Cardiac arrest
| Cardiac arrest | |
|---|---|
| Other names | Cardiopulmonary arrest, circulatory arrest, sudden cardiac arrest (SCA)[1] |
 | |
| CPR being administered during a simulation of cardiac arrest | |
| Specialty | Cardiology, emergency medicine |
| Symptoms | Decreased level or total loss of consciousness, abnormal or no breathing, no pulse[1][2] |
| Complications | If reversed, coma, persistent vegetative state, post-cardiac arrest syndrome; if not reversed, death |
| Usual onset | The risk of onset increases with age[3] |
| Causes | Coronary artery disease, congenital heart defect, major blood loss, lack of oxygen, electrical injury, very low potassium, heart failure, myocardial infarction |
| Diagnostic method | Finding no pulse,[1] ECG (EKG)[4] |
| Prevention | Not smoking, physical activity, maintaining a healthy weight, healthy eating[5] |
| Treatment | Cardiopulmonary resuscitation (CPR), defibrillation[6] |
| Prognosis | Overall survival rate ≈10% (outside of hospital) 25% (in hospital);[7][8] depends strongly on type and cause |
| Frequency | 13 per 10,000 people per year (outside hospital in the US)[9] |
| Deaths | > 425,000 per year (U.S.)[10] |
Cardiac arrest, also known as sudden cardiac arrest, is when the heart suddenly and unexpectedly stops beating.[11][1] As a result, blood cannot properly circulate around the body and there is diminished blood flow to the brain and other organs. When the brain does not receive enough blood, this can cause a person to lose consciousness. Coma and persistent vegetative state may result from cardiac arrest. Cardiac arrest is also identified by a lack of central pulses and abnormal or absent breathing.[1]
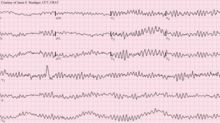
Cardiac arrest and resultant hemodynamic collapse often occur due to arrhythmias (irregular heart rhythms). Ventricular fibrillation and ventricular tachycardia are most commonly recorded.[12] However, as many incidents of cardiac arrest occur out-of-hospital or when a person is not having their cardiac activity monitored, it is difficult to identify the specific mechanism in each case.
Structural heart disease, such as coronary artery disease, is a common underlying condition in people who experience cardiac arrest. The most common risk factors include age and cardiovascular disease.[13] Additional underlying cardiac conditions include heart failure and inherited arrhythmias. Additional factors that may contribute to cardiac arrest include major blood loss, lack of oxygen, electrolyte disturbance (such as very low potassium), electrical injury, and intense physical exercise.[14]
Cardiac arrest is diagnosed by the inability to find a pulse in an unresponsive patient.[4][1] The goal of treatment for cardiac arrest is to rapidly achieve return of spontaneous circulation using a variety of interventions including CPR, defibrillation, and/or cardiac pacing. Two protocols have been established for CPR: basic life support (BLS) and advanced cardiac life support (ACLS).[15]
If return of spontaneous circulation is achieved with these interventions, then sudden cardiac arrest has occurred. By contrast, if the person does not survive the event, this is referred to as sudden cardiac death. Among those whose pulses are re-established, the care team may initiate measures to protect the person from brain injury and preserve neurological function.[16] Some methods may include airway management and mechanical ventilation, maintenance of blood pressure and end-organ perfusion via fluid resuscitation and vasopressor support, correction of electrolyte imbalance, EKG monitoring and management of reversible causes, and temperature management. Targeted temperature management may improve outcomes.[17][18] In post-resuscitation care, an implantable cardiac defibrillator may be considered to reduce the chance of death from recurrence.[5]
Per the 2015 American Heart Association Guidelines, there are approximately 535,000 incidents of cardiac arrest annually (about 13 per 10,000 people).[9] Of these, 326,000 (61%) experience cardiac arrest outside of a hospital setting, while 209,000 (39%) occur within a hospital.[9]
Cardiac arrest becomes more common with age and affects males more often than females.[11] Twice as many black men die from a cardiac arrest as white men. Asian and Hispanic people are not as frequently affected as white people.[11]
Signs and symptoms[edit]
Cardiac arrest is not preceded by any warning symptoms in approximately 50 percent of people.[19] For individuals who do experience symptoms, the symptoms are usually nonspecific to the cardiac arrest.[20] For example, new or worsening chest pain, fatigue, blackouts, dizziness, shortness of breath, weakness, or vomiting.[20][11]
When cardiac arrest is suspected by a layperson (due to signs of unconsciousness, abnormal breathing, and/or no pulse) it should be assumed that the victim is in cardiac arrest. Bystanders should call emergency medical services (such as 911 or 112) and initiate CPR.
Risk factors[edit]
Major risk factors for cardiac arrest include age and underlying cardiovascular disease. A prior episode of sudden cardiac arrest increases the likelihood of future episodes.[21] A 2021 meta-analysis assessing the recurrence of cardiac arrest in out-of-hospital cardiac arrest survivors identified that 15% of survivors experienced a second event, most often in the first year.[22] Furthermore, of those who experienced recurrence, 35% had a third episode.[22]
Additional significant risk factors include cigarette smoking, high blood pressure, high cholesterol, history of arrhythmia, lack of physical exercise, obesity, diabetes, family history, cardiomyopathy, alcohol use, and possibly caffeine intake.[23][24][25][26] Current cigarette smokers with coronary artery disease were found to have a two to threefold increase in the risk of sudden death between ages 30 and 59. Furthermore, it was found that former smokers' risk was closer to that of those who had never smoked.[19][13] A statistical analysis of many of these risk factors determined that approximately 50% of all cardiac arrests occur in 10% of the population perceived to be at greatest risk, due to aggregate harm of multiple risk factors, demonstrating that cumulative risk of multiple comorbidities exceeds the sum of each risk individually.[27]
Causes and mechanisms[edit]
The underlying causes of sudden cardiac arrest can result from cardiac and non-cardiac etiologies. The most common underlying causes are different, depending on the patient's age. Common cardiac causes include coronary artery disease, non-atherosclerotic coronary artery abnormalities, structural heart damage, and inherited arrhythmias. Common non-cardiac causes include respiratory arrest, diabetes, medications, and trauma.
The most common mechanism underlying sudden cardiac arrest is an arrhythmia (an irregular rhythm).[28] Without organized electrical activity in the heart muscle, there is inconsistent contraction of the ventricles, which prevents the heart from generating adequate cardiac output (forward pumping of blood from the heart to the rest of the body).[29] This hemodynamic collapse results in poor blood flow to the brain and other organs, which if prolonged causes persistent damage.
There are many different types of arrhythmias, but the ones most frequently recorded in sudden cardiac arrest are ventricular tachycardia and ventricular fibrillation.[30][31] Both ventricular tachycardia and ventricular fibrillation can prevent the heart from generating coordinated ventricular contractions, thereby failing to sustain adequate blood circulation.
Less common types of arrhythmias occurring in cardiac arrest include pulseless electrical activity, bradycardia, and asystole.[28] These rhythms are seen when there is prolonged cardiac arrest, progression of ventricular fibrillation, or efforts like defibrillation executed to resuscitate the person.[28]
Cardiac causes[edit]
Coronary artery disease[edit]
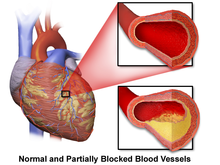
Coronary artery disease (CAD), also known as atherosclerotic cardiovascular disease, involves the deposition of cholesterol and subsequent inflammation-driven formation of atherosclerotic plaques in the arteries. CAD involves the accumulation and remodeling of the coronary vessels along with other systemic blood vessels.[32] When an atherosclerotic plaque dislodges, it can block the flow of blood and oxygen through small arteries, such as the coronary arteries, resulting in ischemic injury. In the heart, this results in myocardial tissue damage which can lead to structural and functional changes that disrupt normal conduction patterns and alter heart rate and contraction.[27]
CAD underlies 68 percent of sudden cardiac deaths in the United States.[33] Indeed, postmortem examinations have shown that the most common finding in cases of sudden cardiac death is chronic, high-grade stenosis of at least one segment of a major coronary artery.[34]
While CAD is a leading contributing factor, this is an age-dependent factor, with CAD being a less common cause of sudden cardiac death in people under the age of 40.[35]
Non-atherosclerotic coronary artery abnormalities[edit]
Abnormalities of the coronary arteries not related to atherosclerosis include inflammation (known as coronary arteritis), embolism, vasospasm, mechanical abnormalities related to connective tissue diseases or trauma, and congenital coronary artery anomalies (most commonly anomalous origin of the left coronary artery from the pulmonary artery). These conditions account for 10-15% of cardiac arrest and sudden cardiac death.[27]
- Coronary arteritis commonly results from a pediatric febrile inflammatory condition known as Kawasaki disease. Other types of vasculitis can also contribute to an increased risk of sudden cardiac death.
- Embolism, or clotting, of the coronary arteries most commonly occurs from septic emboli secondary to endocarditis with involvement of the aortic valve, tricuspid valve, or prosthetic valves.
- Coronary vasospasm may result in cardiac arrhythmias, altering the heart's electrical conduction with a risk of complete cardiac arrest from severe or prolonged rhythm changes.
- Mechanical abnormalities with an associated risk of cardiac arrest may arise from coronary artery dissection, which can be attributed to Marfan Syndrome or trauma.[27]
Structural heart disease[edit]

Examples of structural heart diseases include: cardiomyopathies (hypertrophic, dilated, or arrhythmogenic), cardiac rhythm disturbances, myocarditis, and congestive heart failure.[36]

Left ventricular hypertrophy is a leading cause of sudden cardiac deaths in the adult population.[37][28] This is most commonly the result of longstanding high blood pressure, or hypertension, which has led to maladaptive overgrowth of muscular tissue of the left ventricle, the heart's main pumping chamber.[38] This is because elevated blood pressure over the course of several years requires the heart to adapt to the requirement of pumping harder to adequately circulate blood throughout the body. If the heart does this for a prolonged period of time, the left ventricle can experience hypertrophy (grow larger) in a way that decreases the heart's effectiveness.[39] Left ventricular hypertrophy can be demonstrated on an echocardiogram and electrocardiogram (EKG).[38]
Abnormalities of the cardiac conduction system (notably the Atrioventricular Node and His-Purkinje system) may predispose an individual to arrhythmias with a risk of progressing to sudden cardiac arrest, albeit this risk remains low. Many of these conduction blocks can be treated with internal cardiac defibrillators for those determined to be at high risk due to severity of fibrosis or severe electrophysiologic disturbances.[27]
Structural heart diseases unrelated to coronary artery disease account for 10% of all sudden cardiac deaths.[29][33] A 1999 review of sudden cardiac deaths in the United States found that structural heart diseases accounted for over 30% of sudden cardiac arrests for those under 30 years.[35][33]
Inherited arrhythmia syndromes[edit]
Arrhythmias not due to structural heart disease account for 5 to 10% of sudden cardiac arrests.[40][41][42] These are frequently caused by genetic disorders.[28] The genetic mutations often affect specialized proteins known as ion channels that conduct electrically charged particles across the cell membrane, and this group of conditions is therefore often referred to as channelopathies. Examples of these inherited arrhythmia syndromes include Long QT syndrome (LQTS), Brugada Syndrome, Catecholaminergic polymorphic ventricular tachycardia, and Short QT syndrome. Many are also associated with environmental or neurogenic triggers such as response to loud sounds that can initiate lethal arrhythmias.[27]
LQTS, a condition often mentioned in young people's deaths, occurs in one of every 5000 to 7000 newborns and is estimated to be responsible for 3000 deaths annually compared to the approximately 300,000 cardiac arrests seen by emergency services.[43] These conditions are a fraction of the overall deaths related to cardiac arrest but represent conditions that may be detected prior to arrest and may be treatable. The symptomatic expression of LQTS is quite broad and more often presents with syncope rather than cardiac arrest. The risk of cardiac arrest is still present, and people with family histories of sudden cardiac arrests should be screened for LQTS and other treatable causes of lethal arrhythmia. Higher levels of risk for cardiac arrest are associated with female sex, more significant QT prolongation, history of unexplained syncope (fainting spells), or premature sudden cardiac death.[27] Additionally, individuals with LQTS should avoid certain medications that carry the risk of increasing the severity of this conduction abnormality, such as certain anti-arrhythmics, anti-depressants, and quinolone or macrolide antibiotics.[44]
Another condition that promotes arrhythmias is Wolff-Parkinson-White syndrome, in which an accessory conduction pathway bypassing the atrioventricular node is present and can cause abnormal conduction patterns leading to supraventricular tachycardia and cardiac arrest.[29]
Non-cardiac causes[edit]
Non-cardiac causes account for 15 to 25% of cardiac arrests.[42][45] Common non-cardiac causes include respiratory arrest, diabetes, certain medications, and blunt trauma (especially to the chest).[3][46][47]
- Respiratory arrest will be followed by cardiac arrest unless promptly treated.[47] Respiratory arrest can be caused by pulmonary embolus, choking, drowning, trauma, drug overdose, and poisoning.[3] Pulmonary embolus carries a high mortality rate and may be the triggering cause for up to 5% of cardiac arrests, according to a retrospective study from an urban tertiary care emergency department.[48]
- Diabetes-related factors contributing to cardiac arrest include silent myocardial ischemia, nervous system dysfunction, and electrolyte disturbances leading to abnormal cardiac repolarization.[49]
- Certain medications can worsen an existing arrhythmia. Some examples include antibiotics like macrolides, diuretics, and heart medications such as anti-arrhythmic medications.[3]
Additional non-cardiac causes include hemorrhage, aortic rupture, hypovolemic shock, pulmonary embolism, poisoning such as from the stings of certain jellyfish, and electrical injury.[28][50][51][52]
Circadian patterns are also recognized as triggering factors in cardiac arrest.[53] Per a 2021 systematic review, throughout the day there are two main peak times in which cardiac arrest occurs. The first is in the morning hours and the second is in the afternoon.[54] Moreover, survival rates following cardiac arrest were lowest when occurring between midnight and 6am.[55]
Many of these non-cardiac causes of cardiac arrest are reversible. A common mnemonic used to recall the reversible causes of cardiac arrest is referred to as the Hs and Ts. The Hs are hypovolemia, hypoxia, hydrogen cation excess (acidosis), hyperkalemia, hypokalemia, hypothermia, and hypoglycemia. The Ts are toxins, (cardiac) tamponade, tension pneumothorax, thrombosis (myocardial infarction), thromboembolism, and trauma.
