Diarrhea
| Diarrhea | |
|---|---|
| Specialty | Infectious diseases, gastroenterology |
Diarrhea (from the Greek διάρροια meaning "flowing through"[2]), also spelled diarrhoea, is the condition of having three or more loose or liquid bowel movements per day.[3] It is a common cause of death in developing countries and the second most common cause of infant deaths worldwide. The loss of fluids through diarrhea can cause dehydration and electrolyte imbalances. In 2009 diarrhea was estimated to have caused 1.1 million deaths in people aged 5 and over[4] and 1.5 million deaths in children under the age of 5.[1] Oral rehydration solutions (ORS) with modest amounts of electrolytes and zinc tablets are the treatment of choice and have been estimated to have saved 50 million children in the past 25 years.[1] ORS should be begun at early as possible. Vomiting does often occurs during the first hour or two of treatment with ORS, but this seldom prevents successful rehydration as most of the fluid is still absorbed. The World Health Organization (WHO) recommends that if a child vomits, to wait five or ten minutes and then start again more slowly. Homemade solutions recommended by WHO include salted drinks (e.g. salted rice water or a salted yoghurt drink) and vegetable or chicken soup with salt. If available, supplemental potassium, as well as supplemental zinc, can be added to or given with this homemade solution. It's also recommended that persons with diarrhea, if able, continue or resume eating as this speeds recovery of normal intestinal function and generally leads to diarrhea of shorter duration. Clean plain water can be one of several fluids given.[5] There are commercial solutions such as Pedialyte, and relief agencies such as UNICEF widely distribute packets of salts and sugar. A homemade solution can be made by adding between one-half to one teaspoon of salt (about 2-3 grams) and six teaspoons sugar (about 18 grams) to one liter of water[5][6]. If the person drinks solutions with too much sugar or too much salt, these can draw fluid from the body to the bowel, cause osmotic diarrhea, and make dehydration worse.[5] In a WHO publication, it's stated that a homemade Oral rehydration solution (ORS) should approximately have the “taste of tears.”[7]
Definition

Diarrhea is defined by the World Health Organization as having three or more loose or liquid stools per day, or as having more stools than is normal for that person.[3]
Secretory
Secretory diarrhea means that there is an increase in the active secretion, or there is an inhibition of absorption. There is little to no structural damage. The most common cause of this type of diarrhea is a cholera toxin that stimulates the secretion of anions, especially chloride ions. Therefore, to maintain a charge balance in the lumen, sodium is carried with it, along with water. In this type of diarrhea intestinal fluid secretion is isotonic with plasma even during fasting.[8] It continues even when there is no oral food intake.
Osmotic
Osmotic diarrhea occurs when too much water is drawn into the bowels. If a person drinks solutions with excessive sugar or excessive salt, these can draw water from the body into the bowel and cause osmotic diarrhea.[5] Osmotic diarrhea can also be the result of maldigestion (e.g., pancreatic disease or Coeliac disease), in which the nutrients are left in the lumen to pull in water. Or it can be caused by osmotic laxatives (which work to alleviate constipation by drawing water into the bowels). In healthy individuals, too much magnesium or vitamin C or undigested lactose can produce osmotic diarrhea and distention of the bowel. A person who has lactose intolerance can have difficulty absorbing lactose after an extraordinarily high intake of dairy products. In persons who have fructose malabsorption, excess fructose intake can also cause diarrhea. High-fructose foods that also have a high glucose content are more absorbable and less likely to cause diarrhea. Sugar alcohols such as sorbitol (often found in sugar-free foods) are difficult for the body to absorb and, in large amounts, may lead to osmotic diarrhea.[8] In most of these cases, osmotic diarrhea stops when offending agent (e.g. milk, sorbitol) is stopped.
Exudative
Exudative diarrhea occurs with the presence of blood and pus in the stool. This occurs with inflammatory bowel diseases, such as Crohn's disease or ulcerative colitis, and other severe infections such as E. coli or other forms of food poisoning.[8]
Motility-related
Motility-related diarrhea is caused by the rapid movement of food through the intestines (hypermotility). If the food moves too quickly through the gastrointestinal tract, there is not enough time for sufficient nutrients and water to be absorbed. This can be due to a vagotomy or diabetic neuropathy, or a complication of menstruation[citation needed]. Hyperthyroidism can produce hypermotility and lead to pseudodiarrhea and occasionally real diarrhea. Diarrhea can be treated with antimotility agents (such as loperamide). Hypermotility can be observed in people who have had portions of their bowel removed, allowing less total time for absorption of nutrients.
