Aminoglycoside: Difference between revisions
No edit summary |
Tag: references removed |
||
| Line 39: | Line 39: | ||
*They can also disrupt the integrity of bacterial cell membrane.<ref>{{cite journal |last1=Shakil |first1=Shazi |last2=Khan |first2=Rosina |last3=Zarrilli |first3=Raffaele |last4=Khan |first4=Asad U. |title=Aminoglycosides versus bacteria – a description of the action, resistance mechanism, and nosocomial battleground |journal=Journal of Biomedical Science |volume=15 |issue=1 |pages=5–14 |year=2007 |pmid=17657587 |doi=10.1007/s11373-007-9194-y}}</ref> |
*They can also disrupt the integrity of bacterial cell membrane.<ref>{{cite journal |last1=Shakil |first1=Shazi |last2=Khan |first2=Rosina |last3=Zarrilli |first3=Raffaele |last4=Khan |first4=Asad U. |title=Aminoglycosides versus bacteria – a description of the action, resistance mechanism, and nosocomial battleground |journal=Journal of Biomedical Science |volume=15 |issue=1 |pages=5–14 |year=2007 |pmid=17657587 |doi=10.1007/s11373-007-9194-y}}</ref> |
||
They bind to the bacterial [[30S]] [[ribosome|ribosomal]] subunit<ref name="urlAminoglycosides: Bacteria and Antibacterial Drugs: Merck Manual Professional">{{cite web |month=July |year=2009 |first=Matthew E. |last=Levison |url=http://www.merck.com/mmpe/sec14/ch170/ch170b.html |title=Aminoglycosides: Bacteria and Antibacterial Drugs |work=Merck Manual Professional}}</ref><ref name="urlAminoglycosides">{{cite web |url=http://www.aic.cuhk.edu.hk/web8/aminoglycosides.htm |title=Aminoglycosides |work= |accessdate=}}</ref> |
They bind to the bacterial [[30S]] [[ribosome|ribosomal]] subunit<ref name="urlAminoglycosides: Bacteria and Antibacterial Drugs: Merck Manual Professional">{{cite web |month=July |year=2009 |first=Matthew E. |last=Levison |url=http://www.merck.com/mmpe/sec14/ch170/ch170b.html |title=Aminoglycosides: Bacteria and Antibacterial Drugs |work=Merck Manual Professional}}</ref><ref name="urlAminoglycosides">{{cite web |url=http://www.aic.cuhk.edu.hk/web8/aminoglycosides.htm |title=Aminoglycosides |work= |accessdate=}}</ref> |
||
There is a significant variability in the relationship between the dose administered and the resultant plasma level in blood. [[Therapeutic drug monitoring]] (TDM) is necessary to obtain the correct dose. These agents exhibit a post-antibiotic effect in which there is no or very little drug level detectable in blood, but there still seems to be inhibition of bacterial re-growth. This is due to strong, irreversible binding to the ribosome, and remains intracellular long after plasma levels drop. This allows a prolonged dosage interval. Depending on their concentration, they act as [[Bacteriostatic agent|bacteriostatic]] or [[Bactericide|bactericidal]] agents.{{Citation needed|date=December 2010}} |
There is a significant variability in the relationship between the dose administered and the resultant plasma level in blood. [[Therapeutic drug monitoring]] (TDM) is necessary to obtain the correct dose. These agents exhibit a post-antibiotic effect in which there is no or very little drug level detectable in blood, but there still seems to be inhibition of bacterial re-growth. This is due to strong, irreversible binding to the ribosome, and remains intracellular long after plasma levels drop. This allows a prolonged dosage interval. Depending on their concentration, they act as [[Bacteriostatic agent|bacteriostatic]] or [[Bactericide|bactericidal]] agents.{{Citation needed|date=December 2010}} |
||
Revision as of 17:58, 14 February 2012

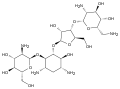
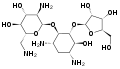
An aminoglycoside is a molecule or a portion of a molecule composed of amino-modified sugars.[1]
Several aminoglycosides function as antibiotics that are effective against certain types of bacteria. They include amikacin, arbekacin, gentamicin, kanamycin, neomycin, netilmicin, paromomycin, rhodostreptomycin,[2] streptomycin, tobramycin, and apramycin[3] .