Mechanism[edit]
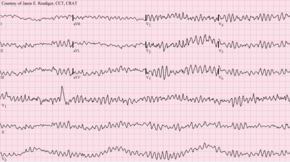
The definitive electrical mechanisms of cardiac arrest, which may arise from any of the functional, structural, or physiologic abnormalities mentioned above, are characterized by arrhythmias.[27] Ventricular fibrillation and pulseless or sustained ventricular tachycardia are the most commonly recorded arrhythmias preceding cardiac arrest. These are rapid and erratic arrhythmias that alter the circulatory pathway such that adequate blood flow cannot be sustained and is inadequate to meet the body's needs.[27]
The mechanism responsible for the majority of sudden cardiac deaths is ventricular fibrillation. Ventricular fibrillation is a tachyarrhythmia characterized by turbulent electrical activity in the ventricular myocardium leading to a heart rate too disorganized and rapid to produce any meaningful cardiac output, thus resulting in insufficient perfusion of the brain and essential organs.[56] Some of the electrophysiologic mechanisms underpinning ventricular fibrillations include ectopic automaticity, re-entry, and triggered activity.[57] However, structural changes in the diseased heart as a result of inherited factors (mutations in ion-channel coding genes, for example) cannot explain the sudden onset of cardiac arrest.[58]
In ventricular tachycardia, the heart also beats faster than normal, which may prevent the heart chambers from properly filling with blood.[59] Ventricular tachycardia is characterized by an altered QRS complex and a heart rate greater than 100 beats per minute.[60] When V-tach is sustained (lasts for at least 30 seconds), inadequate blood flow to heart tissue can lead to cardiac arrest.[61]
Bradyarrhythmias occur following dissociation of spontaneous electrical conduction and the mechanical function of the heart resulting in pulseless electrical activity (PEA) or through complete absence of electrical activity of the heart resulting in asystole. Similar to the result of tachyarrhythmias, these conditions lead to an inability to sustain adequate blood flow as well, though in the case of bradyarrhythmias, the underlying cause is an absence of mechanical activity rather than rapid beats leading to disorganization.[27]
Diagnosis[edit]

Cardiac arrest is synonymous with clinical death.[15] The physical examination to diagnose cardiac arrest focuses on the absence of a pulse.[28] In many cases, lack of a central pulse (carotid arteries or subclavian arteries) is the gold standard. Lack of a pulse in the periphery (radial/pedal) may also result from other conditions (e.g. shock) or be the rescuer's misinterpretation.
Obtaining a thorough history can help inform the potential cause and prognosis.[28] The provider taking the person's clinical history should try to learn whether the episode was observed by anyone else, when it happened, what the patient was doing (in particular whether there was any trauma), and whether drugs were involved.[28]
During resuscitation efforts, continuous monitoring equipment including EKG leads should be attached to the patient so that providers can analyze the electrical activity of the cardiac cycle and use this information to guide the management efforts. EKG readings will help to identify the arrhythmia present and allow the team to monitor any changes that occur with the administration of CPR and defibrillation. Clinicians classify cardiac arrest into "shockable" versus "non-shockable", as determined by the EKG rhythm. This refers to whether a particular class of cardiac dysrhythmia is treatable using defibrillation.[62] The two "shockable" rhythms are ventricular fibrillation and pulseless ventricular tachycardia, while the two "non-shockable" rhythms are asystole and pulseless electrical activity.[63] Moreover, in the post-resuscitation patient, a 12-lead EKG can help identify some causes of cardiac arrest, such as STEMI which may require specific treatments.
Point-of-care ultrasound (POCUS) is a tool that can be used to examine the movement of the heart and its force of contraction at the patient's bedside.[64] POCUS can accurately diagnose cardiac arrest in hospital settings, as well as visualize cardiac wall motion contractions.[64] Using POCUS, clinicians can have limited, two-dimensional views of different parts of the heart during arrest.[65] These images can help clinicians determine whether electrical activity within the heart is pulseless or pseudo-pulseless, as well as help them diagnose the potentially reversible causes of an arrest.[65] Published guidelines from the American Society of Echocardiography, American College of Emergency Physicians, European Resuscitation Council, and the American Heart Association, as well as the 2018 preoperative Advanced Cardiac Life Support guidelines, have recognized the potential benefits of using POCUS in diagnosing and managing cardiac arrest.[65]
POCUS can help predict outcomes in resuscitation efforts. Specifically, use of transthoracic ultrasound can be a helpful tool in predicting mortality in cases of cardiac arrest, with a systematic review from 2020 finding that there is a significant positive correlation between presence of cardiac motion and short term survival with CPR.[66]
Owing to the inaccuracy diagnosis solely based off central pulse detection, some bodies like the European Resuscitation Council have de-emphasized its importance. Instead, the current guidelines prompt individuals to begin CPR on any unconscious person with absent or abnormal breathing.[62] The Resuscitation Council in the United Kingdom stands in line with the European Resuscitation Council's recommendations and those of the American Heart Association.[15] They have suggested that the technique to check carotid pulses should be used only by healthcare professionals with specific training and expertise, and even then that it should be viewed in conjunction with other indicators like agonal respiration.[62]
Various other methods for detecting circulation and therefore diagnosing cardiac arrest have been proposed. Guidelines following the 2000 International Liaison Committee on Resuscitation recommendations were for rescuers to look for "signs of circulation" but not specifically the pulse.[15] These signs included coughing, gasping, color, twitching, and movement.[67] Per evidence that these guidelines were ineffective, the current International Liaison Committee on Resuscitation recommendation is that cardiac arrest should be diagnosed in all casualties who are unconscious and not breathing normally, a similar protocol to that which the European Resuscitation Council has adopted.[15] In a non-acute setting where the patient is expired, diagnosis of cardiac arrest can be done via molecular autopsy or postmortem molecular testing, which uses a set of molecular techniques to find the ion channels that are cardiac defective.[68] This could help elucidate the cause of death in the patient.
Other physical signs or symptoms can help determine the potential cause of the cardiac arrest.[28] Below is a chart of the clinical findings and signs/symptoms a person may have and potential causes associated with them.
| Location | Findings | Possible Causes |
|---|---|---|
| General | Pale skin | Hemorrhage |
| Decreased body temperature | Hypothermia | |
| Airway | Presence of secretions, vomit, blood | Aspiration |
| Inability to provide positive pressure ventilation | Tension pneumothorax | |
| Neck | Distension of the neck veins | Tension pneumothorax |
| Trachea shifted to one side | Tension pneumothorax | |
| Chest | Scar in the middle of the sternum | Cardiac disease |
| Lungs | Breath sounds only on one side | Tension pneumothorax
Aspiration |
| No breath sounds or distant breath sounds | Esophageal intubation
Airway obstruction | |
| Wheezing | Aspiration | |
| Rales | Aspiration
Pulmonary edema Pneumonia | |
| Heart | Decreased heart sounds | Hypovolemia
Cardiac tamponade Tension pneumothorax Pulmonary embolus |
| Abdomen | Distended and dull | Ruptured abdominal aortic aneurysm
Ruptured ectopic pregnancy |
| Distended and tympanic | Esophageal intubation | |
| Rectal | Blood present | Gastrointestinal hemorrhage |
| Extremities | Asymmetrical pulses | Aortic dissection |
| Skin | Needle tracks | Drug abuse |
Prevention[edit]
Primary prevention[edit]
With the lack of positive outcomes following cardiac arrest, efforts have been spent finding effective strategies to prevent cardiac arrest events. The approach to primary prevention promotes a healthy diet, exercise, limited alcohol consumption, and smoking cessation.[5]
Exercise is an effective preventative measure for cardiac arrest in the general population but may be risky for those with pre-existing conditions.[69] The risk of a transient catastrophic cardiac event increases in individuals with heart disease during and immediately after exercise.[69] The lifetime and acute risks of cardiac arrest are decreased in people with heart disease who perform regular exercise, perhaps suggesting the benefits of exercise outweigh the risks.[69]
A 2021 study found that diet may be a modifiable risk factor for a lower incidence of sudden cardiac death.[70] The study found that those who fell under the category of having "Southern diets" representing those of "added fats, fried food, eggs, organ and processed meats, and sugar‐sweetened beverages" had a positive association with an increased risk of cardiac arrest, while those deemed following the "Mediterranean diets" had an inverse relationship regarding the risk of cardiac arrest.[70] According to a 2012 review published, omega-3 PUFA supplementation is not associated with a lower risk of sudden cardiac death.[71]
A Cochrane review published in 2016 found moderate-quality evidence to show that blood pressure-lowering drugs do not reduce the risk of sudden cardiac death.[72]
Secondary prevention[edit]
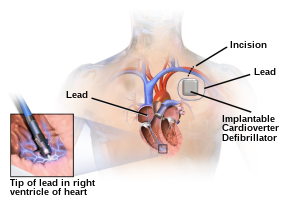
An implantable cardioverter-defibrillator (ICD) is a battery-powered device that monitors electrical activity in the heart, and when an arrhythmia is detected, can deliver an electrical shock to terminate the abnormal rhythm. ICDs are used to prevent sudden cardiac death (SCD) in those who have survived a prior episode of sudden cardiac arrest (SCA) due to ventricular fibrillation or ventricular tachycardia.[73]
Numerous studies have been conducted on the use of ICDs for the secondary prevention of SCD. These studies have shown improved survival with ICDs compared to the use of anti-arrhythmic drugs.[73] ICD therapy is associated with a 50% relative risk reduction in death caused by an arrhythmia and a 25% relative risk reduction in all-cause mortality.[74]
Prevention of SCD with ICD therapy for high-risk patient populations has similarly shown improved survival rates in several large studies. The high-risk patient populations in these studies were defined as those with severe ischemic cardiomyopathy (determined by a reduced left ventricular ejection fraction (LVEF)). The LVEF criteria used in these trials ranged from less than or equal to 30% in MADIT-II to less than or equal to 40% in MUSTT.[73][75]
In certain high-risk patient populations (such as patients with LQTS), ICDs are also used to prevent sudden cardiac death (primary prevention).[75]
Crash teams[edit]
In hospital, a cardiac arrest is referred to as a "crash", or a "code". This typically refers to code blue on the hospital emergency codes. A dramatic drop in vital sign measurements is referred to as "coding" or "crashing", though coding is usually used when it results in cardiac arrest, while crashing might not. Treatment for cardiac arrest is sometimes referred to as "calling a code".
