Malnutrition: Difference between revisions
No edit summary |
in use; merging Hunger (malnutrition) here |
||
| Line 1: | Line 1: | ||
{{in use}} |
|||
{{short description|Medical condition that results from eating too little, too much, or the wrong nutrients}} |
{{short description|Medical condition that results from eating too little, too much, or the wrong nutrients}} |
||
{{redirect|Underfeeding|the concept in metalworking|Underfeeder}} |
{{redirect|Underfeeding|the concept in metalworking|Underfeeder}} |
||
Revision as of 01:31, 30 October 2018
This article is actively undergoing a major edit for a little while. To help avoid edit conflicts, please do not edit this page while this message is displayed. This page was last edited at 01:31, 30 October 2018 (UTC) (6 years ago) – this estimate is cached, . Please remove this template if this page hasn't been edited for a significant time. If you are the editor who added this template, please be sure to remove it or replace it with {{Under construction}} between editing sessions. |
| Malnutrition | |
|---|---|
| Other names | Malnourishment |
 | |
| An orange ribbon—the awareness ribbon for malnutrition. | |
| Specialty | Critical care medicine |
| Symptoms | Problems with physical or mental development, poor energy levels, swollen legs and abdomen[1][2] |
| Causes | Eating a diet in which nutrients are either not enough or are too much, malabsorption[3][4] |
| Risk factors | Not breastfeed, gastroenteritis, pneumonia, malaria, measles[5] |
| Prevention | Improving agricultural practices, reducing poverty, improving sanitation, empowerment of women[6][7] |
| Treatment | Improved nutrition, supplementation, ready-to-use therapeutic foods, treating the underlying cause[6][8][9] |
| Frequency | 815 million undernourished / 11% of the population (2017)[10] |
| Deaths | 406,000 from nutritional deficiencies (2015)[11] |
Malnutrition is a condition that results from eating a diet in which one or more nutrients are either not enough or are too much such that the diet causes health problems.[1][3] It may involve calories, protein, carbohydrates, vitamins or minerals.[1] Not enough nutrients is called undernutrition or undernourishment while too much is called overnutrition.[2] Malnutrition is often used to specifically refer to undernutrition where an individual is not getting enough calories, protein, or micronutrients.[2][12] If undernutrition occurs during pregnancy, or before two years of age, it may result in permanent problems with physical and mental development.[1] Extreme undernourishment, known as starvation, may have symptoms that include: a short height, thin body, very poor energy levels, and swollen legs and abdomen.[1][2] People also often get infections and are frequently cold.[2] The symptoms of micronutrient deficiencies depend on the micronutrient that is lacking.[2]
Undernourishment is most often due to not enough high-quality food being available to eat.[5] This is often related to high food prices and poverty.[1][5] A lack of breastfeeding may contribute, as may a number of infectious diseases such as: gastroenteritis, pneumonia, malaria, and measles, which increase nutrient requirements.[5] There are two main types of undernutrition: protein-energy malnutrition and dietary deficiencies.[12] Protein-energy malnutrition has two severe forms: marasmus (a lack of protein and calories) and kwashiorkor (a lack of just protein).[2] Common micronutrient deficiencies include: a lack of iron, iodine, and vitamin A.[2] During pregnancy, due to the body's increased need, deficiencies may become more common.[13] In some developing countries, overnutrition in the form of obesity is beginning to present within the same communities as undernutrition.[14] Other causes of malnutrition include anorexia nervosa and bariatric surgery.[15][16]
Efforts to improve nutrition are some of the most effective forms of development aid.[6] Breastfeeding can reduce rates of malnutrition and death in children,[1] and efforts to promote the practice increase the rates of breastfeeding.[8] In young children, providing food (in addition to breastmilk) between six months and two years of age improves outcomes.[8] There is also good evidence supporting the supplementation of a number of micronutrients to women during pregnancy and among young children in the developing world.[8] To get food to people who need it most, both delivering food and providing money so people can buy food within local markets are effective.[6][17] Simply feeding students at school is insufficient.[6] Management of severe malnutrition within the person's home with ready-to-use therapeutic foods is possible much of the time.[8] In those who have severe malnutrition complicated by other health problems, treatment in a hospital setting is recommended.[8] This often involves managing low blood sugar and body temperature, addressing dehydration, and gradual feeding.[8][18] Routine antibiotics are usually recommended due to the high risk of infection.[18] Longer-term measures include: improving agricultural practices,[7] reducing poverty, improving sanitation, and the empowerment of women.[6]
There were 815 million undernourished people in the world in 2017 (11% of the total population).[10] This is a reduction of 176 million people since 1990 when 23% were undernourished.[10][19] In 2012 it was estimated that another billion people had a lack of vitamins and minerals.[6] In 2015, protein-energy malnutrition was estimated to have resulted in 323,000 deaths—down from 510,000 deaths in 1990.[11][20] Other nutritional deficiencies, which include iodine deficiency and iron deficiency anemia, result in another 83,000 deaths.[11] In 2010, malnutrition was the cause of 1.4% of all disability adjusted life years.[6][21] About a third of deaths in children are believed to be due to undernutrition, although the deaths are rarely labelled as such.[5] In 2010, it was estimated to have contributed to about 1.5 million deaths in women and children,[22] though some estimate the number may be greater than 3 million.[8] An additional 165 million children were estimated to have stunted growth from malnutrition in 2013.[8] Undernutrition is more common in developing countries.[23] Certain groups have higher rates of undernutrition, including women—in particular while pregnant or breastfeeding—children under five years of age, and the elderly. In the elderly, undernutrition becomes more common due to physical, psychological, and social factors.[24]
Definitions

Unless specifically mentioned otherwise, the term malnutrition refers to undernutrition for the remainder of this article. Malnutrition can be divided into two different types, SAM and MAM. SAM refers to children with severe acute malnutrition. MAM refers to moderate acute malnutrition.[25]
Undernutrition and overnutrition
Malnutrition is caused by eating a diet in which nutrients are not enough or is too much such that it causes health problems.[26] It is a category of diseases that includes undernutrition and overnutrition.[27] Overnutrition can result in obesity and being overweight. In some developing countries, overnutrition in the form of obesity is beginning to present within the same communities as undernutrition.[28]
However, the term malnutrition is commonly used to refer to undernutrition only.[29] This applies particularly to the context of development cooperation. Therefore, "malnutrition" in documents by the World Health Organization, UNICEF, Save the Children or other international non-governmental organizations (NGOs) usually is equated to undernutrition.