Inflammatory
Inflammatory diarrhea occurs when there is damage to the mucosal lining or brush border, which leads to a passive loss of protein-rich fluids, and a decreased ability to absorb these lost fluids. Features of all three of the other types of diarrhea can be found in this type of diarrhea. It can be caused by bacterial infections, viral infections, parasitic infections, or autoimmune problems such as inflammatory bowel diseases. It can also be caused by tuberculosis, colon cancer, and enteritis. [citation needed]
Dysentery
Generally, if there is blood visible in the stools, it is not diarrhea, but dysentery. The blood is trace of an invasion of bowel tissue. Dysentery is a symptom of, among others, Shigella, Entamoeba histolytica, and Salmonella.
Differential diagnosis
Diarrhea is most commonly due to viral gastroenteritis with rotavirus, which accounts for 40% of cases in children under five.[1] (p. 17) In travelers however bacterial infections predominate.[9] Various toxins such as mushroom poisoning and drugs can also cause acute diarrhea.
Chronic diarrhea can be the part of the presentations of a number of chronic medical conditions affecting the intestine. Common causes include ulcerative colitis, Crohn's disease, microscopic colitis, celiac disease, irritable bowel syndrome and bile acid malabsorption.
Infections
There are many causes of infectious diarrhea, which include viruses, bacteria and parasites.[10] Norovirus is the most common cause of viral diarrhea in adults,[11] but rotavirus is the most common cause in children under five years old.[12] Adenovirus types 40 and 41,[13] and astroviruses cause a significant number of infections.[14]
The bacterium Campylobacter is a common cause of bacterial diarrhea, but infections by Salmonellae, Shigellae and some strains of Escherichia coli (E.coli) are frequent.[15]
In the elderly, particularly those who have been treated with antibiotics for unrelated infections, a toxin produced by Clostridium difficile often causes severe diarrhea.[16]
Parasites do not often cause diarrhea except for the protozoan Giardia, which can cause chronic infections if these are not diagnosed and treated with drugs such as metronidazole,[17] and Entamoeba histolytica.[18][19]
Other infectious agents such as parasites and bacterial toxins also occur.[9] In sanitary living conditions where there is ample food and a supply of clean water, an otherwise healthy person usually recovers from viral infections in a few days. However, for ill or malnourished individuals, diarrhea can lead to severe dehydration and can become life-threatening.[20]
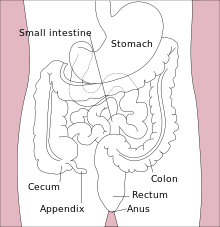
Malabsorption
Malabsorption is the inability to absorb food fully, mostly from disorders in the small bowel, but also due to maldigestion from diseases of the pancreas.
Causes include:
- enzyme deficiencies or mucosal abnormality, as in food allergy and food intolerance, e.g. celiac disease (gluten intolerance), lactose intolerance (intolerance to milk sugar, common in non-Europeans), and fructose malabsorption.
- pernicious anemia, or impaired bowel function due to the inability to absorb vitamin B12,
- loss of pancreatic secretions, which may be due to cystic fibrosis or pancreatitis,
- structural defects, like short bowel syndrome (surgically removed bowel) and radiation fibrosis, such as usually follows cancer treatment and other drugs, including agents used in chemotherapy; and
- certain drugs, like orlistat, which inhibits the absorption of fat.
Inflammatory bowel disease
The two overlapping types here are of unknown origin:
- Ulcerative colitis is marked by chronic bloody diarrhea and inflammation mostly affects the distal colon near the rectum.
- Crohn's disease typically affects fairly well demarcated segments of bowel in the colon and often affects the end of the small bowel.