Patients in general wards often deteriorate for several hours or even days before a cardiac arrest occurs.[62][76] This has been attributed to a lack of knowledge and skill amongst ward-based staff, in particular, a failure to measure the respiratory rate, which is often the major predictor of a deterioration[62] and can often change up to 48 hours prior to a cardiac arrest. In response, many hospitals now have increased training for ward-based staff. A number of "early warning" systems also exist that aim to quantify the person's risk of deterioration based on their vital signs and thus provide a guide to staff. In addition, specialist staff are being used more effectively to augment the work already being done at the ward level. These include:
- Crash teams (or code teams) – These are designated staff members with particular expertise in resuscitation who are called to the scene of all arrests within the hospital. This usually involves a specialized cart of equipment (including a defibrillator) and drugs called a "crash cart" or "crash trolley".
- Medical emergency teams – These teams respond to all emergencies with the aim of treating people in the acute phase of their illness in order to prevent a cardiac arrest. These teams have been found to decrease the rates of in-hospital cardiac arrest (IHCA) and improve survival.[9]
- Critical care outreach – In addition to providing the services of the other two types of teams, these teams are responsible for educating non-specialist staff. In addition, they help to facilitate transfers between intensive care/high dependency units and the general hospital wards. This is particularly important as many studies have shown that a significant percentage of patients discharged from critical care environments quickly deteriorate and are re-admitted; the outreach team offers support to ward staff to prevent this from happening.[citation needed]
Management[edit]
Sudden cardiac arrest may be treated via attempts at resuscitation. This is usually carried out based on basic life support, advanced cardiac life support (ACLS), pediatric advanced life support (PALS), or neonatal resuscitation program (NRP) guidelines.[15][77]

Cardiopulmonary resuscitation[edit]
Early cardiopulmonary resuscitation (CPR) is essential to surviving cardiac arrest with good neurological function.[78][28] It is recommended that it be started as soon as possible with minimal interruptions once begun. The components of CPR that make the greatest difference in survival are chest compressions and defibrillating shockable rhythms.[79] After defibrillation, chest compressions should be continued for two minutes before another rhythm check.[28] This is based on a compression rate of 100-120 compressions per minute, a compression depth of 5–6 centimeters into the chest, full chest recoil, and a ventilation rate of 10 breath ventilations per minute.[28] Mechanical chest compressions (as performed by a machine) are no better than chest compressions performed by hand.[80] It is unclear if a few minutes of CPR before defibrillation results in different outcomes than immediate defibrillation.[81]
Correctly performed bystander CPR has been shown to increase survival, however it is performed in fewer than 30% of out-of-hospital cardiac arrests (OHCAs) as of 2007[update].[82] A 2019 meta-analysis found that use of dispatcher-assisted CPR improved outcomes, including survival, when compared with undirected bystander CPR.[83] Likewise, a 2022 systematic review on exercise-related cardiac arrests supported early intervention of bystander CPR and AED use (for shockable rhythms) as they improve survival outcomes.[84]
If high-quality CPR has not resulted in return of spontaneous circulation and the person's heart rhythm is in asystole, stopping CPR and pronouncing the person's death is generally reasonable after 20 minutes.[85] Exceptions to this include certain cases with hypothermia or drowning victims.[79][85] Some of these cases should have longer and more sustained CPR until they are nearly normothermic.[79]
If cardiac arrest occurs after 20 weeks of pregnancy, the uterus should be pulled or pushed to the left during CPR.[86] If a pulse has not returned by four minutes, an emergency Cesarean section is recommended.[86]
Airway management[edit]
High levels of oxygen are generally given during CPR.[80] Either a bag valve mask or an advanced airway may be used to help with breathing particularly since vomiting and regurgitation are common, especially in OHCA.[80][87][88] If this occurs, then modification to existing oropharyngeal suction may be required, such as using suction-assisted airway management.[89]
Tracheal intubation has not been found to improve survival rates or neurological outcomes in cardiac arrest,[82][90] and in the prehospital environment, may worsen it.[91] Endotracheal tubes and supraglottic airways appear equally useful.[90]
Mouth-to-mouth as a means of providing respirations to the person has been phased out due to the risk of contracting infectious diseases from the affected person.[92]
When done by emergency medical personnel, 30 compressions followed by two breaths appear to be better than continuous chest compressions and breaths being given while compressions are ongoing.[93] For bystanders, CPR that involves only chest compressions results in better outcomes as compared to standard CPR for those who have gone into cardiac arrest due to heart issues.[93]
Defibrillation[edit]

Defibrillation is indicated if an electric-shockable heart rhythm is present. The two shockable rhythms are ventricular fibrillation and pulseless ventricular tachycardia. These shockable rhythms have a 25-40% likelihood of survival, compared with a significantly lower rate (less than 5%) in non-shockable rhythms.[94] The non-shockable rhythms include asystole and pulseless electrical activity.
Ventricular fibrillation involves the ventricles of the heart (lower chambers responsible for pumping blood) rapidly contracting in an disorganized pattern, and thereby limiting blood flow from the heart. This can be due to uncoordinated electrical activity.[95] The electrocardiogram (ECG) generally shows irregular QRS complexes without P-waves.[96] By contrast, the ECG for ventricular tachycardia will generally show a wide complex QRS with more than 100 beats occurring per minute.[97] If sustained, ventricular tachycardia can also lead hemodynamic instability and compromise, resulting in pulselessness and poor perfusion to vital organs.
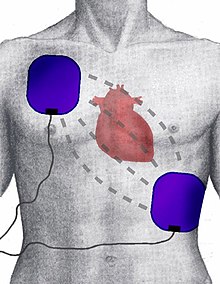
A defibrillator will deliver an electrical current through a pair of electrodes placed on the person's chest. This is thought to depolarize myocardial tissue thereby stopping the arrhythmia.[98] Defibrillators can deliver energy as monophasic or biphasic waveforms, although biphasic defibrillators are the most common.[99][100]
For ventricular fibrillation, defibrillation techniques may utilized either monophasic or biphasic waveforms. Prior studies suggest that biphasic shock is more likely to produce successful defibrillation after a single shock, however rate of survival is comparable between the methods.[100]
In out-of-hospital arrests, the defibrillation is made by an automated external defibrillator (AED), a portable machine that can be used by any user. The AED provides voice instructions that guide the process, automatically checks the person's condition, and applies the appropriate electric shocks. Some defibrillators even provide feedback on the quality of CPR compressions, encouraging the lay rescuer to press the person's chest hard enough to circulate blood.[101]
In addition, there is increasing use of public access defibrillation. This involves placing AEDs in public places and training staff in these areas on how to use them. This allows defibrillation to occur prior to the arrival of emergency services, which has been shown to increase chances of survival. People who have cardiac arrests in remote locations have worse outcomes following cardiac arrest.[102]
Defibrillation is applied to certain arrhythmias such as ventricular fibrillation and pulseless ventricular tachycardia. Defibrillation cannot be applied to asystole, and CPR must be initiated first in this case. Moreover, defibrillation is different than synchronized cardioversion. In synchronized cardioversion, a similar approach is utilized in that electrical current is applied to correct an arrhythmia, however this is used in cases where a pulse is present but the patient is hemodynamically unstable, such as supraventricular tachycardia.
Defibrillators may also be used as part of post-cardiac arrest management. These defibrillators include wearable defibrillator (such as LifeVest), subcutaneous cardiac defibrillator, and implantable cardiac defibrillator.[103]
Medications[edit]
Medications recommended in the ACLS protocol include epinephrine, amiodarone, and lidocaine.[9] The timing and administration of these medications depends on the underlying arrhythmia of the arrest.
Epinephrine acts on the alpha-1 receptor, which in turn increases the blood flow that supplies the heart.[104] Epinephrine in adults improves survival[105] but does not appear to improve neurologically normal survival.[106] In ventricular fibrillation and pulseless ventricular tachycardia, 1 mg of epinephrine is given every 3–5 minutes, following an initial round of CPR and defibrillation.[80] Doses higher than 1 mg of epinephrine are not recommended for routine use in cardiac arrest. If the person has a non-shockable rhythm, such as asystole, following an initial round of CPR, 1 mg of epinephrine should be given every 3–5 minutes, with the goal of obtaining a shockable rhythm.[107]
Amiodarone and lidocaine are anti-arrhythmic medications. Amiodarone is a class III anti-arrhythmic. Amiodarone may be used in cases of ventricular fibrillation, pulseless ventricular tachycardia, and wide complex tachycardia.[108] Lidocaine is a class Ib anti-arrhythmic, also used to manage acute arrhythmias.[109] Anti-arrhythmic medications may be used after an unsuccessful defibrillation attempt. However, neither lidocaine nor amiodarone, in those who continue in ventricular tachycardia or ventricular fibrillation despite defibrillation, improves survival to hospital discharge, despite both equally improving survival to hospital admission.[110] Following an additional round of CPR and defibrillation, amiodarone can also be administered. The first dose is given as a 300 mg bolus. The second dose is given as a 600 mg bolus.[80]
Additional medications[edit]
Bicarbonate, given as sodium bicarbonate, works to stabilize acidosis and hyperkalemia, both of which can contribute to and exacerbate cardiac arrest. If acid-base or electrolyte disturbance is evident, bicarbonate may be used. However, if there is little suspicion that these imbalances are occurring and contributing to the arrest, routine use of bicarbonate is not recommended as it does not provide additional benefit.[111]
Calcium, given as calcium chloride, works as an inotrope and vasopressor. Calcium is used in specific circumstances such as electrolyte disturbances (hyperkalemia) and calcium-channel blocker toxicity. Overall, calcium is not routinely used during cardiac arrest as it does not provide additional benefit (compared to non-use) and may even cause harm (poor neurologic outcomes).[112]
Vasopressin overall does not improve or worsen outcomes compared to epinephrine.[80] The combination of epinephrine, vasopressin, and methylprednisolone appears to improve outcomes.[113]
The use of atropine, lidocaine, and amiodarone have not been shown to improve survival from cardiac arrest.[114][115][79]
Atropine is used for symptomatic bradycardia. It is given at a does of 1 mg (iv), and additional 1 mg (iv) doses can be given every 3–5 minutes for a total of 3 mg. However, the 2010 guidelines from the American Heart Association removed the recommendation for atropine use in pulseless electrical activity and asystole for lack of evidence supporting its use.[116][79]
Special considerations[edit]
Hemodialysis patients carry a greater risk of cardiac arrest events. Multiple factors contribute including increased cardiovascular risk factors, electrolyte disturbances (calcium and potassium, caused by accumulation and aggressive removal), and acid-base disturbances.[117] Calcium levels are considered a key factor contributing to cardiac arrests in this population.[118]
Tricyclic antidepressant (TCA) overdose can lead to cardiac arrest with typical ECG findings including wide QRS and prolonged QTc. Treatment for this condition includes activated charcoal and sodium bicarbonate.[119]
Magnesium can be given at a does of 2 g (iv or oral bolus) to manage torsades de points. However, without specific indication, magnesium is not generally given in cardiac arrest.[120] In people with a confirmed pulmonary embolism as the cause of arrest, thrombolytics may be of benefit.[121][86] Evidence for use of naloxone in those with cardiac arrest due to opioids is unclear, but it may still be used.[86] In people with cardiac arrest due to a local anesthetic, lipid emulsion may be used.[86]
Targeted temperature management[edit]
Current international guidelines suggest cooling adults after cardiac arrest using targeted temperature management (TTM) with the goal of improving neurological outcomes.[122] The process involves cooling for a 24-hour period, with a target temperature of 32–36 °C (90–97 °F), followed by gradual rewarming over the next 12 to 24 hrs.[123][124] There are several methods used to lower the body temperature, such as applying ice packs or cold-water circulating pads directly to the body or infusing cold saline.