Nomenclature
Aminoglycosides that are derived from bacteria of the Streptomyces genus are named with the suffix -mycin, whereas those that are derived from Micromonospora[4] are named with the suffix -micin.[5]
This nomenclature system is not specific for aminoglycosides. For example, vancomycin[6] is a glycopeptide antibiotic and erythromycin, which is produced from the species Saccharopolyspora erythraea (previously misclassified as Streptomyces) along with its synthetic derivatives clarithromycin and azithromycin, is a macrolide.[7][8] All differ in their mechanisms of action, however.
Mechanisms of action
Aminoglycosides have several potential antibiotic mechanisms, some as protein synthesis inhibitors, although their exact mechanism of action is not fully known:
- They interfere with the proofreading process, causing increased rate of error in synthesis with premature termination.[9]
- Also, there is evidence of inhibition of ribosomal translocation where the peptidyl-tRNA moves from the A-site to the P-site.[9]
- They can also disrupt the integrity of bacterial cell membrane.[10]
They bind to the bacterial 30S ribosomal subunit[11][12]
There is a significant variability in the relationship between the dose administered and the resultant plasma level in blood. Therapeutic drug monitoring (TDM) is necessary to obtain the correct dose. These agents exhibit a post-antibiotic effect in which there is no or very little drug level detectable in blood, but there still seems to be inhibition of bacterial re-growth. This is due to strong, irreversible binding to the ribosome, and remains intracellular long after plasma levels drop. This allows a prolonged dosage interval. Depending on their concentration, they act as bacteriostatic or bactericidal agents.[citation needed]
The protein synthesis inhibition of aminoglycosides does not usually produce a bactericidal effect, let alone a rapid one as is frequently observed on susceptible Gram-negative bacilli. Aminoglycosides competitively displace cell biofilm-associated Mg2+ and Ca2+ that link the polysaccharides of adjacent lipopolysaccharide molecules. "The result is shedding of cell membrane blebs, with formation of transient holes in the cell wall and disruption of the normal permeability of the cell wall. This action alone may be sufficient to kill most susceptible Gram-negative bacteria before the aminoglycoside has a chance to reach the 30S ribosome."[13]
The antibacterial properties of aminoglycosides were believed to result from inhibition of bacterial protein synthesis through irreversible binding to the 30S bacterial ribosome. This explanation, however, does not account for the potent bactericidal properties of these agents, since other antibiotics that inhibit the synthesis of proteins (such as tetracycline) are not bactericidal. Recent experimental studies show that the initial site of action is the outer bacterial membrane. The cationic antibiotic molecules create fissures in the outer cell membrane, resulting in leakage of intracellular contents and enhanced antibiotic uptake. This rapid action at the outer membrane, it is presumed, accounts for most of the bactericidal activity. Energy is needed for aminoglycoside uptake into the bacterial cell. Anaerobes have less energy available for this uptake, so aminoglycosides are less active against anaerobes.[citation needed]
Aminoglycosides are useful primarily in infections involving aerobic, gram-negative bacteria, such as Pseudomonas, Acinetobacter, and Enterobacter. In addition, some Mycobacteria, including the bacteria that cause tuberculosis, are susceptible to aminoglycosides. The most frequent use of aminoglycosides is empiric therapy for serious infections such as septicemia, complicated intraabdominal infections, complicated urinary tract infections, and nosocomial respiratory tract infections. Usually, once cultures of the causal organism are grown and their susceptibilities tested, aminoglycosides are discontinued in favor of less toxic antibiotics.[citation needed]
Streptomycin was the first effective drug in the treatment of tuberculosis, though the role of aminoglycosides such as streptomycin and amikacin has been eclipsed (because of their toxicity and inconvenient route of administration) except for multiple-drug-resistant strains.[citation needed]
