. PMID 23425012.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Henry, R. R.; Murray, A. V.; Marmolejo, M. H.; Hennicken, D.; Ptaszynska, A.; List, J. F. (May 2012). "Dapagliflozin, metformin XR, or both: initial pharmacotherapy for type 2 diabetes, a randomised controlled trial: T2DM: dapagliflozin, metformin XR, or both". International Journal of Clinical Practice. 66 (5): 446–456. doi:10.1111/j.1742-1241.2012.02911.x. PMID 22413962.
- ^ Lan NS, Fegan PG, Yeap BB, Dwivedi G (October 2019). "The effects of sodium-glucose cotransporter 2 inhibitors on left ventricular function: current evidence and future directions". ESC Heart Fail. 6 (5): 927–935. doi:10.1002/ehf2.12505. PMC 6816235. PMID 31400090.
- ^ Schubert-Zsilavecz, M, Wurglics, M, Neue Arzneimittel 2008/2009
- ^ "International Nonproprietary Names for Pharmaceutical Substances (INN). Recommended International Nonproprietary Names: List 59" (PDF). World Health Organization. 2008. p. 50. Archived (PDF) from the original on 18 May 2016. Retrieved 15 November 2016.
- ^ "Statement on a Nonproprietary Name Adopted by the USAN Council" (PDF). American Medical Association. Archived from the original (PDF) on 7 February 2012. Retrieved 15 November 2016.
- ^ "US FDA Approves Once-Daily Xigduo XR Tablets for Adults with Type 2 Diabetes". AstraZeneca. 30 October 2014. Archived from the original on 16 November 2016. Retrieved 15 November 2016.
- ^ "Drug Approval Package: Xigduo XR (dapagliflozin and metformin HCl) Extended-Release Tablets". U.S. Food and Drug Administration (FDA). 7 April 2015. Archived from the original on 20 February 2020. Retrieved 5 May 2020.
- ^ "Xigduo XR- dapagliflozin and metformin hydrochloride tablet, film coated, extended release". DailyMed. 3 February 2020. Archived from the original on 2 March 2021. Retrieved 5 May 2020.
- ^ "Qtern EPAR". European Medicines Agency (EMA). Archived from the original on 14 July 2020. Retrieved 7 May 2020.
- ^ "Drug Approval Package: Qtern (dapagliflozin and saxagliptin)". U.S. Food and Drug Administration (FDA). 10 October 2018. Archived from the original on 14 July 2020. Retrieved 8 May 2020.
- ^ "Qtern- dapagliflozin and saxagliptin tablet, film coated". DailyMed. 24 January 2020. Archived from the original on 14 July 2020. Retrieved 17 February 2020.
- ^ "Drug Approval Package: Qternmet XR". U.S. Food and Drug Administration (FDA). 27 January 2020. Archived from the original on 17 February 2020. Retrieved 17 February 2020.
- ^ "Qtrilmet EPAR". European Medicines Agency (EMA). Archived from the original on 29 December 2019. Retrieved 30 March 2020.
- ^ "Forxiga". Drugs.com. 4 May 2020. Archived from the original on 28 August 2021. Retrieved 5 May 2020.
- ^ "Drug Approval Package: Farxiga (dapagliflozin) Tablets NDA #202293". U.S. Food and Drug Administration (FDA). 24 December 1999. Archived from the original on 19 September 2020. Retrieved 5 May 2020.
- ^ McMurray, John J.V.; Solomon, Scott D.; Inzucchi, Silvio E.; Køber, Lars; Kosiborod, Mikhail N.; Martinez, Felipe A.; Ponikowski, Piotr; Sabatine, Marc S.; Anand, Inder S.; Bělohlávek, Jan; Böhm, Michael; Chiang, Chern-En; Chopra, Vijay K.; de Boer, Rudolf A.; Desai, Akshay S.; Diez, Mirta; Drozdz, Jaroslaw; Dukát, Andrej; Ge, Junbo; Howlett, Jonathan G.; Katova, Tzvetana; Kitakaze, Masafumi; Ljungman, Charlotta E.A.; Merkely, Béla; Nicolau, Jose C.; O’Meara, Eileen; Petrie, Mark C.; Vinh, Pham N.; Schou, Morten; Tereshchenko, Sergey; Verma, Subodh; Held, Claes; DeMets, David L.; Docherty, Kieran F.; Jhund, Pardeep S.; Bengtsson, Olof; Sjöstrand, Mikaela; Langkilde, Anna-Maria (21 November 2019). "Dapagliflozin in Patients with Heart Failure and Reduced Ejection Fraction". New England Journal of Medicine. 381 (21): 1995–2008. doi:10.1056/NEJMoa1911303.
- ^ Kato, Eri T.; Silverman, Michael G.; Mosenzon, Ofri; Zelniker, Thomas A.; Cahn, Avivit; Furtado, Remo H.M.; Kuder, Julia; Murphy, Sabina A.; Bhatt, Deepak L.; Leiter, Lawrence A.; McGuire, Darren K.; Wilding, John P.H.; Bonaca, Marc P.; Ruff, Christian T.; Desai, Akshay S.; Goto, Shinya; Johansson, Peter A.; Gause-Nilsson, Ingrid; Johanson, Per; Langkilde, Anna Maria; Raz, Itamar; Sabatine, Marc S.; Wiviott, Stephen D. (28 May 2019). "Effect of Dapagliflozin on Heart Failure and Mortality in Type 2 Diabetes Mellitus". Circulation. 139 (22): 2528–2536. doi:10.1161/CIRCULATIONAHA.119.040130.
