Attention deficit hyperactivity disorder: Difference between revisions
Robert4565 (talk | contribs) mNo edit summary |
→Pathophysiology: reworded and better-newer refs |
||
| Line 113: | Line 113: | ||
==Pathophysiology== |
==Pathophysiology== |
||
[[File:Illu cerebrum lobes.jpg|thumb|Diagram of the human brain]] |
[[File:Illu cerebrum lobes.jpg|thumb|Diagram of the human brain]] |
||
The [[pathophysiology]] of ADHD is unclear and there are a number of competing theories.<ref name=UTP2008/> Research on children with ADHD has shown a general reduction of brain volume, but with a proportionally greater reduction in the volume of the left-sided [[prefrontal cortex]]. These findings suggest that the core ADHD features of inattention, hyperactivity, and impulsivity may reflect [[frontal lobe disorder|frontal lobe dysfunction]], but other brain regions in particular the [[cerebellum]] have also been implicated.<ref>{{Cite journal |last1=Krain |first1=Amy |year=2006 |title=Brain development and ADHD |journal=Clinical Psychology Review |volume=26 |issue=4 |pages=433–444 |id= |url= |doi=10.1016/j.cpr.2006.01.005 |pmid=16480802 |last2=Krain |first2=AL |last3=Castellanos |first3=FX}}</ref> Neuroimaging studies in ADHD have not always given consistent results and as of 2008 are used only for research and not diagnostic purposes.<ref>{{cite web |url=http://www.merckmedicus.com/pp/us/hcp/diseasemodules/adhd/pathophysiology.jsp |title=MerckMedicus Modules: ADHD – Pathophysiology |archiveurl=http://web.archive.org/web/20100501074844/http://www.merckmedicus.com/pp/us/hcp/diseasemodules/adhd/pathophysiology.jsp|archivedate=1 May 2010|date=August 2002}}</ref> Research |
The [[pathophysiology]] of ADHD is unclear and there are a number of competing theories.<ref name=UTP2008/> Research on children with ADHD has shown a general reduction of brain volume, but with a proportionally greater reduction in the volume of the left-sided [[prefrontal cortex]]. These findings suggest that the core ADHD features of inattention, hyperactivity, and impulsivity may reflect [[frontal lobe disorder|frontal lobe dysfunction]], but other brain regions in particular the [[cerebellum]] have also been implicated.<ref>{{Cite journal |last1=Krain |first1=Amy |year=2006 |title=Brain development and ADHD |journal=Clinical Psychology Review |volume=26 |issue=4 |pages=433–444 |id= |url= |doi=10.1016/j.cpr.2006.01.005 |pmid=16480802 |last2=Krain |first2=AL |last3=Castellanos |first3=FX}}</ref> Neuroimaging studies in ADHD have not always given consistent results and as of 2008 are used only for research and not diagnostic purposes.<ref>{{cite web |url=http://www.merckmedicus.com/pp/us/hcp/diseasemodules/adhd/pathophysiology.jsp |title=MerckMedicus Modules: ADHD – Pathophysiology |archiveurl=http://web.archive.org/web/20100501074844/http://www.merckmedicus.com/pp/us/hcp/diseasemodules/adhd/pathophysiology.jsp|archivedate=1 May 2010|date=August 2002}}</ref> Research using neuroimaging, neuropsychological genetics, and neurochemistry has found converging lines of evidence to suggest that a main brain system connecting the [[prefrontal cortex]] and the [[striatum]] is involved in the pathophysiology of ADHD. Nevertheless other brain systems related to attentional, but also other more basic cognitive processes, have also been found to differ between ADHD patients and healthy controls.<ref name="pmid22169776">{{cite journal |author=Castellanos FX, Proal E |title=Large-scale brain systems in ADHD: beyond the prefrontal-striatal model |journal=Trends Cogn. Sci. (Regul. Ed.) |volume=16 |issue=1 |pages=17–26 |year=2012 |month=January |pmid=22169776 |pmc=3272832 |doi=10.1016/j.tics.2011.11.007 |url=}}</ref><ref name="pmid22983386">{{cite journal |author=Cortese S, Kelly C, Chabernaud C, ''et al.'' |title=Toward systems neuroscience of ADHD: a meta-analysis of 55 fMRI studies |journal=Am J Psychiatry |volume=169 |issue=10 |pages=1038–55 |year=2012 |month=October |pmid=22983386 |doi=10.1176/appi.ajp.2012.11101521 |url=}}</ref> |
||
Previously it was thought that the elevated number of dopamine transporters seen in ADHD patients was part of the pathophysiology of ADHD but it now appears that the reason for elevated striatal dopamine transporter density in ADHD individuals is due to neuroadaptations occurring due to the continuous exposure to stimulants such as methylphenidate or dexamphetamine as the body tries to counter-act the effects of the stimulants by developing a tolerance to the stimulant medications.<ref name="pmid22294258">{{cite journal |author=Fusar-Poli P, Rubia K, Rossi G, Sartori G, Balottin U |title=Striatal dopamine transporter alterations in ADHD: pathophysiology or adaptation to psychostimulants? A meta-analysis |journal=Am J Psychiatry |volume=169 |issue=3 |pages=264–72 |year=2012 |month=March |pmid=22294258 |doi=10.1176/appi.ajp.2011.11060940 |url=}}</ref> There is evidence that people with ADHD have a [[Low arousal theory|low arousal]] threshold and compensate for this with increased [[Stimulus (physiology)|stimuli]], which in turn results in disruption of attentional capacity and an increase in hyperactive behaviour. The reason for this is due to abnormalities in how the dopamine system in central nervous system responds to stimuli.<ref>{{Cite journal|author=Sikström S, Söderlund G |title=Stimulus-dependent dopamine release in attention-deficit/hyperactivity disorder |journal=Psychol Rev |volume=114 |issue=4 |pages=1047–75 |year=2007 |month=October |pmid=17907872 |doi=10.1037/0033-295X.114.4.1047 |url=http://content.apa.org/journals/rev/114/4/1047}}</ref> However, abnormalities in the dopamine system alone do not explain ADHD — abnormalities in the functioning of [[adrenergic]], [[serotoninergic]] and [[cholinergic]] or nicotinergic pathways can also be present and contribute to the pathophysiology of ADHD.<ref name="Kooij-2010"/><ref name="Cortese-2012">{{Cite journal | last1 = Cortese | first1 = S. | title = The neurobiology and genetics of Attention-Deficit/Hyperactivity Disorder (ADHD): what every clinician should know. | journal = Eur J Paediatr Neurol | volume = 16 | issue = 5 | pages = 422–33 | month = Sep | year = 2012 | doi = 10.1016/j.ejpn.2012.01.009 | PMID = 22306277 }}</ref> |
Previously it was thought that the elevated number of dopamine transporters seen in ADHD patients was part of the pathophysiology of ADHD but it now appears that the reason for elevated striatal dopamine transporter density in ADHD individuals is due to neuroadaptations occurring due to the continuous exposure to stimulants such as methylphenidate or dexamphetamine as the body tries to counter-act the effects of the stimulants by developing a tolerance to the stimulant medications.<ref name="pmid22294258">{{cite journal |author=Fusar-Poli P, Rubia K, Rossi G, Sartori G, Balottin U |title=Striatal dopamine transporter alterations in ADHD: pathophysiology or adaptation to psychostimulants? A meta-analysis |journal=Am J Psychiatry |volume=169 |issue=3 |pages=264–72 |year=2012 |month=March |pmid=22294258 |doi=10.1176/appi.ajp.2011.11060940 |url=}}</ref> There is evidence that people with ADHD have a [[Low arousal theory|low arousal]] threshold and compensate for this with increased [[Stimulus (physiology)|stimuli]], which in turn results in disruption of attentional capacity and an increase in hyperactive behaviour. The reason for this is due to abnormalities in how the dopamine system in central nervous system responds to stimuli.<ref>{{Cite journal|author=Sikström S, Söderlund G |title=Stimulus-dependent dopamine release in attention-deficit/hyperactivity disorder |journal=Psychol Rev |volume=114 |issue=4 |pages=1047–75 |year=2007 |month=October |pmid=17907872 |doi=10.1037/0033-295X.114.4.1047 |url=http://content.apa.org/journals/rev/114/4/1047}}</ref> However, abnormalities in the dopamine system alone do not explain ADHD — abnormalities in the functioning of [[adrenergic]], [[serotoninergic]] and [[cholinergic]] or nicotinergic pathways can also be present and contribute to the pathophysiology of ADHD.<ref name="Kooij-2010"/><ref name="Cortese-2012">{{Cite journal | last1 = Cortese | first1 = S. | title = The neurobiology and genetics of Attention-Deficit/Hyperactivity Disorder (ADHD): what every clinician should know. | journal = Eur J Paediatr Neurol | volume = 16 | issue = 5 | pages = 422–33 | month = Sep | year = 2012 | doi = 10.1016/j.ejpn.2012.01.009 | PMID = 22306277 }}</ref> |
||
Revision as of 10:44, 12 July 2013
| Attention deficit hyperactivity disorder | |
|---|---|
| Specialty | Psychiatry, child and adolescent psychiatry |
Attention deficit hyperactivity disorder (ADHD, similar to hyperkinetic disorder in the ICD) is a psychiatric disorder[1] or neurobehavioral disorder[2] characterized by significant difficulties either of inattention and/or hyperactivity and impulsiveness. Symptoms emerge before seven years of age.[3] There are three subtypes of the disorder which consist of it being predominantly inattentive (ADHD-PI or ADHD-I), predominantly hyperactive-impulsive (ADHD-HI or ADHD-H), or the two combined (ADHD-C), which shows all three difficulties. Often people refer to ADHD-PI as "attention deficit disorder" (ADD), however, the latter has not been officially accepted since the 1994 revision of the DSM. ADHD impacts school-aged children and results in restlessness, acting impulsively, and lack of focus which may impair school performance.