Irritable bowel syndrome
Another possible cause of diarrhea is irritable bowel syndrome (IBS) which usually presents with abdominal discomfort relieved by defecation and unusual stool (diarrhea or constipation) for at least 3 days a week over the previous 3 months.[21] Symptoms of diarrhea-predominant IBS can be managed through a combination of dietary changes, soluble fiber supplements, and/or medications such as loperamide or codeine. About 30% of patients with diarrhea-predominant IBS have bile acid malabsorption diagnosed with an abnormal SeHCAT test.[22]
Other causes
- Diarrhea can be caused by chronic ethanol ingestion.[23]
- Ischemic bowel disease. This usually affects older people and can be due to blocked arteries.
- Microscopic colitis, a type of inflammatory bowel disease where changes are only seen on histological examination of colonic biopsies.
- Bile salt malabsorption (primary bile acid diarrhea) where excessive bile acids in the colon produce a secretory diarrhea.
- Hormone-secreting tumors: some hormones (e.g., serotonin) can cause diarrhea if excreted in excess (usually from a tumor).
- Chronic mild diarrhea in infants and toddlers may occur with no obvious cause and with no other ill effects; this condition is called toddler's diarrhea.
Pathophysiology
Evolution
According to two researchers, Nesse and Williams, diarrhea may function as an evolved expulsion defense mechanism. As a result, if it is stopped, there might be a delay in recovery.[24] They cite in support of this argument research published in 1973 which found that treating Shigella with the anti-diarrhea drug (Co-phenotrope, Lomotil) caused people to stay feverish twice as long as those not so treated. The researchers indeed themselves observed that: "Lomotil may be contraindicated in shigellosis. Diarrhea may represent a defense mechanism".[25]
Diagnostic approach
The following types of diarrhea may indicate further investigation is needed:
- In infants
- Moderate or severe diarrhea in young children
- Associated with blood
- Continues for more than two days
- Associated non-cramping abdominal pain, fever, weight loss, etc.
- In travelers
- In food handlers, because of the potential to infect others;
- In institutions such as hospitals, child care centers, or geriatric and convalescent homes.
A severity score is used to aid diagnosis in children.[26]
Prevention
A rotavirus vaccine decrease the rates of diarrhea in a population.[1] New vaccines against rotavirus, Shigella, ETEC, and cholera are under development, as well as other causes of infectious diarrhea.
Probiotics decrease the risk of diarrhea in those taking antibiotics.[27] In institutions and in communities, interventions that promote hand washing lead to significant reductions in the incidence of diarrhea.[28]
Management
In many cases of diarrhea, replacing lost fluid and salts is the only treatment needed. This is usually by mouth – oral rehydration therapy – or, in severe cases, intravenously.[1] Diet restrictions such as the BRAT diet are no longer recommended.[29] Research does not support the limiting of milk to children as doing so has no effect on duration of diarrhea.[30]
Medications such as loperamide (Imodium) and bismuth subsalicylate may be beneficial; however they may be contraindicated in certain situations.[31]
Fluids
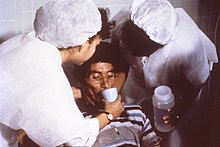
Oral Rehydration Solution (ORS) can be used to prevent dehydration and in many cases is quite literally a life saver. Standard home solutions such as salted rice water, salted yogurt drinks, vegetable and chicken soups with salt can be given. Home solutions such as water in which cereal has been cooked, unsalted soup, green coconut water, weak tea (unsweetened), and unsweetened fresh fruit juices can have from half a teaspoon to full teaspoon of salt (from one-and-a-half to three grams) added per liter. Clean plain water can also be one of several fluids given.[5] There are commercial solutions such as Pedialyte, and relief agencies such as UNICEF widely distribute packets of salts and sugar. A WHO publication for physicians recommends a homemade ORS consisting of one liter water with one teaspoon salt (3 grams) and two tablespoons sugar (18 grams) added[5] (approximately the “taste of tears”[7]). Rehydration Project recommends adding the same amount of sugar but only one-half a teaspoon of salt, stating that this more dilute approach is less risky with very little loss of effectiveness.[6] Both agree that drinks with too much sugar or salt can make dehydration worse.[5][6]
Appropriate amounts of supplemental zinc and potassium should be added if available. But the availability of these should not delay rehydration. As WHO points out, the most important thing is to begin preventing dehydration as early as possible.[5] In another example of prompt ORS hopefully preventing dehydration, CDC recommends for the treatment of cholera continuing to give Oral Rehydration Solution during travel to medical treatment.[32]
Vomiting often occurs during the first hour or two of treatment with ORS, especially if a child drinks the solution too quickly, but this seldom prevents successful rehydration since most of the fluid is still absorbed. WHO recommends that if a child vomits, to wait five or ten minutes and then start to give the solution again more slowly.[5]
WHO recommends a child with diarrhea continue to be fed. Continued feeding speeds the recovery of normal intestinal function. In contrast, children whose food is restricted, have diarrhea of longer duration and recover intestinal function more slowly. A child should also continue to be breastfed.[5] And in the example of the treatment of cholera, CDC also recommends that persons continue to eat and children continue to be breastfed.[32]
Antibiotics
While antibiotics are beneficial in certain types of acute diarrhea, they are usually not used except in specific situations.[33][34] There are concerns that antibiotics may increase the risk of hemolytic uremic syndrome in people infected with Escherichia coli O157:H7.[35] In resource poor countries, treatment with antibiotics may be beneficial.[34] However, some bacteria are developing antibiotic resistance, particularly Shigella.[36]
Antibiotics can also cause diarrhea, and antibiotic-associated diarrhea is the most common adverse effect of treatment with general antibiotics.