Infections caused by gram-positive bacteria can also be treated with aminoglycosides, but other types of antibiotics are more potent and less damaging to the host. In the past, the aminoglycosides have been used in conjunction with beta-lactam antibiotics in streptococcal infections for their synergistic effects, in particular in endocarditis. One of the most frequent combinations is ampicillin (a beta-lactam, or penicillin-related antibiotic) and gentamicin. Often, hospital staff refer to this combination as "amp and gent" or more recently called "pen and gent" for penicillin and gentamicin.[citation needed]
Aminoglycosides are mostly ineffective against anaerobic bacteria, fungi, and viruses.[citation needed]
Nonsense suppression
The interference with DNA proofreading has been exploited to treat genetic diseases that result from premature stop codes (leading to early termination of protein synthesis and truncated proteins). Aminoglycosides can cause the cell to overcome the stop code, insert a random amino acid, and express a full-length protein.[14]
The aminoglycoside gentamicin has been used to treat cystic fibrosis (CF) cells in the laboratory to induce them to grow full-length proteins. CF is caused by a mutation in the gene coding for the cystic fibrosis transmembrane conductance regulator (CFTR) protein. In approximately 10% of CF cases, the mutation in this gene causes its early termination during translation, leading to the formation of is truncated and non-functional CFTR protein. It is believed that gentamicin distorts the structure of the ribosome-RNA complex, leading to a mis-reading of the termination codon, causing the ribosome to "skip" over the stop sequence and to continue with the normal elongation and production of the CFTR protein.[15]
Routes of administration
Since they are not absorbed from the gut, they are administered intravenously and intramuscularly. Some are used in topical preparations for wounds. Oral administration can be used for gut decontamination (e.g., in hepatic encephalopathy). Tobramycin may be administered in a nebulized form.[citation needed]
Clinical use
The recent emergence of infections due to Gram-negative bacterial strains with advanced patterns of antimicrobial resistance has prompted physicians to reevaluate the use of these antibacterial agents.[16] This revived interest in the use of aminoglycosides has brought back to light the debate on the two major issues related to these compounds, namely the spectrum of antimicrobial susceptibility and toxicity. Current evidence shows that aminoglycosides do retain activity against the majority of Gram-negative clinical bacterial isolates in many parts of the world. Still, the relatively frequent occurrence of nephrotoxicity and ototoxicity during aminoglycoside treatment makes physicians reluctant to use these compounds in everyday practice. Recent advances in the understanding of the effect of various dosage schedules of aminoglycosides on toxicity have provided a partial solution to this problem, although more research still needs to be done in order to overcome this problem entirely.[17]
Aminoglycosides are in pregnancy category D,[18] that is, there is positive evidence of human fetal risk based on adverse reaction data from investigational or marketing experience or studies in humans, but potential benefits may warrant use of the drug in pregnant women despite potential risks.
References
- ^ Aminoglycosides at the U.S. National Library of Medicine Medical Subject Headings (MeSH)
- ^ "Bacterial 'battle for survival' leads to new antibiotic" (Press release). Massachusetts Institute of Technology. February 26, 2008. Retrieved December 1, 2010.
- ^ Ryden, R (1977). "BJ". J Antimicrob Chemother. 3 (6): 609–613.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Kroppenstedt RM, Mayilraj S, Wink JM (2005). "Eight new species of the genus Micromonospora, Micromonospora citrea sp. nov., Micromonospora echinaurantiaca sp. nov., Micromonospora echinofusca sp. nov. Micromonospora fulviviridis sp. nov., Micromonospora inyonensis sp. nov., Micromonospora peucetia sp. nov., Micromonospora sagamiensis sp. nov., and Micromonospora viridifaciens sp. nov". Syst Appl Microbiol. 28 (4): 328–39. PMID 15997706.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Paul M. Dewick (2009). Medicinal Natural Products: A Biosynthetic Approach (3rd ed ed.). Wiley. ISBN 0470741678.