The effectiveness of TTM after OHCA is an area of ongoing study. Several recent reviews have found that patients treated with TTM have more favorable neurological outcomes.[18][17] However, pre-hospital TTM after OHCA has been shown to increase the risk of adverse outcomes.[122] The rates of re-arrest may be higher in people who were treated with pre-hospital TTM.[122] Moreover, TTM may have adverse neurological effects in people who survive post-cardiac arrest.[125] Osborn waves on ECG are frequent during TTM, particularly in patients treated with 33 °C.[126] Osborn waves are not associated with increased risk of ventricular arrhythmia, and may be considered a benign physiological phenomenon, associated with lower mortality in univariable analyses.[126]
Do not resuscitate[edit]
Some people choose to avoid aggressive measures at the end of life. A do not resuscitate order (DNR) in the form of an advance health care directive makes it clear that in the event of cardiac arrest, the person does not wish to receive cardiopulmonary resuscitation.[127] Other directives may be made to stipulate the desire for intubation in the event of respiratory failure or, if comfort measures are all that are desired, by stipulating that healthcare providers should "allow natural death".[128]
Chain of survival[edit]
Several organizations promote the idea of a chain of survival. The chain consists of the following "links":
- Early recognition. If possible, recognition of illness before the person develops a cardiac arrest will allow the rescuer to prevent its occurrence. Early recognition that a cardiac arrest has occurred is key to survival, for every minute a patient stays in cardiac arrest, their chances of survival drop by roughly 10%.[62]
- Early CPR improves the flow of blood and of oxygen to vital organs, an essential component of treating a cardiac arrest. In particular, by keeping the brain supplied with oxygenated blood, the chances of neurological damage are decreased.
- Early defibrillation is effective for the management of ventricular fibrillation and pulseless ventricular tachycardia.[62]
- Early advanced care.
- Early post-resuscitation care, which may include percutaneous coronary intervention.[129]
If one or more links in the chain are missing or delayed, then the chances of survival drop significantly.
These protocols are often initiated by a code blue, which usually denotes impending or acute onset of cardiac arrest or respiratory failure.[130]
Other[edit]
Resuscitation with extracorporeal membrane oxygenation devices has been attempted with better results for in-hospital cardiac arrest (29% survival) than OHCA (4% survival) in populations selected to benefit most.[131]
Cardiac catheterization in those who have survived an OHCA appears to improve outcomes, although high-quality evidence is lacking.[132] It is recommended to be done as soon as possible in those who have had a cardiac arrest with ST elevation due to underlying heart problems.[80]
The precordial thump may be considered in those with witnessed, monitored, unstable ventricular tachycardia (including pulseless VT) if a defibrillator is not immediately ready for use, but it should not delay CPR and shock delivery or be used in those with unwitnessed OHCA.[133]
Prognosis[edit]
The overall rate of survival among those who have OHCA is 10%.[134][135] Among those who have an OHCA, 70% occur at home, and their survival rate is 6%.[136][137] For those who have an in-hospital cardiac arrest (IHCA), the survival rate one year from at least the occurrence of cardiac arrest is estimated to be 13%.[138] For IHCA, survival to discharge is around 22%.[139][79] Those who survive to return of spontaneous circulation and hospital admission frequently present with post-cardiac arrest syndrome, which usually presents with neurological injury that can range from mild memory problems to coma.[79] One-year survival is estimated to be higher in people with cardiac admission diagnoses (39%) when compared to those with non-cardiac admission diagnoses (11%).[138]
A 1997 review found rates of survival to discharge of 14%, although different studies varied from 0 to 28%.[140] In those over the age of 70 who have a cardiac arrest while in hospital, survival to hospital discharge is less than 20%.[141] How well these individuals manage after leaving the hospital is not clear.[141]
The global rate of people who were able to recover from OHCA after receiving CPR has been found to be approximately 30%, and the rate of survival to discharge from the hospital has been estimated at 9%.[142] Survival to discharge from the hospital is more likely among people whose cardiac arrest was witnessed by a bystander or emergency medical services, who received bystander CPR, and who live in Europe and North America.[142] Relatively lower survival to hospital discharge rates have been observed in Asian countries.[142]
Prognosis is typically assessed 72 hours or more after cardiac arrest.[143] Rates of survival are better in those who had someone witness their collapse, received bystander CPR, and/or had either V-fib or V-tach when assessed.[144] Survival among those with V-fib or V-tach is 15 to 23%.[144] Women are more likely to survive cardiac arrest and leave the hospital than men.[145] Hypoxic ischemic brain injury is a concerning outcome for people suffering a cardiac arrest.[146] Most improvements in cognition occur during the first three months following cardiac arrest, with some individuals reporting improvement up to one year post-cardiac arrest.[146] 50 – 70% of cardiac arrest survivors report fatigue as a symptom.[146]
Epidemiology[edit]
North America[edit]
The risk of cardiac arrest varies with geographical region, age, and gender. The lifetime risk is three times greater in men (12.3%) than women (4.2%) based on analysis of the Framingham Heart Study.[147] This gender difference disappeared beyond 85 years of age.[148] Around half of these individuals are younger than 65 years of age.[149]
Based on death certificates, sudden cardiac death accounts for about 20% of all deaths in the United States.[150][151] In the United States, approximately 326,000 cases of out-of-hospital and 209,000 cases of IHCA occur among adults annually, which works out to be an incidence of approximately 110.8 per 100,000 adults per year.[9][79][150]
In the United States, during-pregnancy cardiac arrest occurs in about one in twelve-thousand deliveries or 1.8 per 10,000 live births.[86] Rates are lower in Canada.[86]
Other regions[edit]
Non-Western regions of the world have differing incidences. The incidence of sudden cardiac death in China is 41.8 per 100,000 and in South India is 39.7 per 100,000.[150]
Society and culture[edit]
Names[edit]
In many publications, the stated or implicit meaning of "sudden cardiac death" is sudden death from cardiac causes.[152] Some physicians call cardiac arrest "sudden cardiac death" even if the person survives. Thus one can hear mentions of "prior episodes of sudden cardiac death" in a living person.[153]
In 2021, the American Heart Association clarified that "heart attack" is often mistakenly used to describe cardiac arrest. While a heart attack refers to death of heart muscle tissue as a result of blood supply loss, cardiac arrest is caused when the heart's electrical system malfunctions. Furthermore, the American Heart Association explains that "if corrective measures are not taken rapidly, this condition progresses to sudden death. Cardiac arrest should be used to signify an event as described above, that is reversed, usually by CPR and/or defibrillation or cardioversion, or cardiac pacing. Sudden cardiac death should not be used to describe events that are not fatal".[154]
Slow code[edit]
A "slow code" is a slang term for the practice of deceptively delivering sub-optimal CPR to a person in cardiac arrest, when CPR is considered to have no medical benefit.[155] A "show code" is the practice of faking the response altogether for the sake of the person's family.[156]
Such practices are ethically controversial[157] and are banned in some jurisdictions. The European Resuscitation Council Guidelines released a statement in 2021 that clinicians are not suggested to participate/take part in "slow codes".[155] According to the American College of Physicians, half-hearted resuscitation efforts are deceptive and should not be performed by physicians or nurses.[158]
Children[edit]
In children, the most common cause of cardiac arrest is shock or respiratory failure that has not been treated.[28] Cardiac arrhythmias are another possible cause. Arrhythmias such as asystole or bradycardia are more likely in children, in contrast to ventricular fibrillation or tachycardia as seen in adults.[28]
Additional causes of sudden unexplained cardiac arrest in children include hypertrophic cardiomyopathy and coronary artery abnormalities.[159] In childhood hypertrophic cardiomyopathy, previous adverse cardiac events, non-sustained ventricular tachycardia, syncope, and left ventricular hypertrophy have been shown to predict sudden cardiac death.[160] Other causes can include drugs, such as cocaine and methamphetamine, or overdose of medications, such as antidepressants.[28]
For management of pediatric cardiac arrest, CPR should be initiated if suspected. Guidelines provide algorithms for pediatric cardiac arrest management. Recommended medications during pediatric resuscitation include epinephrine, lidocaine, and amiodarone.[161][79][80] However, the use of sodium bicarbonate or calcium is not recommended.[80][162] The use of calcium in children has been associated with poor neurological function as well as decreased survival.[28] Correct dosing of medications in children is dependent on weight, and to minimize time spent calculating medication doses, the use of a Broselow tape is recommended.[28]
Rates of survival in children with cardiac arrest are 3 to 16% in North America.[161]
See also[edit]
References[edit]
- ^ a b c d e f Field JM (2009). The Textbook of Emergency Cardiovascular Care and CPR. Lippincott Williams & Wilkins. p. 11. ISBN 9780781788991. Archived from the original on 2017-09-05.
- ^ "Cardiac Arrest - Symptoms | NHLBI, NIH". www.nhlbi.nih.gov. 27 May 2022. Retrieved 20 September 2023.
- ^ a b c d "Cardiac Arrest - Causes and Risk Factors | NHLBI, NIH". www.nhlbi.nih.gov. 19 May 2022. Retrieved 30 September 2023.
- ^ a b "Cardiac Arrest - Diagnosis | NHLBI, NIH". National Heart, Lung, and Blood Institute, US National Institutes of Health. 19 May 2022. Retrieved 3 October 2022.
- ^ a b c "How Can Death Due to Sudden Cardiac Arrest Be Prevented?". NHLBI. June 22, 2016. Archived from the original on 27 August 2016. Retrieved 16 August 2016.
- ^ "Cardiac Arrest - Treatment". National Heart, Lung, and Blood Institute, US National Institutes of Health. 19 May 2022. Retrieved 24 July 2022.
- ^ Adams JG (2012). Emergency Medicine: Clinical Essentials (Expert Consult – Online). Elsevier Health Sciences. p. 1771. ISBN 978-1455733941. Archived from the original on 2017-09-05.
- ^ Andersen LW, Holmberg MJ, Berg KM, Donnino MW, Granfeldt A (March 2019). "In-Hospital Cardiac Arrest: A Review". JAMA. 321 (12): 1200–1210. doi:10.1001/jama.2019.1696. PMC 6482460. PMID 30912843.
- ^ a b c d e f Kronick SL, Kurz MC, Lin S, Edelson DP, Berg RA, Billi JE, et al. (November 2015). "Part 4: Systems of Care and Continuous Quality Improvement: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care". Circulation. 132 (18 Suppl 2): S397–S413. doi:10.1161/cir.0000000000000258. PMID 26472992. S2CID 10073267.
- ^ Meaney PA, Bobrow BJ, Mancini ME, Christenson J, de Caen AR, Bhanji F, et al. (July 2013). "Cardiopulmonary resuscitation quality: [corrected] improving cardiac resuscitation outcomes both inside and outside the hospital: a consensus statement from the American Heart Association". Circulation. 128 (4): 417–435. doi:10.1161/CIR.0b013e31829d8654. PMID 23801105.