It is the most commonly studied and diagnosed psychiatric disorder in children and adolescents, affecting about 6 to 7 percent of children[4] and is diagnosed in about 2 to 16 percent of school-aged children.[5] It is often a chronic disorder[6] with 30 to 50 percent of those individuals diagnosed in childhood continuing to have symptoms into adulthood.[7] It is estimated that between 2 and 5 percent of adults live with ADHD.[8] ADHD is diagnosed two to four times more frequently in boys than in girls.[9][10] Its symptoms can be difficult to differentiate from other disorders, increasing the likelihood that the diagnosis of ADHD will be missed.[11] In addition, most clinicians have not received formal training in the assessment and treatment of ADHD, in particular in adult patients.[11] Standardized rating scales can be used for ADHD screening and assessment of the disorder's symptoms' severity.[12]
ADHD management usually involves some combination of medications, behavior therapy, lifestyle changes, and counseling. Medications are only recommended as a first-line treatment option in children who have severe symptoms. Medication therapy can also be considered for those with moderate ADHD symptoms who either refuse psychotherapeutic options or else fail to respond to psychotherapeutic input.[13]: p.317 Adolescents and adults with ADHD tend to develop coping mechanisms to compensate for some or all of their impairments.[14]
ADHD and its diagnosis and treatment have been considered controversial since the 1970s.[15] The controversies have involved clinicians, teachers, policymakers, parents and the media. Topics include ADHD's causes, and the use of stimulant medications in its treatment.[16][17] Most healthcare providers accept ADHD as a genuine disorder—debate in the scientific community centers mainly around how it is diagnosed and treated.[18][19][20] The National Institute for Clinical Excellence, while acknowledging the controversy, states that the current treatments and methods of diagnosis are based on the dominant view of the academic literature.[13]: p.133
Signs and symptoms
Inattention, hyperactivity, disruptive behavior and impulsivity are common in ADHD.[21][22] Academic difficulties are also frequent.[21] The symptoms are especially difficult to define because it is hard to draw a line at where normal levels of inattention, hyperactivity, and impulsivity end and clinically significant levels requiring intervention begin.[23] To be diagnosed with ADHD, symptoms must be observed in two different settings for six months or more and to a degree that is greater than other children of the same age.[24]
The symptom categories yield three potential classifications of ADHD—predominantly inattentive type, predominantly hyperactive-impulsive type, or combined type if criteria for both subtypes are met:[25]
Predominantly inattentive type symptoms as listed by the U.S. National Institute of Mental Health may include:[26]
- Be easily distracted, miss details, forget things, and frequently switch from one activity to another
- Have difficulty maintaining focus on one task
- Become bored with a task after only a few minutes, unless doing something enjoyable
- Have difficulty focusing attention on organizing and completing a task or learning something new or trouble completing or turning in homework assignments, often losing things (e.g., pencils, toys, assignments) needed to complete tasks or activities
- Not seem to listen when spoken to
- Daydream, become easily confused, and move slowly
- Have difficulty processing information as quickly and accurately as others
- Struggle to follow instructions.
Predominantly hyperactive-impulsive type symptoms may include:[26]
- Fidget and squirm in their seats
- Talk nonstop
- Dash around, touching or playing with anything and everything in sight
- Have trouble sitting still during dinner, school, and story time
- Be constantly in motion
- Have difficulty doing quiet tasks or activities
and also these manifestations primarily of impulsivity:[26]
- Be very impatient
- Blurt out inappropriate comments, show their emotions without restraint, and act without regard for consequences
- Blurts out comments better left unsaid (not always innapropriate)
- Have difficulty waiting for things they want or waiting their turns in games
Some children, adolescents, and adults with ADHD have an increased risk of experiencing difficulties with social skills, such as social interaction and forming and maintaining friendships. About half of children and adolescents with ADHD experience rejection by their peers compared to 10-15 percent of non-ADHD children and adolescents. Training in social skills, behavioural modification and medication may have some limited beneficial effects. The most important factor in reducing emergence of later psychopathology, such as major depression, criminality, school failure, and substance use disorders is formation of friendships with people who are not involved in delinquent activities.[27] Adolescents with ADHD are more likely to have difficulty making and keeping friends due to impairments in processing verbal and nonverbal language.[28]
Handwriting difficulties seem to be common in children with ADHD.[29] Delays in speech and language as well as motor development occur more commonly in the ADHD population.[30][31]
Associated disorders
Inattention and hyperactive behavior are not necessarily the only problems in children with ADHD. ADHD exists alone in only about 1/3 of the children diagnosed with it.[citation needed] The combination of ADHD with other conditions can greatly complicate diagnosis and treatment. Many co-existing (comorbid) conditions require other courses of treatment and should be diagnosed separately instead of being grouped in the ADHD diagnosis.[citation needed]
Some of the associated conditions are:
- Oppositional defiant disorder and conduct disorder, which occur with ADHD at a rate of 50 percent and 20 percent respectively,[32] are characterized by antisocial behaviors such as stubbornness, aggression, frequent temper tantrums, deceitfulness, lying, or stealing,[33] inevitably linking these comorbid disorders with antisocial personality disorder (ASPD); about half of those with hyperactivity and ODD or CD develop ASPD in adulthood.[34] However, modern brain imaging technology indicates that conduct disorder and ADHD are two distinct disorders.[35]
- Primary disorder of vigilance, which is characterized by poor attention and concentration, as well as difficulties staying awake. These children tend to fidget, yawn and stretch and appear to be hyperactive in order to remain alert and active.[33]
- Mood disorders (especially Bipolar disorder and Major depressive disorder). Boys diagnosed with the combined ADHD subtype have been shown to be more likely to suffer from a mood disorder.[36] Adults with ADHD sometimes have co-morbid bipolar disorder, which requires careful assessment in order to accurately diagnose and treat both conditions.[37]
- Anxiety disorders, have been found to occur more commonly in the ADHD population.[36]
- Obsessive-compulsive disorder. OCD can co-occur with ADHD and shares many of its characteristics.[33]
- Substance use disorders. Adolescents and adults with ADHD are at a significantly increased risk of developing a substance abuse problem which can interfere with the evaluation and treatment of ADHD. The reason for this increased risk may be due to an altered reward pathway in the brains of ADHD individuals.[8] The most commonly misused substances by the ADHD population are alcohol and cannabis; serious substance misuse problems should be treated first due to the serious risks and impairments that occur,[13]: p.38 [38] with long-term alcohol misuse and long-term cannabis misuse and other drug misuse.
- Restless legs syndrome, is associated with ADHD and is often due to iron deficiency anaemia.[39][40] However, restless legs can simply be a part of ADHD and requires careful assessment to differentiate between the two disorders.[41]
- Sleep disorders such as obstructive sleep apnea syndrome, can cause neurocognitive and behavioural symptoms in children that fulfil the ADHD diagnostic criteria.[42] Sleep disorders also commonly co-exist with ADHD or can be caused by side effects of medications used to treat ADHD; insomnia is the most common sleep disorder found in ADHD children. Behavioural therapy is preferred as a first line treatment of insomnia rather than medication in these children.[43][44] Melatonin is sometimes used in children who have sleep onset insomnia.[45]
There is a strong association between persistent bed wetting and ADHD[46] as well as dyspraxia with up to 50 percent of dyspraxics having ADHD.[47] Multiple research studies have also found a significant association between ADHD and language delay.[48] Anxiety and depression are some of the disorders that can accompany ADHD. Academic studies, and research in private practice suggest that depression in ADHD appears to be increasingly prevalent in children as they get older, with a higher rate of increase in girls than in boys, and to vary in prevalence with the subtype of ADHD.
Cause
The causes of ADHD remain an area of controversy - prenatal and perinatal risks such as exposure to lead and other environmental toxins, genetic contributions and social factors have been considered as possible causes. There is evidence that a combination of factors rather than a single cause explains ADHD.[49]
Genetics
Twin studies indicate that the disorder is highly heritable and that genetics are a factor in about 75 percent of all cases.[13] Hyperactivity also seems to be primarily a genetic condition; however, other causes have been identified.[50]
A large majority of ADHD cases may arise from a combination of various genes, many of which affect dopamine transporters. Candidate genes include DAT1, DRD4, DRD5, 5HTT, HTR1B, and SNAP25. There is also strong heterogeneity for the associations between ADHD and DAT1, DRD4, DRD5, dopamine beta hydroxylase, ADRA2A, 5HTT, TPH2, MAOA, and SNAP25.[51] A common variant of a gene called LPHN3 is estimated to be responsible for about 9% of the incidence of ADHD, and ADHD cases where this gene is present are particularly responsive to stimulant medication.[52]
Executive function
Cognitive processes that regulate, control, and manage other cognitive processes are termed executive functions (EF).[53] Examples of such regulated processes are planning, working memory, attention, inhibition, mental flexibility, and initiation and monitoring of actions.[54] One of the primary neuropsychologic theories of ADHD suggests that its symptoms arise from a primary deficit in executive functions.[55] Groups with ADHD showed significant impairment on all EF tasks. The strongest effects were on measures of response inhibition, vigilance, working memory, and planning. However, the effect sizes were moderate and there were also individual differences.[56] Not all individuals with ADHD show deficits in executive functioning;[57] the criteria for an executive function deficit are met in 30–50% of children and adolescents with ADHD.[58] Furthermore, deficits in EF are not unique to ADHD[57] being present in individuals with oppositional defiant disorder and conduct disorder.[57] One study found that 80% of individuals with ADHD were impaired in at least one EF task, compared to 50% for individuals without ADHD.[59] Deficits in certain executive functions play an important role in ADHD; however, "EF weaknesses are neither necessary nor sufficient to cause all cases of ADHD".[56]
Evolution
At more than 1 percent of the population, researchers have proposed that the high prevalence of ADHD may be due to natural selection having favoured ADHD, possibly because the individual traits may be beneficial on their own, and only become dysfunctional when these traits combine to form ADHD.[60] The high prevalence of ADHD may in part be because women in general are more attracted to males who are risk takers, thereby promoting ADHD in the gene pool.[61]
Further evidence that hyperactivity might be evolutionarily beneficial was put forth in a 2006 study finding that it may carry specific benefits for certain forms of society. In these societies, those with ADHD are hypothesized to have been more proficient in tasks involving risk, competition, and/or unpredictable behavior (i.e. exploring new areas, finding new food sources, etc.), where these societies may have benefited from confining impulsive or unpredictable behavior to a small subgroup. In these situations, ADHD would have been beneficial to society as a whole even while severely detrimental to the individual.[61] More recent research suggests that because it is more common in anxious or stressed mothers, ADHD primes a child to face a stressful or dangerous environment with—for example—increased impulsivity and explorative behaviour.[62] A genetic variant associated with ADHD (DRD4 48bp VNTR 7R allele) has been found to be at higher frequency in more nomadic populations and those with more of a history of migration.[63] Consistent with this, another group of researchers observed that the health status of nomadic Ariaal men was higher if they had the ADHD associated genetic variant (7R alleles). However in recently sedentary (non-nomadic) Ariaal those with 7R alleles seemed to have slightly worse health.[64]