{{cite book}}:|edition=has extra text (help) - ^ Walter P. Hammes1 and Francis C. Neuhaus (1974). "On the Mechanism of Action of Vancomycin: Inhibition of Peptidoglycan Synthesis in Gaffkya homari". 6 (6): 722–728. PMC 444726.
{{cite journal}}: Cite journal requires|journal=(help)CS1 maint: numeric names: authors list (link) - ^ Protein synthesis inhibitors: macrolides mechanism of action animation. Classification of agents Pharmamotion. Author: Gary Kaiser. The Community College of Baltimore County. Retrieved on July 31, 2009
- ^ The Mechanism of Action of Macrolides, Lincosamides and Streptogramin B Reveals the Nascent Peptide Exit Path in the Ribosome Martin Lovmar and Måns Ehrenberg
- ^ a b Pharmamotion --> Protein synthesis inhibitors: aminoglycosides mechanism of action animation. Classification of agents Posted by Flavio Guzmán on 12/08/08[self-published source?]
- ^ Shakil, Shazi; Khan, Rosina; Zarrilli, Raffaele; Khan, Asad U. (2007). "Aminoglycosides versus bacteria – a description of the action, resistance mechanism, and nosocomial battleground". Journal of Biomedical Science. 15 (1): 5–14. doi:10.1007/s11373-007-9194-y. PMID 17657587.
- ^ Levison, Matthew E. (2009). "Aminoglycosides: Bacteria and Antibacterial Drugs". Merck Manual Professional.
{{cite web}}: Unknown parameter|month=ignored (help) - ^ "Aminoglycosides".
- ^ Lorian, Victor (1996). Antibiotics in Laboratory Medicine. Williams & Wilkins Press. pp. 589–90. ISBN 0-683-05169-5.
- ^ Feero, W. Gregory; Guttmacher, Alan E.; Dietz, Harry C. (2010). "New Therapeutic Approaches to Mendelian Disorders". New England Journal of Medicine. 363 (9): 852–63. doi:10.1056/NEJMra0907180. PMID 20818846.
- ^ Wilschanski, Michael; Yahav, Yaacov; Yaacov, Yasmin; Blau, Hannah; Bentur, Lea; Rivlin, Joseph; Aviram, Micha; Bdolah-Abram, Tali; Bebok, Zsuzsa (2003). "Gentamicin-Induced Correction of CFTR Function in Patients with Cystic Fibrosis andCFTRStop Mutations". New England Journal of Medicine. 349 (15): 1433–41. doi:10.1056/NEJMoa022170. PMID 14534336.
- ^ Falagas, Matthew E; Grammatikos, Alexandros P; Michalopoulos, Argyris (2008). "Potential of old-generation antibiotics to address current need for new antibiotics". Expert Review of Anti-infective Therapy. 6 (5): 593–600. doi:10.1586/14787210.6.5.593. PMID 18847400.
- ^ Durante-Mangoni, Emanuele; Grammatikos, Alexandros; Utili, Riccardo; Falagas, Matthew E. (2009). "Do we still need the aminoglycosides?". International Journal of Antimicrobial Agents. 33 (3): 201–5. doi:10.1016/j.ijantimicag.2008.09.001. PMID 18976888.
- ^ Merck Manual > Bacteria and Antibacterial Drugs Last full review/revision July 2009 by Matthew E. Levison, MD
External links
- MedlinePlus drug information - Aminoglycosides (Systemic)
- Science Daily Bacterial 'Battle for Survival' - Rhodostreptomycin