Protein-energy malnutrition
Undernutrition is sometimes used as a synonym of protein–energy malnutrition (PEM).[2] While other include both micronutrient deficiencies and protein energy malnutrition in its definition.[12] It differs from calorie restriction in that calorie restriction may not result in negative health effects. The term hypoalimentation means underfeeding.[30]
The term "severe malnutrition" or "severe undernutrition" is often used to refer specifically to PEM.[31] PEM is often associated with micronutrient deficiency.[31] Two forms of PEM are kwashiorkor and marasmus, and they commonly coexist.[26]
Kwashiorkor
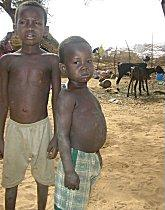
Kwashiorkor is mainly caused by inadequate protein intake.[26] The main symptoms are edema, wasting, liver enlargement, hypoalbuminaemia, steatosis, and possibly depigmentation of skin and hair.[26] Kwashiorkor is further identified by swelling of the belly, which is deceiving of actual nutritional status.[32] The term means ‘displaced child’ and is derived from a Ghana language of West Africa, means "the sickness the older one gets when the next baby is born," as this is when the older child is deprived of breast feeding and weaned to a diet composed largely of carbohydrates.[33]
Marasmus
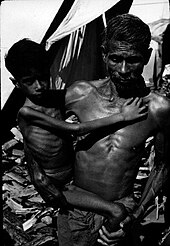
Marasmus (‘to waste away’) is caused by an inadequate intake of protein and energy. The main symptoms are severe wasting, leaving little or no edema, minimal subcutaneous fat, severe muscle wasting, and non-normal serum albumin levels.[26] Marasmus can result from a sustained diet of inadequate energy and protein, and the metabolism adapts to prolong survival.[26] It is traditionally seen in famine, significant food restriction, or more severe cases of anorexia.[26] Conditions are characterized by extreme wasting of the muscles and a gaunt expression.[32]
Undernutrition, hunger
Undernutrition encompasses stunted growth (stunting), wasting, and deficiencies of essential vitamins and minerals (collectively referred to as micronutrients). The term hunger, which describes a feeling of discomfort from not eating, has been used to describe undernutrition, especially in reference to food insecurity.[34]
Definition by Gomez
In 1956, Gómez and Galvan studied factors associated with death in a group of malnourished (undernourished) children in a hospital in Mexico City, Mexico and defined categories of malnutrition: first, second, and third degree.[35] The degrees were based on weight below a specified percentage of median weight for age.[36] The risk of death increases with increasing degree of malnutrition.[35] An adaptation of Gomez's original classification is still used today. While it provides a way to compare malnutrition within and between populations, the classification has been criticized for being "arbitrary" and for not considering overweight as a form of malnutrition. Also, height alone may not be the best indicator of malnutrition; children who are born prematurely may be considered short for their age even if they have good nutrition.[37]
| Degree of PEM | % of desired body weight for age and sex | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Normal | 90%-100% | ||||||||||||||
| Mild: Grade I (1st degree) | 75%-89% | ||||||||||||||
| Moderate: Grade II (2nd degree) | 60%-74% | ||||||||||||||
| Severe: Grade III (3rd degree) | <60% | ||||||||||||||
| SOURCE:"Serum Total Protein and Albumin Levels in Different Grades of Protein Energy Malnutrition"[32] | |||||||||||||||
Definition by Waterlow
John Conrad Waterlow established a new classification for malnutrition.[38] Instead of using just weight for age measurements, the classification established by Waterlow combines weight-for-height (indicating acute episodes of malnutrition) with height-for-age to show the stunting that results from chronic malnutrition.[39] One advantage of the Waterlow classification over the Gomez classification is that weight for height can be examined even if ages are not known.[38]
| Degree of PEM | Stunting (%) Height for age | Wasting (%) Weight for height | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Normal: Grade 0 | >95% | >90% | |||||||||||||
| Mild: Grade I | 87.5-95% | 80-90% | |||||||||||||
| Moderate: Grade II | 80-87.5% | 70-80% | |||||||||||||
| Severe: Grade III | <80% | <70% | |||||||||||||
| SOURCE: "Classification and definition of protein-calorie malnutrition." by Waterlow, 1972[38] | |||||||||||||||
These classifications of malnutrition are commonly used with some modifications by WHO.[36]
Effects

Malnutrition increases the risk of infection and infectious disease, and moderate malnutrition weakens every part of the immune system.[40] For example, it is a major risk factor in the onset of active tuberculosis.[41] Protein and energy malnutrition and deficiencies of specific micronutrients (including iron, zinc, and vitamins) increase susceptibility to infection.[40] Malnutrition affects HIV transmission by increasing the risk of transmission from mother to child and also increasing replication of the virus.[40] In communities or areas that lack access to safe drinking water, these additional health risks present a critical problem. Lower energy and impaired function of the brain also represent the downward spiral of malnutrition as victims are less able to perform the tasks they need to in order to acquire food, earn an income, or gain an education.
Vitamin-deficiency-related diseases (such as scurvy and rickets).
Hypoglycemia (low blood sugar) can result from a child not eating for 4 to 6 hours. Hypoglycemia should be considered if there is lethargy, limpness, convulsion, or loss of consciousness. If blood sugar can be measured immediately and quickly, perform a finger or heel stick.
Signs
In those with malnutrition some of the signs of dehydration differ.[42] Children; however, may still be interested in drinking, have decreased interactions with the world around them, have decreased urine output, and may be cool to touch.[42]
| Site | Sign | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Face | Moon face (kwashiorkor), simian facies (marasmus) | ||||||||||||||
| Eye | Dry eyes, pale conjunctiva, Bitot's spots (vitamin A), periorbital edema | ||||||||||||||
| Mouth | Angular stomatitis, cheilitis, glossitis, spongy bleeding gums (vitamin C), parotid enlargement | ||||||||||||||
| Teeth | Enamel mottling, delayed eruption | ||||||||||||||
| Hair | Dull, sparse, brittle hair, hypopigmentation, flag sign (alternating bands of light and normal color), broomstick eyelashes, alopecia | ||||||||||||||
| Skin | Loose and wrinkled (marasmus), shiny and edematous (kwashiorkor), dry, follicular hyperkeratosis, patchy hyper- and hypopigmentation, erosions, poor wound healing | ||||||||||||||
| Nail | Koilonychia, thin and soft nail plates, fissures or ridges | ||||||||||||||
| Musculature | Muscles wasting, particularly in the buttocks and thighs | ||||||||||||||
| Skeletal | Deformities usually a result of calcium, vitamin D, or vitamin C deficiencies | ||||||||||||||
| Abdomen | Distended - hepatomegaly with fatty liver, ascites may be present | ||||||||||||||
| Cardiovascular | Bradycardia, hypotension, reduced cardiac output, small vessel vasculopathy | ||||||||||||||
| Neurologic | Global development delay, loss of knee and ankle reflexes, poor memory | ||||||||||||||
| Hematological | Pallor, petechiae, bleeding diathesis | ||||||||||||||
| Behavior | Lethargic, apathetic | ||||||||||||||
| Source: "Protein Energy Malnutrition"[36] | |||||||||||||||
Cognitive development
Protein-calorie malnutrition can cause cognitive impairments. For humans, "critical period varies from the final third of gestation to the first 2 years of life".[43] Iron deficiency anemia in children under two years of age likely affects brain function acutely and probably also chronically. Folate deficiency has been linked to neural tube defects.[44]
Malnutrition in the form of iodine deficiency is "the most common preventable cause of mental impairment worldwide."[45][citation needed] "Even moderate deficiency, especially in pregnant women and infants, lowers intelligence by 10 to 15 I.Q. points, shaving incalculable potential off a nation's development. The most visible and severe effects — disabling goiters, cretinism and dwarfism — affect a tiny minority, usually in mountain villages. But 16 percent of the world's people have at least mild goiter, a swollen thyroid gland in the neck."[45]
Causes

Major causes of malnutrition include poverty and food prices, dietary practices and agricultural productivity, with many individual cases being a mixture of several factors. Clinical malnutrition, such as cachexia, is a major burden also in developed countries. Various scales of analysis also have to be considered in order to determine the sociopolitical causes of malnutrition. For example, the population of a community that is within poor governments, may be at risk if the area lacks health-related services, but on a smaller scale certain households or individuals may be at an even higher risk due to differences in income levels, access to land, or levels of education.[46]
Diseases
Malnutrition can be a consequence of health issues such as gastroenteritis[47] or chronic illness,[48] especially the HIV/AIDS pandemic.[49] Diarrhea and other infections can cause malnutrition through decreased nutrient absorption, decreased intake of food, increased metabolic requirements, and direct nutrient loss.[50] Parasite infections, in particular intestinal worm infections (helminthiasis), can also lead to malnutrition.[50] A leading cause of diarrhea and intestinal worm infections in children in developing countries is lack of sanitation and hygiene.
People may become malnourished due to abnormal nutrient loss (due to diarrhea or chronic illness affecting the small bowel).[36][51] This conditions may include Crohn's disease or untreated coeliac disease.[4][9][52] Malnutrition may also occur due to increased energy expenditure (secondary malnutrition).[36][51]
Dietary practices
Undernutrition
A lack of adequate breastfeeding leads to malnutrition in infants and children, associated with the deaths of an estimated one million children annually. Illegal advertising of breast milk substitutes contributed to malnutrition and continued three decades after its 1981 prohibition under the WHO International Code of Marketing Breast Milk Substitutes.[53]
Maternal malnutrition can also factor into the poor health or death of a baby. Over 800,000 neonatal death have occurred because of deficient growth of the fetus in the mother's womb.[54]
Deriving too much of one's diet from a single source, such as eating almost exclusively corn or rice, can cause malnutrition. This may either be from a lack of education about proper nutrition, or from only having access to a single food source.[55]
It is not just the total amount of calories that matters but specific nutritional deficiencies such as vitamin A deficiency, iron deficiency or zinc deficiency can also increase risk of death.[56]
Overnutrition
Overnutrition caused by overeating is also a form of malnutrition. In the United States, more than half of all adults are now overweight — a condition that, like hunger, increases susceptibility to disease and disability, reduces worker productivity, and lowers life expectancy.[57] Overeating is much more common in the United States, where for the majority of people, access to food is not an issue. Many parts of the world have access to a surplus of non-nutritious food, in addition to increased sedentary lifestyles. Yale psychologist Kelly Brownell calls this a "toxic food environment" where fat and sugar laden foods have taken precedence over healthy nutritious foods.[57]
The issue in these developed countries is choosing the right kind of food. More fast food is consumed per capita in the United States than in any other country. The reason for this mass consumption of fast food is its affordability and accessibility. Often fast food, low in cost and nutrition, is high in calories and heavily promoted. When these eating habits are combined with increasingly urbanized, automated, and more sedentary lifestyles, it becomes clear why weight gain is difficult to avoid.[58]
Not only does obesity occur in developed countries, problems are also occurring in developing countries in areas where income is on the rise.[57] Overeating is also a problem in countries where hunger and poverty persist. In China, consumption of high-fat foods has increased while consumption of rice and other goods has decreased.[57]
Overeating leads to many diseases, such as heart disease and diabetes, that may result in death.