- ^ a b c d "Cardiac Arrest - What Is Cardiac Arrest? | NHLBI, NIH". www.nhlbi.nih.gov. 19 May 2022. Retrieved 20 September 2023.
- ^ Bayés de Luna A, Coumel P, Leclercq JF (January 1989). "Ambulatory sudden cardiac death: mechanisms of production of fatal arrhythmia on the basis of data from 157 cases". American Heart Journal. 117 (1): 151–159. doi:10.1016/0002-8703(89)90670-4. PMID 2911968.
- ^ a b Goldenberg I, Jonas M, Tenenbaum A, Boyko V, Matetzky S, Shotan A, et al. (October 2003). "Current smoking, smoking cessation, and the risk of sudden cardiac death in patients with coronary artery disease". Archives of Internal Medicine. 163 (19): 2301–2305. doi:10.1001/archinte.163.19.2301. PMID 14581249.
- ^ Zheng ZJ, Croft JB, Giles WH, Mensah GA (October 2001). "Sudden cardiac death in the United States, 1989 to 1998". Circulation. 104 (18): 2158–2163. doi:10.1161/hc4301.098254. PMID 11684624.
- ^ a b c d e f ECC Committee, Subcommittees and Task Forces of the American Heart Association (December 2005). "2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care". Circulation. 112 (24 Suppl): IV1-203. doi:10.1161/CIRCULATIONAHA.105.166550. PMID 16314375.
- ^ Neumar RW, Nolan JP, Adrie C, Aibiki M, Berg RA, Böttiger BW, et al. (December 2008). "Post-cardiac arrest syndrome: epidemiology, pathophysiology, treatment, and prognostication. A consensus statement from the International Liaison Committee on Resuscitation (American Heart Association, Australian and New Zealand Council on Resuscitation, European Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Asia, and the Resuscitation Council of Southern Africa); the American Heart Association Emergency Cardiovascular Care Committee; the Council on Cardiovascular Surgery and Anesthesia; the Council on Cardiopulmonary, Perioperative, and Critical Care; the Council on Clinical Cardiology; and the Stroke Council". Circulation. 118 (23): 2452–2483. doi:10.1161/CIRCULATIONAHA.108.190652. PMID 18948368.
- ^ a b Schenone AL, Cohen A, Patarroyo G, Harper L, Wang X, Shishehbor MH, et al. (November 2016). "Therapeutic hypothermia after cardiac arrest: A systematic review/meta-analysis exploring the impact of expanded criteria and targeted temperature". Resuscitation. 108: 102–110. doi:10.1016/j.resuscitation.2016.07.238. PMID 27521472.
- ^ a b Arrich J, Schütz N, Oppenauer J, Vendt J, Holzer M, Havel C, Herkner H (May 2023). "Hypothermia for neuroprotection in adults after cardiac arrest". The Cochrane Database of Systematic Reviews. 5 (5): CD004128. doi:10.1002/14651858.CD004128.pub5. PMC 10202224. PMID 37217440.
- ^ a b Lilly LS, Braunwald E, Mann DL, Zipes DP, Libby P, Bonow RO, Braunwald E (2015). "Cardiac Arrest and Sudden Cardiac Death". In Myerburg RJ (ed.). Braunwald's heart disease: a textbook of cardiovascular medicine (Tenth ed.). Philadelphia, PA: Saunders. pp. 821–860. ISBN 9781455751341. OCLC 890409638.
- ^ a b "What Are the Signs and Symptoms of Sudden Cardiac Arrest?". National Heart, Lung and Blood Institute. 1 April 2011. Archived from the original on 21 June 2015. Retrieved 2015-06-21.
- ^ Kasper DL, Fauci AS, Hauser SL, Longo DL, Jameson JL, Loscalzo J (2014). "327. Cardiovascular Collapse, Cardiac Arrest, and Sudden Cardiac Death". Harrison's principles of internal medicine (19th ed.). New York: Mcgraw-Hill. ISBN 9780071802154. OCLC 893557976.
- ^ a b Lam TJ, Yang J, Poh JE, Ong ME, Liu N, Yeo JW, et al. (July 2022). "Long term risk of recurrence among survivors of sudden cardiac arrest: A systematic review and meta-analysis". Resuscitation. 176: 30–41. doi:10.1016/j.resuscitation.2022.04.027. PMID 35526728. S2CID 248569642.
- ^ Friedlander Y, Siscovick DS, Weinmann S, Austin MA, Psaty BM, Lemaitre RN, et al. (January 1998). "Family history as a risk factor for primary cardiac arrest". Circulation. 97 (2): 155–160. doi:10.1161/01.cir.97.2.155. PMID 9445167.
- ^ Ha AC, Doumouras BS, Wang CN, Tranmer J, Lee DS (April 2022). "Prediction of Sudden Cardiac Arrest in the General Population: Review of Traditional and Emerging Risk Factors". The Canadian Journal of Cardiology. 38 (4): 465–478. doi:10.1016/j.cjca.2022.01.007. PMID 35041932.
- ^ Weinmann S, Siscovick DS, Raghunathan TE, Arbogast P, Smith H, Bovbjerg VE, et al. (September 1997). "Caffeine intake in relation to the risk of primary cardiac arrest". Epidemiology. 8 (5): 505–508. doi:10.1097/00001648-199709000-00006. PMID 9270951.
- ^ Tu SJ, Gallagher C, Elliott AD, Linz D, Pitman BM, Hendriks JM, et al. (February 2022). "Alcohol consumption and risk of ventricular arrhythmias and sudden cardiac death: An observational study of 408,712 individuals". Heart Rhythm. 19 (2): 177–184. doi:10.1016/j.hrthm.2021.09.040. PMID 35101186. S2CID 245422237.
- ^ a b c d e f g h i j Mann DL, Zipes PL, Libby P, Bonow RO, Braunwald E, eds. (2015). Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine (Tenth ed.). Philadelphia, PA: Saunders. p. 826. ISBN 978-1-4557-5134-1. OCLC 881838985.
- ^ a b c d e f g h i j k l m n o p q r s Walls R, Hockberger R, Gausche-Hill M (2017-03-09). Walls RM, Hockberger RS, Gausche-Hill M (eds.). Rosen's emergency medicine : concepts and clinical practice. Elsevier Health Sciences. ISBN 9780323390163. OCLC 989157341.
- ^ a b c Podrid PJ (2016-08-22). "Pathophysiology and etiology of sudden cardiac arrest". www.uptodate.com. Retrieved 2017-12-03.
- ^ Zipes DP, Camm AJ, Borggrefe M, Buxton AE, Chaitman B, Fromer M, et al. (September 2006). "ACC/AHA/ESC 2006 Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death: a report of the American College of Cardiology/American Heart Association Task Force and the European Society of Cardiology Committee for Practice Guidelines (writing committee to develop Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death): developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society". Circulation. 114 (10): e385–e484. doi:10.1161/CIRCULATIONAHA.106.178233. PMID 16935995.
- ^ Landaw J, Yuan X, Chen PS, Qu Z (February 2021). "The transient outward potassium current plays a key role in spiral wave breakup in ventricular tissue". American Journal of Physiology. Heart and Circulatory Physiology. 320 (2): H826–H837. doi:10.1152/ajpheart.00608.2020. PMC 8082802. PMID 33385322.
- ^ Pahwa R, Jialal I (2021). "Atherosclerosis". StatPearls. Treasure Island (FL): StatPearls Publishing. PMID 29939576. Retrieved 2021-11-05.
- ^ a b c Zheng ZJ, Croft JB, Giles WH, Mensah GA (October 2001). "Sudden cardiac death in the United States, 1989 to 1998". Circulation. 104 (18): 2158–2163. doi:10.1161/hc4301.098254. PMID 11684624.
- ^ Falk E, Shah PK (2005). "Pathogenesis of atherothrombosis. Role of vulnerable, ruptured, and eroded plaques". In Fuster V, Topol EJ, Nabel EG (eds.). Atherothrombosis and Coronary Artery Disease. Lippincott Williams & Wilkins. ISBN 9780781735834. Archived from the original on 2016-06-03.
- ^ a b Centers for Disease Control Prevention (CDC) (February 2002). "State-specific mortality from sudden cardiac death--United States, 1999". MMWR. Morbidity and Mortality Weekly Report. 51 (6): 123–126. PMID 11898927.
- ^ Kannel WB, Wilson PW, D'Agostino RB, Cobb J (August 1998). "Sudden coronary death in women". American Heart Journal. 136 (2): 205–212. doi:10.1053/hj.1998.v136.90226. PMID 9704680.
- ^ Stevens SM, Reinier K, Chugh SS (February 2013). "Increased left ventricular mass as a predictor of sudden cardiac death: is it time to put it to the test?". Circulation: Arrhythmia and Electrophysiology. 6 (1): 212–217. doi:10.1161/CIRCEP.112.974931. PMC 3596001. PMID 23424223.
- ^ a b Katholi RE, Couri DM (2011). "Left ventricular hypertrophy: major risk factor in patients with hypertension: update and practical clinical applications". International Journal of Hypertension. 2011: 495349. doi:10.4061/2011/495349. PMC 3132610. PMID 21755036.
- ^ Bornstein AB, Rao SS, Marwaha K (2021). "Left Ventricular Hypertrophy". StatPearls. Treasure Island (FL): StatPearls Publishing. PMID 32491466. Retrieved 2021-11-05.
- ^ Chugh SS, Kelly KL, Titus JL (August 2000). "Sudden cardiac death with apparently normal heart". Circulation. 102 (6): 649–654. doi:10.1161/01.cir.102.6.649. PMID 10931805.
- ^ "Survivors of out-of-hospital cardiac arrest with apparently normal heart. Need for definition and standardized clinical evaluation. Consensus Statement of the Joint Steering Committees of the Unexplained Cardiac Arrest Registry of Europe and of the Idiopathic Ventricular Fibrillation Registry of the United States". Circulation. 95 (1): 265–272. January 1997. doi:10.1161/01.cir.95.1.265. PMID 8994445.
- ^ a b Drory Y, Turetz Y, Hiss Y, Lev B, Fisman EZ, Pines A, Kramer MR (November 1991). "Sudden unexpected death in persons less than 40 years of age". The American Journal of Cardiology. 68 (13): 1388–1392. doi:10.1016/0002-9149(91)90251-f. PMID 1951130.
- ^ "Sudden Cardiac Death". American Heart Association. Archived from the original on 2010-03-25.
- ^ Fazio G, Vernuccio F, Grutta G, Re GL (April 2013). "Drugs to be avoided in patients with long QT syndrome: Focus on the anaesthesiological management". World Journal of Cardiology. 5 (4): 87–93. doi:10.4330/wjc.v5.i4.87. PMC 3653016. PMID 23675554.
- ^ Kuisma M, Alaspää A (July 1997). "Out-of-hospital cardiac arrests of non-cardiac origin. Epidemiology and outcome". European Heart Journal. 18 (7): 1122–1128. doi:10.1093/oxfordjournals.eurheartj.a015407. PMID 9243146.
- ^ Smith JE, Rickard A, Wise D (January 2015). "Traumatic cardiac arrest". Journal of the Royal Society of Medicine. 108 (1): 11–16. doi:10.1177/0141076814560837. PMC 4291327. PMID 25572990.
- ^ a b Chen N, Callaway CW, Guyette FX, Rittenberger JC, Doshi AA, Dezfulian C, Elmer J (September 2018). "Arrest etiology among patients resuscitated from cardiac arrest". Resuscitation. 130: 33–40. doi:10.1016/j.resuscitation.2018.06.024. PMC 6092216. PMID 29940296.
- ^ Kürkciyan I, Meron G, Sterz F, Janata K, Domanovits H, Holzer M, et al. (May 2000). "Pulmonary embolism as a cause of cardiac arrest: presentation and outcome". Archives of Internal Medicine. 160 (10): 1529–1535. doi:10.1001/archinte.160.10.1529. PMID 10826469.