Bismuth compounds
While bismuth compounds (Pepto-Bismol) decreased the number of bowel movements in those with travelers' diarrhea, they do not decrease the length of illness.[37] These agents should only be used if bloody diarrhea is not present.[38]
Anti motility agents
Anti motility agents like loperamide are effective at reducing the duration of diarrhea.[34]
Codeine is used in the treatment of diarrhea to slow down peristalsis and the passage of fecal material through the bowels - this means that more time is given for water to reabsorb back into the body, which gives a firmer stool, and also means that feces is passed less frequently.[39]
Bile acid sequestrants
Bile acid sequestrants such as cholestyramine, colestipol and colesevelam can be effective in chronic diarrhea due to bile acid malabsorption. Therapeutic trials of these drugs are indicated in chronic diarrhea if bile acid malabsorption cannot be diagnosed with a specific test, such as SeHCAT retention.
Alternative therapies
Zinc supplementation benefits children suffering from diarrhea in developing countries, but only in infants over six months old. This supports the World Health Organisation guidelines for zinc, but not in the very young.[40]
Probiotics reduce the duration of symptoms by one day and reduced the chances of symptoms lasting longer than four days by 60%.[41] The probiotic lactobacillus can help prevent antibiotic associated diarrhea in adults but possibly not children.[42] For those who with lactose intolerance, taking digestive enzymes containing lactase when consuming dairy products is recommended.
Epidemiology

World wide in 2004 approximately 2.5 billion cases of diarrhea occurred which results in 1.5 million deaths among children under the age of five.[1] Greater than half of these were in Africa and South Asia.[1] This is down from a death rate of 5 million per year two decades ago.[1] Diarrhea remains the second leading cause of death (16%) after pneumonia (17%) in this age group.[1]
See also
References
- ^ a b c d e f g h i j "whqlibdoc.who.int" (PDF). World Health Organization.
- ^ medterms dictionary. "Definition of Diarrhea". Medterms.com.
- ^ a b "Diarrhoea". World Health Organization.
- ^ Straits Times:Diarrhoea kills 3 times more[dead link]
- ^ a b c d e f g h i j k The Treatment Of Diarrhea, A manual for physicians and other senior health workers, World Health Organization, 2005. Sometimes needs to be downloaded twice. See “4.2 Treatment Plan A: home therapy to prevent dehydration and malnutrition,” “4.3 Treatment Plan B: oral rehydration therapy for children with some dehydration,” and “4.4 Treatment Plan C: for patients with severe dehydration” on pages 8 to 16 (12 -20 in PDF). See also “8. MANAGEMENT OF DIARRHOEA WITH SEVERE MALNUTRITION” on pages 22-24 (26-30 in PDF) and “ANNEX 2: ORAL AND INTRAVENOUS REHYDRATION SOLUTIONS” on pages 33-37 (37-41 in PDF).
- ^ a b c Rehydration Project, http://rehydrate.org/ Homemade Oral Rehydration Solution Recipe.
