Risk factors of schizophrenia: Difference between revisions
→External links: rm site per WP:ELNO |
|||
| Line 118: | Line 118: | ||
===Other factors=== |
===Other factors=== |
||
There is an emerging literature on a wide range of prenatal risk factors, such as prenatal stress, intrauterine (in the [[womb]]) malnutrition, and prenatal infection. [[Paternal age effect|Increased paternal age]] has been linked to schizophrenia, possibly due to "chromosomal aberrations and mutations of the aging germline."<ref name="Torrey-2009">{{Cite journal | author = Torrey EF, Buka S, Cannon TD, Goldstein JM, Seidman LJ, Liu T, Hadley T, Rosso IM, Bearden C, Yolken RH | title = Paternal age as a risk factor for schizophrenia: how important is it? | journal = Schizophr Res | volume = 114 | issue = 1-3 | pages = 1–5 | year = 2009 | doi = 10.1016/j.schres.2009.06.017 | pmid = 19683417 | url = http://www.schres-journal.com/article/S0920-9964%2809%2900290-4/abstract }}</ref> Maternal-fetal rhesus or genotype incompatibility has also been linked, via increasing the risk of an adverse prenatal environment. And, in mothers with schizophrenia, an increased risk has been identified via a complex interaction between maternal genotype, maternal behavior, prenatal environment and possibly medication and socioeconomic factors.<ref name=Clarke2006/> |
There is an emerging literature on a wide range of prenatal risk factors, such as prenatal stress, intrauterine (in the [[womb]]) malnutrition, and prenatal infection. [[Paternal age effect|Increased paternal age]] has been linked to schizophrenia, possibly due to "chromosomal aberrations and mutations of the aging germline."<ref name="Torrey-2009">{{Cite journal | author = Torrey EF, Buka S, Cannon TD, Goldstein JM, Seidman LJ, Liu T, Hadley T, Rosso IM, Bearden C, Yolken RH | title = Paternal age as a risk factor for schizophrenia: how important is it? | journal = Schizophr Res | volume = 114 | issue = 1-3 | pages = 1–5 | year = 2009 | doi = 10.1016/j.schres.2009.06.017 | pmid = 19683417 | url = http://www.schres-journal.com/article/S0920-9964%2809%2900290-4/abstract }}</ref> Maternal-fetal rhesus or genotype incompatibility has also been linked, via increasing the risk of an adverse prenatal environment. And, in mothers with schizophrenia, an increased risk has been identified via a complex interaction between maternal genotype, maternal behavior, prenatal environment and possibly medication and socioeconomic factors.<ref name=Clarke2006/> References for many of these environmental risk factors are stocked in an [http://www.polygenicpathways.co.uk/schizrisk.html online database] |
||
==Infections== |
==Infections== |
||
Revision as of 22:06, 9 June 2010
This article may be confusing or unclear to readers. (July 2009) |
The causes of schizophrenia have been the subject of much debate, with various factors proposed and discounted or modified. The language of schizophrenia research under the medical model is scientific. Such studies suggest that genetics, prenatal development, early environment, neurobiology and psychological and social processes are important contributory factors. Current psychiatric research into the development of the disorder is often based on a neurodevelopmental model.
Although no common cause of schizophrenia has been identified in all individuals diagnosed with the condition, currently most researchers and clinicians believe it results from a combination of both brain vulnerabilities (either inherited or acquired) and life events. This widely-adopted approach is known as the 'stress-vulnerability' model,[1] and much scientific debate now focuses on how much each of these factors contributes to the development and maintenance of schizophrenia. Schizophrenia is most commonly first diagnosed during late adolescence or early adulthood, suggesting it is often the end process of childhood and adolescent development. There is on average a somewhat earlier onset for men than women, with the possible influence of the female hormone estrogen being one hypothesis and sociocultural influences another.[2]
Genetics
Evidence suggests that genetic vulnerability and environmental factors can act in combination to result in diagnosis of schizophrenia.[3] Research suggests that genetic vulnerability to schizophrenia is multifactorial, caused by interactions of several genes.[4]
Both individual twin studies and meta-analyses of twin studies estimate the heritability of risk for schizophrenia to be approximately 80% (this refers to the proportion of variation between individuals in a population that is influenced by genetic factors, not the degree of genetic determination of individual risk). Concordance rates between monozygotic twins was close to 50%; whereas dizygotic twins was 17%. Adoption studies have also indicated a somewhat increased risk in those with a parent with schizophrenia even when raised apart. Studies suggest that the phenotype is genetically influenced but not genetically determined; that the variants in genes are generally within the range of normal human variation and have low risk associated with them each individually; and that some interact with each other and with environmental risk factors; and that they may not be specific to schizophrenia.[5]
Some twin studies[6][7] have found rates as low as 11.0%–13.8% among monozygotic twins, and 1.8%–4.1% among dizygotic twins, however. In the "Pairs of Veteran Twins" study, for example, 338 pairs were schizophrenic with only 26 pairs concordant, and it was concluded in one report: "the role of the suggested genetic factor appears to be a limited one; 85 percent of the affected monozygotic pairs in the sample were discordant for schizophrenia".[8] In addition, some scientists criticize the methodology of the twin studies, and have argued that the genetic basis of schizophrenia is still largely unknown or open to different interpretations.[5]
For example, although the concordance of schizophrenia occurrence in monozygotic twins has traditionally been used to estimate a genetic component to the illness, the results could be skewed because of environmental factors like a shared placenta [9][10][11]
After reviewing techniques like: Genome Wide Association Studies; Single Neucleotide Polymorphisms and Copy Number Variations; the Nature journal reports: the basic observation is that, "You have this clear tangible phenomenon in which children resemble their parents"...."Despite what children get told in elementary school science we just don't know how that works," as Professor of ecology and evolutionary biology at Princeton, Leonid Kruglyak says (in reviewing hereditibility in general).[12] It cites schizophrenia as a trait in which the genes have gone missing.
A great deal of effort has been put into molecular genetic studies of schizophrenia, which attempt to identify specific genes which may increase risk. A 2003 review of linkage studies listed seven genes as likely to increase risk for a later diagnosis of the disorder.[3] Two recent reviews[4][5] suggested that the evidence was strongest for two genes known as dysbindin (DTNBP1) and neuregulin (NRG1), and that a number of other genes (such as COMT, RGS4, PPP3CC, ZDHHC8, DISC1, and AKT1) showed some early promising results. Variations near the gene FXYD6 have also been associated with schizophrenia in the UK[13][14] but not in Japan.[15] In 2008, rs7341475 SNP of the reelin gene was associated with an increased risk of schizophrenia in women, but not in men. This female-specific association was replicated in several populations.[16]
The largest most comprehensive genetic study of its kind, involving tests of several hundred single nucleotide polymorphisms (SNPs) in nearly 1,900 individuals with schizophrenia or schizoaffective disorder and 2,000 comparison subjects, reported in 2008 that there was no evidence of any significant association between the disorders and any of 14 previously identified candidate genes (RGS4, DISC1, DTNBP1, STX7, TAAR6, PPP3CC, NRG1, DRD2, HTR2A, DAOA, AKT1, CHRNA7, COMT, and ARVCF). The statistical distributions suggested nothing more than chance variation. The authors concluded that the findings make it unlikely that common SNPs in these genes account for a substantial proportion of the genetic risk for schizophrenia, although small effects could not be ruled out.[17]
The perhaps largest analysis of genetic associations in schizophrenia is with the SzGene database at the Schizophrenia Research Forum. One 2008 meta-analysis examined genetic variants in 16 genes and found nominally significant effects.[18]
Other research has suggested that a greater than average number of rare deletions or duplications of tiny DNA sequences within genes (known as copy number variants) are linked to increased risk for schizophrenia, especially in those "sporadic" cases not linked to family history of schizophrenia, and that the genetic factors and developmental pathways can thus be different in different individuals.[19][20] A genome wide survey of 3,391 individuals with schizophrenia found CNVs in less than 1% of cases. Within them, deletions in regions related to psychosis were observed, as well as deletions on chromosome 15q13.3 and 1q21.1.[21] CNVs occur due to non-homologous allelic recombination mediated by low copy repeats (sequentially similar regions). This results in deletions and duplications of dosage sensitive genes. It has been speculated that CNVs underlie a significant proportion of normal human variation, including differences in cognitive, behavioral, and psychological features, and that CNVs in at least three loci can result in increased risk for schizophrenia in a few individuals.[22] Epigenetics may also play a role in schizophrenia, with the expression of Protocadherin 11 X/Protocadherin Y playing a possible role in schizophrenia.[23]
A 2009 study was able to create mice matching schizophrenic symptoms by the deletion of only one gene set, those of the neuregulin post-synaptic receptor. The result showed that although the mice mostly developed normally, on further brain development, glutamate receptors brokedown. This theory supports the glutamate hypothesis of schizophrenia.[24] Another study in 2009 by Simon Fraser University researchers identifies a link between Autism and Schizophrenia :
"The SFU group found that variations in four sets of genes are related to both autism and schizophrenia. People normally have two copies of each gene, but in autistics some genome locations have only single copies and in schizophrenics extra copies are present at the same locations." "Source"
Obstetric events
It is well established that obstetric complications or events are associated with an increased chance of the child later developing schizophrenia, although overall they constitute a non-specific risk factor with a relatively small effect. Obstetric complications occur in approximately 25 to 30% of the general population and the vast majority do not develop schizophrenia, and likewise the majority of individuals with schizophrenia have not had a detectable obstetric event. Nevertheless, the increased average risk is well-replicated, and such events may moderate the effects of genetic or other environmental risk factors. The specific complications or events most linked to schizophrenia, and the mechanisms of their effects, are still under examination.[25]
One epidemiological finding is that people diagnosed with schizophrenia are more likely to have been born in winter or spring[26] (at least in the northern hemisphere). However, the effect is not large. Explanations have included a greater prevalence of viral infections at that time, or a greater likelihood of vitamin D deficiency. A similar effect (increased likelihood of being born in winter and spring) has also been found with other, healthy populations, such as chess players.[27] Women who were pregnant during the Dutch famine of 1944, where many people were close to starvation (experiencing malnutrition) had a higher chance of having a child who would later develop schizophrenia.[28] Studies of Finnish mothers who were pregnant when they found out that their husbands had been killed during the Winter War of 1939–1940 have shown that their children were significantly more likely to develop schizophrenia when compared with mothers who found out about their husbands' death after pregnancy, suggesting that maternal stress may have an effect.[29]
Fetal growth
Lower than average birth weight has been one of the most consistent findings, indicating slowed fetal growth possibly mediated by genetic effects. Almost any factor adversely affecting the fetus will affect growth rate, however, so the association has been described as not particularly informative regarding causation.[25] In addition, the majority of birth cohort studies have failed to find a link between schizophrenia and low birth weight or other signs of growth retardation.[30]
Animal models have suggested links between intrauterine growth restriction and specific neurological abnormalities similar to those that may be involved in the development of schizophrenia, including ventricular enlargement and reduced hippocampal volume in guinea pigs.[31]