- ^ Bergner DW, Goldberger JJ (2010). "Diabetes mellitus and sudden cardiac death: what are the data?". Cardiology Journal. 17 (2): 117–129. PMID 20544609.
- ^ Raab H, Lindner KH, Wenzel V (November 2008). "Preventing cardiac arrest during hemorrhagic shock with vasopressin". Critical Care Medicine. 36 (11 Suppl). Ovid Technologies (Wolters Kluwer Health): S474–S480. doi:10.1097/ccm.0b013e31818a8d7e. PMID 20449913.
- ^ Voelckel WG, Lurie KG, Lindner KH, Zielinski T, McKnite S, Krismer AC, Wenzel V (September 2000). "Vasopressin improves survival after cardiac arrest in hypovolemic shock". Anesthesia and Analgesia. 91 (3). Ovid Technologies (Wolters Kluwer Health): 627–634. doi:10.1097/00000539-200009000-00024. PMID 10960389.
- ^ Waldmann V, Narayanan K, Combes N, Jost D, Jouven X, Marijon E (April 2018). "Electrical cardiac injuries: current concepts and management". European Heart Journal. 39 (16): 1459–1465. doi:10.1093/eurheartj/ehx142. PMID 28444167.
- ^ Willich SN, Levy D, Rocco MB, Tofler GH, Stone PH, Muller JE (October 1987). "Circadian variation in the incidence of sudden cardiac death in the Framingham Heart Study population". The American Journal of Cardiology. 60 (10): 801–806. doi:10.1016/0002-9149(87)91027-7. PMID 3661393.
- ^ Tran DT, St Pierre Schneider B, McGinnis GR (July 2021). "Circadian Rhythms in Sudden Cardiac Arrest: A Review". Nursing Research. 70 (4): 298–309. doi:10.1097/NNR.0000000000000512. PMID 33883500. S2CID 233349757.
- ^ Tran DT, St Pierre Schneider B, McGinnis GR (July–August 2021). "Circadian Rhythms in Sudden Cardiac Arrest: A Review". Nursing Research. 70 (4): 298–309. doi:10.1097/NNR.0000000000000512. PMID 33883500. S2CID 233349757.
- ^ "Ventricular tachycardia - Symptoms and causes". Mayo Clinic. Retrieved 2021-11-29.
- ^ Szabó Z, Ujvárosy D, Ötvös T, Sebestyén V, Nánási PP (2020-01-29). "Handling of Ventricular Fibrillation in the Emergency Setting". Frontiers in Pharmacology. 10: 1640. doi:10.3389/fphar.2019.01640. PMC 7043313. PMID 32140103.
- ^ Rubart M, Zipes DP (September 2005). "Mechanisms of sudden cardiac death". The Journal of Clinical Investigation. 115 (9): 2305–2315. doi:10.1172/JCI26381. PMC 1193893. PMID 16138184.
- ^ "Ventricular fibrillation - Symptoms and causes". Mayo Clinic. Retrieved 2021-11-29.
- ^ AlMahameed ST, Ziv O (September 2019). "Ventricular Arrhythmias". The Medical Clinics of North America. 103 (5): 881–895. doi:10.1016/j.mcna.2019.05.008. PMID 31378332. S2CID 199437558.
- ^ Baldzizhar A, Manuylova E, Marchenko R, Kryvalap Y, Carey MG (September 2016). "Ventricular Tachycardias: Characteristics and Management". Critical Care Nursing Clinics of North America. 28 (3): 317–329. doi:10.1016/j.cnc.2016.04.004. PMID 27484660.
- ^ a b c d e f g "Resuscitation Council (UK) Guidelines 2005". Archived from the original on 2009-12-15.
- ^ Soar J, Perkins JD, Nolan J, eds. (2012). ABC of resuscitation (6th ed.). Chichester, West Sussex: Wiley-Blackwell. p. 43. ISBN 9781118474853. Archived from the original on 2017-09-05.
- ^ a b Long B, Alerhand S, Maliel K, Koyfman A (March 2018). "Echocardiography in cardiac arrest: An emergency medicine review". The American Journal of Emergency Medicine. 36 (3): 488–493. doi:10.1016/j.ajem.2017.12.031. PMID 29269162. S2CID 3874849.
- ^ a b c Paul JA, Panzer OP (September 2021). "Point-of-care Ultrasound in Cardiac Arrest". Anesthesiology. 135 (3): 508–519. doi:10.1097/ALN.0000000000003811. PMID 33979442. S2CID 234486749.
- ^ Kedan I, Ciozda W, Palatinus JA, Palatinus HN, Kimchi A (January 2020). "Prognostic value of point-of-care ultrasound during cardiac arrest: a systematic review". Cardiovascular Ultrasound. 18 (1): 1. doi:10.1186/s12947-020-0185-8. PMC 6958750. PMID 31931808.
- ^ British Red Cross, St Andrew's Ambulance Association, St John Ambulance (2006). First Aid Manual: The Authorised Manual of St. John Ambulance, St. Andrew's Ambulance Association, and the British Red Cross. Dorling Kindersley. ISBN 978-1-4053-1573-9.
- ^ Glatter KA, Chiamvimonvat N, He Y, Chevalier P, Turillazzi E (2006), Rutty GN (ed.), "Postmortem Analysis for Inherited Ion Channelopathies", Essentials of Autopsy Practice: Current Methods and Modern Trends, Springer, pp. 15–37, doi:10.1007/1-84628-026-5_2, ISBN 978-1-84628-026-9
- ^ a b c Fanous Y, Dorian P (July 2019). "The prevention and management of sudden cardiac arrest in athletes". CMAJ. 191 (28): E787–E791. doi:10.1503/cmaj.190166. PMC 6629536. PMID 31308007.
- ^ a b Shikany JM, Safford MM, Soroka O, Brown TM, Newby PK, Durant RW, Judd SE (July 2021). "Mediterranean Diet Score, Dietary Patterns, and Risk of Sudden Cardiac Death in the REGARDS Study". Journal of the American Heart Association. 10 (13): e019158. doi:10.1161/JAHA.120.019158. PMC 8403280. PMID 34189926.
- ^ Rizos EC, Ntzani EE, Bika E, Kostapanos MS, Elisaf MS (September 2012). "Association between omega-3 fatty acid supplementation and risk of major cardiovascular disease events: a systematic review and meta-analysis". JAMA. 308 (10): 1024–1033. doi:10.1001/2012.jama.11374. PMID 22968891.
- ^ Taverny G, Mimouni Y, LeDigarcher A, Chevalier P, Thijs L, Wright JM, Gueyffier F (March 2016). "Antihypertensive pharmacotherapy for prevention of sudden cardiac death in hypertensive individuals". The Cochrane Database of Systematic Reviews. 2016 (3): CD011745. doi:10.1002/14651858.CD011745.pub2. PMC 8665834. PMID 26961575.
- ^ a b c Epstein AE, DiMarco JP, Ellenbogen KA, Estes NA, Freedman RA, Gettes LS, et al. (May 2008). "ACC/AHA/HRS 2008 Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the ACC/AHA/NASPE 2002 Guideline Update for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices): developed in collaboration with the American Association for Thoracic Surgery and Society of Thoracic Surgeons". Circulation. 117 (21): e350–e408. doi:10.1161/CIRCUALTIONAHA.108.189742. PMID 18483207.
- ^ Connolly SJ, Hallstrom AP, Cappato R, Schron EB, Kuck KH, Zipes DP, et al. (December 2000). "Meta-analysis of the implantable cardioverter defibrillator secondary prevention trials. AVID, CASH and CIDS studies. Antiarrhythmics vs Implantable Defibrillator study. Cardiac Arrest Study Hamburg . Canadian Implantable Defibrillator Study". European Heart Journal. 21 (24): 2071–2078. doi:10.1053/euhj.2000.2476. PMID 11102258.
- ^ a b Shun-Shin MJ, Zheng SL, Cole GD, Howard JP, Whinnett ZI, Francis DP (June 2017). "Implantable cardioverter defibrillators for primary prevention of death in left ventricular dysfunction with and without ischaemic heart disease: a meta-analysis of 8567 patients in the 11 trials". European Heart Journal. 38 (22): 1738–1746. doi:10.1093/eurheartj/ehx028. PMC 5461475. PMID 28329280.
- ^ Kause J, Smith G, Prytherch D, Parr M, Flabouris A, Hillman K (September 2004). "A comparison of antecedents to cardiac arrests, deaths and emergency intensive care admissions in Australia and New Zealand, and the United Kingdom--the ACADEMIA study". Resuscitation. 62 (3): 275–282. doi:10.1016/j.resuscitation.2004.05.016. PMID 15325446.
- ^ American Heart Association (May 2006). "2005 American Heart Association (AHA) guidelines for cardiopulmonary resuscitation (CPR) and emergency cardiovascular care (ECC) of pediatric and neonatal patients: pediatric advanced life support". Pediatrics. 117 (5): e1005–e1028. doi:10.1542/peds.2006-0346. PMID 16651281. S2CID 46720891.
- ^ "AHA Releases 2015 Heart and Stroke Statistics | Sudden Cardiac Arrest Foundation". www.sca-aware.org. Retrieved 21 September 2019.
- ^ a b c d e f g h i Wang VJ, Joing SA, Fitch MT, Cline DM, John Ma O, Cydulka RK (2017-08-28). Cydulka RK (ed.). Tintinalli's emergency medicine manual. McGraw-Hill Education. ISBN 9780071837026. OCLC 957505642.
- ^ a b c d e f g h i Neumar RW, Shuster M, Callaway CW, Gent LM, Atkins DL, Bhanji F, et al. (November 2015). "Part 1: Executive Summary: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care". Circulation. 132 (18 Suppl 2): S315–S367. doi:10.1161/cir.0000000000000252. PMID 26472989.
- ^ Huang Y, He Q, Yang LJ, Liu GJ, Jones A (September 2014). "Cardiopulmonary resuscitation (CPR) plus delayed defibrillation versus immediate defibrillation for out-of-hospital cardiac arrest". The Cochrane Database of Systematic Reviews. 9 (9): CD009803. doi:10.1002/14651858.CD009803.pub2. PMC 6516832. PMID 25212112.
- ^ a b Mutchner L (January 2007). "The ABCs of CPR--again". The American Journal of Nursing. 107 (1): 60–9, quiz 69–70. doi:10.1097/00000446-200701000-00024. PMID 17200636.
- ^ Nikolaou N, Dainty KN, Couper K, Morley P, Tijssen J, Vaillancourt C (May 2019). "A systematic review and meta-analysis of the effect of dispatcher-assisted CPR on outcomes from sudden cardiac arrest in adults and children" (PDF). Resuscitation. 138: 82–105. doi:10.1016/j.resuscitation.2019.02.035. PMID 30853623. S2CID 73727100.
- ^ Grubic N, Hill B, Phelan D, Baggish A, Dorian P, Johri AM (April 2022). "Bystander interventions and survival after exercise-related sudden cardiac arrest: a systematic review". British Journal of Sports Medicine. 56 (7): 410–416. doi:10.1136/bjsports-2021-104623. PMID 34853034. S2CID 244800392.
- ^ a b Resuscitation Council (UK). "Pre-hospital cardiac arrest" (PDF). www.resus.org.uk. p. 41. Archived (PDF) from the original on 13 May 2015. Retrieved 3 September 2014.
- ^ a b c d e f g Lavonas EJ, Drennan IR, Gabrielli A, Heffner AC, Hoyte CO, Orkin AM, et al. (November 2015). "Part 10: Special Circumstances of Resuscitation: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care". Circulation. 132 (18 Suppl 2): S501–S518. doi:10.1161/cir.0000000000000264. PMID 26472998.
- ^ Simons RW, Rea TD, Becker LJ, Eisenberg MS (September 2007). "The incidence and significance of emesis associated with out-of-hospital cardiac arrest". Resuscitation. 74 (3): 427–431. doi:10.1016/j.resuscitation.2007.01.038. PMID 17433526.