Poverty and food prices
In Bangladesh, poor socioeconomic position was associated with chronic malnutrition since it inhibits purchase of nutritious foods such as milk, meat, poultry, and fruits.[59] As much as food shortages may be a contributing factor to malnutrition in countries with lack of technology, the FAO (Food and Agriculture Organization) has estimated that eighty percent of malnourished children living in the developing world live in countries that produce food surpluses.[57] The economist Amartya Sen observed that, in recent decades, famine has always been a problem of food distribution and/or poverty, as there has been sufficient food to feed the whole population of the world. He states that malnutrition and famine were more related to problems of food distribution and purchasing power.[60]
It is argued that commodity speculators are increasing the cost of food. As the real estate bubble in the United States was collapsing, it is said that trillions of dollars moved to invest in food and primary commodities, causing the 2007–2008 food price crisis.[61]
The use of biofuels as a replacement for traditional fuels raises the price of food.[62] The United Nations special rapporteur on the right to food, Jean Ziegler proposes that agricultural waste, such as corn cobs and banana leaves, rather than crops themselves be used as fuel.[63]
Agricultural productivity
Local food shortages can be caused by a lack of arable land, adverse weather, lower farming skills such as crop rotation, or by a lack of technology or resources needed for the higher yields found in modern agriculture, such as fertilizers, pesticides, irrigation, machinery and storage facilities. As a result of widespread poverty, farmers cannot afford or governments cannot provide the resources necessary to improve local yields. The World Bank and some wealthy donor countries also press nations that depend on aid to cut or eliminate subsidized agricultural inputs such as fertilizer, in the name of free market policies even as the United States and Europe extensively subsidized their own farmers.[64][65] Many, if not most, farmers cannot afford fertilizer at market prices, leading to low agricultural production and wages and high, unaffordable food prices.[64] Reasons for the unavailability of fertilizer include moves to stop supplying fertilizer on environmental grounds, cited as the obstacle to feeding Africa by the Green Revolution pioneers Norman Borlaug and Keith Rosenberg.[66]
Future threats
There are a number of potential disruptions to global food supply that could cause widespread malnutrition.
Global warming is of importance to food security, with 95 percent of all malnourished peoples living in the relatively stable climate region of the sub-tropics and tropics. According to the latest IPCC reports, temperature increases in these regions are "very likely."[67] Even small changes in temperatures can lead to increased frequency of extreme weather conditions.[67] Many of these have great impact on agricultural production and hence nutrition. For example, the 1998–2001 central Asian drought brought about an 80 percent livestock loss and 50 percent reduction in wheat and barley crops in Iran.[68] Similar figures were present in other nations. An increase in extreme weather such as drought in regions such as Sub-Saharan Africa would have even greater consequences in terms of malnutrition. Even without an increase of extreme weather events, a simple increase in temperature reduces the productivity of many crop species, also decreasing food security in these regions.[67][69]
Colony collapse disorder is a phenomenon where bees die in large numbers.[70] Since many agricultural crops worldwide are pollinated by bees, this represents a threat to the supply of food.[71]
An epidemic of wheat stem rust caused by race Ug99 is currently spreading across Africa and into Asia and, it is feared, could wipe out more than 80 percent of the world’s wheat crops.[72][73]
Prevention

Food security
The effort to bring modern agricultural techniques found in the West, such as nitrogen fertilizers and pesticides, to Asia, called the Green Revolution, resulted in decreases in malnutrition similar to those seen earlier in Western nations. This was possible because of existing infrastructure and institutions that are in short supply in Africa, such as a system of roads or public seed companies that made seeds available.[74] Investments in agriculture, such as subsidized fertilizers and seeds, increases food harvest and reduces food prices.[64][75] For example, in the case of Malawi, almost five million of its 13 million people used to need emergency food aid. However, after the government changed policy and subsidies for fertilizer and seed were introduced against World Bank strictures, farmers produced record-breaking corn harvests as production leaped to 3.4 million in 2007 from 1.2 million in 2005, making Malawi a major food exporter.[64] This lowered food prices and increased wages for farm workers.[64] Such investments in agriculture are still needed in other African countries like the Democratic Republic of the Congo. The country has one of the highest prevalence of malnutrition even though it is blessed with great agricultural potential John Ulimwengu explains in his article for D+C.[76] Proponents for investing in agriculture include Jeffrey Sachs, who has championed the idea that wealthy countries should invest in fertilizer and seed for Africa’s farmers.[64][77]
In Nigeria, the use of imported Ready to Use Therapeutic Food (RUTF) has been used to treat malnutrition in the North. Soy Kunu, a locally sourced and prepared blend consisting of peanut, millet and soya beans may also be used.[78]
New technology in agricultural production also has great potential to combat undernutrition.[79] By improving agricultural yields, farmers could reduce poverty by increasing income as well as open up area for diversification of crops for household use. The World Bank itself claims to be part of the solution to malnutrition, asserting that the best way for countries to succeed in breaking the cycle of poverty and malnutrition is to build export-led economies that will give them the financial means to buy foodstuffs on the world market.
Economics
There is a growing realization among aid groups that giving cash or cash vouchers instead of food is a cheaper, faster, and more efficient way to deliver help to the hungry, particularly in areas where food is available but unaffordable.[80] The UN's World Food Program, the biggest non-governmental distributor of food, announced that it will begin distributing cash and vouchers instead of food in some areas, which Josette Sheeran, the WFP's executive director, described as a "revolution" in food aid.[80][81] The aid agency Concern Worldwide is piloting a method through a mobile phone operator, Safaricom, which runs a money transfer program that allows cash to be sent from one part of the country to another.[80]
However, for people in a drought living a long way from and with limited access to markets, delivering food may be the most appropriate way to help.[80] Fred Cuny stated that "the chances of saving lives at the outset of a relief operation are greatly reduced when food is imported. By the time it arrives in the country and gets to people, many will have died."[82] U.S. law, which requires buying food at home rather than where the hungry live, is inefficient because approximately half of what is spent goes for transport.[83] Cuny further pointed out "studies of every recent famine have shown that food was available in-country — though not always in the immediate food deficit area" and "even though by local standards the prices are too high for the poor to purchase it, it would usually be cheaper for a donor to buy the hoarded food at the inflated price than to import it from abroad."[84]
Ethiopia has been pioneering a program that has now become part of the World Bank's prescribed method for coping with a food crisis and had been seen by aid organizations as a model of how to best help hungry nations. Through the country's main food assistance program, the Productive Safety Net Program, Ethiopia has been giving rural residents who are chronically short of food, a chance to work for food or cash. Foreign aid organizations like the World Food Program were then able to buy food locally from surplus areas to distribute in areas with a shortage of food.[85] Ethiopia been pioneering a program, and Brazil has established a recycling program for organic waste that benefits farmers, urban poor, and the city in general. City residents separate organic waste from their garbage, bag it, and then exchange it for fresh fruit and vegetables from local farmers. As a result, the country's waste is reduced and the urban poor get a steady supply of nutritious food.[58]
World population
Restricting population size is a proposed solution. Thomas Malthus argued that population growth could be controlled by natural disasters and voluntary limits through "moral restraint."[86] Robert Chapman suggests that an intervention through government policies is a necessary ingredient of curtailing global population growth.[87] The interdependence and complementarity of population growth with poverty and malnutrition (as well as the environment) is also recognised by the United Nations.[88] More than 200 million women worldwide do not have adequate access to family planning services. According to the World Health Organisation, "Family planning is key to slowing unsustainable population growth and the resulting negative impacts on the economy, environment, and national and regional development efforts".[89]
However, there are many who believe that the world has more than enough resources to sustain its population. Instead, these theorists point to unequal distribution of resources and under- or unutilized arable land as the cause for malnutrition problems.[90][91] For example, Amartya Sen advocates that, "no matter how a famine is caused, methods of breaking it call for a large supply of food in the public distribution system. This applies not only to organizing rationing and control, but also to undertaking work programmes and other methods of increasing purchasing power for those hit by shifts in exchange entitlements in a general inflationary situation."[60]
Food sovereignty
One suggested policy framework to resolve access issues is termed food sovereignty—the right of peoples to define their own food, agriculture, livestock, and fisheries systems, in contrast to having food largely subjected to international market forces. Food First is one of the primary think tanks working to build support for food sovereignty. Neoliberals advocate for an increasing role of the free market.