Hypoxia
It has been hypothesized since the 1970s that brain hypoxia (low oxygen levels) before, at or immediately after birth may be a risk factor for the development of schizophrenia.[32][33] This has been recently described as one of the most important of the external factors that influence susceptibility, although studies have been mainly epidemiological. Fetal hypoxia, in the presence of certain unidentified genes, has been correlated with reduced volume of the hippocampus, which is in turn correlated with schizophrenia.[34] Although most studies have interpreted hypoxia as causing some form of neuronal dysfunction or even subtle damage, it has been suggested that the physiological hypoxia that prevails in normal embryonic and fetal development, or pathological hypoxia or ischemia, may exert an effect by regulating or dysregulating genes involved in neurodevelopment. A literature review judged that over 50% of the candidate genes for susceptibility to schizophrenia met criteria for "ischemia–hypoxia regulation and/or vascular expression".[35]
A longitudinal study found that obstetric complications involving hypoxia were one factor associated with neurodevelopmental impairments in childhood and with the later development of schizophreniform disorders.[36] Fetal hypoxia has been found to predict unusual movements at age 4 (but not age 7) among children who go on to develop schizophrenia, suggesting that its effects are specific to the stage of neurodevelopment.[37] A Japanese case study of monozygotic twins discordant for schizophrenia (one has the diagnosis while the other does not) draws attention to their different weights at birth and concludes hypoxia may be the differentiating factor.[38] The unusual functional laterality in speech production (e.g. right hemisphere auditory processing) found in some individuals with schizophrenia could be due to aberrant neural networks established as a compensation for left temporal lobe damage induced by pre- or perinatal hypoxia.[39] Prenatal and perinatal hypoxia appears to be important as one factor in the neurodevelopmental model, with the important implication that some forms of schizophrenia may thus be preventable.[40]
Research on rodents seeking to understand the possible role of prenatal hypoxia in disorders such as schizophrenia has indicated that it can lead to a range of sensorimotor and learning/memory abnormalities. Impairments in motor function and coordination, evident on challenging tasks when the hypoxia was severe enough to cause brain damage, were long-lasting and described as a "hallmark of prenatal hypoxia".[41][42] Several animal studies have indicated that fetal hypoxia can affect many of the same neural substrates implicated in schizophrenia, depending on the severity and duration of the hypoxic event as well as the period of gestation, and in humans moderate or severe (but not mild) fetal hypoxia has been linked to a series of motor, language and cognitive deficits in children, regardless of genetic liability to schizophrenia.[43]
Whereas most studies find only a modest effect of hypoxia in schizophrenia, a longitudinal study using a combination of indicators to detect possible fetal hypoxia, such as early equivalents of Neurological Soft Signs or obstetric complications, reported that the risk of schizophrenia and other nonaffective psychoses was "strikingly elevated" (5.75% versus 0.39%). Although objective estimates of hypoxia did not account for all schizophrenic cases; the study revealed increasing odds of schizophrenia according to graded increase in severity of hypoxia.[44]
Other factors
There is an emerging literature on a wide range of prenatal risk factors, such as prenatal stress, intrauterine (in the womb) malnutrition, and prenatal infection. Increased paternal age has been linked to schizophrenia, possibly due to "chromosomal aberrations and mutations of the aging germline."[45] Maternal-fetal rhesus or genotype incompatibility has also been linked, via increasing the risk of an adverse prenatal environment. And, in mothers with schizophrenia, an increased risk has been identified via a complex interaction between maternal genotype, maternal behavior, prenatal environment and possibly medication and socioeconomic factors.[25] References for many of these environmental risk factors are stocked in an online database
Infections
Numerous viral infections, in utero or in childhood, have been associated with an increased risk of later developing schizophrenia.[46] Schizophrenia is somewhat more common in those born in winter to early spring, when infections are more common.[47]
Influenza has long been studied as a possible factor. A 1988 study found that individuals who were exposed to the Asian flu as second trimester fetuses were at increased risk of eventually developing schizophrenia.[48] This result was corroborated by a later British study of the same pandemic,[49] but not by a 1994 study of the pandemic in Croatia.[50] A Japanese study also found no support for a link between schizophrenia and birth after an influenza epidemic.[51]
Polio, measles, varicella-zoster, rubella, herpes simplex virus type 2, maternal genital infections, and more recently Toxoplasma gondii, have been correlated with the later development of schizophrenia.[52] Psychiatrists E. Fuller Torrey and R.H. Yolken have hypothesized that the latter, a common parasite in humans, contributes to some, if not many, cases of schizophrenia.[53] In a meta-analysis of several studies, they found moderately higher levels of Toxoplasma antibodies in those with schizophrenia[54][55] and possibly higher rates of prenatal or early postnatal exposure to Toxoplasma gondii, but not acute infection. However, in another study of postmortem brain tissue, the authors have reported equivocal or negative results, including no evidence of herpes virus or T. gondii involvement in schizophrenia.[56]
There is some evidence for the role of autoimmunity in the development of some cases of schizophrenia. A statistical correlation has been reported with various autoimmune diseases[57] and direct studies have linked dysfunctional immune status to some of the clinical features of schizophrenia.[58][59]
Childhood antecedents
In general, the antecedents of schizophrenia are subtle and those who will go on to develop schizophrenia do not form a readily identifiable subgroup - which would lead to identification of a specific cause. Average group differences from the norm may be in the direction of superior as well as inferior performance. Overall, birth cohort studies have indicated subtle nonspecific behavioral features, some evidence for psychotic-like experiences (particularly hallucinations), and various cognitive antecedents. There have been some inconsistencies in the particular domains of functioning identified and whether they continue through childhood and whether they are specific to schizophrenia.[30]
A prospective study found average differences across a range of developmental domains, including reaching milestones of motor development at a later age, having more speech problems, lower educational test results, solitary play preferences at ages four and six, and being more socially anxious at age 13. Lower ratings of the mother's skills and understanding of the child at age 4 were also related.[60]
Some of the early developmental differences were identified in the first year of life in a study in Finland, although generally related to psychotic disorders rather than schizophrenia in particular.[61] The early subtle motor signs persisted to some extent, showing a small link to later school performance in adolescence.[62] An earlier Finnish study found that childhood performance of 400 individuals diagnosed with schizophrenia was significantly worse than controls on subjects involving motor co-ordination (sports and handcrafts) between ages 7 and 9, but there were no differences on academic subjects (contrary to some other IQ findings).[63] (Patients in this age group with these symptoms were significantly less likely to progress to high school, despite academic ability[64]) However, reanalysis of the data from the later Finnish study, on older children (14 to 16) in a changed school system, using narrower diagnostic criteria and with less cases but more controls, did not support a significant difference on sports and handicraft performance.[65] However, another study found that unusual motor coordination scores at 7 years of age were associated in adulthood with both those with schizophrenia and their unaffected siblings, while unusual movements at ages 4 and 7 predicted adult schizophrenia but not unaffected sibling status.[37]
A birth cohort study in New Zealand found that children who went on to develop schizophreniform disorder had, as well as emotional problems and interpersonal difficulties linked to all adult psychiatric outcomes measured, significant impairments in neuromotor, receptive language, and cognitive development.[36] A retrospective study found that adults with schizophrenia had performed better than average in artistic subjects at ages 12 and 15, and in linguistic and religious subjects at age 12, but worse than average in gymnastics at age 15.[66]
Some small studies on offspring of individuals with schizophrenia have identified various neurobehavioral deficits,[67] a poorer family environment and disruptive school behaviour,[68] poor peer engagement, immaturity or unpopularity[69] or poorer social competence and increasing schizophrenic symptomology emerging during adolescence.[70]
A minority "deficit syndrome" subtype of schizophrenia is proposed to be more marked by early poor adjustment and behavioral problems, as compared to non-deficit subtypes.[71]
Substance use
The relationship between schizophrenia and drug use is complex, meaning that a clear causal connection between drug use and schizophrenia has been difficult to tease apart. There is strong evidence that using certain drugs can trigger either the onset or relapse of schizophrenia in some people. It may also be the case, however, that people with schizophrenia use drugs to overcome negative feelings associated with both the commonly prescribed antipsychotic medication and the condition itself, where negative emotion, paranoia and anhedonia are all considered to be core features.
The rate of substance use is known to be particularly high in this group. In a recent study, 60% of people with schizophrenia were found to use substances and 37% would be diagnosable with a substance use disorder.[72]
Amphetamines
As amphetamines trigger the release of dopamine and excessive dopamine function is believed to be responsible for many symptoms of schizophrenia (known as the dopamine hypothesis of schizophrenia), amphetamines may worsen schizophrenia symptoms.[73]
Hallucinogens
Schizophrenia can sometimes be triggered by heavy use of hallucinogenic or stimulant drugs,[74] although some[who?] claim that a predisposition towards developing schizophrenia is needed for this to occur. There is also some evidence suggesting that people suffering schizophrenia but responding to treatment can have relapse because of subsequent drug use.
Drugs such as ketamine, PCP, and LSD have been used to mimic schizophrenia for research purposes. Using LSD and other psychedelics as a model has now fallen out of favor with the scientific research community, as the differences between the drug induced states and the typical presentation of schizophrenia have become clear. The dissociatives ketamine and PCP are still considered to produce states that are remarkably similar however.
Cannabis
There is some evidence that cannabis use can contribute to schizophrenia. Some studies suggest that cannabis is neither a sufficient nor necessary factor in developing schizophrenia, but that cannabis may significantly increase the risk of developing schizophrenia and may be, among other things, a significant causal factor. Nevertheless, some previous research in this area has been criticised as it has often not been clear whether cannabis use is a cause or effect of schizophrenia. To address this issue, a recent review of studies from which a causal contribution to schizophrenia can be assessed has suggested that cannabis statistically doubles the risk of developing schizophrenia on the individual level, and may, assuming a causal relationship, be responsible for up to 8% of cases in the population.[75]
An older longitudinal study, published in 1987, suggested sixfold increase of schizophrenia risks for high consumers of cannabis (use on more than fifty occasions) in Sweden.[76]
Despite increases in cannabis consumption in the 1960s and 1970s in western society, rates of psychotic disorders such as schizophrenia remained relatively stable. Sweden and Japan, where self-reported marijuana use is very low, do not have lower rates of psychosis than the U.S. and Canada do.[77] For the theory of true causality to be correct, other factors which are thought to contribute to schizophrenia would have to have converged almost flawlessly to mask the effect of increased cannabis usage.