Environmental
ADHD is predominantly a genetic disorder with environmental factors contributing a small role to the etiology of ADHD. Twin studies have shown that ADHD is largely genetic with 76 percent of the phenotypic variance being explained by inherited genetic factors.[65][66] Alcohol intake during pregnancy can cause the child to have a fetal alcohol spectrum disorder which can include symptoms similar to ADHD.[67] Exposure to tobacco smoke during pregnancy impairs normal development of the feotus including the central nervous system and can increase the risk of the child being diagnosed with ADHD.[68] Many children exposed to tobacco do not develop ADHD or else only have mild symptoms which do not reach the threshold of a diagnosis of ADHD. A combination of a genetic vulnerability to developing ADHD as well as the toxic developmental effects of tobacco on the foetus explain why some children exposed to tobacco smoke in utero develop ADHD and others don't.[69] Children exposed to lead, even relatively low levels of lead develop neurocognitive deficits which resemble ADHD and these children can fulfill the diagnostic criteria for ADHD. There is also some evidence that exposure to polychlorinated biphenyls during childhood causes developmental damage and can cause ADHD type symptoms which are then diagnosed as ADHD.[70] Exposure to the organophosphate insecticides chlorpyrifos and dialkyl phosphate is associated with an increased risk of ADHD. However, the evidence is not definitive as 5 of 17 studies failed to find an association.[71]
Very low birth weight, premature birth and exceptional early adversity increase the risk of the child having ADHD.[72] At least 30 percent of children who experience a pediatric traumatic brain injury develop ADHD.[73] Infections during pregnancy, at birth, and in early childhood are linked to an increased risk of developing ADHD. These include various viruses (measles, varicella, rubella, enterovirus 71) and streptococcal bacterial infection.[74]
Diet
According to one researcher, Weiss, concerns were first raised by Benjamin Feingold, a pediatric allergist, that food colourings and additives may affect children's behaviour in 1973. There is evidence suggesting that some food colourings may make some children hyperactive. However, the evidence for a link between food colourings and hyperactive behaviour remains uncertain. The FDA interpreted the evidence as being inconclusive as to whether food colours caused hyperactivity or not. The FDA review of food colours has been criticised for only doing a very narrow investigation into food colourings and their possible association with causing hyperactivity instead of investigating their possible effect on neurobehaviour in general.[75] It is possible that certain food colourings act as a trigger for ADHD symptoms in subgroup of children who have a genetic vulnerability. The U.K, followed by the European Union as a whole, took regulatory action on food colourings due to concerns about their possible adverse effects in children.[76] According to the Food Standards Agency, the food regulatory agency in the UK, food manufacturers were encouraged to voluntarily phase out the use of most artificial food colors by the end of 2009. Sunset yellow FCF (E110), quinoline yellow (E104), carmoisine (E122), allura red (E129), tartrazine (E102) and ponceau 4R (E124) are collectively called the "Southampton six". Following the FSA's actions, the European Food Safety Authority ruled that any food products containing the contentious colourings must display warning labels on their packaging by 2010.[77]
Social
The World Health Organization states that the diagnosis of ADHD can represent family dysfunction or inadequacies in the educational system rather than individual psychopathology.[78] Other researchers believe that relationships with caregivers have a profound effect on attentional and self-regulatory abilities. A study of foster children found that a high number of them had symptoms closely resembling ADHD.[79] Researchers have found behavior typical of ADHD in children who have suffered violence and emotional abuse.[13]
Social construction theory states that it is societies that determine where the line between normal and abnormal behavior is drawn. Thus society members including physicians, parents, teachers, and others are the ones who determine which diagnostic criteria are applied and, thus, determine the number of people affected.[80] This is exemplified in the fact that the DSM IV arrives at levels of ADHD three to four times higher than those obtained with use of the ICD 10.[10] Thomas Szasz, a proponent of this theory, has argued that ADHD was "invented and not discovered."[81][82]
Pathophysiology

The pathophysiology of ADHD is unclear and there are a number of competing theories.[33] Research on children with ADHD has shown a general reduction of brain volume, but with a proportionally greater reduction in the volume of the left-sided prefrontal cortex. These findings suggest that the core ADHD features of inattention, hyperactivity, and impulsivity may reflect frontal lobe dysfunction, but other brain regions in particular the cerebellum have also been implicated.[83] Neuroimaging studies in ADHD have not always given consistent results and as of 2008 are used only for research and not diagnostic purposes.[84] Research using neuroimaging, neuropsychological genetics, and neurochemistry has found converging lines of evidence to suggest that a main brain system connecting the prefrontal cortex and the striatum is involved in the pathophysiology of ADHD. Nevertheless other brain systems related to attentional, but also other more basic cognitive processes, have also been found to differ between ADHD patients and healthy controls.[85][86]
Previously it was thought that the elevated number of dopamine transporters seen in ADHD patients was part of the pathophysiology of ADHD but it now appears that the reason for elevated striatal dopamine transporter density in ADHD individuals is due to neuroadaptations occurring due to the continuous exposure to stimulants such as methylphenidate or dexamphetamine as the body tries to counter-act the effects of the stimulants by developing a tolerance to the stimulant medications.[87] There is evidence that people with ADHD have a low arousal threshold and compensate for this with increased stimuli, which in turn results in disruption of attentional capacity and an increase in hyperactive behaviour. The reason for this is due to abnormalities in how the dopamine system in central nervous system responds to stimuli.[88] However, abnormalities in the dopamine system alone do not explain ADHD — abnormalities in the functioning of adrenergic, serotoninergic and cholinergic or nicotinergic pathways can also be present and contribute to the pathophysiology of ADHD.[8][89]
Diagnosis
ADHD is diagnosed via a pediatric or psychiatric assessment of the person's childhood behavioural and cognitive development symptoms; this assessment includes ruling out the effects of drugs, medications and other medical or psychiatric disorders as possible explanations for the signs and symptoms.[13]: p.19–27 ADHD is diagnosed three to four times more commonly in boys than in girls.[9][10]
In North America, the DSM-IV criteria are often the basis for a diagnosis, while European countries usually use the ICD-10. If the DSM-IV criteria are used, rather than the ICD-10, a diagnosis of ADHD is 3–4 times more likely.[10] Factors other than those within the DSM or ICD, however, have been found to affect the diagnosis in clinical practice. For example, a study found that the youngest children in a class are much more likely to be diagnosed as having ADHD compared to their older counterparts in the same year. This is because these children may behave more hyperactively, not because they have ADHD, but because they are younger and developmentally behind their classmates. It is estimated that about 20 percent of children given a diagnosis of ADHD are misdiagnosed because of the month they were born.[90]
Children who display the behavioural symptoms of ADHD but who do not have any significant functional impairments compared to their age-matched peers cannot be diagnosed as having the psychiatric disorder, ADHD.[91]
The previously used term ADD expired with the most recent revision of the DSM. As a consequence, ADHD is the current nomenclature used to describe the disorder as one distinct disorder that can manifest itself as being a primary deficit resulting in hyperactivity/impulsivity (ADHD, predominantely hyperactive-impulsive type) or inattention (ADHD, predominantely inattentive type) or both (ADHD combined type).[24]
Classification
ADHD may be seen as one or more continuous traits found normally throughout the general population.[13] However, the definition of ADHD is based on behaviour and it does not imply a neurological disease.[13] ADHD is classified as a disruptive behavior disorder along with oppositional defiant disorder, conduct disorder and antisocial personality disorder.[92]
The Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR) classifies ADHD according to the predominance of symptoms of:
- Inattention;
- Hyperactivity–impulsivity;
- or a combination of both (Combined type).[24]
This subdivision is based on presence of at least six out of nine long-term maladaptive symptoms (lasting at least 6 months) of either inattention, hyperactivity–impulsivity, or both. Thus, a child who is diagnosed with the inattention subtype may also show signs of hyperactivity–impulsivity, and vice-versa. To be considered, the symptoms must have appeared before the age of 6, manifest in more than one environment (e.g. at home and at school or work), and not be better explained by another mental disorder.[24]
Most children with ADHD have the combined type. Children with the inattention subtype are less likely to act out or have difficulties getting along with other children. They may sit quietly, but without paying attention to what they are doing. Therefore, the child may be overlooked, and parents and teachers may not notice symptoms of ADHD.[24]
Diagnostic and Statistical Manual
As with many other psychiatric and medical disorders, the formal diagnosis is made by a qualified professional in the field based on a set number of criteria. In the USA these criteria are laid down by the American Psychiatric Association in their Diagnostic and Statistical Manual of Mental Disorders (DSM-IV). Based on the DSM-IV criteria listed below, three types of ADHD are classified:[91]
- ADHD, Combined Type is a combination of the two other ADHD subtypes.[91]
- ADHD Predominantly Inattentive Type presents with symptoms including being easily distracted, forgetful, daydreaming, disorganisation, poor concentration, and difficulty completing tasks.[91]
- ADHD, Predominantly Hyperactive-Impulsive Type presents with excessive fidgetiness and restlessness, hyperactivity, difficulty waiting and remaining seated, immature behaviour; destructive behaviors may also be present.[91]
For a diagnosis of ADHD to be made the signs must not be due to the course of a pervasive developmental disorder, schizophrenia, or other Psychotic Disorder. The signs are not better accounted for by another mental disorder (such as mood disorder, anxiety disorder, dissociative identity disorder, or a personality disorder).[24]
International Classification of Diseases
In the tenth edition of the International Statistical Classification of Diseases and Related Health Problems (ICD-10) the signs of ADHD are given the name "hyperkinetic disorders". When a conduct disorder (as defined by ICD-10[30]) is present, the condition is referred to as "hperkinetic conduct disorder". Otherwise the disorder is classified as "disturbance of activity and attention", "other hyperkinetic disorders" or "hyperkinetic disorders, unspecified". The latter is sometimes referred to as, "hyperkinetic syndrome".[30]
Other guidelines
The American Academy of Pediatrics' clinical practice guideline for children and adolescents with ADHD recommends the following:[93]
- ADHD should be considered as a possible diagnosis in children and adolescents aged 4-18 years old who present with academic or behavioural problems of hyperactivity, impulsiveness and inattention.