- ^ "FARXIGA Granted Fast Track Designation in the US for Heart Failure Following Acute Myocardial Infarction Leveraging an Innovative Registry-Based Trial Design". www.businesswire.com. 16 July 2020. Archived from the original on 20 July 2020. Retrieved 20 July 2020.
- ^ "FARXIGA Demonstrated Unprecedented Reduction in the Risk of Kidney Failure and Cardiovascular or Renal Death in Patients with Chronic Kidney Disease in the Phase III DAPA-CKD Trial". 30 August 2020. Archived from the original on 31 August 2020. Retrieved 4 September 2020.
- ^ "Drugs@FDA: Dapagliflozin". U.S. Food and Drug Administration (FDA). Archived from the original on 25 March 2022. Retrieved 25 March 2022.
- ^ "Archived copy". Archived from the original on 10 June 2022. Retrieved 8 June 2022.
{{cite web}}: CS1 maint: archived copy as title (link) - ^ "Dapagliflozin – USA". 15 October 2021. Archived from the original on 10 June 2022. Retrieved 8 June 2022.
- ^ McMurray JJ, Solomon SD, Inzucchi SE, et al. (November 2019). "Dapagliflozin in Patients with Heart Failure and Reduced Ejection Fraction". New England Journal of Medicine. 381 (21): 1995–2008. doi:10.1056/NEJMoa1911303. PMID 31535829.
- ^ Zhai, Miaobo; Du, Xin; Liu, Changmei; Xu, Huipu (30 June 2021). "The Effects of Dapagliflozin in Patients With Heart Failure Complicated With Type 2 Diabetes: A Meta-Analysis of Placebo-Controlled Randomized Trials". Frontiers in Clinical Diabetes and Healthcare. 2: 703937. doi:10.3389/fcdhc.2021.703937.
External links
- "Dapagliflozin". Drug Information Portal. U.S. National Library of Medicine.
- "Dapagliflozin mixture with metformin hydrochloride". Drug Information Portal. U.S. National Library of Medicine.
- "Dapagliflozin mixture with saxagliptin". Drug Information Portal. U.S. National Library of Medicine.
Clinical trials
- Clinical trial number NCT00528372 for "A Phase III Study of BMS-512148 (Dapagliflozin) in Patients With Type 2 Diabetes Who Are Not Well Controlled With Diet and Exercise" at ClinicalTrials.gov
- Clinical trial number NCT00643851 for "An Efficacy & Safety Study of BMS-512148 in Combination With Metformin Extended Release Tablets" at ClinicalTrials.gov
- Clinical trial number NCT00859898 for "Study of Dapagliflozin in Combination With Metformin XR to Initiate the Treatment of Type 2 Diabetes" at ClinicalTrials.gov
- Clinical trial number NCT00528879 for "A Phase III Study of BMS-512148 (Dapagliflozin) in Patients With Type 2 Diabetes Who Are Not Well Controlled on Metformin Alone" at ClinicalTrials.gov
- Clinical trial number NCT00660907 for "Efficacy and Safety of Dapagliflozin in Combination With Metformin in Type 2 Diabetes Patients" at ClinicalTrials.gov
- Clinical trial number NCT00680745 for "Efficacy and Safety of Dapagliflozin in Combination With Glimepiride (a Sulphonylurea) in Type 2 Diabetes Patients" at ClinicalTrials.gov
- Clinical trial number NCT01392677 for "Evaluation of Safety and Efficacy of Dapagliflozin in Subjects With Type 2 Diabetes Who Have Inadequate Glycaemic Control on Background Combination of Metformin and Sulfonylurea" at ClinicalTrials.gov
- Clinical trial number NCT00683878 for "Add-on to Thiazolidinedione (TZD) Failures" at ClinicalTrials.gov
- Clinical trial number NCT00984867 for "Dapagliflozin DPPIV Inhibitor add-on Study" at ClinicalTrials.gov
- Clinical trial number NCT00673231 for "Efficacy and Safety of Dapagliflozin, Added to Therapy of Patients With Type 2 Diabetes With Inadequate Glycemic Control on Insulin" at ClinicalTrials.gov
- Clinical trial number NCT02229396 for "Phase 3 28-Week Study With 24-Week and 52-week Extension Phases to Evaluate Efficacy and Safety of Exenatide Once Weekly and Dapagliflozin Versus Exenatide and Dapagliflozin Matching Placebo" at ClinicalTrials.gov
- Clinical trial number NCT02413398 for "A Study to Evaluate the Effect of Dapagliflozin on Blood Glucose Level and Renal Safety in Patients With Type 2 Diabetes (DERIVE)" at ClinicalTrials.gov
- Clinical trial number NCT01730534 for "Multicenter Trial to Evaluate the Effect of Dapagliflozin on the Incidence of Cardiovascular Events (DECLARE-TIMI58)" at ClinicalTrials.gov
- Clinical trial number NCT03036124 for "Study to Evaluate the Effect of Dapagliflozin on the Incidence of Worsening Heart Failure or Cardiovascular Death in Patients With Chronic Heart Failure (DAPA-HF)" at ClinicalTrials.gov