Health facilities
Another possible long term solution would be to increase access to health facilities to rural parts of the world. These facilities could monitor undernourished children, act as supplemental food distribution centers, and provide education on dietary needs. These types of facilities have already proven very successful in countries such as Peru and Ghana.[92][93]
Breastfeeding
As of 2016 is estimated that about 821,000 deaths of children less than five years old could be prevented globally per year through more widespread breastfeeding.[94] In addition to reducing infant death, breast milk feeding provides an important source of micronutrients, clinically proven to bolster the immune system of children, and provide long-term defenses against non-communicable and allergic diseases.[95] Breastfeeding has also been shown to improve cognitive abilities in children, with a strong correlation to individual educational achievements.[95][96] As previously noted, lack of proper breastfeeding is a major factor in child mortality rates, and a primary determinant of disease development for children. The medical community recommends exclusively breastfeeding infants for 6 months, with nutritional whole food supplementation and continued breastfeeding up to 2 years or older for overall optimal health outcomes.[96][97][98] Exclusive breastfeeding is defined as only giving an infant breast milk for six months as a source of food and nutrition.[96][98] This means no other liquids, including water or semi-solid foods.[98]
Barriers to breastfeeding
Breastfeeding is noted as one of the most cost effective medical interventions for providing beneficial child health.[97] While there are considerable differences within developed and developing countries: income, employment, social norms, and access to healthcare were found to be universal determinants of whether a mother breast or formula fed their children.[96][97] Community based healthcare workers have helped alleviate financial barriers faced by newly made mothers, and provided a viable alternative to traditional and expensive hospital based medical care.[96] Recent studies based upon surveys conducted from 1995-2010 shows exclusive breastfeeding rates have gone up globally, from 33% to 39%.[98] Despite the growth rates, medical professionals acknowledge the need for improvement given the importance of exclusive breastfeeding.[98]
Global initiatives
Food security and global malnutrition has long been a topic of international concern, with one of the first official global documents addressing it being the 1948 Universal Declaration of Human Rights(UDHR). Within this document it stated that access to food was part of an adequate right to a standard of living.[99] The Right to food was asserted in the International Covenant on Economic, Social and Cultural Rights, a treaty adopted by the United Nations General Assembly on December 16, 1966. The Right to food is a human right for people to feed themselves in dignity, be free from hunger, food insecurity, and malnutrition.[100] As of 2018, the treaty has been signed by 166 countries, by signing states agreed to take steps to the maximum of their available resources to achieve the right to adequate food.
However, after the 1966 International Covenant the global concern for the access to sufficient food only became more present, leading to the first ever World Food Conference that was held in 1974 in Rome, Italy. The Universal Declaration on the Eradication of Hunger and Malnutrition was a UN resolution adopted November 16, 1974 by all 135 countries that attended the 1974 World Food Conference.[101] This non-legally binding document set forth certain aspirations for countries to follow to sufficiently take action on the global food problem. Ultimately this document outline and provided guidance as to how the international community as one could work towards fighting and solving the growing global issue of malnutrition and hunger.
Adoption of the right to food was included in the Additional Protocol to the American Convention on Human Rights in the area of Economic, Social, and Cultural Rights, this 1978 document was adopted by many countries in the Americas, the purpose of the document is, "to consolidate in this hemisphere, within the framework of democratic institutions, a system of personal liberty and social justice based on respect for the essential rights of man."[102]
The next document in the timeline of global inititaves for malnutrition was the 1996 Rome Declaration on World Food Security, organized by the Food and Agriculture Organization. This document reaffirmed the right to have access to safe and nutritous food by everyone, also considering that everyone gets sufficient food, and set the goals for all nations to improve their commitment to food security by halfing their amount of undernourished people by 2015.[103] In 2004 the Food and Agriculture Organization adopted the Right to Food Guidelines, which offered states a framework of how to increase the right to food on a national basis.
One of the most recent and powerful global policies to reduce hunger and poverty are the Sustainable Development Goals. In particular Goal 2: Zero hunger sets globally agreed targets to end hunger, achieve food security and improved nutrition and promote sustainable agriculture.[104] The partnership Compact2025, led by IFPRI with the involvement of UN organisations, NGOs and private foundations develops and disseminates evidence-based advice to politicians and other decision-makers aimed at ending hunger and undernutrition in the coming 10 years, by 2025.[105][106]
In April 2012, the Food Assistance Convention was signed, the world's first legally binding international agreement on food aid. The May 2012 Copenhagen Consensus recommended that efforts to combat hunger and malnutrition should be the first priority for politicians and private sector philanthropists looking to maximize the effectiveness of aid spending. They put this ahead of other priorities, like the fight against malaria and AIDS.[107]
The EndingHunger campaign is an online communication campaign aimed at raising awareness of the hunger problem. It has many worked through viral videos depicting celebrities voicing their anger about the large number of hungry people in the world. Another initiative focused on improving the hunger situation by improving nutrition is the Scaling up Nutrition movement (SUN). Started in 2010 this movement of people from governments, civil society, the United Nations, donors, businesses and researchers, publishes a yearly progress report on the changes in their 55 partner countries.[108]
Treatment


In response to child malnutrition, the Bangladeshi government recommends ten steps for treating severe malnutrition. They are to prevent or treat dehydration, low blood sugar, low body temperature, infection, correct electrolyte imbalances and micronutrient deficiencies, start feeding cautiously, achieve catch-up growth, provide psychological support, and prepare for discharge and follow-up after recovery.[109]
Among those who are hospitalized, nutritional support improves protein, calorie intake and weight.[110]
Food
The evidence for benefit of supplementary feeding is poor.[111] This is due to the small amount of research done on this treatment.
Specially formulated foods do however appear useful in those from the developing world with moderate acute malnutrition.[112] In young children with severe acute malnutrition it is unclear if ready-to-use therapeutic food differs from a normal diet.[113] They may have some benefits in humanitarian emergencies as they can be eaten directly from the packet, do not require refrigeration or mixing with clean water, and can be stored for years.[114]
In those who are severely malnourished, feeding too much too quickly can result in refeeding syndrome.[115] This can result regardless of route of feeding and can present itself a couple of days after eating with heart failure, dysrhythmias and confusion that can result in death.[115][116]
Manufacturers are trying to fortify everyday foods with micronutrients that can be sold to consumers such as wheat flour for Beladi bread in Egypt or fish sauce in Vietnam and the iodization of salt.[114]
For example, flour has been fortified with iron, zinc, folic acid and other B vitamins such as thiamine, riboflavin, niacin and vitamin B12.[56]
Micronutrients
Treating malnutrition, mostly through fortifying foods with micronutrients (vitamins and minerals), improves lives at a lower cost and shorter time than other forms of aid, according to the World Bank.[117] The Copenhagen Consensus, which look at a variety of development proposals, ranked micronutrient supplements as number one.[118][83]
In those with diarrhea, once an initial four-hour rehydration period is completed, zinc supplementation is recommended. Daily zinc increases the chances of reducing the severity and duration of the diarrhea, and continuing with daily zinc for ten to fourteen days makes diarrhea less likely recur in the next two to three months.[119]
In addition, malnourished children need both potassium and magnesium.[109] This can be obtained by following the above recommendations for the dehydrated child to continue eating within two to three hours of starting rehydration,[109][119] and including foods rich in potassium as above. Low blood potassium is worsened when base (as in Ringer's/Hartmann's) is given to treat acidosis without simultaneously providing potassium.[119] As above, available home products such as salted and unsalted cereal water, salted and unsalted vegetable broth can be given early during the course of a child's diarrhea along with continued eating.[119] Vitamin A, potassium, magnesium, and zinc should be added with other vitamins and minerals if available.[109]
For a malnourished child with diarrhea from any cause, this should include foods rich in potassium such as bananas, green coconut water, and unsweetened fresh fruit juice.[119]
Diarrhea