- To aid in the diagnosis the DSM IV should be used in combination with gathering evidence from family members, guardians, teachers and mental health workers who know the child or adolescent. Before making a diagnosis causes for the symptoms other than ADHD should be considered.
- Co-morbid disorders such as anxiety, depression, oppositional defiant disorder, and conduct disorder, as well as learning and language disorders which often co-exist with ADHD should be looked for. Additionally other neurodevelopmental disorders), as well as tics, sleep apnea should be screened for. Finally the guidance recommends when substance use disorders are present that these are treated first before the ADHD and given priority.
- ADHD should be viewed as a chronic disorder that has special healthcare needs and treatments which can include behavioural, pharmacological or a combination of both should take into consideration the age of the patient.
Adults often continue to be impaired by ADHD. Adults with ADHD are diagnosed under the same criteria, including the stipulation that their signs must have been present prior to the age of seven. Questioning parents or guardians as to how the person behaved and developed as a child also forms part of the clinical assessment of the individual; a family history of ADHD also adds weight to a diagnosis of adult ADHD due the strong heritability of ADHD.[8] While the core symptoms of ADHD are similar in children and adults they often present differently in adults than in children, for example excessive physical activity seen in children may present as feelings of restlessness and constant mental activity in adults.[8]
The American Academy of Child and Adolescent Psychiatry (AACAP) considers it necessary that the following be present before attaching the label of ADHD to a child:[94]
- The behaviors must appear before age 7.
- They must continue for at least six months.
- The symptoms must also create a real handicap in at least two of the following areas of the child's life:
- in the classroom,
- on the playground,
- at home,
- in the community, or
- in social settings.
If a child seems too active on the playground but not elsewhere, the problem might not be ADHD. It might also not be ADHD if the behaviors occur in the classroom but nowhere else. A child who shows some symptoms would not be diagnosed with ADHD if his or her schoolwork or friendships are not impaired by the behaviors.[94]
Differential
| ADHD symptoms which are related to other disorders[95] | |||
|---|---|---|---|
| Depression | Anxiety disorder | Bipolar disorder | |
|
|
| |
Symptoms of ADHD such as low mood and poor self-image, mood swings, and irritability can be confused with dysthymia, cyclothymia or bipolar disorder as well as with borderline personality disorder,[8] Some of the symptoms that are due to anxiety disorders, antisocial personality disorder, developmental disabilities or mental retardation or the effects of substance abuse such as intoxication and withdrawal symptoms can overlap with some ADHD symptoms. These various disorders which can mimic some ADHD symptoms are sometimes comorbid with ADHD. Medical conditions which can cause ADHD type symptoms and require consideration for a differential diagnosis include hyperthyroidism, seizure disorder, lead toxicity, hearing deficits, hepatic disease, sleep apnea, drug interactions, and head injury.[96]
Primary sleep disorders play a role in symptoms of inattention and behavioral dysregulation. There are multilevel and bidirectional relationships among sleep, neurobehavioral functioning and the clinical syndrome of ADHD.[97] Many sleep disorders are important causes of symptoms that may overlap with the core symptoms of ADHD; children with ADHD should be regularly and systematically assessed for sleep problems.[98][99] Behavioral manifestations of sleepiness in children range from the classic ones (yawning, rubbing eyes), to externalizing behaviors (impulsivity, hyperactivity, aggressiveness), to mood lability and inattentiveness.[98][100]
Management
The management of ADHD involves either psychotherapy or medication therapy alone or a combination of the two. Medications used in the treatment of ADHD include stimulants, noradrenergic agents, adrenergic agonists and certain antidepressants.[36] Medications have at least some effect in about 80% of people.[101] Dietary modifications may also be of benefit.[102]
Psychosocial
The evidence is strong for the effectiveness of behavioral treatments in ADHD.[103] It is recommended first line in those who have mild symptoms and in preschool-aged children.[104] Psychological therapies used include psychoeducational input, behavior therapy, cognitive behavioral therapy (CBT), interpersonal psychotherapy (IPT), family therapy, school-based interventions, social skills training, parent management training,[13] neurofeedback,[105] and outdoor activities.[106] Parent training and education have been found to have short-term benefits.[107] There is a deficiency of good research on the effectiveness of family therapy for ADHD, but the evidence that exists shows that it is comparable in effectiveness to treatment as usual in the community and is superior to medication placebo.[108] Several ADHD specific support groups exist as informational sources and to help families cope with challenges associated with dealing with ADHD.
Medication

Stimulant medications are the medical treatment of choice.[109] There are a number of non-stimulant medications, such as atomoxetine, that may be used as alternatives.[109] There are no good studies of comparative effectiveness between various medications, and there is a lack of evidence on their effects on academic performance and social behaviors.[110] While stimulants and atomoxetine are generally safe, there are side-effects and contraindications to their use.[109] Medications are not recommended for preschool children, as their long-term effects in such young people are unknown.[13][111] Research into the long-term effects of stimulants in ADHD have come to conflicting conclusions with one study finding benefit, another finding no benefit while another finding evidence of harm. The current research has methodological problems and more robust research has been recommended.[112] Any drug used for ADHD may have adverse drug reactions such as psychosis and mania,[113] though methylphenidate-induced psychosis is uncommon. Regular monitoring of individuals receiving long-term stimulant therapy for possible treatment emergent psychosis has been recommended.[114] Stimulant therapy is recommended to be discontinued periodically during protracted therapy to assess for continuing need for medication.[115] Tolerance to the therapeutic effects of stimulants can occur,[87] with rebound effects occurring when the dose wears off.[8] Therefore due to the risk of discontinuation/rebound effects abrupt withdrawal of stimulants is not recommended.[116] People with ADHD have an increased risk of substance abuse, and research studies have found that stimulant medications reduce this risk or have no effect on substance abuse.[8] Additionally, stimulant medications approved for treating ADHD have the potential for abuse and dependence.[117] Atomoxetine due to its lack of abuse potential may be preferred in individuals who are at risk of abusing stimulant medication.[8] Guidelines on when to use medications vary internationally, with the UK's National Institute of Clinical Excellence, for example, recommending use only in severe cases, while most United States guidelines recommend medications in nearly all cases.[118] Deficiency in zinc has been associated with inattentive symptoms of ADHD and there is evidence that zinc supplementation can benefit ADHD children who have low zinc levels. There is also some evidence that zinc supplementation leads to a significant reduction in the dosage of stimulants required for ADHD.[119]
Prognosis
A large study that followed children diagnosed with ADHD (combined type) over a period of 8 years found that they often have significant difficulties in adolescence, regardless of treatment or lack thereof.[120] In the United States, 37 percent of those with ADHD do not get a high school diploma even though many of them will receive special education services.[121] Also in the US, less than 5 percent of individuals with ADHD get a college degree[122] compared to 28 percent of the general population aged 25 years and older.[123] The proportion of children meeting the diagnostic criteria for ADHD drops by about 50 percent over three years after the diagnosis. This occurs regardless of the treatments used and also occurs in untreated children with ADHD.[124][125][126] ADHD persists into adulthood in about 30 to 50 percent of cases.[7] Those affected are likely to develop coping mechanisms as they mature, thus compensating for their previous ADHD.[14]
Epidemiology

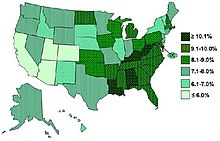
ADHD is estimated to affect about 6 to 7 percent of people aged 18 and under.[4] There is, however, both geographical and local variability among studies. Children in North America appear to have a higher rate of ADHD than children in Africa and the Middle East - however, this may be due to the methodology employed by different studies.[128] Published studies have found rates of ADHD as low as 2 percent and as high as 14 percent among school-aged children.[129] The rates of diagnosis and treatment of ADHD are also much higher on the east coast of the United States than on its west coast.[130] The frequency of the diagnosis differs between male children (10%) and female children (4%) in the United States.[131] This difference between genders may reflect either a difference in susceptibility or that females with ADHD are less likely to be diagnosed than males.[132]
Rates of ADHD diagnosis and treatment have increased in both the UK and the US since the 1970s. In the UK an estimated 0.5 per 1,000 children had ADHD in the 1970s, while 3 per 1,000 received ADHD medications in the late 1990s. In the US in the 1970s 12 per 1,000 children had the diagnosis, while in the late 1990s 34 per 1,000 had the diagnosis and the numbers continue to increase.[13] In the UK in 2003 a prevalence of 3.6 percent is reported in male children and less than 1 percent is reported in female children.[13]: 134
History
Hyperactivity has long been part of the human condition. Sir Alexander Crichton describes "mental restlessness" in his book An inquiry into the nature and origin of mental derangement written in 1798.[133][134] The terminology used to describe the symptoms of ADHD has gone through many changes over history including: "minimal brain damage", "minimal brain dysfunction" (or disorder), "learning/behavioral disabilities" and "hyperactivity". In the DSM-II (1968) it was the "Hyperkinetic Reaction of Childhood or adolescence". In the DSM-III "ADD (Attention-Deficit Disorder) with or without hyperactivity" was introduced. In 1987 this was changed to ADHD in the DSM-III-R and in 1994 the DSM-IV split the ADHD diagnosis into three subtypes, ADHD inattentive type, ADHD hyperactive-impulsive type and ADHD combined type.[135] The use of stimulants to treat ADHD was first described in 1937.[136]
Society and culture