- ^ Voss S, Rhys M, Coates D, Greenwood R, Nolan JP, Thomas M, Benger J (December 2014). "How do paramedics manage the airway during out of hospital cardiac arrest?". Resuscitation. 85 (12): 1662–1666. doi:10.1016/j.resuscitation.2014.09.008. eISSN 1873-1570. PMC 4265730. PMID 25260723.
- ^ Root CW, Mitchell OJ, Brown R, Evers CB, Boyle J, Griffin C, et al. (2020-03-01). "Suction Assisted Laryngoscopy and Airway Decontamination (SALAD): A technique for improved emergency airway management". Resuscitation Plus. 1–2: 100005. doi:10.1016/j.resplu.2020.100005. PMC 8244406. PMID 34223292.
- ^ a b White L, Melhuish T, Holyoak R, Ryan T, Kempton H, Vlok R (December 2018). "Advanced airway management in out of hospital cardiac arrest: A systematic review and meta-analysis" (PDF). The American Journal of Emergency Medicine. 36 (12): 2298–2306. doi:10.1016/j.ajem.2018.09.045. PMID 30293843. S2CID 52931036.
- ^ Studnek JR, Thestrup L, Vandeventer S, Ward SR, Staley K, Garvey L, Blackwell T (September 2010). "The association between prehospital endotracheal intubation attempts and survival to hospital discharge among out-of-hospital cardiac arrest patients". Academic Emergency Medicine. 17 (9): 918–925. doi:10.1111/j.1553-2712.2010.00827.x. PMID 20836771.
- ^ Hallstrom A, Cobb L, Johnson E, Copass M (May 2000). "Cardiopulmonary resuscitation by chest compression alone or with mouth-to-mouth ventilation". The New England Journal of Medicine. 342 (21): 1546–1553. doi:10.1056/NEJM200005253422101. PMID 10824072.
- ^ a b Zhan L, Yang LJ, Huang Y, He Q, Liu GJ (March 2017). "Continuous chest compression versus interrupted chest compression for cardiopulmonary resuscitation of non-asphyxial out-of-hospital cardiac arrest". The Cochrane Database of Systematic Reviews. 3 (12): CD010134. doi:10.1002/14651858.CD010134.pub2. PMC 6464160. PMID 28349529.
- ^ Woolcott OO, Reinier K, Uy-Evanado A, Nichols GA, Stecker EC, Jui J, Chugh SS (October 2020). "Sudden cardiac arrest with shockable rhythm in patients with heart failure". Heart Rhythm. 17 (10): 1672–1678. doi:10.1016/j.hrthm.2020.05.038. PMC 7541513. PMID 32504821.
- ^ "Arrhythmias - What Is an Arrhythmia? | NHLBI, NIH". www.nhlbi.nih.gov. 2022-03-24. Retrieved 2024-01-31.
- ^ Ludhwani D, Goayal A, Jagtap M (2024). "Ventricular Fibrillation". StatPearls. Treasure Island (FL): StatPearls Publishing. PMID 30725805. Retrieved 2024-01-31.
- ^ Foth C, Gangwani MK, Ahmed I, Alvey H (2024). "Ventricular Tachycardia". StatPearls. Treasure Island (FL): StatPearls Publishing. PMID 30422549. Retrieved 2024-01-31.
- ^ Knight BP (23 January 2023). Page RL, Dardas TF (eds.). "Basic principles and technique of external electrical cardioversion and defibrillation". UpToDate. Retrieved 2024-01-18.
- ^ Leng CT, Paradis NA, Calkins H, Berger RD, Lardo AC, Rent KC, Halperin HR (June 2000). "Resuscitation after prolonged ventricular fibrillation with use of monophasic and biphasic waveform pulses for external defibrillation". Circulation. 101 (25): 2968–2974. doi:10.1161/01.CIR.101.25.2968. PMID 10869271.
- ^ a b Schneider T, Martens PR, Paschen H, Kuisma M, Wolcke B, Gliner BE, et al. (October 2000). "Multicenter, randomized, controlled trial of 150-J biphasic shocks compared with 200- to 360-J monophasic shocks in the resuscitation of out-of-hospital cardiac arrest victims. Optimized Response to Cardiac Arrest (ORCA) Investigators". Circulation. 102 (15): 1780–1787. doi:10.1161/01.CIR.102.15.1780. PMID 11023932.
- ^ "Zoll Automated External Defibrillator (AED) Plus". Life Assistance Training. Archived from the original on 2011-06-21.
- ^ Lyon RM, Cobbe SM, Bradley JM, Grubb NR (September 2004). "Surviving out of hospital cardiac arrest at home: a postcode lottery?". Emergency Medicine Journal. 21 (5): 619–624. doi:10.1136/emj.2003.010363. PMC 1726412. PMID 15333549.
- ^ Chieng D, Paul V, Denman R (January 2019). "Current Device Therapies for Sudden Cardiac Death Prevention - the ICD, Subcutaneous ICD and Wearable ICD". Heart, Lung & Circulation. 28 (1): 65–75. doi:10.1016/j.hlc.2018.09.011. PMID 30389367. S2CID 53272603.
- ^ "Deep Dive into the Evidence: Epinephrine in Cardiac Arrest". www.emra.org. Retrieved 2021-11-12.
- ^ Vargas M, Buonanno P, Iacovazzo C, Servillo G (March 2019). "Epinephrine for out of hospital cardiac arrest: A systematic review and meta-analysis of randomized controlled trials". Resuscitation. 136: 54–60. doi:10.1016/j.resuscitation.2019.10.026. PMID 30685547. S2CID 207940828.
- ^ Aves T, Chopra A, Patel M, Lin S (27 November 2019). "Epinephrine for Out-of-Hospital Cardiac Arrest: An Updated Systematic Review and Meta-Analysis". Critical Care Medicine. 48 (2): 225–229. doi:10.1097/CCM.0000000000004130. PMID 31789700. S2CID 208537959.
- ^ Panchal AR, Berg KM, Hirsch KG, Kudenchuk PJ, Del Rios M, Cabañas JG, et al. (December 2019). "2019 American Heart Association Focused Update on Advanced Cardiovascular Life Support: Use of Advanced Airways, Vasopressors, and Extracorporeal Cardiopulmonary Resuscitation During Cardiac Arrest: An Update to the American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care". Circulation. 140 (24): e881–e894. doi:10.1161/CIR.0000000000000732. PMID 31722552. S2CID 208019248.
- ^ Florek JB, Lucas A, Girzadas D (2024). "Amiodarone". StatPearls. Treasure Island (FL): StatPearls Publishing. PMID 29489285. Retrieved 2024-01-31.
- ^ Beecham GB, Nessel TA, Goyal A (2024). "Lidocaine". StatPearls. Treasure Island (FL): StatPearls Publishing. PMID 30969703. Retrieved 2024-01-31.
- ^ Sanfilippo F, Corredor C, Santonocito C, Panarello G, Arcadipane A, Ristagno G, Pellis T (October 2016). "Amiodarone or lidocaine for cardiac arrest: A systematic review and meta-analysis". Resuscitation. 107: 31–37. doi:10.1016/j.resuscitation.2016.07.235. PMID 27496262.
- ^ Xu T, Wu C, Shen Q, Xu H, Huang H (November 2023). "The effect of sodium bicarbonate on OHCA patients: A systematic review and meta-analysis of RCT and propensity score studies". The American Journal of Emergency Medicine. 73: 40–46. doi:10.1016/j.ajem.2023.08.020. PMID 37611525. S2CID 260893519.
- ^ Messias Hirano Padrao E, Bustos B, Mahesh A, de Almeida Castro M, Randhawa R, John Dipollina C, et al. (December 2022). "Calcium use during cardiac arrest: A systematic review". Resuscitation Plus. 12: 100315. doi:10.1016/j.resplu.2022.100315. PMC 9550532. PMID 36238582.
- ^ Belletti A, Benedetto U, Putzu A, Martino EA, Biondi-Zoccai G, Angelini GD, et al. (May 2018). "Vasopressors During Cardiopulmonary Resuscitation. A Network Meta-Analysis of Randomized Trials" (PDF). Critical Care Medicine. 46 (5): e443–e451. doi:10.1097/CCM.0000000000003049. hdl:1983/d002beb9-1298-4134-b062-c617f3df43f2. PMID 29652719. S2CID 4851288. Archived (PDF) from the original on 5 March 2020.
- ^ McLeod SL, Brignardello-Petersen R, Worster A, You J, Iansavichene A, Guyatt G, Cheskes S (December 2017). "Comparative effectiveness of antiarrhythmics for out-of-hospital cardiac arrest: A systematic review and network meta-analysis". Resuscitation. 121: 90–97. doi:10.1016/j.resuscitation.2017.10.012. PMID 29037886.
- ^ Ali MU, Fitzpatrick-Lewis D, Kenny M, Raina P, Atkins DL, Soar J, et al. (November 2018). "Effectiveness of antiarrhythmic drugs for shockable cardiac arrest: A systematic review" (PDF). Resuscitation. 132: 63–72. doi:10.1016/j.resuscitation.2018.08.025. PMID 30179691. S2CID 52154562. Archived (PDF) from the original on 5 March 2020.
- ^ Neumar RW, Otto CW, Link MS, Kronick SL, Shuster M, Callaway CW, et al. (November 2010). "Part 8: adult advanced cardiovascular life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care". Circulation. 122 (18 Suppl 3): S729–S767. doi:10.1161/CIRCULATIONAHA.110.970988. PMID 20956224.
- ^ Makar MS, Pun PH (May 2017). "Sudden Cardiac Death Among Hemodialysis Patients". American Journal of Kidney Diseases. 69 (5): 684–695. doi:10.1053/j.ajkd.2016.12.006. PMC 5457912. PMID 28223004.
- ^ Kim ED, Parekh RS (November 2015). "Calcium and Sudden Cardiac Death in End-Stage Renal Disease". Seminars in Dialysis. 28 (6): 624–635. doi:10.1111/sdi.12419. PMID 26257009. S2CID 5503149.
- ^ Woolf AD, Erdman AR, Nelson LS, Caravati EM, Cobaugh DJ, Booze LL, et al. (January 2007). "Tricyclic antidepressant poisoning: an evidence-based consensus guideline for out-of-hospital management". Clinical Toxicology. 45 (3): 203–233. doi:10.1080/15563650701226192. PMID 17453872.
- ^ Ludwin K, Smereka J, Jaguszewski MJ, Filipiak KJ, Ladny JR, Szarpak L, Wozniak S, Evrin T (2020-10-28). "Place of magnesium sulfate in cardiopulmonary resuscitation. A systematic review and meta-analysis". Disaster and Emergency Medicine Journal. 5 (4): 182–189. doi:10.5603/DEMJ.a2020.0041. ISSN 2543-5957.
- ^ Perrott J, Henneberry RJ, Zed PJ (December 2010). "Thrombolytics for cardiac arrest: case report and systematic review of controlled trials". The Annals of Pharmacotherapy. 44 (12): 2007–2013. doi:10.1345/aph.1P364. PMID 21119096. S2CID 11006778.
- ^ a b c Lindsay PJ, Buell D, Scales DC (March 2018). "The efficacy and safety of pre-hospital cooling after out-of-hospital cardiac arrest: a systematic review and meta-analysis". Critical Care. 22 (1): 66. doi:10.1186/s13054-018-1984-2. PMC 5850970. PMID 29534742.
- ^ Neumar RW, Shuster M, Callaway CW, Gent LM, Atkins DL, Bhanji F, et al. (November 2015). "Part 1: Executive Summary: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care". Circulation. 132 (18 Suppl 2): S315–S367. doi:10.1161/cir.0000000000000252. PMID 26472989.
- ^ Lundbye JB (2012). Therapeutic hypothermia after cardiac arrest : clinical application and management. London: Springer. ISBN 9781447129509. OCLC 802346256.