Clues from tobacco use
People with schizophrenia tend to smoke significantly more tobacco than the general population. The rates are exceptionally high amongst institutionalized patients and homeless people. In a UK census from 1993, 74% of people with schizophrenia living in institutions were found to be smokers.[78][79] A 1999 study that covered all people with schizophrenia in Nithsdale, Scotland found a 58% prevalence rate of cigarette smoking, to compare with 28% in the general population.[80] An older study found that as much as 88% of outpatients with schizophrenia were smokers.[81]
Despite the higher prevalence of tobacco smoking, people diagnosed with schizophrenia have a much lower than average chance of developing and dying from lung cancer. While the reason for this is unknown, it may be because of a genetic resistance to the cancer, a side-effect of drugs being taken, or a statistical effect of increased likelihood of dying from causes other than lung cancer.[82]
A 2003 study of over 50,000 Swedish conscripts found that there was a small but significant protective effect of smoking cigarettes on the risk of developing schizophrenia later in life.[83] While the authors of the study stressed that the risks of smoking far outweigh these minor benefits, this study provides further evidence for the 'self-medication' theory of smoking in schizophrenia and may give clues as to how schizophrenia might develop at the molecular level. Furthermore, many people with schizophrenia have smoked tobacco products long before they are diagnosed with the illness, and some groups advocate that the chemicals in tobacco have actually contributed to the onset of the illness and have no benefit of any kind.[citation needed]
It is of interest that cigarette smoking affects liver function such that the antipsychotic drugs used to treat schizophrenia are broken down in the blood stream more quickly. This means that smokers with schizophrenia need slightly higher doses of antipsychotic drugs in order for them to be effective than do their non-smoking counterparts.[citation needed]
The increased rate of smoking in schizophrenia may be due to a desire to self-medicate with nicotine. One possible reason is that smoking produces a short term effect to improve alertness and cognitive functioning in persons who suffer this illness.[84] It has been postulated that the mechanism of this effect is that people with schizophrenia have a disturbance of nicotinic receptor functioning which is temporarily abated by tobacco use.[84]
A study from 1989[85] and a 2004 case study[86] show that when haloperidol is administered, nicotine limits the extent to which the antipsychotic increases the sensitivity of the dopamine 2 receptor. Dependent on the dopamine system, symptoms of Tardive Dyskinesia are not found in the nicotine administered patients despite a roughly 70% increase in dopamine receptor activity, but the controls have more than 90% and do develop symptoms.A 1997 study showed that akathisia was significantly reduced upon administration of nicotine when the akathisia was induced by antipsychotics.[87] This gives credence to the idea tobacco could be used to self medicate by limiting effects of the illness, the medication, or both.
Life experiences
Social adversity
The chance of developing schizophrenia has been found to increase with the number of adverse social factors (e.g. indicators of socioeconomic disadvantage or social exclusion) present in childhood.[88][89] Stressful life events generally precede the onset of schizophrenia.[90] A personal or recent family history of migration is a considerable risk factor for schizophrenia, which has been linked to psychosocial adversity, social defeat from being an outsider, racial discrimination, family dysfunction, unemployment and poor housing conditions.[91][92] Childhood experiences of abuse or trauma are risk factors for a diagnosis of schizophrenia later in life.[93][94][95][96] Recent large-scale general population studies indicate the relationship is a causal one, with an increasing risk with additional experiences of maltreatment,[97] although a critical review suggests conceptual and methodological issues require further research.[98] There is some evidence that adversities may lead to cognitive biases and/or altered dopamine neurotransmission, a process that has been termed "sensitization".[99] Specific social experiences have been linked to specific psychological mechanisms and psychotic experiences in schizophrenia. In addition, structural neuroimaging studies of victims of sexual abuse and other traumas have sometimes reported findings similar to those sometimes found in psychotic patients, such as thinning of the corpus callosum, loss of volume in the anterior cingulate cortex, and reduced hippocampal volume.[100]
Urbanicity
A particularly stable and replicable finding has been the association between living in an urban environment and the development of schizophrenia, even after factors such as drug use, ethnic group and size of social group have been controlled for.[101] A recent study of 4.4 million men and women in Sweden found an 68%–77% increased risk of diagnosed psychosis for people living in the most urbanized environments, a significant proportion of which is likely to be described as schizophrenia.[102] The effect does not appear to be due to a higher incidence of obstetric complications in urban environments.[103] The risk increases with the number of years and degree of urban living in childhood and adolescence, suggesting that constant, cumulative, or repeated exposures during upbringing occurring more frequently in urbanized areas are responsible for the association.[104] Various possible explanations for the effect have been judged unlikely based on the nature of the findings, including infectious causes or a generic stress effect. It is thought to interact with genetic dispositions and, since there appears to be nonrandom variation even across different neighborhoods, and an independent association with social isolation, it has been proposed that the degree of "social capital" (e.g. degree of mutual trust, bonding and safety in neighborhoods) can exert a developmental impact on children growing up in these environments.[105]
Close relationships
Evidence is consistent that negative attitudes from others increase the risk of schizophrenia relapse, in particular critical comments, hostility, authoritarian, and intrusive or controlling attitudes (termed 'high expressed emotion' by researchers).[106] Although family members and significant others are not held responsible for schizophrenia - the attitudes, behaviors and interactions of all parties are addressed - unsupportive dysfunctional relationships may also contribute to an increased risk of developing schizophrenia.[107][108]
Neural processes
Structural
Studies have tended to show various subtle average differences in the volume of certain areas of brain structure between people with and without diagnoses of schizophrenia, although it has become increasingly clear that there is no single pathological neuropsychological or structural neuroanatomic profile, due partly to heterogeneity within the disorder.[109] The most consistent volumetric findings are (first-onset patient vs control group averages), slightly less grey matter volume and slightly increased ventricular volume in certain areas of the brain. The two findings are thought to be linked. Although the differences are found in first-episode cases, grey matter volumes are partly a result of life experiences, drugs and malnutrition etc., so the exact role in the disorder is unclear.[110] In addition, ventricle volumes are amongst the mostly highly variable and environmentally-influenced aspects of brain structure, and the percentage difference in group averages in schizophrenia studies has been described as "not a very profound difference in the context of normal variation."[111] A slightly smaller than average whole-brain volume has also been also been found, and slightly smaller hippocampal volume in terms of group averages. These differences may be present from birth or develop later, and there is substantial variation between individuals.[110]
Most schizophrenia studies have found average reduced volume of the left medial temporal lobe and left superior temporal gyrus, and half of studies have revealed deficits in certain areas of the frontal gyrus, parahippocampal gyrus and temporal gyrus.[112] However, at variance with some findings in individuals with chronic schizophrenia (where use of antipsychotics and other factors may have a confounding effect), significant group differences of temporal lobe and amygdala volumes are not shown in first-episode patients on average.[113] The neurobiological abnormalities are so varied that no single abnormality is observed across the entire group of people with DSM-IV–defined schizophrenia. In addition, it remains unclear whether the structural differences are unique to schizophrenia or cut across the traditional diagnostic boundaries between schizophrenia and affective disorders - though perhaps being unique to conditions with psychotic features.[114]
Studies of the rare childhood-onset schizophrenia (before age 13) indicate a greater-than-normal loss of grey matter over several years, progressing from the back of the brain to the front, levelling out in early adulthood. Such a pattern of "pruning" occurs as part of normal brain development but appears to be exaggerated in childhood-onset psychotic diagnoses, particularly schizophrenia. Abnormalities in the volume of the ventricles or frontal lobes have also been found in several studies but not in others. Volume changes are most likely glial and vascular rather than purely neuronal, and reduction in grey matter may primarily reflect a reduction of neuropil rather than a deficit in the total number of neurons. Other studies, especially some computational studies, have shown that a reduction in the number of neurons can cause psychotic symptoms.[115] Studies to date have been based on small numbers of the most severe and treatment-resistant patients taking antipsychotics.[116]
Functional
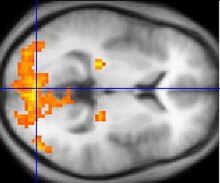
Some studies using neuropsychological tests and brain imaging technologies such as fMRI and PET to examine functional differences in brain activity have shown that differences seem to most commonly occur in the frontal lobes, hippocampus, and temporal lobes.[117] Abnormalities of the kind shown are linked to the same neurocognitive deficits often associated with schizophrenia, particularly in areas of memory,[118] attention, problem solving, executive function, and social cognition.[citation needed] Observations of the frontal lobe in patients with schizophrenia are inconsistent: While many studies have found abnormalities, others have found no[119] or only a statistically insignificant[120] difference. Data from a PET study[121] suggests that the less the frontal lobes are activated during a working memory task, the greater the increase in abnormal dopamine activity in the striatum, thought to be related to the neurocognitive deficits in schizophrenia.
Electroencephalograph (EEG) recordings of persons with schizophrenia performing perception oriented tasks showed an absence of gamma band activity in the brain, indicating weak integration of critical neural networks in the brain.[122] Those who experienced intense hallucinations, delusions and disorganized thinking showed the lowest frequency synchronization. None of the drugs taken by the persons scanned had moved neural synchrony back into the gamma frequency range. Gamma band and working memory alterations may be related to alterations in interneurons that produce the neurotransmitter GABA.
Atypical connectivity in the default network and other resting-state networks in the brain has been observed in schizophrenic patients. The greater connectivity in the default network and the task-positive network may reflect excessive orientation of attention to introspection and to extrospection, respectively, and the greater anti-correlation between the two networks suggests excessive rivalry between the networks. Increased deactivation of specific default-network regions is associated with the positive symptoms of schizophrenia.[123]
Dopamine

Particular focus has been placed upon the function of dopamine in the mesolimbic pathway of the brain. This focus largely resulted from the accidental finding that a drug group which blocks dopamine function, known as the phenothiazines, could reduce psychotic symptoms. An influential theory, known as the "dopamine hypothesis of schizophrenia", proposed that a malfunction involving dopamine pathways was therefore the cause of (the positive symptoms of) schizophrenia. Evidence for this theory includes[126] findings that the potency of many antipsychotics is correlated with their affinity to dopamine D2 receptors;[127] and the exacerbatory effects of a dopamine agonist (amphetamine) and a dopamine beta hydroxylase inhibitor (disulfiram) on schizophrenia;[128][129] and post-mortem studies initially suggested increased density of dopamine D2 receptors in the striatum[1]. Such high levels of D[2] receptors intensify brain signals in schizophrenia and causes positive symptoms such as hallucinations and paranoia. Impaired glutamate (a neurotransmitter which directs neuron to pass along an impulse) activity appears to be another source of schizophrenia symptoms.[130]
However, there was controversy and conflicting findings over whether post-mortem findings resulted from chronic antipsychotic treatment. Compared to the success of postmortem studies in finding profound changes of dopamine receptors, imaging studies using SPET and PET methods in drug naive patients have generally failed to find any difference in dopamine D2 receptor density compared to controls. Comparable findings in longitudinal studies show: " Particular emphasis is given to methodological limitations in the existing literature, including lack of reliability data, clinical heterogeneity among studies, and inadequate study designs and statistic," suggestions are made for improving future longitudinal neuroimaging studies of treatment effects in schizophrenia[131] A recent review of imaging studies in schizophrenia shows confidence in the techniques, while disussing such operator error.[132] In 2007 one report said, "During the last decade, results of brain imaging studies by use of PET and SPET in schizophrenic patients showed a clear dysregulation of the dopaminergic system." [133]
Recent findings from meta-analyses suggest that there may be a small elevation in dopamine D2 receptors in drug-free patients with schizophrenia, but the degree of overlap between patients and controls makes it unlikely that this is clinically meaningful.[134][135] In addition, newer antipsychotic medication (called atypical antipsychotic medication) can be as potent as older medication (called typical antipsychotic medication) while also affecting serotonin function and having somewhat less of a dopamine blocking effect. In addition, dopamine pathway dysfunction has not been reliably shown to correlate with symptom onset or severity. HVA levels correlate trendwise to symptoms severity. During the application of debrisoquin this correlation becomes significant[136]
Giving a more precise explanation of this discrepancy in d2 receptor radioligand imaging measurements involves the monomer and dimer ratio, Dr Philip Seeman has said: "In schizophrenia, therefore, the density of [11C]methylspiperone sites rises, reflecting an increase in monomers, while the density of [11C]raclopride sites remains the same, indicating that the total population of D2 monomers and dimers does not change."[2]. With this difference in measurement technique in mind; the above mentioned meta analysis uses results from 10 different ligands[137].