The World Health Organization (WHO) recommends rehydrating a severely undernourished child who has diarrhea relatively slowly. The preferred method is with fluids by mouth using a drink called oral rehydration solution (ORS). The oral rehydration solution is both slightly sweet and slightly salty and the one recommended in those with severe undernutrition should have half the usual sodium and greater potassium. Fluids by nasogastric tube may be use in those who do not drink. Intravenous fluids are recommended only in those who have significant dehydration due to their potential complications. These complications include congestive heart failure.[42] Over time, ORS developed into ORT, or oral rehydration therapy, which focused on increasing fluids by supplying salts, carbohydrates, and water. This switch from type of fluid to amount of fluid was crucial in order to prevent dehydration from diarrhea.[120]
Breast feeding and eating should resume as soon as possible.[42] Drinks such as soft drinks, fruit juices, or sweetened teas are not recommended as they contain too much sugar and may worsen diarrhea.[121] Broad spectrum antibiotics are recommended in all severely undernourished children with diarrhea requiring admission to hospital.[42]
To prevent dehydration readily available fluids, preferably with a modest amount of sugars and salt such as vegetable broth or salted rice water, may be used. The drinking of additional clean water is also recommended. Once dehydration develops oral rehydration solutions are preferred. As much of these drinks as the person wants can be given, unless there are signs of swelling. If vomiting occurs, fluids can be paused for 5–10 minutes and then restarting more slowly. Vomiting rarely prevents rehydration as fluid are still absorbed and the vomiting rarely last long.[121] A severely malnourished child with what appears to be dehydration but who has not had diarrhea should be treated as if they have an infection.[42]
For babies a dropper or syringe without the needle can be used to put small amounts of fluid into the mouth; for children under 2, a teaspoon every one to two minutes; and for older children and adults, frequent sips directly from a cup.[119] After the first two hours, rehydration should be continued at the same or slower rate, determined by how much fluid the child wants and any ongoing diarrheal loses. After the first two hours of rehydration it is recommended that to alternate between rehydration and food.[109]
In 2003, WHO and UNICEF recommended a reduced-osmolarity ORS which still treats dehydration but also reduced stool volume and vomiting. Reduced-osmolarity ORS is the current standard ORS with reasonably wide availability.[122][123] For general use, one packet of ORS (glucose sugar, salt, potassium chloride, and trisodium citrate) is added to one liter of water; however, for malnourished children it is recommended that one packet of ORS be added to two liters of water along with an extra 50 grams of sucrose sugar and some stock potassium solution.[124]
Malnourished children have an excess of body sodium.[109] Recommendations for home remedies agree with one liter of water (34 oz.) and 6 teaspoons sugar and disagree regarding whether it is then one teaspoon of salt added or only 1/2, with perhaps most sources recommending 1/2 teaspoon of added salt to one liter water.[119][125][126][127]
Low blood sugar
Hypoglycemia, whether known or suspected, can be treated with a mixture of sugar and water. If the child is conscious, the initial dose of sugar and water can be given by mouth.[128] If the child is unconscious, give glucose by intravenous or nasogastric tube. If seizures occur after despite glucose, rectal diazepam is recommended. Blood sugar levels should be re-checked on two hour intervals.[109]
Hypothermia
Hypothermia can occur. To prevent or treat this, the child can be kept warm with covering including of the head or by direct skin-to-skin contact with the mother or father and then covering both parent and child. Prolonged bathing or prolonged medical exams should be avoided. Warming methods are usually most important at night.[109]
Epidemiology


| no data <200 200-400 400-600 600-800 800-1000 1000-1200 | 1200-1400 1400-1600 1600-1800 1800-2000 2000-2200 >2200 |
The figures provided in this section on epidemiology all refer to undernutrition even if the term malnutrition is used which, by definition, could also apply to too much nutrition.
People affected
There were 815 million undernourished people in the world in 2017.[10] This was 176 million fewer people than in 1990 when it was 991 million undernourished people.[10] This is despite the world's farmers producing enough food to feed around 12 billion people – almost double the current world population.[130]
Malnutrition, as of 2010, was the cause of 1.4% of all disability adjusted life years.[21]
| Year | 1970 | 1980 | 1990 | 1995 | 2005 | 2007/08 | 2014/16 |
|---|---|---|---|---|---|---|---|
| Number in millions[131][132] | 843 | 788 | 848 | 923 | 793 | ||
| Percentage in the developing world[131][133][134] | 37% | 28% | 20% | 16% | 17% | 13.5% |
Mortality

Mortality due to malnutrition accounted for 58 percent of the total mortality in 2006: "In the world, approximately 62 million people, all causes of death combined, die each year. One in twelve people worldwide is malnourished and according to the Save the Children 2012 report, one in four of the world’s children are chronically malnourished.[135] In 2006, more than 36 million died of hunger or diseases due to deficiencies in micronutrients".[136]
In 2010 protein-energy malnutrition resulted in 600,000 deaths down from 883,000 deaths in 1990.[137] Other nutritional deficiencies, which include iodine deficiency and iron deficiency anemia, result in another 84,000 deaths.[137] In 2010 malnutrition caused about 1.5 million deaths in women and children.[22]
According to the World Health Organization, malnutrition is the biggest contributor to child mortality, present in half of all cases.[138] Six million children die of hunger every year.[139] Underweight births and intrauterine growth restrictions cause 2.2 million child deaths a year. Poor or non-existent breastfeeding causes another 1.4 million. Other deficiencies, such as lack of vitamin A or zinc, for example, account for 1 million. Malnutrition in the first two years is irreversible. Malnourished children grow up with worse health and lower education achievement. Their own children tend to be smaller. Malnutrition was previously[when?] seen as something that exacerbates the problems of diseases such as measles, pneumonia and diarrhea, but malnutrition actually causes diseases, and can be fatal in its own right.[138]
Society and culture
Roughly $300 million of aid goes to basic nutrition each year, less than $2 for each child below two in the 20 worst affected countries.[138] In contrast, HIV/AIDS, which causes fewer deaths than child malnutrition, received $2.2 billion—$67 per person with HIV in all countries.[138]
The International Crops Research Institute for the Semi-Arid Tropics (ICRISAT), a member of the CGIAR consortium, partners with farmers, governments, researchers and NGOs to help farmers grow nutritious crops, such as chickpea, groundnut, pigeonpea, millet and sorghum. This helps their communities have more balanced diets and become more resilient to pests and drought. The Harnessing Opportunities for Productivity Enhancement of Sorghum and Millets in Sub-Saharan Africa and the Indian-Subcontinent (HOPE) project, for example, is increasing yields of finger millet in Tanzania by encouraging farmers to grow improved varieties. Finger millet is very high in calcium, rich in iron and fiber, and has a better energy content than other cereals. These characteristics make it ideal for feeding to infants and the elderly.[140]
Some organizations have begun working with teachers, policymakers, and managed food service contractors to mandate improved nutritional content and increased nutritional resources in school cafeterias from primary to university-level institutions. Health and nutrition have been proven to have close links with overall educational success.[141]
The verb form is "malnourish"; "malnourishment" is sometimes used instead of "malnutrition."
Special populations
Undernutrition is an important determinant of maternal and child health, accounting for more than a third of child deaths and more than 10 percent of the total global disease burden according to 2008 studies.[34]
Children
The World Health Organization estimates that malnutrition accounts for 54 percent of child mortality worldwide,[31] about 1 million children.[142] Another estimate also by WHO states that childhood underweight is the cause for about 35% of all deaths of children under the age of five years worldwide.[143]
As underweight children are more vulnerable to almost all infectious diseases, the indirect disease burden of malnutrition is estimated to be an order of magnitude higher than the disease burden of the direct effects of malnutrition.[143] The combination of direct and indirect deaths from malnutrition caused by unsafe water, sanitation and hygiene (WASH) practices is estimated to lead to 860,000 deaths per year in children under five years of age.[143]
Women
Gender
Researchers from the Centre for World Food Studies in 2003 found that the gap between levels of undernutrition in men and women is generally small, but that the gap varies from region to region and from country to country.[144] These small-scale studies showed that female undernutrition prevalence rates exceeded male undernutrition prevalence rates in South/Southeast Asia and Latin America and were lower in Sub-Saharan Africa.[144] Datasets for Ethiopia and Zimbabwe reported undernutrition rates between 1.5 and 2 times higher in men than in women; however, in India and Pakistan, datasets rates of undernutrition were 1.5-2 times higher in women than in men. Intra-country variation also occurs, with frequent high gaps between regional undernutrition rates.[144] Gender inequality in nutrition in some countries such as India is present in all stages of life.[145]