A number of notable individuals have given controversial opinions on ADHD. Scientologist Tom Cruise has referred to the ADHD medications Ritalin and Adderall as being "street drugs" - this viewpoint (as well as his other viewpoints on psychiatry) has received criticism - for example the doses of stimulants used in the treatment of ADHD do not cause behavioural addiction and there is some evidence of a reduced risk of later substance addiction in children who had their ADHD treated with stimulants.[137] In England Baroness Susan Greenfield, a leading neuroscientist, spoke out publicly in 2007 in the House of Lords about the need for a wide-ranging inquiry into the dramatic increase in the diagnosis of ADHD in the UK and possible causes following a BBC Panorama programme that highlighted US research (The Multimodal Treatment Study of Children with ADHD by the University of Buffalo) suggesting drugs are no better than other forms of therapy for ADHD in the long term.[138] However, in 2010 the BBC Trust criticized the 2007 BBC Panorama programme for summarizing the US research as showing "no demonstrable improvement in children's behaviour after staying on ADHD medication for three years" when in actuality "the study found that medication did offer a significant improvement over time" although the long-term benefits of medication were found to be "no better than children who were treated with behaviour therapy."[139]
As of 2009[update], eight percent of all USMajor League Baseball players had been diagnosed with ADHD, making the disorder common among this population. The increase coincided with the League's 2006 ban on stimulants which has raised concern that some players are mimicking the symptoms of ADHD in order to get around the ban on the use of stimulants in sport.[140]
Controversies
ADHD and its diagnosis and treatment have been considered controversial since the 1970s.[15][16][141] The controversies have involved clinicians, teachers, policymakers, parents and the media. Opinions regarding ADHD range from not believing it exists at all[13]: p.23 [142] to believing there are genetic and physiological bases for the condition as well as disagreement about the use of stimulant medications in treatment.[16][17] Some sociologists consider ADHD to be a "classic example of the medicalization of deviant behavior, defining a previously nonmedical problem as a medical one".[15] Most healthcare providers in U.S. accept that ADHD is a genuine disorder with debate in centering mainly around how it is diagnosed and treated.[18][19][20]
Possible overdiagnosis of ADHD, the use of stimulant medications in children, and the methods by which ADHD is diagnosed and treated are some of the main areas of controversy.[143] Possible long-term side-effects of stimulants and their usefulness are largely unknown because of a lack of long-term studies.[144] Some research raises questions about the long-term effectiveness and side-effects of medications used to treat ADHD.[145] With a "wide variation in diagnosis across states, races, and ethnicities" some investigators suspect that factors other than neurological conditions play a role when the diagnosis of ADHD is made.[90]
Special populations
Adults
Between 2 and 5 percent of adults have ADHD.[8] Around two thirds of ADHD children continue to have ADHD as adults, however, not all of these children will continue to have the full disorder. About 15 percent of ADHD children continue to have the full ADHD disorder as adults whereas 50 percent partially 'grow out' of it with the remainder not displaying ADHD symptomatology as adults.[8] Most adults, however, remain untreated.[146] Untreated adults with ADHD often have chaotic lifestyles, may appear to be disorganized and may rely on non-prescribed drugs and alcohol to get by.[96] Other problems include relationship and job difficulties, and an increased propensity to become involved in criminal activities.[8] They often have such associated psychiatric comorbidities as depression, anxiety disorder, substance abuse, or a learning disability.[96]
Some ADHD symptoms of in adults differ from those seen in children — for example whereas children with ADHD may climb and run about excessively, adults may experience an inability to relax and talk excessively in social situations. Adults with ADHD may start relationships impulsively and may display sensation seeking behaviour and be short-tempered. Addictive behaviour such as substance abuse and gambling are also very common. The DSM-IV criteria have been criticised for not being developmentally appropriate for adults as these impairments present differently to children thus leading to claims that adults are outgrowing the diagnostic criteria rather than the ADHD disorder itself and thus are not being properly diagnosed.[8]
High IQ children
The diagnosis of ADHD and the significance of its impact in children with a high intelligence quotient (IQ) has been controversial.[147] Most studies have shown a similar profile of functional impairments than found in ADHD children with a normal IQ.[147] When compared with children without ADHD evidence supports an increased likelihood of repeating grades and more social and functional impairments. Additionally, more than half of high IQ ADHD people experience major depressive disorder or oppositional defiant disorder at some point in their lives. Generalised anxiety disorder, separation anxiety disorder and social phobia are also more common. However,there is some evidence that high IQ ADHD individuals have a lowered risk of substance abuse and anti-social behaviour compared to low and average IQ ADHD young people.[147] Regarding testing, high IQ children and adolescents with ADHD can have their intelligence level missed when a standard evaluation is performed; high IQ ADHD people tend to require more comprehensive testing to detect their true intelligence level.[147]
References
- ^ Bray, edited by Melissa A. (2011). The Oxford handbook of school psychology. New York: Oxford University Press. p. 285. ISBN 978-0-19-536980-9.
{{cite book}}:|first=has generic name (help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ "Attention Deficit-Hyperactivity Disorder Information Page". National Institute of Neurological Disorders and Stroke. National Institute of Health. 30 September 2012. Retrieved 8 September 2012.
- ^ "Attention-Deficit / Hyperactivity Disorder (ADHD): Symptoms and Diagnosis". Centers for Disease Control and Prevention. National Center on Birth Defects and Developmental Disabilities. 12 December 2010. Retrieved 8 September 2012.
- ^ a b Willcutt EG (2012). "The prevalence of DSM-IV attention-deficit/hyperactivity disorder: a meta-analytic review". Neurotherapeutics. 9 (3): 490–9. doi:10.1007/s13311-012-0135-8. PMID 22976615.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Rader R, McCauley L, Callen EC (2009). "Current strategies in the diagnosis and treatment of childhood attention-deficit/hyperactivity disorder". Am Fam Physician. 79 (8): 657–65. PMID 19405409.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Van Cleave J, Leslie LK (2008). "Approaching ADHD as a chronic condition: implications for long-term adherence". Journal of Psychosocial Nursing and Mental Health Services. 46 (8): 28–37. PMID 18777966.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ a b Bálint S, Czobor P, Mészáros A, Simon V, Bitter I (2008). "[Neuropsychological impairments in adult attention deficit hyperactivity disorder: a literature review]". Psychiatr Hung (in Hungarian). 23 (5): 324–35. PMID 19129549.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b c d e f g h i j k l m Kooij, SJ.; Bejerot, S.; Blackwell, A.; Caci, H.; Casas-Brugué, M.; Carpentier, PJ.; Edvinsson, D.; Fayyad, J.; Foeken, K. (2010). "European consensus statement on diagnosis and treatment of adult ADHD: The European Network Adult ADHD". BMC Psychiatry. 10: 67. doi:10.1186/1471-244X-10-67. PMID 20815868.
{{cite journal}}: Unknown parameter|displayauthors=ignored (|display-authors=suggested) (help)CS1 maint: unflagged free DOI (link) - ^ a b Emond V, Joyal C, Poissant H (2009). "[Structural and functional neuroanatomy of attention-deficit hyperactivity disorder (ADHD)]". Encephale (in French). 35 (2): 107–14. doi:10.1016/j.encep.2008.01.005. PMID 19393378.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ a b c d Singh I (2008). "Beyond polemics: science and ethics of ADHD". Nature Reviews. Neuroscience. 9 (12): 957–64. doi:10.1038/nrn2514. PMID 19020513.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ a b Ramsay, J. Russell (2007). Cognitive behavioral therapy for adult ADHD. Routledge. p. 25. ISBN 0-415-95501-7.
- ^ Kessler RC, Adler L, Ames M; et al. (2005). "The World Health Organization Adult ADHD Self-Report Scale (ASRS): a short screening scale for use in the general population". Psychological Medicine. 35 (2): 245–56. doi:10.1017/S0033291704002892. PMID 15841682.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ a b c d e f g h i j k l m National Institute for Health and Clinical Excellence (24 September 2008). "CG72 Attention deficit hyperactivity disorder (ADHD): full guideline" (PDF). NHS.
- ^ a b Gentile, Julie; Atiq, R; Gillig, PM (2004). "Adult ADHD: diagnosis, differential diagnosis and medication management". Psychiatry. 3 (8): 24–30. PMC 2957278. PMID 20963192.
- ^ a b c Parrillo, Vincent (2008). Encyclopedia of Social Problems. SAGE. p. 63. ISBN 978-1-4129-4165-5. Retrieved 2 May 2009.
- ^ a b c Mayes R, Bagwell C, Erkulwater J (2008). "ADHD and the rise in stimulant use among children". Harv Rev Psychiatry. 16 (3): 151–66. doi:10.1080/10673220802167782. PMID 18569037.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Cohen, Donald J.; Cicchetti, Dante (2006). Developmental psychopathology. Chichester: John Wiley & Sons. ISBN 0-471-23737-X.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ^ a b Sim MG, Hulse G, Khong E (2004). "When the child with ADHD grows up" (PDF). Aust Fam Physician. 33 (8): 615–8. PMID 15373378.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ a b Silver, Larry B (2004). Attention-deficit/hyperactivity disorder (3rd ed.). American Psychiatric Publishing. p. 4–7. ISBN 1-58562-131-5.
- ^ a b Schonwald A, Lechner E (2006). "Attention deficit/hyperactivity disorder: complexities and controversies". Curr. Opin. Pediatr. 18 (2): 189–95. doi:10.1097/01.mop.0000193302.70882.70. PMID 16601502.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ a b c Dobie, C (2012). "Diagnosis and management of attention deficit hyperactivity disorder in primary care for school-age children and adolescents". Institute for Clinical Systems Improvement: 79.
{{cite journal}}: Cite journal requires|journal=(help) - ^ Centers for Disease Control and Prevention. "Facts About ADHD". NCBDDD. Retrieved 13 November 2012.
- ^ Ramsay, J. Russell (2007). Cognitive behavioral therapy for adult ADHD. Routledge. p. 26. ISBN 0-415-95501-7.
- ^ a b c d e f Diagnostic and statistical manual of mental disorders: DSM-IV. Washington, DC: American Psychiatric Association. 2000. ISBN 0-89042-025-4.
- ^ Ramsay, J. Russell (2007). Cognitive behavioral therapy for adult ADHD. Routledge. p. 4. ISBN 0-415-95501-7.
- ^ a b c National Institute of Mental Health (2008). "Attention Deficit Hyperactivity Disorder (ADHD)". USA: National Institutes of Health.
- ^ Mikami AY (2010). "The importance of friendship for youth with attention-deficit/hyperactivity disorder". Clin Child Fam Psychol Rev. 13 (2): 181–98. doi:10.1007/s10567-010-0067-y. PMC 2921569. PMID 20490677.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Coleman WL (2008). "Social competence and friendship formation in adolescents with attention-deficit/hyperactivity disorder". Adolesc Med State Art Rev. 19 (2): 278–99, x. PMID 18822833.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Racine, MB.; Majnemer, A.; Shevell, M.; Snider, L. (2008). "Handwriting performance in children with attention deficit hyperactivity disorder (ADHD)". J Child Neurol. 23 (4): 399–406. doi:10.1177/0883073807309244. PMID 18401033.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ a b c "International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10) Version for 2010". World Health Organisation. 2010.