It has been said that, "...Numerous postmortem studies have consistently revealed D2 receptors to be elevated in the striata of patients with schizophrenia"[138]. However, the authors were concerned the effect of medication may not have been fully accounted for. The study introduced an experiment by Abi-Dargham et al.[139] in which it was shown medication free live schizophrenics had more d2 receptors involved in the schizophrenic process and more dopamine. Since then another study has shown such elevated percentages in d2 receptors is brain-wide (using a different ligand, which did not need dopamine depletion)[140][141] In a 2009 study Annisa Abi-Dagham et al. confirmed the findings of her previous study regarding increased baseline d2 receptors in schizophrenics and showing a correlation between this magnitude and the result of amphetamine stimulation experiments.[142]
Even in 1986 the effect of antipsychotics on receptor measurement was controversial. An article in Science sought to clarify whether the increase was solely due to medication by using drug naive schizophrenics: "The finding that D2 dopamine receptors are substantially increased in schizophrenic patients who have never been treated with neuroleptic drugs raises the possibility that dopamine receptors are involved in the schizophrenic disease process itself. Alternatively, the increased D2 receptor number may reflect presynaptic factors such as increased endogenous dopamine levels (16). In either case, our findings support the hypothesis that dopamine receptor abnormalities are present in untreated schizophrenic patients." [143] (The experiment used 3-N-[11C]methylspiperone- the same as mentioned by Dr Seeman detects d2 monomers and binding was double that of controls.)
It is still thought that dopamine mesolimbic pathways may be hyperactive, resulting in hyperstimulation of D2 receptors and positive symptoms. There is also growing evidence that, conversely, mesocortical pathway dopamine projections to the prefrontal cortex might be hypoactive (underactive), resulting in hypostimulation of D1 receptors, which may be related to negative symptoms and cognitive impairment. The overactivity and underactivity in these different regions may be linked, and may not be due to a primary dysfunction of dopamine systems but to more general neurodevelopmental issues that precede them.[144] Increased dopamine sensitivity may be a common final pathway.[145]
Another reliable finding, repeatedly found, is that there is a some sixfold excess of binding sites insensitive to a certain testing agent (raclopride)[146][147] Dr Seeman later said this increase was probably due to the increase in d2 monomers. [3] Such an increase in monomers, occurs via the cooperativity mechanism[148] which is responsible for d2high and d2low, the supersensitive and lowsensitivity states of the d2 dopamine receptor[149]. More specifically, "an increase in monomers, may be one basis for dopamine supersensitivity." [150]
Another one of Philip Seeman's findings was that the dopamine D2 receptor protein looked abnormal in schizophrenia. Proteins change states by flexing. The activating of the protein by folding could be permanent or fluctuating,[151] just like the courses of patients' illnesses waxes and wanes. Increased folding of a protein leads to increased risk of 'additional fragments' forming[152] The schizophrenic d2 receptor has a unique additional fragment when digested by papain in the test-tube, but none of the controls exhibited the same fragment.[151] The D2 receptor in schizophrenia are thus in a highly active state as found by Philip Seeman et al.[145]
Glutamate
Interest has also focused on the neurotransmitter glutamate and the reduced function of the NMDA glutamate receptor in schizophrenia. This has largely been suggested by abnormally low levels of glutamate receptors found in postmortem brains of people previously diagnosed with schizophrenia[153] and the discovery that the glutamate blocking drugs such as phencyclidine and ketamine can mimic the symptoms and cognitive problems associated with the condition.[154] The fact that reduced glutamate function is linked to poor performance on tests requiring frontal lobe and hippocampal function and that glutamate can affect dopamine function, all of which have been implicated in schizophrenia, have suggested an important mediating (and possibly causal) role of glutamate pathways in schizophrenia.[155] Further support of this theory has come from preliminary trials suggesting the efficacy of coagonists at the NMDA receptor complex in reducing some of the positive symptoms of schizophrenia.[156]
Other
Dyregulation of neural calcium homeostasis has been hypothesized to be a link between the glutamate and dopaminergic abnormalities[157] and some small studies have indicated that calcium channel blocking agents can lead to improvements on some measures in schizophrenia with tardive dyskinesia.[158]
There is evidence of irregular cellular metabolism and oxidative stress in the prefrontal cortex in schizophrenia, involving increased glucose demand and/or cellular hypoxia.[159]
Mutations in the gene for brain-derived neurotrophic factor (BDNF) have been reported to be a risk factor for the disease.[160]
Other proposed etiologies
Psychiatrists R. D. Laing, Silvano Arieti, Theodore Lidz and others have argued that the symptoms of what is called mental illness are comprehensible reactions to impossible demands that society and particularly family life places on some sensitive individuals. Laing, Arieti and Lidz were notable in valuing the content of psychotic experience as worthy of interpretation, rather than considering it simply as a secondary and essentially meaningless marker of underlying psychological or neurological distress. Laing described eleven case studies of people diagnosed with schizophrenia and argued that the content of their actions and statements was meaningful and logical in the context of their family and life situations.[161] In 1956, Palo Alto, Gregory Bateson and his colleagues Paul Watzlawick, Donald Jackson, and Jay Haley[162] articulated a theory of schizophrenia, related to Laing's work, as stemming from double bind situations where a person receives different or contradictory messages. Madness was therefore an expression of this distress and should be valued as a cathartic and transformative experience. In the books Schizophrenia and the Family and The Origin and Treatment of Schizophrenic Disorders Lidz and his colleagues explain their belief that parental behaviour can result in mental illness in children. Arieti's Interpretation of Schizophrenia won the 1975 scientific National Book Award in the United States.
The concept of schizophrenia as a result of civilization has been developed further by psychologist Julian Jaynes in his 1976 book The Origin of Consciousness in the Breakdown of the Bicameral Mind; he proposed that until the beginning of historic times, schizophrenia or a similar condition was the normal state of human consciousness.[163] This would take the form of a "bicameral mind" where a normal state of low affect, suitable for routine activities, would be interrupted in moments of crisis by "mysterious voices" giving instructions, which early people characterized as interventions from the gods. Researchers into shamanism have speculated that in some cultures schizophrenia or related conditions may predispose an individual to becoming a shaman;[164] the experience of having access to multiple realities is not uncommon in schizophrenia, and is a core experience in many shamanic traditions. Equally, the shaman may have the skill to bring on and direct some of the altered states of consciousness psychiatrists label as illness. Psychohistorians, on the other hand, accept the psychiatric diagnoses. However, unlike the current medical model of mental disorders they may argue that poor parenting in tribal societies causes the shaman's schizoid personalities.[165] Commentators such as Paul Kurtz and others have endorsed the idea that major religious figures experienced psychosis, heard voices and displayed delusions of grandeur.[166]
Evolutionary explanations
Psychiatrist Tim Crow has argued that schizophrenia may be the evolutionary price we pay for a left brain hemisphere specialization for language.[167] Since psychosis is associated with greater levels of right brain hemisphere activation and a reduction in the usual left brain hemisphere dominance, our language abilities may have evolved at the cost of causing schizophrenia when this system breaks down. Other approaches have linked schizophrenia to psychological dissociation[168] or states of awareness and identity understood from phenomenological and other perspectives.[169][170]
References
- ^ Zubin J, Spring B (1977). "Vulnerability--a new view of schizophrenia". J Abnorm Psychol. 86 (2): 103–26. doi:10.1037/0021-843X.86.2.103. PMID 858828.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Age of menarche and schizophrenia onset in women Schizophrenia Research, Volume 69, Issues 2-3, 1 August 2004, Pages 183-188 Karen M. Hochman, Richard R. Lewine
- ^ a b Harrison PJ, Owen MJ (2003). "Genes for schizophrenia? Recent findings and their pathophysiological implications". Lancet. 361 (9355): 417–9. doi:10.1016/S0140-6736(03)12379-3. PMID 12573388.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ a b Owen MJ, Craddock N, O'Donovan MC (2005). "Schizophrenia: genes at last?". Trends Genet. 21 (9): 518–25. doi:10.1016/j.tig.2005.06.011. PMID 16009449.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ a b c Riley B, Kendler KS (2006). "Molecular genetic studies of schizophrenia". Eur J Hum Genet. 14 (6): 669–80. doi:10.1038/sj.ejhg.5201571. PMID 16721403.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Koskenvuo M, Langinvainio H, Kaprio J, Lönnqvist J, Tienari P (1984). "Psychiatric hospitalization in twins". Acta Genet Med Gemellol (Roma). 33 (2): 321–32. PMID 6540965.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Hoeffer A, Pollin W (1970). "Schizophrenia in the NAS-NRC panel of 15,909 veteran twin pairs". Arch Gen Psychiatry. 23 (5): 469–77. PMID 5478575.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ WILLIAM POLLIN M.D., MARTIN G. ALLEN M.D., AXEL HOFFER M.D., JAMES R. STABENAU M.D., , and ZDENEK HRUBEC D.SC.Psychopathology in 15,909 Pairs of Veteran Twins: Evidence for a Genetic Factor in the Pathogenesis of Schizophrenia and Its Relative Absence in Psychoneurosis Am J Psychiatry 126:597-610, November 1969 doi: 10.1176/appi.ajp.126.5.597
- ^ Molecular Psychiatry November 2001, Volume 6, Number 6, Pages 634-646 Schizophrenia and viral infection during neurodevelopment: a focus on mechanisms B D Pearce
- ^ http://en.wikipedia.org/wiki/Twin#Monochorionic
- ^ Schizophr Bull. 1995;21(3):357-66. Prenatal development of monozygotic twins and concordance for schizophrenia. Davis JO, Phelps JA, Bracha HS. Erratum in: Schizophr Bull 1995;21(4):539. http://www.ncbi.nlm.nih.gov/pubmed/7481567 . (The erratum was needed to substantiate the percentages quoted)
- ^ Maher, Brendan; "The case of the missing hereditability"; NEWS FEATURE PERSONAL GENOMES NATURE|Vol 456|6 November 2008 p21
- ^ "Getting crowded on chromosome 11q22—make way for phosphohippolin". Schizophrenia Research Forum. 14 March 2007. Retrieved 2007-05-16.