Studies on nutrition concerning gender bias within households look at patterns of food allocation, and one study from 2003 suggested that women often receive a lower share of food requirements than men.[144] Gender discrimination, gender roles, and social norms affecting women can lead to early marriage and childbearing, close birth spacing, and undernutrition, all of which contribute to malnourished mothers.[59]
Within the household, there may be differences in levels of malnutrition between men and women, and these differences have been shown to vary significantly from one region to another, with problem areas showing relative deprivation of women.[144] Samples of 1000 women in India in 2008 demonstrated that malnutrition in women is associated with poverty, lack of development and awareness, and illiteracy.[145] The same study showed that gender discrimination in households can prevent a woman's access to sufficient food and healthcare.[145] How socialization affects the health of women in Bangladesh, Najma Rivzi explains in an article about a research program on this topic.[146] In some cases, such as in parts of Kenya in 2006, rates of malnutrition in pregnant women were even higher than rates in children.[147]
Women in some societies are traditionally given less food than men since men are perceived to have heavier workloads.[148] Household chores and agricultural tasks can in fact be very arduous and require additional energy and nutrients; however, physical activity, which largely determines energy requirements, is difficult to estimate.[144]
Physiology
Women have unique nutritional requirements, and in some cases need more nutrients than men; for example, women need twice as much calcium as men.[148]
Pregnancy and breastfeeding
During pregnancy and breastfeeding, women must ingest enough nutrients for themselves and their child, so they need significantly more protein and calories during these periods, as well as more vitamins and minerals (especially iron, iodine, calcium, folic acid, and vitamins A, C, and K).[148] In 2001 the FAO of the UN reported that iron deficiency afflicted 43 percent of women in developing countries and increased the risk of death during childbirth.[148] A 2008 review of interventions estimated that universal supplementation with calcium, iron, and folic acid during pregnancy could prevent 105,000 maternal deaths (23.6 percent of all maternal deaths).[149] Malnutrition has been found to affect three quarters of UK women aged 16-49 indicated by them having less folic acid than the WHO recommended levels.[150]
Frequent pregnancies with short intervals between them and long periods of breastfeeding add an additional nutritional burden.[144]
Educating children
According to the FAO, women are often responsible for preparing food and have the chance to educate their children about beneficial food and health habits, giving mothers another chance to improve the nutrition of their children.[148]
Elderly

Malnutrition and being underweight are more common in the elderly than in adults of other ages.[151] If elderly people are healthy and active, the aging process alone does not usually cause malnutrition.[152] However, changes in body composition, organ functions, adequate energy intake and ability to eat or access food are associated with aging, and may contribute to malnutrition.[153] Sadness or depression can play a role, causing changes in appetite, digestion, energy level, weight, and well-being.[152] A study on the relationship between malnutrition and other conditions in the elderly found that malnutrition in the elderly can result from gastrointestinal and endocrine system disorders, loss of taste and smell, decreased appetite and inadequate dietary intake.[153] Poor dental health, ill-fitting dentures, or chewing and swallowing problems can make eating difficult.[152] As a result of these factors, malnutrition is seen to develop more easily in the elderly.[154]
Rates of malnutrition tend to increase with age with less than 10 percent of the "young" elderly (up to age 75) malnourished, while 30 to 65 percent of the elderly in home care, long-term care facilities, or acute hospitals are malnourished.[155] Many elderly people require assistance in eating, which may contribute to malnutrition.[154] However, the mortality rate due to undernourishment may be reduced.[156] Because of this, one of the main requirements of elderly care is to provide an adequate diet and all essential nutrients.[157] Providing the different nutrients such as protein and energy keeps even small but consistent weight gain.[156]
In Australia malnutrition or risk of malnutrition occurs in 80 percent of elderly people presented to hospitals for admission.[158] Malnutrition and weight loss can contribute to sarcopenia with loss of lean body mass and muscle function.[151] Abdominal obesity or weight loss coupled with sarcopenia lead to immobility, skeletal disorders, insulin resistance, hypertension, atherosclerosis, and metabolic disorders.[153] A paper from the Journal of the American Dietetic Association noted that routine nutrition screenings represent one way to detect and therefore decrease the prevalence of malnutrition in the elderly.[152]
See also
References
- ^ a b c d e f g Facts for life (PDF) (4th ed.). New York: United Nations Children's Fund. 2010. pp. 61 and 75. ISBN 978-92-806-4466-1.
- ^ a b c d e f g h i Young, E.M. (2012). Food and development. Abingdon, Oxon: Routledge. pp. 36–38. ISBN 9781135999414.
- ^ a b "malnutrition" at Dorland's Medical Dictionary
- ^ a b Papadia C, Di Sabatino A, Corazza GR, Forbes A (2014). "Diagnosing small bowel malabsorption: a review". Intern Emerg Med (Review). 9 (1): 3–8. doi:10.1007/s11739-012-0877-7. PMID 23179329.
- ^ a b c d e "Maternal, newborn, child and adolescent health". WHO. Retrieved July 4, 2014.
- ^ a b c d e f g h "An update of 'The Neglected Crisis of Undernutrition: Evidence for Action'" (PDF). www.gov.uk. Department for International Development. October 2012. Retrieved July 5, 2014.
- ^ a b Jonathan A. Foley; Navin Ramankutty; Kate A. Brauman; Emily S. Cassidy; James S. Gerber; Matt Johnston; Nathaniel D. Mueller; Christine O’Connell; Deepak K. Ray; Paul C. West; Christian Balzer; Elena M. Bennett; Stephen R. Carpenter; Jason Hill; Chad Monfreda; Stephen Polasky; Johan Rockström; John Sheehan; Stefan Siebert; David Tilman; David P. M. Zaks (October 2011). "Solutions for a cultivated planet". Nature. 478 (7369): 337–342. doi:10.1038/nature10452. PMID 21993620.
- ^ a b c d e f g h i Bhutta, ZA; Das, JK; Rizvi, A; Gaffey, MF; Walker, N; Horton, S; Webb, P; Lartey, A; Black, RE; Lancet Nutrition Interventions Review, Group; Maternal and Child Nutrition Study, Group (August 3, 2013). "Evidence-based interventions for improvement of maternal and child nutrition: what can be done and at what cost?". Lancet. 382 (9890): 452–77. doi:10.1016/s0140-6736(13)60996-4. PMID 23746776.
{{cite journal}}:|first10=has generic name (help) - ^ a b Kastin DA, Buchman AL (2002). "Malnutrition and gastrointestinal disease". Curr Opin Clin Nutr Metab Care (Review). 5 (6): 699–706. doi:10.1097/01.mco.0000038815.16540.bc. PMID 12394647.
- ^ a b c d e "The State of Food Insecurity in the World 2017". Food and Agricultural Organization of the United Nations. Retrieved June 19, 2018.
- ^ a b c GBD 2015 Mortality and Causes of Death, Collaborators. (October 8, 2016). "Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1459–1544. doi:10.1016/s0140-6736(16)31012-1. PMC 5388903. PMID 27733281.
{{cite journal}}:|first1=has generic name (help)CS1 maint: numeric names: authors list (link) - ^ a b c Essentials of International Health. Jones & Bartlett Publishers. 2011. p. 194. ISBN 9781449667719.
- ^ Arora, Mala; Konje, Justin C., eds. (2007). Recurrent pregnancy loss (2nd ed.). New Delhi: Jaypee Bros. Medical Publishers. ISBN 9788184480061.
- ^ "Progress For Children: A Report Card On Nutrition" (PDF). UNICEF.
- ^ Caballero, Benjamin; Allen, Lindsay; Prentice, eds. (2005). Encyclopedia of human nutrition (2nd ed.). Amsterdam: Elsevier/Academic Press. p. 68. ISBN 9780080454283.
- ^ Stoelting's anesthesia and co-existing disease (6th ed.). Philadelphia: Saunders/Elsevier. 2012. p. 324. ISBN 9781455738120.
- ^ "World Food Programme, Cash and Vouchers for Food" (PDF). WFP.org. April 2012. Retrieved July 5, 2014.
- ^ a b Ann Ashworth (2003). Guidelines for the inpatient treatment of severely malnourished children. Geneva: World Health Organization. ISBN 9241546093.
- ^ "Global hunger declining, but still unacceptably high International hunger targets difficult to reach" (PDF). Food and Agriculture Organization of the United Nations. September 2010. Retrieved July 1, 2014.
- ^ GBD 2013 Mortality and Causes of Death, Collaborators (December 17, 2014). "Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013". Lancet. 385 (9963): 117–71. doi:10.1016/S0140-6736(14)61682-2. PMC 4340604. PMID 25530442.
{{cite journal}}:|first1=has generic name (help)CS1 maint: numeric names: authors list (link) - ^ a b Murray, CJ (December 15, 2012). "Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010". Lancet. 380 (9859): 2197–223. doi:10.1016/S0140-6736(12)61689-4. PMID 23245608.
- ^ a b Lim SS, Vos T, Flaxman AD, et al. (December 2012). "A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010". Lancet. 380 (9859): 2224–60. doi:10.1016/S0140-6736(12)61766-8. PMC 4156511. PMID 23245609.
- ^ Liz Young (2002). World Hunger Routledge Introductions to Development. p. 20. ISBN 9781134774944.
- ^ editors, Ronnie A. Rosenthal, Michael E. Zenilman, Mark R. Katlic, (2011). Principles and practice of geriatric surgery (2nd ed.). Berlin: Springer. p. 78. ISBN 9781441969996.
{{cite book}}:|last1=has generic name (help)CS1 maint: extra punctuation (link) CS1 maint: multiple names: authors list (link) - ^ Sathish Subramanian; Sayeeda Huq; Tanya Yatsunenko; Rashidul Haque; Mustafa Mahfuz; Mohammed A. Alam (June 19, 2014). "Persistent gut microbiota immaturity in malnourished Bangladeshi children". Nature. 510. Nature Publishing Group.