- ^ Bellani, M.; Moretti, A.; Perlini, C.; Brambilla, P. (2011). "Language disturbances in ADHD". Epidemiol Psychiatr Sci. 20 (4): 311–5. PMID 22201208.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ McBurnett K, Pfiffner LJ (2009). "Treatment of aggressive ADHD in children and adolescents: conceptualization and treatment of comorbid behavior disorders". Postgrad Med. 121 (6): 158–65. doi:10.3810/pgm.2009.11.2084. PMID 19940426.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ a b c d Krull, K.R. (5 December 2007). "Evaluation and diagnosis of attention deficit hyperactivity disorder in children" (Subscription required). Uptodate. Retrieved 12 September 2008.
- ^ Hofvander B, Ossowski D, Lundström S, Anckarsäter H (2009). "Continuity of aggressive antisocial behavior from childhood to adulthood: The question of phenotype definition". Int J Law Psychiatry. 32 (4): 224–34. doi:10.1016/j.ijlp.2009.04.004. PMID 19428109.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Rubia K (2011). ""Cool" inferior frontostriatal dysfunction in attention-deficit/hyperactivity disorder versus "hot" ventromedial orbitofrontal-limbic dysfunction in conduct disorder: a review". Biol. Psychiatry. 69 (12): e69–87. doi:10.1016/j.biopsych.2010.09.023. PMID 21094938.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ a b c Wilens, TE.; Spencer, TJ. (2010). "Understanding attention-deficit/hyperactivity disorder from childhood to adulthood". Postgrad Med. 122 (5): 97–109. doi:10.3810/pgm.2010.09.2206. PMID 20861593.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Baud P, Perroud N, Aubry JM (2011). "[Bipolar disorder and attention deficit/hyperactivity disorder in adults: differential diagnosis or comorbidity]". Rev Med Suisse (in French). 7 (297): 1219–22. PMID 21717696.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Wilens, TE.; Morrison, NR. (2011). "The intersection of attention-deficit/hyperactivity disorder and substance abuse". Curr Opin Psychiatry. 24 (4): 280–5. doi:10.1097/YCO.0b013e328345c956. PMID 21483267.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Merino-Andreu M (2011). "Trastorno por déficit de atención/hiperactividad y síndrome de piernas inquietas en niños". Rev Neurol (in Spanish; Castilian). 52 Suppl 1: S85–95. PMID 21365608.
{{cite journal}}: Unknown parameter|month=ignored (help); Unknown parameter|trans_title=ignored (|trans-title=suggested) (help)CS1 maint: unrecognized language (link) - ^ Picchietti MA, Picchietti DL (2010). "Advances in pediatric restless legs syndrome: Iron, genetics, diagnosis and treatment". Sleep Med. 11 (7): 643–51. doi:10.1016/j.sleep.2009.11.014. PMID 20620105.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Karroum E, Konofal E, Arnulf I (2008). "[Restless-legs syndrome]". Rev. Neurol. (Paris) (in French). 164 (8–9): 701–21. doi:10.1016/j.neurol.2008.06.006. PMID 18656214.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Lal C, Strange C, Bachman D (2012). "Neurocognitive impairment in obstructive sleep apnea". Chest. 141 (6): 1601–10. doi:10.1378/chest.11-2214. PMID 22670023.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Corkum P, Davidson F, Macpherson M (2011). "A framework for the assessment and treatment of sleep problems in children with attention-deficit/hyperactivity disorder". Pediatr. Clin. North Am. 58 (3): 667–83. doi:10.1016/j.pcl.2011.03.004. PMID 21600348.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Tsai MH, Huang YS (2010). "Attention-deficit/hyperactivity disorder and sleep disorders in children". Med. Clin. North Am. 94 (3): 615–32. doi:10.1016/j.mcna.2010.03.008. PMID 20451036.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Bendz LM, Scates AC (2010). "Melatonin treatment for insomnia in pediatric patients with attention-deficit/hyperactivity disorder". Ann Pharmacother. 44 (1): 185–91. doi:10.1345/aph.1M365. PMID 20028959.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Shreeram S, He JP, Kalaydjian A, Brothers S, Merikangas KR (2009). "Prevalence of enuresis and its association with attention-deficit/hyperactivity disorder among U.S. children: results from a nationally representative study". J Am Acad Child Adolesc Psychiatry. 48 (1): 35–41. doi:10.1097/CHI.0b013e318190045c. PMC 2794242. PMID 19096296.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Fliers EA, Franke B, Buitelaar JK (2011). "[Motor problems in children with ADHD receive too little attention in clinical practice]". Ned Tijdschr Geneeskd (in Dutch; Flemish). 155 (50): A3559. PMID 22186361.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: unrecognized language (link) - ^ Hagberg BS, Miniscalco C, Gillberg C (2010). "Clinic attenders with autism or attention-deficit/hyperactivity disorder: cognitive profile at school age and its relationship to preschool indicators of language delay". Res Dev Disabil. 31 (1): 1–8. doi:10.1016/j.ridd.2009.07.012. PMID 19713073.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Thapar A, Cooper M, Eyre O, Langley K (2013). "What have we learnt about the causes of ADHD?". J Child Psychol Psychiatry. 54 (1): 3–16. doi:10.1111/j.1469-7610.2012.02611.x. PMC 3572580. PMID 22963644.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Barkley, Russel A. "Attention-Deficit/Hyperactivity Disorder: Nature, Course, Outcomes, and Comorbidity". Archived from the original on 8 July 2006. Retrieved 26 June 2006.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Gizer, IR.; Ficks, C.; Waldman, ID. (2009). "Candidate gene studies of ADHD: a meta-analytic review". Hum Genet. 126 (1): 51–90. doi:10.1007/s00439-009-0694-x. PMID 19506906.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Arcos-Burgos M, Muenke M (2010). "Toward a better understanding of ADHD: LPHN3 gene variants and the susceptibility to develop ADHD". Atten Defic Hyperact Disord. 2 (3): 139–47. doi:10.1007/s12402-010-0030-2. PMC 3280610. PMID 21432600.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Elliott R (2003). "Executive functions and their disorders". Br. Med. Bull. 65: 49–59. PMID 12697616.
- ^ Chan RCK, Shum D, Toulopoulou T, Chen EYH, R; Shum, D; Toulopoulou, T; Chen, E (2008). "Assessment of executive functions: Review of instruments and identification of critical issues". Archives of Clinical Neuropsychology. 2. 23 (2): 201–216. doi:10.1016/j.acn.2007.08.010. PMID 18096360.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Brown, TE. (2008). "ADD/ADHD and Impaired Executive Function in Clinical Practice". Curr Psychiatry Rep. 10 (5): 407–11. PMID 18803914.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ a b Willcutt, EG.; Doyle, AE.; Nigg, JT.; Faraone, SV.; Pennington, BF. (2005). "Validity of the executive function theory of attention-deficit/hyperactivity disorder: a meta-analytic review" (PDF). Biol Psychiatry. 57 (11): 1336–46. doi:10.1016/j.biopsych.2005.02.006. PMID 15950006.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ a b c Nass RD (2005). "Evaluation and assessment issues in the diagnosis of attention deficit hyperactivity disorder". Seminars in Pediatric Neurology. 12 (4): 200–16. doi:10.1016/j.spen.2005.12.002. PMID 16780291.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Lambek R, Tannock R, Dalsgaard S, Trillingsgaard A, Damm D, Thomsen PH (2010). "Validating neuropsychological subtypes of ADHD: how do children with and without an executive function deficit differ?". Journal of Child Psychology and Psychiatry. 51 (8): 895–904. doi:10.1111/j.1469-7610.2010.02248.x. PMID 20406332.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Nigg, JT.; Willcutt, EG.; Doyle, AE.; Sonuga-Barke, EJ. (2005). "Causal heterogeneity in attention-deficit/hyperactivity disorder: do we need neuropsychologically impaired subtypes?" (PDF). Biol Psychiatry. 57 (11): 1224–30. doi:10.1016/j.biopsych.2004.08.025. PMID 15949992.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Cardo E, Nevot A, Redondo M; et al. (2010). "Trastorno por déficit de atención/hiperactividad: ¿un patrón evolutivo?". Rev Neurol (in Spanish; Castilian). 50 Suppl 3: S143–7. PMID 20200842.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help); Unknown parameter|trans_title=ignored (|trans-title=suggested) (help)CS1 maint: multiple names: authors list (link) CS1 maint: unrecognized language (link) - ^ a b Williams J, Taylor E (2006). "The evolution of hyperactivity, impulsivity and cognitive diversity". J R Soc Interface. 3 (8): 399–413. doi:10.1098/rsif.2005.0102. PMC 1578754. PMID 16849269.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Glover V (2011). "Annual Research Review: Prenatal stress and the origins of psychopathology: an evolutionary perspective". J Child Psychol Psychiatry. 52 (4): 356–67. doi:10.1111/j.1469-7610.2011.02371.x. PMID 21250994.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Chen CS, Burton M, Greenberger E, Dmitrieva J (1999). "Population migration and the variation of dopamine D4 receptor (DRD4) allele frequencies around the globe". Evolution and Human Behavior. 20 (5): 309–324. doi:10.1016/S1090-5138(99)00015-X.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Eisenberg DT, Campbell B, Gray PB, Sorenson MD (2008). "Dopamine receptor genetic polymorphisms and body composition in undernourished pastoralists: an exploration of nutrition indices among nomadic and recently settled Ariaal men of northern Kenya". BMC Evol. Biol. 8: 173. doi:10.1186/1471-2148-8-173. PMC 2440754. PMID 18544160.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - ^ Neale, BM; Medland, SE; Ripke, S; Asherson, P; Franke, B.; Lesch, KP; Faraone, SV; Nguyen, TT; Schäfer, H (2010). "Meta-analysis of genome-wide association studies of attention-deficit/hyperactivity disorder". J Am Acad Child Adolesc Psychiatry. 49 (9): 884–97. doi:10.1016/j.jaac.2010.06.008. PMC 2928252. PMID 20732625.
{{cite journal}}: Unknown parameter|displayauthors=ignored (|display-authors=suggested) (help); Unknown parameter|month=ignored (help) - ^ Burt, SA (2009). "Rethinking environmental contributions to child and adolescent psychopathology: a meta-analysis of shared environmental influences". Psychol Bull. 135 (4): 608–37. doi:10.1037/a0015702. PMID 19586164.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Burger, PH; Goecke, TW; Fasching, PA; Moll, G; Heinrich, H; Beckmann, MW; Kornhuber, J (2011). "Einfluss des mütterlichen Alkoholkonsums während der Schwangerschaft auf die Entwicklung von ADHS beim Kind". Fortschr Neurol Psychiatr (in German). 79 (9): 500–6. doi:10.1055/s-0031-1273360. PMID 21739408.