- ^ Choudhury K, McQuillin A, Puri V; et al. (2007). "A genetic association study of chromosome 11q22-24 in two different samples implicates the FXYD6 gene, encoding phosphohippolin, in susceptibility to schizophrenia". Am J Hum Genet. 80 (4): 664–72. doi:10.1086/513475. PMC 1852702. PMID 17357072.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Ito Y, Nakamura Y, Takahashi N; et al. (2008). "A genetic association study of the FXYD domain containing ion transport regulator 6 (FXYD6) gene, encoding phosphohippolin, in susceptibility to schizophrenia in a Japanese population". Neurosci. Lett. 438 (1): 70–5. doi:10.1016/j.neulet.2008.04.010. PMID 18455306.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Shifman S, Johannesson M, Bronstein M, Chen SX, Collier DA, Craddock NJ, Kendler KS, Li T, O'Donovan M, O'Neill FA, Owen MJ, Walsh D, Weinberger DR, Sun C, Flint J, Darvasi A (2008). "Genome-Wide Association Identifies a Common Variant in the Reelin Gene That Increases the Risk of Schizophrenia Only in Women". PLoS Genetics. 4 (2): e28. doi:10.1371/journal.pgen.0040028. PMID 18282107.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - ^
- Sanders AR, Duan J, Levinson DF, Shi J, He D, Hou C; et al. (2008). "No significant association of 14 candidate genes with schizophrenia in a large European ancestry sample: implications for psychiatric genetics". American Journal of Psychiatry. 165 (4): 497–506. doi:10.1176/appi.ajp.2007.07101573. PMID 18198266.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Hamilton SP (2008). "Schizophrenia candidate genes: are we really coming up blank?". American Journal of Psychiatry. 165 (4): 420–3. doi:10.1176/appi.ajp.2008.08020218. PMID 18381911.
{{cite journal}}: Unknown parameter|month=ignored (help)
- Sanders AR, Duan J, Levinson DF, Shi J, He D, Hou C; et al. (2008). "No significant association of 14 candidate genes with schizophrenia in a large European ancestry sample: implications for psychiatric genetics". American Journal of Psychiatry. 165 (4): 497–506. doi:10.1176/appi.ajp.2007.07101573. PMID 18198266.
- ^ Allen NC, Bagade S, McQueen MB, Ioannidis JPA, Kawoura FK, Khoury MJ, Tanzi RE, Bertram L (2008). "Systematic meta-analyses and field synopsis of genetic association studies in schizophrenia: the SzGene database". Nature Genetics. 40 (7): 827–824. doi:10.1038/ng.171. PMID 18583979.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Walsh T (2008). "Rare structural variants disrupt multiple genes in neurodevelopmental pathways in schizophrenia". Science. 320 (5875): 539–43. doi:10.1126/science.1155174. PMID 18369103.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ^ Xu B, Roos JL, Levy S, van Rensburg EJ, Gogos JA, Karayiorgou M (2008). "Strong association of de novo copy number mutations with sporadic schizophrenia". Nat Genet. 40 (7): 880–5. doi:10.1038/ng.162. PMID 18511947.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ The International Schizophrenia Consortium (11 September 2008). "Rare chromosomal deletions and duplications increase risk of schizophrenia". Nature. 455 (7210): 237–41. doi:10.1038/nature07239. PMID 18668038.
- ^ Lee JA, Lupski JR (2006). "Genomic rearrangements and gene copy-number alterations as a cause of nervous system disorders". Neuron. 52: 103–121. doi:10.1016/j.neuron.2006.09.027. PMID 17015230.
- ^ Kalmady, Sunil V; Ganesan Venkatasubramanian (2009). "Evidence for positive selection on Protocadherin Y gene in Homo sapiens: Implications for schizophrenia". Schizophrenia Research. 108: 299. doi:10.1016/j.schres.2008.09.015.
{{cite journal}}: More than one of|author1=and|author=specified (help) - ^ Barros CS, Calabrese B, Chamero P, Roberts AJ, Korzus E, Lloyd K, Stowers L, Mayford M, Halpain S, Müller U (17 March 2009). "Impaired maturation of dendritic spines without disorganization of cortical cell layers in mice lacking NRG1/ErbB signaling in the central nervous system". Proc Natl Acad Sci U S A. 106 (11): 4507–12. doi:10.1073/pnas.0900355106. PMID 19240213.
{{cite journal}}: Unknown parameter|laysummary=ignored (help)CS1 maint: multiple names: authors list (link) - ^ a b c
Clarke MC, Harley M, Cannon M (2006). "The role of obstetric events in schizophrenia". Schizophr Bull. 32 (1): 3–8. doi:10.1093/schbul/sbj028. PMID 16306181.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Davies G, Welham J, Chant D, Torrey EF, McGrath J (2003). "A systematic review and meta-analysis of Northern Hemisphere season of birth studies in schizophrenia". Schizophr Bull. 29 (3): 587–93. PMID 14609251.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Gobet F, Chassy P (2008). "Season of birth and chess expertise" (PDF). J Biosoc Sci. 40 (2): 313–6. doi:10.1017/S0021932007002222. PMID 18335581.
{{cite journal}}: Unknown parameter|month=ignored (help)PDF (65.8 KiB) - ^ Susser E, Neugebauer R, Hoek HW; et al. (1996). "Schizophrenia after prenatal famine. Further evidence". Arch. Gen. Psychiatry. 53 (1): 25–31. PMID 8540774.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Huttunen MO, Niskanen P (1978). "Prenatal loss of father and psychiatric disorders". Arch. Gen. Psychiatry. 35 (4): 429–31. PMID 727894.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ a b Welham J, Isohanni M, Jones P, McGrath J (2008). "The Antecedents of Schizophrenia: A Review of Birth Cohort Studies". Schizophr Bull. 35: 603. doi:10.1093/schbul/sbn084. PMID 18658128.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Mallard EC, Rehn A, Rees S, Tolcos M, Copolov D (1999). "Ventriculomegaly and reduced hippocampal volume following intrauterine growth-restriction: implications for the aetiology of schizophrenia". Schizophr. Res. 40 (1): 11–21. doi:10.1016/S0920-9964(99)00041-9. PMID 10541002.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Handford HA (1975). "Brain hypoxia, minimal brain dysfunction, and schizophrenia". Am J Psychiatry. 132 (2): 192–4. PMID 1111324.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ The above reference is cited in a 2006 work, in giving a history of minimal brain dysfunction saying: "It was also noted that individuals who experienced perinatal brain hypoxia constituted a population at risk for minimal brain dysfunction, and that children attending psychiatric clinics often presented with illnesses or perinatal complications of a sort known to be associated with neurological brain damage (Handford 1975)."Disorganized Children : A Guide for Parents and Professionals Jessica Kingsley Publishers Ltd. Stein, Samuel M.p135
- ^ Van Erp TG, Saleh PA, Rosso IM; et al. (2002). "Contributions of genetic risk and fetal hypoxia to hippocampal volume in patients with schizophrenia or schizoaffective disorder, their unaffected siblings, and healthy unrelated volunteers". The American journal of psychiatry. 159 (9): 1514–20. doi:10.1176/appi.ajp.159.9.1514. PMID 12202271.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Schmidt-Kastner R, van Os J, W M Steinbusch H, Schmitz C (2006). "Gene regulation by hypoxia and the neurodevelopmental origin of schizophrenia". Schizophrenia research. 84 (2–3): 253–71. doi:10.1016/j.schres.2006.02.022. PMID 16632332.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ a b Cannon M, Caspi A, Moffitt TE; et al. (2002). "Evidence for early-childhood, pan-developmental impairment specific to schizophreniform disorder: results from a longitudinal birth cohort". Arch. Gen. Psychiatry. 59 (5): 449–56. doi:10.1001/archpsyc.59.5.449. PMID 11982449.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ a b Rosso IM, Bearden CE, Hollister JM; et al. (2000). "Childhood neuromotor dysfunction in schizophrenia patients and their unaffected siblings: a prospective cohort study". Schizophr Bull. 26 (2): 367–78. PMID 10885637.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Kunugi H, Urushibara T, Murray RM, Nanko S, Hirose T (2003). "Prenatal underdevelopment and schizophrenia: a case report of monozygotic twins". Psychiatry Clin. Neurosci. 57 (3): 271–4. doi:10.1046/j.1440-1819.2003.01116.x. PMID 12753566.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Murray RM, Fearon P (1999). "The developmental 'risk factor' model of schizophrenia". J Psychiatr Res. 33 (6): 497–9. doi:10.1016/S0022-3956(99)00032-1. PMID 10628525.