- ^ a b c d e f g Nikolaos Katsilambros (2011). Clinical Nutrition in Practice. John Wiley & Sons. p. 37. ISBN 978-1-4443-4777-7.
- ^ "WHO, nutrition experts take action on malnutrition". World Health Organization. Retrieved February 10, 2012.
- ^ "Progress For Children: A Report Card On Nutrition" (PDF). UNICEF.
- ^ Nikolaos Katsilambros (2011). Clinical Nutrition in Practice. John Wiley & Sons. p. 39. ISBN 978-1-4443-4777-7.
- ^ "hypoalimentation" at Dorland's Medical Dictionary
- ^ a b c Duggan, Christopher; Watkins, John B.; Walker, W. Allan, eds. (2008). Nutrition in pediatrics: basic science, clinical application. Hamilton: BC Decker. pp. 127–141. ISBN 978-1-55009-361-2.
- ^ a b c Chowdhury, M. S. I.; Akhter, N.; Haque, M.; Aziz, R.; Nahar, N. (2009). "Serum Total Protein and Albumin Levels in Different Grades of Protein Energy Malnutrition". Journal of Bangladesh Society of Physiologist. 3. doi:10.3329/jbsp.v3i0.1799.
- ^ Stanton J (2001). "Listening to the Ga: Cicely Williams' Discovery of Kwashiorkor on the Gold Coast". Clio Medica: Studies in the History of Medicine and Health. 61: 149–171. PMID 11603151.
- ^ a b Black, R. E.; Allen, L. H.; Bhutta, Z. A.; Caulfield, L. E.; De Onis, M.; Ezzati, M.; Mathers, C.; Rivera, J.; Maternal Child Undernutrition Study Group (2008). "Maternal and child undernutrition: Global and regional exposures and health consequences". The Lancet. 371 (9608): 243–260. doi:10.1016/S0140-6736(07)61690-0. PMID 18207566.
- ^ a b Stevenson, R. D.; Conaway, M. R. (August 2011). "Weight and Mortality Rates: "Gomez Classification" for Children With Cerebral Palsy?". Pediatrics. 128 (2): e436–e437. doi:10.1542/peds.2011-1472. PMID 21768321.
- ^ a b c d e Grover, Zubin; Ee, Looi C. (2009). "Protein Energy Malnutrition". Pediatric Clinics of North America. 56 (5): 1055–1068. doi:10.1016/j.pcl.2009.07.001. PMID 19931063.
- ^ Gueri, M.; J. M. Gurney, P. Jutsum (1980). "The gomez classification. Time for a change?" (PDF). Bulletin of the World Health Organization. 58 (5): 773–777. PMC 2395976. PMID 6975186.
- ^ a b c J. C. Waterlow (1972). "Classification and Definition of Protein-Calorie Malnutrition". British Medical Journal. 3 (5826): 566–569. doi:10.1136/bmj.3.5826.566. PMC 1785878. PMID 4627051.
- ^ Watts, Geoff (December 2010). "John Conrad Waterlow". The Lancet. 376 (9757): 1982. doi:10.1016/S0140-6736(10)62252-0.
- ^ a b c Stillwaggon, Eileen (2008). "Race, Sex, and the Neglected Risks for Women and Girls in Sub-Saharan Africa". Feminist Economics. 14 (4): 67–86. doi:10.1080/13545700802262923.
- ^ Schaible, U. E.; Kaufmann, S. H. E. (2007). "Malnutrition and Infection: Complex Mechanisms and Global Impacts". PLoS Medicine. 4 (5): e115. doi:10.1371/journal.pmed.0040115. PMC 1858706. PMID 17472433.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ a b c d e f "8. Management of diarrhoea with severe malnutrition". The Treatment of diarrhoea : a manual for physicians and other senior health workers (PDF) (4 ed.). Geneva: World Health Organization. 2005. pp. 22–24. ISBN 924159318 0.
- ^ Laus, M. F.; Duarte Manhas Ferreira Vales, L.; Braga Costa, T. M.; Sousa Almeida, S. O. (2011). "Early Postnatal Protein-Calorie Malnutrition and Cognition: A Review of Human and Animal Studies". International Journal of Environmental Research and Public Health. 8 (2): 590–612. doi:10.3390/ijerph8020590. PMC 3084481. PMID 21556206.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Kenton R. Holden. "Chapter 2 Malnutrition and Brain Development: A Review. In Neurologic Consequences of Malnutrition, World Federation of Neurology Seminars in Clinical Neurology, 2008, World Federation of Neurology," (PDF). Demos Medical Publishing. Archived from the original (PDF) on May 10, 2013. Retrieved March 3, 2014.
{{cite journal}}: Cite journal requires|journal=(help); Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ a b McNeil Jr, Donald G. (December 16, 2006). "In raising the world's IQ the secret is in salt". New York Times.
- ^ Fotso, J. C.; Kuate-Defo, B. (2005). "Measuring socioeconomic status in health research in developing countries: Should we be focusing on households, communities or both?". Social Indicators Research. 72 (2): 189–237. doi:10.1007/s11205-004-5579-8.
- ^ Mandell, Gerald L.; Bennett, John Eugene; Dolin, Raphael; Douglas, Robert Gordon, eds. (2010). Mandell, Douglas, and Bennett's principles and practice of infectious diseases (7th ed.). Philadelphia, PA: Churchill Livingstone/Elsevier. pp. Chp 93. ISBN 0-443-06839-9.
- ^ Malnutrition at eMedicine
- ^ Baro, M.; Deubel, T. F. (2006). "Persistent Hunger: Perspectives on Vulnerability, Famine, and Food Security in Sub-Saharan Africa". Annual Review of Anthropology. 35: 521–538. doi:10.1146/annurev.anthro.35.081705.123224.
- ^ a b Musaiger, Abdulrahman O.; Hassan, Abdelmonem S.; Obeid, Omar (August 2011). "The Paradox of Nutrition-Related Diseases in the Arab Countries: The Need for Action". International Journal of Environmental Research and Public Health. 8 (9): 3637–3671. doi:10.3390/ijerph8093637. PMC 3194109. PMID 22016708.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ a b World Health Organization (2001). "Water-related diseases: Malnutrition".
- ^ Newnham ED (2017). "Coeliac disease in the 21st century: paradigm shifts in the modern age". J Gastroenterol Hepatol (Review). 32 Suppl 1: 82–85. doi:10.1111/jgh.13704. PMID 28244672.
The epidemiology of coeliac disease (CD) is changing. Presentation of CD with malabsorptive symptoms or malnutrition is now the exception rather than the rule

- ^ Brady JP (June 2012). "Marketing breast milk substitutes: problems and perils throughout the world". Arch Dis Child. 97 (6): 529–32. doi:10.1136/archdischild-2011-301299. PMC 3371222. PMID 22419779.
- ^ "Malnutrition Kills Over 3 Million Children Annually Worldwide". Medical News Today. Retrieved February 20, 2018.
- ^ Burchi F, Fanzo J, Frison E (February 2011). "The role of food and nutrition system approaches in tackling hidden hunger". Int J Environ Res Public Health. 8 (2): 358–73. doi:10.3390/ijerph8020358. PMC 3084466. PMID 21556191.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ a b UNICEF (2013). Improving Child Nutrition - The achievable imperative for global progress. UNICEF
- ^ a b c d e Gardner, Gary; Halweil, Brian (2000). "Escaping Hunger, Escaping Excess". World Watch. 13 (4): 24.
- ^ a b Gardner, Gary; Halweil, Brian (2000). "Escaping Hunger, Escaping Excess". World Watch. 13 (4): 5.
- ^ a b Khan, MM; Kraemer, A (August 2009). "Factors associated with being underweight, overweight and obese among ever-married non-pregnant urban women in Bangladesh". Singapore medical journal. 50 (8): 804–13. PMID 19710981.
- ^ a b Sen, Amartya Kumar (1981). Poverty and famines: An essay on entitlement and deprivation. Oxford University Press. ISBN 978-0-19-828463-5.
- ^ "The role of speculators in the global food crisis". Spiegel Online.
- ^ "Biofuel use increasing poverty". BBC News. June 25, 2008.
- ^ Ferrett, Grant (October 27, 2007). "Biofuels 'crime against humanity'". BBC News.
- ^ a b c d e f Dugger, Celia W. (December 2, 2007). "Ending Famine, Simply by Ignoring the Experts". New York Times.
- ^ Biles, Peter (February 6, 2006). "Zambia: fertile but hungry". BBC News.
- ^ "Forgotten benefactor of humanity". The Atlantic.
- ^ a b c "Climate Change 2007: Synthesis Report" (PDF). Intergovernmental Panel on Climate Change. November 12–17, 2007. Retrieved January 27, 2010.