{{cite journal}}: Unknown parameter|month=ignored (help); Unknown parameter|trans_title=ignored (|trans-title=suggested) (help) - ^ Abbott, LC; Winzer-Serhan, UH (2012). "Smoking during pregnancy: lessons learned from epidemiological studies and experimental studies using animal models". Crit Rev Toxicol. 42 (4): 279–303. doi:10.3109/10408444.2012.658506. PMID 22394313.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Neuman RJ, Lobos E, Reich W, Henderson CA, Sun LW, Todd RD (2007 Jun 15). "Prenatal smoking exposure and dopaminergic genotypes interact to cause a severe ADHD subtype". Biol Psychiatry. 61 (12): 1320–8. PMID 17157268.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|laysummary=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Eubig, PA; Aguiar, A; Schantz, SL (2010). "Lead and PCBs as risk factors for attention deficit/hyperactivity disorder". Environ Health Perspect. 118 (12): 1654–67. doi:10.1289/ehp.0901852. PMID 20829149.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ de Cock, M; Maas, YG; van de Bor, M (2012). "Does perinatal exposure to endocrine disruptors induce autism spectrum and attention deficit hyperactivity disorders?". Acta Paediatrica (Review). 101 (8): 811–8. doi:10.1111/j.1651-2227.2012.02693.x. PMID 22458970.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Thapar, A.; Cooper, M.; Jefferies, R.; Stergiakouli, E. (2012). "What causes attention deficit hyperactivity disorder?". Arch Dis Child. 97 (3): 260–5. doi:10.1136/archdischild-2011-300482. PMID 21903599.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Eme, R (2012). "ADHD: an integration with pediatric traumatic brain injury". Expert Rev Neurother. 12 (4): 475–83. doi:10.1586/ern.12.15. PMID 22449218.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Millichap JG (2008). "Etiologic classification of attention-deficit/hyperactivity disorder". Pediatrics. 121 (2): e358–65. doi:10.1542/peds.2007-1332. PMID 18245408.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Weiss, B. (2012). "Synthetic food colours and neurobehavioral hazards: the view from environmental health research". Environ Health Perspect. 120 (1): 1–5. doi:10.1289/ehp.1103827. PMID 21926033.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Kleinman, RE; Brown, RT; Cutter, GR; Dupaul, GJ; Clydesdale, FM (2011). "A research model for investigating the effects of artificial food colorings on children with ADHD". Pediatrics. 127 (6): e1575-84. doi:10.1542/peds.2009-2206. PMID 21576306.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Sarah Chapman (2011). "Guidelines on approaches to the replacement of Tartrazine, Allura Red, Ponceau 4R, Quinoline Yellow, Sunset Yellow and Carmoisine in food and beverages" (PDF). United Kingdom: Food Standards Agency.
{{cite web}}: Unknown parameter|month=ignored (help) - ^ "Mental health of children and adolescents" (PDF). 12–15 January 2005. Archived from the original (PDF) on 24 October 2009. Retrieved 13 October 2011.
- ^ Marni Finkelstein, Mark Wamsley, Doreen Miranda (2002). "What keeps children in foster care from succeeding in school?" (PDF). VERA Institute of Justice. Archived from the original (PDF) on 6 March 2008.
{{cite web}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Parens E, Johnston J (2009). "Facts, values, and Attention-Deficit Hyperactivity Disorder (ADHD): an update on the controversies". Child Adolesc Psychiatry Ment Health. 3 (1): 1. doi:10.1186/1753-2000-3-1. PMC 2637252. PMID 19152690.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Chriss, James J. (2007). Social control: an introduction. Cambridge, UK: Polity. p. 230. ISBN 0-7456-3858-9.
- ^ Szasz, Thomas Stephen (2001). Pharmacracy: medicine and politics in America. New York: Praeger. p. 212. ISBN 0-275-97196-1.
- ^ Krain, Amy; Krain, AL; Castellanos, FX (2006). "Brain development and ADHD". Clinical Psychology Review. 26 (4): 433–444. doi:10.1016/j.cpr.2006.01.005. PMID 16480802.
- ^ "MerckMedicus Modules: ADHD – Pathophysiology". August 2002. Archived from the original on 1 May 2010.
- ^ Castellanos FX, Proal E (2012). "Large-scale brain systems in ADHD: beyond the prefrontal-striatal model". Trends Cogn. Sci. (Regul. Ed.). 16 (1): 17–26. doi:10.1016/j.tics.2011.11.007. PMC 3272832. PMID 22169776.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Cortese S, Kelly C, Chabernaud C; et al. (2012). "Toward systems neuroscience of ADHD: a meta-analysis of 55 fMRI studies". Am J Psychiatry. 169 (10): 1038–55. doi:10.1176/appi.ajp.2012.11101521. PMID 22983386.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ a b Fusar-Poli P, Rubia K, Rossi G, Sartori G, Balottin U (2012). "Striatal dopamine transporter alterations in ADHD: pathophysiology or adaptation to psychostimulants? A meta-analysis". Am J Psychiatry. 169 (3): 264–72. doi:10.1176/appi.ajp.2011.11060940. PMID 22294258.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Sikström S, Söderlund G (2007). "Stimulus-dependent dopamine release in attention-deficit/hyperactivity disorder". Psychol Rev. 114 (4): 1047–75. doi:10.1037/0033-295X.114.4.1047. PMID 17907872.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Cortese, S. (2012). "The neurobiology and genetics of Attention-Deficit/Hyperactivity Disorder (ADHD): what every clinician should know". Eur J Paediatr Neurol. 16 (5): 422–33. doi:10.1016/j.ejpn.2012.01.009. PMID 22306277.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ a b Elder, TE. (2010). "The importance of relative standards in ADHD diagnoses: evidence based on exact birth dates". J Health Econ. 29 (5): 641–56. doi:10.1016/j.jhealeco.2010.06.003. PMC 2933294. PMID 20638739.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ a b c d e Berger I (2011). "Diagnosis of attention deficit hyperactivity disorder: much ado about something" (PDF). Isr. Med. Assoc. J. 13 (9): 571–4. PMID 21991721.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Wiener, Jerry M., Editor (2003). Textbook Of Child & Adolescent Psychiatry. Washington, DC: American Psychiatric Association. ISBN 1-58562-057-2.
{{cite book}}:|author=has generic name (help)CS1 maint: multiple names: authors list (link) - ^ Wolraich, M.; Brown, L.; Brown, RT.; DuPaul, G.; Earls, M.; Feldman, HM.; Ganiats, TG.; Kaplanek, B.; Meyer, B. (2011). "ADHD: clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents". Pediatrics. 128 (5): 1007–22. doi:10.1542/peds.2011-2654. PMID 22003063.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ a b "ADHD – A Guide for Families". USA: American Academy of Child Adolescent Psychiatry. 2010.
- ^ Consumer Reports; Drug Effectiveness Review Project (March 2012). "Evaluating Prescription Drugs Used to Treat: Attention Deficit Hyperactivity Disorder (ADHD) Comparing Effectiveness, Safety, and Price" (Document). Consumer Reports. p. 2.
{{cite document}}: Unknown parameter|accessdate=ignored (help); Unknown parameter|url=ignored (help); Unknown parameter|work=ignored (help)CS1 maint: postscript (link) - ^ a b c Gentile, Julie; Atiq, R; Gillig, PM (2006). "Adult ADHD: Diagnosis, Differential Diagnosis, and Medication Management". Psychiatry (Edgmont (Pa. : Township)). 3 (8). Psychiatrymmc.com: 25–30. PMC 2957278. PMID 20963192.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Owens JA (2008). "Sleep disorders and attention-deficit/hyperactivity disorder". Current Psychiatry Reports. 10 (5): 439–44. doi:10.1007/s11920-008-0070-x. PMID 18803919.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ a b Owens JA (2005). "The ADHD and sleep conundrum: a review". Journal of Developmental and Behavioral Pediatrics. 26 (4): 312–22. doi:10.1097/00004703-200508000-00011. PMID 16100507.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Walters AS, Silvestri R, Zucconi M, Chandrashekariah R, Konofal E (2008). "Review of the possible relationship and hypothetical links between attention deficit hyperactivity disorder (ADHD) and the simple sleep related movement disorders, parasomnias, hypersomnias, and circadian rhythm disorders". Journal of Clinical Sleep Medicine. 4 (6): 591–600. PMC 2603539. PMID 19110891.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Hirshkowitz, Max (2004). "Neuropsychiatric Aspects of Sleep and Sleep Disorders". In Yudofsky, Stuart C. and Robert E. Hales, editors (ed.). Essentials of neuropsychiatry and clinical neurosciences (4 ed.). Arlington, Virginia, USA: American Psychiatric Publishing. pp. 315–40. ISBN 978-1-58562-005-0.
{{cite book}}:|editor=has generic name (help);|format=requires|url=(help); Cite has empty unknown parameters:|origmonth=and|origdate=(help); External link in|chapterurl=|chapterurl=ignored (|chapter-url=suggested) (help)CS1 maint: multiple names: editors list (link) - ^ "Canadian ADHD Practice Guidelines" (PDF). Canadian ADHD Alliance. Retrieved 4 February 2011.
- ^ Nigg, JT (2012 Jan). "Meta-analysis of attention-deficit/hyperactivity disorder or attention-deficit/hyperactivity disorder symptoms, restriction diet, and synthetic food color additives". Journal of the American Academy of Child and Adolescent Psychiatry. 51 (1): 86–97.e8. PMID 22176942.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Fabiano GA, Pelham WE, Coles EK, Gnagy EM, Chronis-Tuscano A, O'Connor BC (2009). "A meta-analysis of behavioral treatments for attention-deficit/hyperactivity disorder". Clinical Psychology Review. 29 (2): 129–40. doi:10.1016/j.cpr.2008.11.001. PMID 19131150.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Kratochvil CJ, Vaughan BS, Barker A, Corr L, Wheeler A, Madaan V (2009). "Review of pediatric attention deficit/hyperactivity disorder for the general psychiatrist". Psychiatr. Clin. North Am. 32 (1): 39–56. doi:10.1016/j.psc.2008.10.001. PMID 19248915.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Arns, M (July 2009). "Efficacy of neurofeedback treatment in ADHD: the effects on inattention, impulsivity and hyperactivity: a meta-analysis". Clinical EEG and neuroscience : official journal of the EEG and Clinical Neuroscience Society (ENCS). 40 (3): 180–9. PMID 19715181.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Kuo, FE.; Taylor, AF. (2004). "A potential natural treatment for attention-deficit/hyperactivity disorder: evidence from a national study". Am J Public Health. 94 (9): 1580–6. PMID 15333318.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Pliszka S; AACAP Work Group on Quality Issues (2007). "Practice parameter for the assessment and treatment of children and adolescents with attention-deficit/hyperactivity disorder". Journal of the American Academy of Child and Adolescent Psychiatry. 46 (7): 894–921. doi:10.1097/chi.0b013e318054e724. PMID 17581453.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Bjornstad G, Montgomery P (2005). "Family therapy for attention-deficit disorder or attention-deficit/hyperactivity disorder in children and adolescents". Cochrane Database Syst Rev (2): CD005042. doi:10.1002/14651858.CD005042.pub2. PMID 15846741.