- ^ Cannon M, Murray RM (1998). "Neonatal origins of schizophrenia". Arch. Dis. Child. 78 (1): 1–3. doi:10.1136/adc.78.1.1. PMC 1717442. PMID 9534666.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Golan H, Huleihel M (2006). "The effect of prenatal hypoxia on brain development: short- and long-term consequences demonstrated in rodent models". Developmental science. 9 (4): 338–49. doi:10.1111/j.1467-7687.2006.00498.x. PMID 16764607.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Golan H, Kashtutsky I, Hallak M, Sorokin Y, Huleihel M (2004). "Maternal hypoxia during pregnancy delays the development of motor reflexes in newborn mice". Developmental neuroscience. 26 (1): 24–9. doi:10.1159/000080708. PMID 15509895.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Ellman, LM and Cannon TD, "Chapter 7. Environmental pre- and preinatal influences in etiology" in Clinical Handbook of Schizophrenia by Kim T. Mueser, Dilip V. Jeste New York : Guilford Press, ©2008 p69
- ^ Zornberg GL, Buka SL, Tsuang MT (2000). "Hypoxic-ischemia-related fetal/neonatal complications and risk of schizophrenia and other nonaffective psychoses: a 19-year longitudinal study". The American journal of psychiatry. 157 (2): 196–202. doi:10.1176/appi.ajp.157.2.196. PMID 10671387.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Torrey EF, Buka S, Cannon TD, Goldstein JM, Seidman LJ, Liu T, Hadley T, Rosso IM, Bearden C, Yolken RH (2009). "Paternal age as a risk factor for schizophrenia: how important is it?". Schizophr Res. 114 (1–3): 1–5. doi:10.1016/j.schres.2009.06.017. PMID 19683417.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Brown AS (2008). "The risk for schizophrenia from childhood and adult infections". The American journal of psychiatry. 165 (1): 7–10. doi:10.1176/appi.ajp.2007.07101637. PMID 18178749.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Torrey EF, Miller J, Rawlings R, Yolken RH (1997). "Seasonality of births in schizophrenia and bipolar disorder: a review of the literature". Schizophrenia research. 28 (1): 1–38. doi:10.1016/S0920-9964(97)00092-3. PMID 9428062.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Mednick SA, Machon RA, Huttunen MO, Bonett D (1988). "Adult schizophrenia following prenatal exposure to an influenza epidemic". Archives of general psychiatry. 45 (2): 189–92. PMID 3337616.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Cooper SJ (1992). "Schizophrenia after prenatal exposure to 1957 A2 influenza epidemic". The British journal of psychiatry. 161: 394–6. doi:10.1192/bjp.161.3.394. PMID 1393310.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Erlenmeyer-Kimling L, Folnegović Z, Hrabak-Zerjavić V, Borcić B, Folnegović-Smalc V, Susser E (1994). "Schizophrenia and prenatal exposure to the 1957 A2 influenza epidemic in Croatia". The American journal of psychiatry. 151 (10): 1496–8. PMID 8092342.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Mino Y, Oshima I, Tsuda T, Okagami K (2000). "No relationship between schizophrenic birth and influenza epidemics in Japan". J Psychiatr Res. 34 (2): 133–8. doi:10.1016/S0022-3956(00)00003-0. PMID 10758255.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Mortensen PB, Nørgaard-Pedersen B, Waltoft BL, Sørensen TL, Hougaard D, Yolken RH (2007). "Early infections of Toxoplasma gondii and the later development of schizophrenia". Schizophr Bull. 33 (3): 741–4. doi:10.1093/schbul/sbm009. PMID 17329231.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Torrey EF, Yolken RH (2003). "Toxoplasma gondii and schizophrenia". Emerging Infect. Dis. 9 (11): 1375–80. PMID 14725265.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Torrey EF, Bartko JJ, Lun ZR, Yolken RH (2007). "Antibodies to Toxoplasma gondii in patients with schizophrenia: a meta-analysis". Schizophr Bull. 33 (3): 729–36. doi:10.1093/schbul/sbl050. PMID 17085743.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Wang HL, Wang GH, Li QY, Shu C, Jiang MS, Guo Y (2006). "Prevalence of Toxoplasma infection in first-episode schizophrenia and comparison between Toxoplasma-seropositive and Toxoplasma-seronegative schizophrenia". Acta Psychiatr Scand. 114 (1): 40–8. doi:10.1111/j.1600-0447.2006.00780.x. PMID 16774660.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Conejero-Goldberg C, Torrey EF, Yolken RH (2003). "Herpesviruses and Toxoplasma gondii in orbital frontal cortex of psychiatric patients". Schizophr. Res. 60 (1): 65–9. doi:10.1016/S0920-9964(02)00160-3. PMID 12505139.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Eaton WW, Byrne M, Ewald H; et al. (2006). "Association of schizophrenia and autoimmune diseases: linkage of Danish national registers". Am J Psychiatry. 163 (3): 521–8. doi:10.1176/appi.ajp.163.3.521. PMID 16513876.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Jones AL, Mowry BJ, Pender MP, Greer JM (2005). "Immune dysregulation and self-reactivity in schizophrenia: do some cases of schizophrenia have an autoimmune basis?". Immunol. Cell Biol. 83 (1): 9–17. doi:10.1111/j.1440-1711.2005.01305.x. PMID 15661036.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Strous RD, Shoenfeld Y (2006). "Schizophrenia, autoimmunity and immune system dysregulation: a comprehensive model updated and revisited". J. Autoimmun. 27 (2): 71–80. doi:10.1016/j.jaut.2006.07.006. PMID 16997531.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Jones P, Rodgers B, Murray R, Marmot M (1994). "Child development risk factors for adult schizophrenia in the British 1946 birth cohort". Lancet. 344 (8934): 1398–402. doi:10.1016/S0140-6736(94)90569-X. PMID 7968076.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Isohanni M, Jones PB, Moilanen K; et al. (2001). "Early developmental milestones in adult schizophrenia and other psychoses. A 31-year follow-up of the Northern Finland 1966 Birth Cohort". Schizophr. Res. 52 (1–2): 1–19. doi:10.1016/S0920-9964(00)00179-1. PMID 11595387.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Isohanni M, Murray GK, Jokelainen J, Croudace T, Jones PB (2004). "The persistence of developmental markers in childhood and adolescence and risk for schizophrenic psychoses in adult life. A 34-year follow-up of the Northern Finland 1966 birth cohort". Schizophr. Res. 71 (2–3): 213–25. doi:10.1016/j.schres.2004.03.008. PMID 15474893.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Cannon M, Jones P, Huttunen MO, Tanskanen A, Murray R (1999). "Motor Co-ordination Deficits as Predictors of Schizophrenia Among Finnish School Children". Hum. Psychopharmacol. Clin. Exp. 14 (7): 491–7. doi:10.1002/(SICI)1099-1077(199910)14:7<491::AID-HUP134>3.0.CO;2-V.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ School Performance in Finnish Children and Later Development of Schizophrenia A Population-Based Longitudinal Study Mary Cannon, MD, MSc; Peter Jones, MD, PhD; Matti O. Huttunen, MD, PhD; Antti Tanskanen, BSc; Tiia Huttunen, MSc; Sophia Rabe-Hesketh, PhD; Robin M. Murray, MD, DSc Arch Gen Psychiatry. 1999;56:457-463. http://archpsyc.ama-assn.org/cgi/content/abstract/56/5/457
- ^ Isohanni, M., Isohanni, I., Nieminen, P., Jokelainen, J. and Järvelin, M.-R., 2000. School predictors of schizophrenia. Letter to the editor. Arch. Gen. Psychiatry 57, p. 813.
- ^ I. Helling, A. Öhman, C. M. Hultman School achievements and schizophrenia: a case–control study Acta Psychiatrica Scandinavica Volume 108 Issue 5, Pages 381 - 386
- ^ Hans SL, Marcus J, Nuechterlein KH, Asarnow RF, Styr B, Auerbach JG (1999). "Neurobehavioral deficits at adolescence in children at risk for schizophrenia: The Jerusalem Infant Development Study". Arch. Gen. Psychiatry. 56 (8): 741–8. doi:10.1001/archpsyc.56.8.741. PMID 10435609.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Carter JW, Schulsinger F, Parnas J, Cannon T, Mednick SA (2002). "A multivariate prediction model of schizophrenia". Schizophr Bull. 28 (4): 649–82. PMID 12795497.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Hans SL, Auerbach JG, Asarnow JR, Styr B, Marcus J (2000). "Social adjustment of adolescents at risk for schizophrenia: the Jerusalem Infant Development Study". J Am Acad Child Adolesc Psychiatry. 39 (11): 1406–14. doi:10.1097/00004583-200011000-00015. PMID 11068896.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Dworkin RH, Bernstein G, Kaplansky LM; et al. (1991). "Social competence and positive and negative symptoms: a longitudinal study of children and adolescents at risk for schizophrenia and affective disorder". Am J Psychiatry. 148 (9): 1182–8. PMID 1882996.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Galderisi S, Maj M, Mucci A, Cassano GB, Invernizzi G, Rossi A, Vita A, Dell'Osso L, Daneluzzo E, Pini S. (2002) Historical, psychopathological, neurological, and neuropsychological aspects of deficit schizophrenia: a multicenter study Am J Psychiatry. 2002 Jun;159(6):983-90.
- ^ Swartz MS, Wagner HR, Swanson JW; et al. (2006). "Substance use in persons with schizophrenia: baseline prevalence and correlates from the NIMH CATIE study". J. Nerv. Ment. Dis. 194 (3): 164–72. doi:10.1097/01.nmd.0000202575.79453.6e. PMID 16534433.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Proc Natl Acad Sci U S A. 1996 Aug 20;93(17):9235-40.Single photon emission computerized tomography imaging of amphetamine-induced dopamine release in drug-free schizophrenic subjects.Laruelle M, Abi-Dargham A, van Dyck CH, Gil R, D'Souza CD, Erdos J, McCance E, Rosenblatt W, Fingado C, Zoghbi SS, Baldwin RM, Seibyl JP, Krystal JH, Charney DS, Innis RB.
- ^ Mueser KT, Yarnold PR, Levinson DF; et al. (1990). "Prevalence of substance abuse in schizophrenia: demographic and clinical correlates". Schizophr Bull. 16 (1): 31–56. PMID 2333480.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Arseneault L, Cannon M, Witton J, Murray RM (2004). "Causal association between cannabis and psychosis: examination of the evidence". Br J Psychiatry. 184: 110–7. doi:10.1192/bjp.184.2.110. PMID 14754822.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Andréasson S, Allebeck P, Engström A, Rydberg U (1987). "Cannabis and schizophrenia. A longitudinal study of Swedish conscripts". Lancet. 2 (8574): 1483–6. doi:10.1016/S0140-6736(87)92620-1. PMID 2892048.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ "Interpreting hazy warnings about pot and mental illness". Huffington Post. 2007-08-07. Retrieved 2009-01-23.
- ^ McNeill, Ann (2001). "Smoking and mental health — a review of the literature" (PDF). SmokeFree London Programme. Retrieved 2006-12-14.
{{cite journal}}: Cite journal requires|journal=(help) - ^ Meltzer H, Gill B, Petticrew M, Hinds K. (1995). "OPCS Surveys of Psychiatric Morbidity Report 3: Economic Activity and Social Functioning of Adults With Psychiatric Disorders". London, Her Majesty’s Stationery Office.
{{cite journal}}: Cite journal requires|journal=(help)CS1 maint: multiple names: authors list (link) Available for fee. - ^ Kelly, C (1 November 1999). "Smoking Habits, Current Symptoms, and Premorbid Characteristics of Schizophrenic Patients in Nithsdale, Scotland". The American Journal of Psychiatry. 156 (11). American Psychiatric Association: 1751–1757. PMID 10553739. Retrieved 2006-12-14.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Hughes, JR (1 August 1986). "Prevalence of smoking among psychiatric outpatients". The American Journal of Psychiatry. 143 (8). American Psychiatric Association: 993–997. PMID 3487983. Retrieved 2006-12-14.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ "Conditions in Occupational Therapy: effect on occupational performance." ed. Ruth A. Hansen and Ben Atchison (Baltimore: Lippincott Williams & Williams, 2000), 54–74. ISBN 0-683-30417-8
- ^ Zammit S, Allebeck P, Dalman C, Lundberg I, Hemmingsson T, Lewis G (2003). "Investigating the association between cigarette smoking and schizophrenia in a cohort study". Am J Psychiatry. 160 (12): 2216–21. doi:10.1176/appi.ajp.160.12.2216. PMID 14638593.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ a b Compton, Michael T. (2005-11-16). "Cigarette Smoking in Individuals with Schizophrenia". Medscape Psychiatry & Mental Health. Retrieved 2007-05-17.