- ^ Kalra R, Arora G, Patel N, Doshi R, Berra L, Arora P, Bajaj NS (March 2018). "Targeted Temperature Management After Cardiac Arrest: Systematic Review and Meta-analyses". Anesthesia and Analgesia. 126 (3): 867–875. doi:10.1213/ANE.0000000000002646. PMC 5820193. PMID 29239942.
- ^ a b Hadziselimovic E, Thomsen JH, Kjaergaard J, Køber L, Graff C, Pehrson S, et al. (July 2018). "Osborn waves following out-of-hospital cardiac arrest-Effect of level of temperature management and risk of arrhythmia and death". Resuscitation. 128: 119–125. doi:10.1016/j.resuscitation.2018.04.037. PMID 29723608. S2CID 19236851.
- ^ Loertscher L, Reed DA, Bannon MP, Mueller PS (January 2010). "Cardiopulmonary resuscitation and do-not-resuscitate orders: a guide for clinicians". The American Journal of Medicine. 123 (1): 4–9. doi:10.1016/j.amjmed.2009.05.029. PMID 20102982.
- ^ Knox C, Vereb JA (December 2005). "Allow natural death: a more humane approach to discussing end-of-life directives". Journal of Emergency Nursing. 31 (6): 560–561. doi:10.1016/j.jen.2005.06.020. PMID 16308044.
- ^ Millin MG, Comer AC, Nable JV, Johnston PV, Lawner BJ, Woltman N, et al. (November 2016). "Patients without ST elevation after return of spontaneous circulation may benefit from emergent percutaneous intervention: A systematic review and meta-analysis". Resuscitation. 108: 54–60. doi:10.1016/j.resuscitation.2016.09.004. PMID 27640933.
- ^ Eroglu SE, Onur O, Urgan O, Denizbasi A, Akoglu H (2014). "Blue code: Is it a real emergency?". World Journal of Emergency Medicine. 5 (1): 20–23. doi:10.5847/wjem.j.issn.1920-8642.2014.01.003. PMC 4129865. PMID 25215142.
- ^ Lehot JJ, Long-Him-Nam N, Bastien O (December 2011). "[Extracorporeal life support for treating cardiac arrest]". Bulletin de l'Académie Nationale de Médecine. 195 (9): 2025–33, discussion 2033–6. doi:10.1016/S0001-4079(19)31894-1. PMID 22930866.
- ^ Camuglia AC, Randhawa VK, Lavi S, Walters DL (November 2014). "Cardiac catheterization is associated with superior outcomes for survivors of out of hospital cardiac arrest: review and meta-analysis". Resuscitation. 85 (11): 1533–1540. doi:10.1016/j.resuscitation.2014.08.025. PMID 25195073. S2CID 207517242.
- ^ Cave DM, Gazmuri RJ, Otto CW, Nadkarni VM, Cheng A, Brooks SC, et al. (November 2010). "Part 7: CPR techniques and devices: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care". Circulation. 122 (18 Suppl 3): S720–S728. doi:10.1161/CIRCULATIONAHA.110.970970. PMC 3741663. PMID 20956223.
- ^ Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, et al. (March 2017). "Heart Disease and Stroke Statistics-2017 Update: A Report From the American Heart Association". Circulation. 135 (10): e146–e603. doi:10.1161/CIR.0000000000000485. PMC 5408160. PMID 28122885.
- ^ Kusumoto FM, Bailey KR, Chaouki AS, Deshmukh AJ, Gautam S, Kim RJ, et al. (September 2018). "Systematic Review for the 2017 AHA/ACC/HRS Guideline for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society". Circulation. 138 (13): e392–e414. doi:10.1161/CIR.0000000000000550. PMID 29084732.
- ^ Institute of Medicine (2015-06-30). Strategies to Improve Cardiac Arrest Survival: A Time to Act. doi:10.17226/21723. ISBN 9780309371995. PMID 26225413.
- ^ Jollis JG, Granger CB (December 2016). "Improving Care of Out-of-Hospital Cardiac Arrest: Next Steps". Circulation. 134 (25): 2040–2042. doi:10.1161/CIRCULATIONAHA.116.025818. PMID 27994023.
- ^ a b Schluep M, Gravesteijn BY, Stolker RJ, Endeman H, Hoeks SE (November 2018). "One-year survival after in-hospital cardiac arrest: A systematic review and meta-analysis". Resuscitation. 132: 90–100. doi:10.1016/j.resuscitation.2018.09.001. hdl:1765/110349. PMID 30213495. S2CID 52270938.
- ^ Kronick SL, Kurz MC, Lin S, Edelson DP, Berg RA, Billi JE, et al. (November 2015). "Part 4: Systems of Care and Continuous Quality Improvement: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care". Circulation. 132 (18 Suppl 2): S397–S413. doi:10.1161/cir.0000000000000258. PMID 26472992. S2CID 10073267.
- ^ Ballew KA (May 1997). "Cardiopulmonary resuscitation". BMJ. 314 (7092): 1462–1465. doi:10.1136/bmj.314.7092.1462. PMC 2126720. PMID 9167565.
- ^ a b van Gijn MS, Frijns D, van de Glind EM, C van Munster B, Hamaker ME (July 2014). "The chance of survival and the functional outcome after in-hospital cardiopulmonary resuscitation in older people: a systematic review". Age and Ageing. 43 (4): 456–463. doi:10.1093/ageing/afu035. PMID 24760957.
- ^ a b c Yan S, Gan Y, Jiang N, Wang R, Chen Y, Luo Z, et al. (February 2020). "The global survival rate among adult out-of-hospital cardiac arrest patients who received cardiopulmonary resuscitation: a systematic review and meta-analysis". Critical Care. 24 (1): 61. doi:10.1186/s13054-020-2773-2. PMC 7036236. PMID 32087741.
- ^ Neumar RW, Shuster M, Callaway CW, Gent LM, Atkins DL, Bhanji F, et al. (November 2015). "Part 1: Executive Summary: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care". Circulation. 132 (18 Suppl 2): S315–S367. doi:10.1161/cir.0000000000000252. PMID 26472989.
- ^ a b Sasson C, Rogers MA, Dahl J, Kellermann AL (January 2010). "Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis". Circulation: Cardiovascular Quality and Outcomes. 3 (1): 63–81. doi:10.1161/circoutcomes.109.889576. PMID 20123673.
- ^ Bougouin W, Mustafic H, Marijon E, Murad MH, Dumas F, Barbouttis A, et al. (September 2015). "Gender and survival after sudden cardiac arrest: A systematic review and meta-analysis". Resuscitation. 94: 55–60. doi:10.1016/j.resuscitation.2015.06.018. PMID 26143159.
- ^ a b c Gräsner JT, Herlitz J, Tjelmeland IB, Wnent J, Masterson S, Lilja G, et al. (April 2021). "European Resuscitation Council Guidelines 2021: Epidemiology of cardiac arrest in Europe". Resuscitation. 161: 61–79. doi:10.1016/j.resuscitation.2021.02.007. PMID 33773833. S2CID 232408830.
- ^ Lloyd-Jones DM, Berry JD, Ning H, Cai X, Goldberger JJ (2009). "Lifetime risk for sudden cardiac death at selected index ages and by risk factor strata and race: cardiovascular lifetime risk pooling project". Circulation. 120: S416–S417. doi:10.1161/circ.120.suppl_18.S416-c (inactive 31 January 2024).
{{cite journal}}: CS1 maint: DOI inactive as of January 2024 (link) - ^ Zheng ZJ, Croft JB, Giles WH, Mensah GA (October 2001). "Sudden cardiac death in the United States, 1989 to 1998". Circulation. 104 (18): 2158–2163. doi:10.1161/hc4301.098254. PMID 11684624.
- ^ Wang VJ, Joing SA, Fitch MT, Cline DM, John Ma O, Cydulka RK (2017-08-28). Cydulka RK (ed.). Tintinalli's emergency medicine manual. McGraw-Hill Education. ISBN 9780071837026. OCLC 957505642.
- ^ a b c Wong CX, Brown A, Lau DH, Chugh SS, Albert CM, Kalman JM, Sanders P (January 2019). "Epidemiology of Sudden Cardiac Death: Global and Regional Perspectives". Heart, Lung & Circulation. 28 (1): 6–14. doi:10.1016/j.hlc.2018.08.026. PMID 30482683. S2CID 53744984.
- ^ Zimmerman DS, Tan HL (December 2021). "Epidemiology and risk factors of sudden cardiac arrest". Current Opinion in Critical Care. 27 (6): 613–616. doi:10.1097/MCC.0000000000000896. PMID 34629421. S2CID 238581415.
- ^ Dorland WA (9 December 2019). Dorland's illustrated medical dictionary. Elsevier. ISBN 978-1-4557-5643-8. OCLC 1134470998.
- ^ Porter I, Vacek J (May 2008). "Single ventricle with persistent truncus arteriosus as two rare entities in an adult patient: a case report". Journal of Medical Case Reports. 2: 184. doi:10.1186/1752-1947-2-184. PMC 2424060. PMID 18513397.
- ^ Virani SS, Alonso A, Aparicio HJ, Benjamin EJ, Bittencourt MS, Callaway CW, et al. (February 2021). "Heart Disease and Stroke Statistics-2021 Update: A Report From the American Heart Association". Circulation. 143 (8): e254–e743. doi:10.1161/CIR.0000000000000950. PMID 33501848. S2CID 231762900.
- ^ a b Primož P, Gräsner GD, Semeraro JT, Olasveengen F, Soar T, Lott J, Van de Voorde C, Madar P, Zideman J, Mentzelopoulos DA, Gradišek S. European Resuscitation Council Guidelines 2021 : executive summary. OCLC 1258336024.
- ^ "Slow Codes, Show Codes and Death". The New York Times. 22 August 1987. Archived from the original on 18 May 2013. Retrieved 2013-04-06.
- ^ DePalma JA, Ozanich E, Miller S, Yancich LM (November 1999). ""Slow" code: perspectives of a physician and critical care nurse". Critical Care Nursing Quarterly. 22 (3). Lippincott Williams and Wilkins: 89–97. doi:10.1097/00002727-199911000-00014. PMID 10646457. Archived from the original on 2013-03-28. Retrieved 2013-04-07.
- ^ Sulmasy LS, Bledsoe TA (January 2019). "American College of Physicians Ethics Manual: Seventh Edition". Annals of Internal Medicine. 170 (2_Suppl): S1–S32. doi:10.7326/M18-2160. PMID 30641552. S2CID 58004782.
- ^ Topjian AA, Raymond TT, Atkins D, Chan M, Duff JP, Joyner BL, et al. (January 2021). "Part 4: Pediatric Basic and Advanced Life Support 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care". Pediatrics. 147 (Suppl 1): e2020038505D. doi:10.1542/peds.2020-038505D. PMID 33087552. S2CID 224826594.
- ^ Norrish G, Cantarutti N, Pissaridou E, Ridout DA, Limongelli G, Elliott PM, Kaski JP (July 2017). "Risk factors for sudden cardiac death in childhood hypertrophic cardiomyopathy: A systematic review and meta-analysis". European Journal of Preventive Cardiology. 24 (11): 1220–1230. doi:10.1177/2047487317702519. PMID 28482693. S2CID 206821305.
- ^ a b de Caen AR, Berg MD, Chameides L, Gooden CK, Hickey RW, Scott HF, et al. (November 2015). "Part 12: Pediatric Advanced Life Support: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care". Circulation. 132 (18 Suppl 2): S526–S542. doi:10.1161/cir.0000000000000266. PMC 6191296. PMID 26473000.
- ^ Velissaris D, Karamouzos V, Pierrakos C, Koniari I, Apostolopoulou C, Karanikolas M (April 2016). "Use of Sodium Bicarbonate in Cardiac Arrest: Current Guidelines and Literature Review". Journal of Clinical Medicine Research. 8 (4): 277–283. doi:10.14740/jocmr2456w. PMC 4780490. PMID 26985247.