- ^ a b A GUIDE ON SAFE FOOD FOR TRAVELLERS, WELCOME TO SOUTH AFRICA, HOST TO THE 2010 FIFA WORLD CUP (bottom left of page 1).
- ^ a b c "The Basics of Diarrhea". Webmd.com. 17 February 2011. Retrieved 9 March 2011.
- ^ a b Wilson ME (2005). "Diarrhea in nontravelers: risk and etiology". Clin. Infect. Dis. 41. 41 (Suppl 8): S541–6. doi:10.1086/432949. PMID 16267716.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Navaneethan U, Giannella RA (2008). "Mechanisms of infectious diarrhea". Nature Clinical Practice. Gastroenterology & Hepatology. 5 (11): 637–47. doi:10.1038/ncpgasthep1264. PMID 18813221.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Patel MM, Hall AJ, Vinjé J, Parashar UD (2009). "Noroviruses: a comprehensive review". Journal of Clinical Virology. 44 (1): 1–8. doi:10.1016/j.jcv.2008.10.009. PMID 19084472.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Greenberg HB, Estes MK (2009). "Rotaviruses: from pathogenesis to vaccination". Gastroenterology. 136 (6): 1939–51. doi:10.1053/j.gastro.2009.02.076. PMID 19457420.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Uhnoo I, Svensson L, Wadell G (1990). "Enteric adenoviruses". Baillière's Clinical Gastroenterology. 4 (3): 627–42. doi:10.1016/0950-3528(90)90053-J. PMID 1962727.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Mitchell DK (2002). "Astrovirus gastroenteritis". The Pediatric Infectious Disease Journal. 21 (11): 1067–9. doi:10.1097/01.inf.0000036683.11146.c7. PMID 12442031.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Viswanathan VK, Hodges K, Hecht G (2009). "Enteric infection meets intestinal function: how bacterial pathogens cause diarrhoea". Nature Reviews. Microbiology. 7 (2): 110–9. doi:10.1038/nrmicro2053. PMID 19116615.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Rupnik M, Wilcox MH, Gerding DN (2009). "Clostridium difficile infection: new developments in epidemiology and pathogenesis". Nature Reviews. Microbiology. 7 (7): 526–36. doi:10.1038/nrmicro2164. PMID 19528959.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Kiser JD, Paulson CP, Brown C (2008). "Clinical inquiries. What's the most effective treatment for giardiasis?". The Journal of Family Practice. 57 (4): 270–2. PMID 18394362. Retrieved 3 August 2009.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Dans L, Martínez E (2006). "Amoebic dysentery". Clinical Evidence (15): 1007–13. PMID 16973041.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Gonzales ML, Dans LF, Martinez EG (2009). Gonzales, Maria Liza M (ed.). "Antiamoebic drugs for treating amoebic colitis". Cochrane Database Syst Rev (2): CD006085. doi:10.1002/14651858.CD006085.pub2. PMID 19370624.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Alam NH, Ashraf H (2003). "Treatment of infectious diarrhea in children". Paediatr Drugs. 5 (3): 151–65. PMID 12608880.
- ^ Longstreth GF, Thompson WG, Chey WD, Houghton LA, Mearin F, Spiller RC (2006). "Functional bowel disorders". Gastroenterology. 130 (5): 1480–91. doi:10.1053/j.gastro.2005.11.061. PMID 16678561.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Wedlake, L (2009). "Systematic review: the prevalence of idiopathic bile acid malabsorption as diagnosed by SeHCAT scanning in patients with diarrhoea-predominant irritable bowel syndrome". Alimentary pharmacology & therapeutics. 30 (7): 707–17. doi:10.1111/j.1365-2036.2009.04081.x. PMID 19570102.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Kasper DL, Braunwald E, Fauci AS, Hauser SL, Longo DL, Jameson JL. Harrison's Principles of Internal Medicine. New York: McGraw-Hill, 2005. ISBN 0-07-139140-1.
- ^ Williams, George; Nesse, Randolph M. (1996). Why we get sick: the new science of Darwinian medicine. New York: Vintage Books. pp. 36–38. ISBN 0-679-74674-9.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ^ DuPont HL, Hornick RB (1973). "Adverse effect of lomotil therapy in shigellosis". JAMA. 226 (13): 1525–8. doi:10.1001/jama.226.13.1525. PMID 4587313.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Ruuska T, Vesikari T (1990). "Rotavirus disease in Finnish children: use of numerical scores for clinical severity of diarrhoeal episodes". Scand. J. Infect. Dis. 22 (3): 259–67. doi:10.3109/00365549009027046. PMID 2371542.