- ^ Prasad C, Spahn SA, Ikegami H (1989). "Chronic nicotine use blocks haloperidol-induced increase in striatal D2-dopamine receptor density". Biochem. Biophys. Res. Commun. 159 (1): 48–52. doi:10.1016/0006-291X(89)92402-9. PMID 2522303.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Silvestri S, Negrete JC, Seeman MV, Shammi CM, Seeman P (2004). "Does nicotine affect D2 receptor upregulation? A case-control study". Acta Psychiatr Scand. 109 (4): 313–7, discussion 317–8. doi:10.1111/j.1600-0447.2004.00293.x. PMID 15008806.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Anfang MK, Pope HG (1997). "Treatment of neuroleptic-induced akathisia with nicotine patches". Psychopharmacology (Berl.). 134 (2): 153–6. doi:10.1007/s002130050436. PMID 9399378.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Wicks S, Hjern A, Gunnell D, Lewis G, Dalman C (2005). "Social adversity in childhood and the risk of developing psychosis: a national cohort study". The American journal of psychiatry. 162 (9): 1652–7. doi:10.1176/appi.ajp.162.9.1652. PMID 16135624.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Mueser KT, McGurk SR (2004). "Schizophrenia". The Lancet. 363 (9426): 2063–72. doi:10.1016/S0140-6736(04)16458-1. PMID 15207959.
- ^ Day R, Nielsen JA, Korten A; et al. (1987). "Stressful life events preceding the acute onset of schizophrenia: a cross-national study from the World Health Organization". Cult Med Psychiatry. 11 (2): 123–205. doi:10.1007/BF00122563. PMID 3595169.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Selten JP, Cantor-Graae E, Kahn RS (2007). "Migration and schizophrenia". Current Opinion in Psychiatry. 20 (2): 111–115. doi:10.1097/YCO.0b013e328017f68e. PMID 17278906. Retrieved 2008-07-06.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Cantor-Graae E, Selten JP (2005). "Schizophrenia and migration: a meta-analysis and review". Am J Psychiatry. 162 (1): 12–24. doi:10.1176/appi.ajp.162.1.12. PMID 15625195.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ MacMillan HL, Fleming JE, Streiner DL; et al. (2001). "Childhood abuse and lifetime psychopathology in a community sample". Am J Psychiatry. 158 (11): 1878–83. doi:10.1176/appi.ajp.158.11.1878. PMID 11691695.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Schenkel LS, Spaulding WD, DiLillo D, Silverstein SM (2005). "Histories of childhood maltreatment in schizophrenia: relationships with premorbid functioning, symptomatology, and cognitive deficits". Schizophr. Res. 76 (2–3): 273–86. doi:10.1016/j.schres.2005.03.003. PMID 15949659.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Janssen I, Krabbendam L, Bak M; et al. (2004). "Childhood abuse as a risk factor for psychotic experiences". Acta Psychiatr Scand. 109 (1): 38–45. doi:10.1046/j.0001-690X.2003.00217.x. PMID 14674957.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Read J, Perry BD, Moskowitz A, Connolly J (2001). "The contribution of early traumatic events to schizophrenia in some patients: a traumagenic neurodevelopmental model" (PDF). Psychiatry. 64 (4): 319–45. PMID 11822210.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Read J, van Os J, Morrison AP, Ross CA (2005). "Childhood trauma, psychosis and schizophrenia: a literature review with theoretical and clinical implications". Acta psychiatrica Scandinavica. 112 (5): 330–50. doi:10.1111/j.1600-0447.2005.00634.x. PMID 16223421.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Morgan C, Fisher H (2007). "Environment and schizophrenia: environmental factors in schizophrenia: childhood trauma--a critical review". Schizophrenia bulletin. 33 (1): 3–10. doi:10.1093/schbul/sbl053. PMID 17105965.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Collip D, Myin-Germeys I, Van Os J (2008). "Does the concept of "sensitization" provide a plausible mechanism for the putative link between the environment and schizophrenia?". Schizophr Bull. 34 (2): 220–5. doi:10.1093/schbul/sbm163. PMID 18203757.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Bentall RP, Fernyhough C (2008). "Social Predictors of Psychotic Experiences: Specificity and Psychological Mechanisms". Schizophr Bull. 34: 1012. doi:10.1093/schbul/sbn103. PMID 18703667.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ van Os J (2004). "Does the urban environment cause psychosis?". Br J Psychiatry. 184: 287–8. doi:10.1192/bjp.184.4.287. PMID 15056569.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Sundquist K, Frank G, Sundquist J (2004). "Urbanisation and incidence of psychosis and depression: follow-up study of 4.4 million women and men in Sweden". Br J Psychiatry. 184: 293–8. doi:10.1192/bjp.184.4.293. PMID 15056572.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Eaton WW, Mortensen PB, Frydenberg M (2000). "Obstetric factors, urbanization and psychosis". Schizophr. Res. 43 (2–3): 117–23. doi:10.1016/S0920-9964(99)00152-8. PMID 10858630.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Pedersen CB, Mortensen PB (2001). "Evidence of a dose-response relationship between urbanicity during upbringing and schizophrenia risk". Arch. Gen. Psychiatry. 58 (11): 1039–46. doi:10.1001/archpsyc.58.11.1039. PMID 11695950.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Krabbendam L, van Os J (2005). "Schizophrenia and urbanicity: a major environmental influence—conditional on genetic risk". Schizophr Bull. 31 (4): 795–9. doi:10.1093/schbul/sbi060. PMID 16150958.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Bebbington P, Kuipers L (1994). "The predictive utility of expressed emotion in schizophrenia: an aggregate analysis". Psychol Med. 24 (3): 707–18. PMID 7991753.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Bentall RP (2007). "Prospects for a cognitive-developmental account of psychotic experiences". Br J Clin Psychol. 46 (Pt 2): 155–73. doi:10.1348/014466506X123011. PMID 17524210.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Subotnik, KL (2002). "Are Communication Deviance and Expressed Emotion Related to Family History of Psychiatric Disorders in Schizophrenia?". Schizophrenia Bulletin. 28 (4): 719–29. PMID 12795501.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Flashman LA, Green MF (2004). "Review of cognition and brain structure in schizophrenia: profiles, longitudinal course, and effects of treatment". Psychiatr. Clin. North Am. 27 (1): 1–18, vii. doi:10.1016/S0193-953X(03)00105-9. PMID 15062627.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ a b Steen RG, Mull C, McClure R, Hamer RM, Lieberman JA (2006). "Brain volume in first-episode schizophrenia: systematic review and meta-analysis of magnetic resonance imaging studies". Br J Psychiatry. 188: 510–8. doi:10.1192/bjp.188.6.510. PMID 16738340.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Allen JS, Damasio H, Grabowski TJ (2002). "Normal neuroanatomical variation in the human brain: an MRI-volumetric study". American journal of physical anthropology. 118 (4): 341–58. doi:10.1002/ajpa.10092. PMID 12124914.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Honea R, Crow TJ, Passingham D, Mackay CE (2005). "Regional deficits in brain volume in schizophrenia: a meta-analysis of voxel-based morphometry studies". American Journal of Psychiatry. 162 (12): 2233–45. doi:10.1176/appi.ajp.162.12.2233. PMID 16330585.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Vita A, De Peri L, Silenzi C, Dieci M (2006). "Brain morphology in first-episode schizophrenia: a meta-analysis of quantitative magnetic resonance imaging studies". Schizophrenia Research. 82 (1): 75–88. doi:10.1016/j.schres.2005.11.004. PMID 16377156.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Prasad KM, Keshavan MS (2008). "Structural cerebral variations as useful endophenotypes in schizophrenia: do they help construct "extended endophenotypes"?". Schizophrenia Bulletin. 34 (4): 774–90. doi:10.1093/schbul/sbn017. PMID 18408230.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Hoffman R, McGlashan T (2001). "Neural network models of schizophrenia". Neuroscientist. 7 (5): 441–54. doi:10.1177/107385840100700513. PMID 11597103.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Arango C, Moreno C, Martínez S; et al. (2008). "Longitudinal brain changes in early-onset psychosis". Schizophrenia Bulletin. 34 (2): 341–53. doi:10.1093/schbul/sbm157. PMID 18234701.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Green, Michael (2001). Schizophrenia revealed: from neurons to social interactions. New York: Norton. ISBN 0-393-70334-7.
- ^ Park S, Holzman PS (1992). "Schizophrenics show spatial working memory deficits". Arch. Gen. Psychiatry. 49 (12): 975–82. PMID 1449384.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Wible CG, Shenton ME, Hokama H; et al. (1995). "Prefrontal cortex and schizophrenia. A quantitative magnetic resonance imaging study". Arch. Gen. Psychiatry. 52 (4): 279–88. PMID 7702444.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Selemon LD, Rajkowska G, Goldman-Rakic PS (1998). "Elevated neuronal density in prefrontal area 46 in brains from schizophrenic patients: application of a three-dimensional, stereologic counting method". J. Comp. Neurol. 392 (3): 402–12. doi:10.1002/(SICI)1096-9861(19980316)392:3<402::AID-CNE9>3.0.CO;2-5. PMID 9511926.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Meyer-Lindenberg A, Miletich RS, Kohn PD; et al. (2002). "Reduced prefrontal activity predicts exaggerated striatal dopaminergic function in schizophrenia". Nat. Neurosci. 5 (3): 267–71. doi:10.1038/nn804. PMID 11865311.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Spencer KM, Nestor PG, Perlmutter R; et al. (2004). "Neural synchrony indexes disordered perception and cognition in schizophrenia". Proc. Natl. Acad. Sci. U.S.A. 101 (49): 17288–93. doi:10.1073/pnas.0406074101. PMC 535363. PMID 15546988.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Broyd SJ, Demanuele C, Debener S, Helps SK, James CJ, Sonuga-Barke EJS (2009). "Default-mode brain dysfunction in mental disorders: a systematic review". Neurosci Biobehav Rev. 33 (3): 279–96. doi:10.1016/j.neubiorev.2008.09.002. PMID 18824195.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Experimental Eye Research Volume 83, Issue 5, November 2006, Pages 1246-1251 Copyright © 2006 Elsevier Ltd All rights reserved. GLC756 decreases TNF-α via an alpha2 and beta2 adrenoceptor related mechanismUlrich W. Laenglea, Anne U. Trendelenburgb, Rudolf Marksteina, Vicente Noguesa, Anne Provencher-Bollinger and Danielle Romana
- ^ Dopamine D4-like receptors in untreated schizophrenic patients demonstrated with PET and 11C-SDZ GLC 756 European Neuropsychopharmacology, Volume 8, Supplement 2, November 1998, Page S235 A. Klimke, C. Boy, M. Eickhoff, H. Herzog, M. Holschbach, H. Mühlensiepen, M. Weckesser, E. Rota Kops, F. Sonnenberg, W. Gaebel, R. Markstein, G. Stöcklin, H. H. Coenen, H. W Müller-Gärtner
- ^ Stefan, Martin (2002). An Atlas of Schizophrenia, p. 54
- ^ Creese I, Burt DR, Snyder SH (1976). "Dopamine receptor binding predicts clinical and pharmacological potencies of antischizophrenic drugs". Science (journal). 192 (4238): 481–3. PMID 3854.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Angrist B, van Kammen DP (1984). "CNS stimulants as a tool in the study of schizophrenia," Trends in Neurosciences, 7:388–90
- ^ Lieberman JA, Kane JM, Alvir J (1987). "Provocative tests with psychostimulant drugs in schizophrenia". Psychopharmacology (Berl.). 91 (4): 415–33. doi:10.1007/BF00216006. PMID 2884687.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Myers, David G. "Schizophrenia". Psychology. 2007. 678-85.