- ^ a b c Wigal SB (2009). "Efficacy and safety limitations of attention-deficit hyperactivity disorder pharmacotherapy in children and adults". CNS Drugs. 23 Suppl 1: 21–31. doi:10.2165/00023210-200923000-00004. PMID 19621975.
- ^ McDonagh MS, Peterson K, Thakurta S, Low A (2011). "Drug Class Review: Pharmacologic Treatments for Attention Deficit Hyperactivity Disorder". U.S. Library of Medicine. PMID 22420008.
{{cite journal}}: Cite journal requires|journal=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Greenhill LL, Posner K, Vaughan BS, Kratochvil CJ (2008). "Attention deficit hyperactivity disorder in preschool children". Child and Adolescent Psychiatric Clinics of North America. 17 (2): 347–66, ix. doi:10.1016/j.chc.2007.11.004. PMID 18295150.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Hazell P (2011). "The challenges to demonstrating long-term effects of psychostimulant treatment for attention-deficit/hyperactivity disorder". Curr Opin Psychiatry. 24 (4): 286–90. doi:10.1097/YCO.0b013e32834742db. PMID 21519262.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Mosholder, AD (February 2009). "Hallucinations and other psychotic symptoms associated with the use of attention-deficit/hyperactivity disorder drugs in children". Pediatrics. 123 (2): 611–6. doi:10.1542/peds.2008-0185. PMID 19171629.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Kraemer M, Uekermann J, Wiltfang J, Kis B (2010). "Methylphenidate-induced psychosis in adult attention-deficit/hyperactivity disorder: report of 3 new cases and review of the literature". Clin Neuropharmacol. 33 (4): 204–6. doi:10.1097/WNF.0b013e3181e29174. PMID 20571380.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ van de Loo-Neus GH, Rommelse N, Buitelaar JK (2011). "To stop or not to stop? How long should medication treatment of attention-deficit hyperactivity disorder be extended?". Eur Neuropsychopharmacol. 21 (8): 584–99. doi:10.1016/j.euroneuro.2011.03.008. PMID 21530185.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Medical Association, British (2007). "4 Central Nervous System". British National Formulary (54 ed.). UK: Royal Pharmaceutical Society of Great Britain. p. 212. ISBN 978-0-85369-736-7.
{{cite book}}: Unknown parameter|month=ignored (help) - ^ Oregon Health & Science University, Portland, Oregon (2009). "Black box warnings of ADHD drugs approved by the US Food and Drug Administration". U.S. National Library of Medicine.
{{cite web}}: CS1 maint: multiple names: authors list (link) - ^ "Canadian ADHD Practice Guidelines" (PDF). Canadian ADHD Alliance. Retrieved 4 February 2011.
- ^ Millichap JG, Yee MM (2012). "The diet factor in attention-deficit/hyperactivity disorder". Pediatrics. 129 (2): 330–7. doi:10.1542/peds.2011-2199. PMID 22232312.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Molina BS, Hinshaw SP, Swanson JM; et al. (2009). "The MTA at 8 years: prospective follow-up of children treated for combined-type ADHD in a multisite study". Journal of the American Academy of Child and Adolescent Psychiatry. 48 (5): 484–500. doi:10.1097/CHI.0b013e31819c23d0. PMC 3063150. PMID 19318991.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ "Attention-Deficit/Hyperactivity Disorder: Nature, Course, Outcomes, and Comorbidity". Barkley, Russell. Archived from the original on 17 September 2008. Retrieved 19 September 2008.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Cimera, Robert E. (2002). Making ADHD a gift : teaching Superman how to fly. Lanham, Md.: Scarecrow Press. p. 116. ISBN 978-0-8108-4318-9.
- ^ "College Degree Nearly Doubles Annual Earnings, Census Bureau Reports". Archived from the original on 30 March 2005. Retrieved 2 October 2008.
- ^ Smucker WD, Hedayat M (2001). "Evaluation and treatment of ADHD". American Family Physician. 64 (5): 817–29. PMID 11563573.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Jensen PS, Arnold LE, Swanson JM (2007). "3-year follow-up of the NIMH MTA study". Journal of the American Academy of Child and Adolescent Psychiatry. 46 (8): 989–1002. doi:10.1097/CHI.0b013e3180686d48. PMID 17667478.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ "What is the evidence for using CNS stimulants to treat ADHD in children? | Therapeutics Initiative". Archived from the original on 6 September 2010.
- ^ "CDC – ADHD, Prevalence – NCBDDD".
- ^ Polanczyk G, de Lima MS, Horta BL, Biederman J, Rohde LA (2007). "The worldwide prevalence of ADHD: a systematic review and metaregression analysis". The American Journal of Psychiatry. 164 (6): 942–8. doi:10.1176/appi.ajp.164.6.942. PMID 17541055.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ "LONI: Laboratory of Neuro Imaging". Archived from the original on 6 September 2008. Retrieved 19 September 2008.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Centers for Disease Control and Prevention (17 October 2013). "ADHD Home". USA: CDC.gov.
- ^ CDC.gov (2004). "Summary Health Statistics for U.S. Children: National Health Interview Survey, 2002" (PDF). 10 Number 221. USA: CDC.gov.
{{cite web}}: Unknown parameter|month=ignored (help) - ^ Staller J, Faraone SV (2006). "Attention-deficit hyperactivity disorder in girls: epidemiology and management". CNS Drugs. 20 (2): 107–23. doi:10.2165/00023210-200620020-00003. PMID 16478287.
- ^ "An early description of ADHD (inattentive subtype): Dr Alexander Crichton and 'Mental restlessness' (1798)". Child and Adolescent Mental Health. 6 (2): 66–73. 2001. doi:10.1111/1475-3588.00324.
{{cite journal}}: Cite uses deprecated parameter|authors=(help); Unknown parameter|month=ignored (help) - ^ Crichton, Andrew (1798). An inquiry into the nature and origin of mental derangement: comprehending a concise system of the physiology and pathology of the human mind and a history of the passions and their effects. United Kingdom: AMS Press. p. 271.
- ^ Millichap, J. Gordon (2010). "1. Definition and History of ADHD". Attention Deficit Hyperactivity Disorder Handbook. Springer Verlag Gmbh. pp. 2–3. ISBN 978-1-4419-1409-5.
{{cite book}}: Unknown parameter|month=ignored (help) - ^ Patrick KS, Straughn AB, Perkins JS, González MA (2009). "Evolution of stimulants to treat ADHD: transdermal methylphenidate". Human Psychopharmacology. 24 (1): 1–17. doi:10.1002/hup.992. PMC 2629554. PMID 19051222.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Neill US (2005). "Tom Cruise is dangerous and irresponsible". J. Clin. Invest. 115 (8): 1964–5. doi:10.1172/JCI26200. PMC 1180571. PMID 16075033.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ "Peer calls for ADHD care review". BBC News. 14 November 2007. Retrieved 29 January 2012.
- ^ Singh A (25 February 2010). "BBC must broadcast apology over inaccurate Panorama programme". The Telegraph. Retrieved 29 January 2012.
- ^ Saletan, William (12 January 2009). "Doping Deficit Disorder. Need performance-enhancing drugs? Claim ADHD". Slate. Archived from the original on 21 May 2009. Retrieved 2 May 2009.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Foreman, DM (2006). "Attention deficit hyperactivity disorder: legal and ethical aspects". Archives of Disease in Childhood. 91 (2): 192–4. doi:10.1136/adc.2004.064576. PMC 2082674. PMID 16428370.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Faraone, Stephen V (2005). "The scientific foundation for understanding attention-deficit/hyperactivity disorder as a valid psychiatric disorder". Eur Child Adolesc Psychiatry. 14 (1): 1–10. doi:10.1007/s00787-005-0429-z. PMID 15756510.
- ^ Cormier E (2008). "Attention deficit/hyperactivity disorder: a review and update". J Pediatr Nurs. 23 (5): 345–57. doi:10.1016/j.pedn.2008.01.003. PMID 18804015.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Ashton H, Gallagher P, Moore B (2006). "The adult psychiatrist's dilemma: psychostimulant use in attention deficit/hyperactivity disorder". J. Psychopharmacol. (Oxford). 20 (5): 602–10. doi:10.1177/0269881106061710. PMID 16478756.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Lakhan, SE; Hagger-Johnson, GE (2007). "The impact of prescribed psychotropics on youth". Clin Pract Epidemol Ment Health. 3 (1): 21. doi:10.1186/1745-0179-3-21. PMC 2100041. PMID 17949504.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - ^ Culpepper, L, Mattingly G (2010). "Challenges in identifying and managing attention-deficit/hyperactivity disorder in adults in the primary care setting: a review of the literature". Prim Care Companion J Clin Psychiatry. 12 (6). doi:10.4088/PCC.10r00951pur. PMC 3067998. PMID 21494335.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b c d Antshel, KM (2008). "Attention-Deficit Hyperactivity Disorder in the context of a high intellectual quotient/giftedness". Dev Disabil Res Rev. 14 (4): 293–9. doi:10.1002/ddrr.34. PMID 19072757.
External links
- National Institute of Mental Health on ADHD
- "CG72 Attention deficit hyperactivity disorder (ADHD): full guideline" (PDF). NHS. 9 March 2009. Retrieved 8 January 2009.
- New Zealand MOH Guidelines for the Assessment and Treatment of Attention-Deficit/Hyperactivity Disorder