- ^ Hempel, S (2012 May 9). "Probiotics for the prevention and treatment of antibiotic-associated diarrhea: a systematic review and meta-analysis". JAMA : the journal of the American Medical Association. 307 (18): 1959–69. PMID 22570464.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Ejemot RI, Ehiri JE, Meremikwu MM, Critchley JA (2008). Ejemot, Regina I (ed.). "Hand washing for preventing diarrhoea". Cochrane Database Syst Rev (1): CD004265. doi:10.1002/14651858.CD004265.pub2. PMID 18254044.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ King CK, Glass R, Bresee JS, Duggan C (2003). "Managing acute gastroenteritis among children: oral rehydration, maintenance, and nutritional therapy". MMWR Recomm Rep. 52 (RR–16): 1–16. PMID 14627948.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ "BestBets: Does Withholding milk feeds reduce the duration of diarrhoea in children with acute gastroenteritis?".
- ^ Schiller LR (2007). "Management of diarrhea in clinical practice: strategies for primary care physicians". Rev Gastroenterol Disord. 7 (Suppl 3): S27–38. PMID 18192963.
- ^ a b c Community Health Worker Training Materials for Cholera Prevention and Control, CDC, slides at back are dated 11/17/2010. Page 7 states " . . . Continue to breastfeed your baby if the baby has watery diarrhea, even when traveling to get treatment. Adults and older children should continue to eat frequently."
- ^ Dryden MS, Gabb RJ, Wright SK (1996). "Empirical treatment of severe acute community-acquired gastroenteritis with ciprofloxacin". Clin. Infect. Dis. 22 (6): 1019–25. doi:10.1093/clinids/22.6.1019. PMID 8783703.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ a b c de Bruyn G (2008). "Diarrhoea in adults (acute)". Clin Evid (Online). 2008. PMC 2907942. PMID 19450323.
- ^ Wong CS, Jelacic S, Habeeb RL, Watkins SL, Tarr PI (2000). "The risk of the hemolytic-uremic syndrome after antibiotic treatment of Escherichia coli O157:H7 infections". N. Engl. J. Med. 342 (26): 1930–6. doi:10.1056/NEJM200006293422601. PMID 10874060.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ "Diarrhoeal Diseases". World Health Organization. February 2009.
- ^ DuPont HL; Ericsson CD; Farthing MJ; et al. (2009). "Expert review of the evidence base for self-therapy of travelers' diarrhea". J Travel Med. 16 (3): 161–71. doi:10.1111/j.1708-8305.2009.00300.x. PMID 19538576.
{{cite journal}}: Unknown parameter|author-separator=ignored (help) - ^ Pawlowski SW, Warren CA, Guerrant R (2009). "Diagnosis and treatment of acute or persistent diarrhea". Gastroenterology. 136 (6): 1874–86. doi:10.1053/j.gastro.2009.02.072. PMC 2723735. PMID 19457416.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ "Codeine phosphate tablets". London: netdoctor.co.uk. Retrieved 5 July 2010.
- ^ Lazzerini M, Ronfani L (2008). Lazzerini, Marzia (ed.). "Oral zinc for treating diarrhoea in children". Cochrane Database Syst Rev (3): CD005436. doi:10.1002/14651858.CD005436.pub2. PMID 18646129.
- ^ Allen SJ, Martinez EG, Gregorio GV, Dans LF (2010). Allen, Stephen J (ed.). "Probiotics for treating acute infectious diarrhoea". Cochrane Database Syst Rev. 2010 (11): CD003048. doi:10.1002/14651858.CD003048.pub3. PMID 21069673.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Kale-Pradhan PB, Jassal HK, Wilhelm SM (2010). "Role of Lactobacillus in the prevention of antibiotic-associated diarrhea: a meta-analysis". Pharmacotherapy. 30 (2): 119–26. doi:10.1592/phco.30.2.119. PMID 20099986.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ "Mortality and Burden of Disease Estimates for WHO Member States in 2004" (xls). World Health Organization.
External links