- ^ Schizophrenia Research Volume 78, Issue 1, 1 October 2005, Pages 45-60 doi:10.1016/j.schres.2005.05.009 Copyright © 2005 Elsevier B.V. All rights reserved Review of longitudinal functional neuroimaging studies of drug treatments in patients with schizophrenia C. Ervin Davisa, Dilip V. Jestea, and Lisa T. Eylera,
- ^ http://www.acnp.org/g4/GN401000114/CH112.html
- ^ E.M. Meisenzahl, G.J.Schmitt, J.Scheuerecker & H.-J. Moller, The role of dopamine for the pathophysiology of schizophrenia, Internationnal Review of Psychiatry, August 2007, 19(4)337-345
- ^ Laruelle M (1998). "Imaging dopamine transmission in schizophrenia. A review and meta-analysis". Q J Nucl Med. 42 (3): 211–21. PMID 9796369.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Stone, James M.; Morrison, Paul D.; Pilowsky, Lyn S. (2006), "Review: Glutamate and dopamine dysregulation in schizophrenia a synthesis and selective review", Journal of Psychopharmacology, 21 (4): 440, doi:10.1177/0269881106073126, PMID 17259207
{{citation}}: CS1 maint: multiple names: authors list (link) - ^ Arch Gen Psychiatry. 1988 Jun;45(6):553-9. Dopamine metabolism and disposition in schizophrenic patients. Studies using debrisoquin. Maas JW, Contreras SA, Seleshi E, Bowden CL.
- ^ Dopamine D2 densities and the schizophrenic brain Schizophrenia Research, Volume 32, Issue 3, 17 August 1998, Pages 201-206 Konstantine K. Zakzanis, Kevin T. Hansen
- ^ Proc Natl Acad Sci U S A. 2000 July 5; 97(14): 7673–7675. PMCID: PMC33999 Copyright © 2000, The National Academy of Sciences Schizophrenia: More dopamine, more D2 receptors Philip Seeman* and Shitij Kapur†
- ^ Proc Natl Acad Sci U S A. 2000 Jul 5;97(14):8104-9.Increased baseline occupancy of D2 receptors by dopamine in schizophrenia.Abi-Dargham A, Rodenhiser J, Printz D, Zea-Ponce Y, Gil R, Kegeles LS, Weiss R, Cooper TB, Mann JJ, Van Heertum RL, Gorman JM, Laruelle M.
- ^ Elevated D2/3-receptor availability in schizophrenia: A [18F]fallypride study Ingo Vernalekena, S.B. Eickhoffb, T. Veselinovica, M. Klompa, K. Spreckelmeyera, W. Schäferc and G. Gründera NeuroImage Volume 41, Supplement 2, 2008, Page T145
- ^ Small Effect of Dopamine Release and No Effect of Dopamine Depletion on [18F]Fallypride Binding in Healthy Humans VANESSA L. CROPLEY,1,2 ROBERT B. INNIS,1 PRADEEP J. NATHAN,3 AMIRA K. BROWN,1 JANET L. SANGARE,1 ALICJA LERNER,1 YONG HOON RYU,1,4 KELLY E. SPRAGUE,1 VICTOR W. PIKE,1 AND MASAHIRO FUJITA SYNAPSE 62:399–408 (2008)
- ^ Baseline and Amphetamine-Stimulated Dopamine Activity Are Related in Drug-Naïve Schizophrenic Subjects Biological Psychiatry, Volume 65, Issue 12, 15 June 2009, Pages 1091-1093 Anissa Abi-Dargham, Elsmarieke van de Giessen, Mark Slifstein, Lawrence S. Kegeles, Marc Laruelle
- ^ Dean F. Wong. Positron emission tomography reveals elevated D2 dopamine receptors in drug-naive schizophrenics.Science 234.(Dec 19, 1986): pp1558(6).
- ^ Abi-Dargham A, Moore H (2003). "Prefrontal DA transmission at D1 receptors and the pathology of schizophrenia". Neuroscientist. 9 (5): 404–16. doi:10.1177/1073858403252674. PMID 14580124.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ a b Seeman P, Schwarz J, Chen JF; et al. (2006). "Psychosis pathways converge via D2high dopamine receptors". Synapse. 60 (4): 319–46. doi:10.1002/syn.20303. PMID 16786561.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Albert Hung Choy Wonga, Hubert H.M. Van Tol (2003) "Schizophrenia: from phenomenology to neurobiology" Neuroscience and Biobehavioral Reviews 27, p276 http://www.nature.com/nature/journal/v365/n6445/abs/365441a0.html
- ^ for a discussion of opposing studies see p 143 PHILIP SEEMAN,*1 HONG-CHANG GUAN,1 JOSE NOBREGA,2 DILSHAD JIWA,2 RUDOLPH MARKSTEIN,3 JA-HYUN BALK,4 ROBERTO PICETTI,4 EMILIANA BORRELLI,4 AND HUBERT H.M. VAN TOL1, Dopamine D2-Like Sites in Schizophrenia, But Not in Alzheimer’s, Huntington’s, or Control Brains, for [3H]Benzquinoline SYNAPSE 25:137–146 (1997) http://www3.interscience.wiley.com/journal/52595/abstract?CRETRY=1&SRETRY=0
- ^ Cooperativity in associating proteins. Monomer-dimer equilibrium coupled to ligand binding Alexander Levitzki, Joseph Schlessinger Biochemistry, 1974, 13 (25), pp 5214–5219 DOI: 10.1021/bi00722a026 Publication Date: December 1974 http://pubs.acs.org/doi/abs/10.1021/bi00722a026
- ^ All Psychotic Roads Lead to Increased Dopamine D2High Receptors: A Perspective Journal Clinical Schizophrenia & Related Psychoses Publisher Walsh Medical Media ISSN 1935-1232 Issue Volume 1, Number 4 / January 2008 Category Translational Medicine DOI 10.3371/CSRP.1.4.7 Pages 351-355 http://clinicalschizophrenia.metapress.com/content/x32848665282821k/
- ^ "Dopamine receptor pharmacology", Trends in Pharmacological Sciences, Volume 15, Issue 7, July 1994, Pages 264-270 Philip Seeman, Hubert H.M. Van Tol
- ^ a b Philip Seeman & H. B. Niznik (1990). "Dopamine receptors and transporters in Parkinson's disease and schizophrenia". FASEB Journal. 4: 2737–2744.
- ^ Rote KV, Rechsteiner M (1986). "Degradation of proteins microinjected into HeLa cells. The role of substrate flexibility". J. Biol. Chem. 261 (33): 15430–6. PMID 2430958.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Konradi C, Heckers S (2003). "Molecular aspects of glutamate dysregulation: implications for schizophrenia and its treatment". Pharmacol. Ther. 97 (2): 153–79. doi:10.1016/S0163-7258(02)00328-5. PMID 12559388.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Lahti AC, Weiler MA, Tamara Michaelidis BA, Parwani A, Tamminga CA (2001). "Effects of ketamine in normal and schizophrenic volunteers". Neuropsychopharmacology. 25 (4): 455–67. doi:10.1016/S0893-133X(01)00243-3. PMID 11557159.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Coyle JT, Tsai G, Goff D (2003). "Converging evidence of NMDA receptor hypofunction in the pathophysiology of schizophrenia". Ann. N. Y. Acad. Sci. 1003: 318–27. doi:10.1196/annals.1300.020. PMID 14684455.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Tuominen HJ, Tiihonen J, Wahlbeck K (2005). "Glutamatergic drugs for schizophrenia: a systematic review and meta-analysis". Schizophr. Res. 72 (2–3): 225–34. doi:10.1016/j.schres.2004.05.005. PMID 15560967.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Yarlagadda A (2002). "Role of calcium regulation in pathophysiology model of schizophrenia and possible interventions". Med. Hypotheses. 58 (2): 182–6. doi:10.1054/mehy.2001.1511. PMID 11812200.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Yamada K, Ashikari I, Onishi K, Kanba S, Yagi G, Asai M (1995). "Effectiveness of nilvadipine in two cases of chronic schizophrenia". Psychiatry Clin. Neurosci. 49 (4): 237–8. doi:10.1111/j.1440-1819.1995.tb01891.x. PMID 9179944.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Prabakaran S, Swatton JE, Ryan MM; et al. (2004). "Mitochondrial dysfunction in schizophrenia: evidence for compromised brain metabolism and oxidative stress". Mol. Psychiatry. 9 (7): 684–97, 643. doi:10.1038/sj.mp.4001511. PMID 15098003.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 18408624, please use {{cite journal}} with
|pmid=18408624instead. - ^ R.D. Laing's and Aaron Esterson. Sanity, Madness and the Family (1964)
- ^ Bateson G, Jackson DD, Haley J, Weakland JH (1956). "Toward a theory of schizophrenia". Behavioral Science. 1: 251–264.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Jaynes J (1976). The origin of consciousness in the breakdown of the bicameral mind. Boston: Houghton Mifflin. ISBN 0-395-20729-0.
- ^ Polimeni J, Reiss JP (2002). "How shamanism and group selection may reveal the origins of schizophrenia". Med. Hypotheses. 58 (3): 244–8. doi:10.1054/mehy.2001.1504. PMID 12018978. Retrieved 2008-07-07.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ DeMause L (2002). "The seven stages of historical personality". Emotional Life of Nations. Other Press (NY). ISBN 1-892746-98-0.
{{cite book}}:|access-date=requires|url=(help); External link in|chapterurl=|chapterurl=ignored (|chapter-url=suggested) (help) - ^ Kurtz P (1991). The transcendental temptation: a critique of religion and the paranormal. Buffalo, N.Y: Prometheus Books. ISBN 0-87975-645-4.
- ^ Crow TJ (1997). "Schizophrenia as failure of hemispheric dominance for language". Trends Neurosci. 20 (8): 339–43. doi:10.1016/S0166-2236(97)01071-0. PMID 9246721. Retrieved 2008-07-07.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Colin R (2004). Schizophrenia: Innovations in Diagnosis and Treatment. Haworth Press. ISBN 0789022699.
- ^ Sass LA, Parnas J (2003). "Schizophrenia, consciousness, and the self". Schizophr Bull. 29 (3): 427–44. PMID 14609238.
- ^ Lysaker PH, Lysaker JT (2008). "Schizophrenia and Alterations in Self-experience: A Comparison of 6 Perspectives". Schizophr Bull. doi:10.1093/schbul/sbn077. PMID 18635676.
{{cite journal}}: Unknown parameter|month=ignored (help)
External links
- Template:Dmoz
- Template:Dmoz — Support Groups
- Template:Dmoz - Articles and research
- Schizophrenia at the National Institute of Mental Health