- ^ Battisti, David S. "Climate Change in Developing Countries." University of Washington. Seattle. October 27, 2008.[verification needed]
- ^ Black, Richard (August 9, 2010). "Rice yields falling under global warming". BBC News; Science & Environment.
- ^ Honey Bee Die-Off Alarms Beekeepers, Crop growers and researchers
- ^ Wells, Matt (March 11, 2007). "Vanishing bees threaten US crops". BBC News.
- ^ McKie, Robin; Rice, Xan (April 22, 2007). "Millions face famine as crop disease rages". Guardian. London.
- ^ Kaplan, Karen (June 14, 2009). "A time bomb for world wheat crop". LA Times.
- ^ Dugger, Celia W. (October 10, 2007). "In Africa, prosperity from seeds falls short". New York Times.
- ^ Barclay, Eliza (June 18, 2008). "How a Kenyan village tripled its corn harvest". Christian Science Monitor.
- ^ John Ulimwengu; et al. (March 2013). "Need in a land of planty". dandc.eu.
- ^ Baker, Peter; Dugger, Celia W. (July 9, 2009). "Obama enlists major powers to aid poor farmers with $15 billion". The New York Times.
- ^ Chinedu, Obasi (October 12, 2018). "Severe Malnutrition, A Disturbance in Nigerian Health Sector". Public Health Nigeria.
- ^ Li, Jiming, Yeyun Xin and Longping Yuan. (2010). Pushing the Yield Frontier: Hybrid rice in China. In MillionsFed: Proved Success in Agriculture Development. Washington, DC: International Policy Research Institute
- ^ a b c d "UN aid debate: give cash not food?". Christian Science Monitor. June 4, 2008.
- ^ "Cash roll-out to help hunger hot spots". World Food Programme. December 8, 2008. Archived from the original on February 12, 2009.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Andrew S. Natsios (Administrator U.S. Agency for International Development)
- ^ a b "Let them eat micronutrients". Newsweek.
- ^ Memorandum to former Representative Steve Solarz (United States, Democratic Party, New York), July 1994
- ^ "A model of African food aid is now in trouble". Christian Science Monitor. May 6, 2008.
- ^ Malthus, Thomas Robert; Appleman, Philip (1976). An essay on the principle of population: text, sources and background, criticism. Norton. ISBN 978-0-393-09202-8.
- ^ Chapman, R. (1999). "No room at the inn, or why population problems are not all economic". Population and Environment. 21: 81–97. doi:10.1007/BF02436122.
- ^ "Environment - United Nations Population Division | Department of Economic and Social Affairs". www.un.org. Retrieved September 21, 2018.
- ^ "Family planning/Contraception". World Health Organization. Retrieved September 21, 2018.
- ^ Ohlin, G. (1967). Population control and economic development. Paris: Dev Centers, OECD.
- ^ Nielson, K. (1992). Global Justice, Capitalism and the Third World. (R. A. Wilkons, Ed.)
- ^ Waters, H. R.; Penny, M. E.; Creed-Kanashiro, H. M.; Robert, R. C.; Narro, R.; Willis, J.; Caulfield, L. E.; Black, R. E. (2006). "The cost-effectiveness of a child nutrition education programme in Peru". Health Policy and Planning. 21 (4): 257–264. doi:10.1093/heapol/czl010. PMID 16672293.
- ^ Nyonator, Frank, J Koku Awooner-Williams, James Phillips, Tanya Jones, Robert Miller. (2003). The Ghana Community-based Health Planning and Services Initiative: Fostering Evidence-based Organizational Change and Development in a Resource-constrained Setting. In Policy Research Division Working Papers 180. New York: Population Council. "Archived copy" (PDF). Archived from the original (PDF) on March 11, 2012. Retrieved March 15, 2012.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help)CS1 maint: archived copy as title (link) - ^ Victora, CG; Bahl, R; Barros, AJ; França, GV; Horton, S; Krasevec, J; Murch, S; Sankar, MJ; Walker, N; Rollins, NC; Lancet Breastfeeding Series, Group (January 30, 2016). "Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect". Lancet. 387 (10017): 475–90. doi:10.1016/S0140-6736(15)01024-7. PMID 26869575.
{{cite journal}}:|first11=has generic name (help) - ^ a b Lessen, Rachelle; Kavanagh, Katherine (March 1, 2015). "Position of the Academy of Nutrition and Dietetics: Promoting and Supporting Breastfeeding". Journal of the Academy of Nutrition and Dietetics. 115 (3): 444–449. doi:10.1016/j.jand.2014.12.014. ISSN 2212-2672.
- ^ a b c d e Balogun, Olukunmi Omobolanle; Dagvadorj, Amarjagal; Anigo, Kola Mathew; Ota, Erika; Sasaki, Satoshi (October 1, 2015). "Factors influencing breastfeeding exclusivity during the first 6 months of life in developing countries: a quantitative and qualitative systematic review". Maternal & Child Nutrition. 11 (4): 433–451. doi:10.1111/mcn.12180. ISSN 1740-8709.
- ^ a b c Pugh, Linda C.; Milligan, Renee A.; Frick, Kevin D.; Spatz, Diane; Bronner, Yvonne (June 1, 2002). "Breastfeeding Duration, Costs, and Benefits of a Support Program for Low-Income Breastfeeding Women". Birth. 29 (2): 95–100. doi:10.1046/j.1523-536X.2002.00169.x. ISSN 1523-536X.
- ^ a b c d e Cai, Xiaodong; Wardlaw, Tessa; Brown, David W. (September 28, 2012). "Global trends in exclusive breastfeeding". International Breastfeeding Journal. 7: 12. doi:10.1186/1746-4358-7-12. ISSN 1746-4358.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ "Universal Declaration of Human Rights". www.un.org. Retrieved February 24, 2018.
- ^ "What is the Right to Food? | Right to food". www.righttofood.org. Retrieved February 24, 2018.
- ^ "Universal Declaration on the Eradication of Hunger and Malnutrition". Retrieved February 24, 2018.
- ^ "American Convention on Human Rights". www.hrcr.org. Retrieved March 17, 2018.
- ^ "Rome Declaration and Plan of Action". www.fao.org. Retrieved March 17, 2018.
- ^ Description and targets for Goal 2 of the Sustainable Development Goals
- ^ Compact2025: Ending hunger and undernutrition. 2015. Project Paper. IFPRI: Washington, DC.
- ^ Leadership Council members from the website of the Compact 2025 partnership
- ^ Outcome of the 2012 Copenhagen Consensus
- ^ Scaling Up Nutrition Website, About page
- ^ a b c d e f g h National Guidelines for the Management of Severely Malnourished Children in Bangladesh, Institute of Public Health Nutrition, Directorate General of Health Services, Ministry of Health and Family Welfare, Government of the People’s Republic of Bangladesh, May 2008, page 18 (19 in PDF) and following pages.
- ^ Bally, MR; Blaser Yildirim, PZ; Bounoure, L; Gloy, VL; Mueller, B; Briel, M; Schuetz, P (January 1, 2016). "Nutritional Support and Outcomes in Malnourished Medical Inpatients: A Systematic Review and Meta-analysis". JAMA Internal Medicine. 176 (1): 43–53. doi:10.1001/jamainternmed.2015.6587. PMID 26720894.
- ^ Sguassero, Y; de Onis, M; Bonotti, AM; Carroli, G (June 13, 2012). "Community-based supplementary feeding for promoting the growth of children under five years of age in low and middle income countries". The Cochrane Database of Systematic Reviews. 6: CD005039. doi:10.1002/14651858.CD005039.pub3. PMID 22696347.
- ^ Lazzerini, M; Rubert, L; Pani, P (June 21, 2013). "Specially formulated foods for treating children with moderate acute malnutrition in low- and middle-income countries". The Cochrane Database of Systematic Reviews. 6: CD009584. doi:10.1002/14651858.CD009584.pub2. PMID 23794237.
- ^ Schoonees, A; Lombard, M; Musekiwa, A; Nel, E; Volmink, J (June 6, 2013). "Ready-to-use therapeutic food for home-based treatment of severe acute malnutrition in children from six months to five years of age". The Cochrane Database of Systematic Reviews. 6: CD009000. doi:10.1002/14651858.CD009000.pub2. PMID 23744450.
- ^ a b Anderson, Tatum (June 24, 2009). "Firms target nutrition for the poor". BBC News.
- ^ a b Viana Lde, A; Burgos, MG; Silva Rde, A (January–March 2012). "Refeeding syndrome: clinical and nutritional relevance". Arquivos brasileiros de cirurgia digestiva : ABCD = Brazilian archives of digestive surgery. 25 (1): 56–9. PMID 22569981.
- ^ Boateng, AA; Sriram, K; Meguid, MM; Crook, M (February 2010). "Refeeding syndrome: treatment considerations based on collective analysis of literature case reports". Nutrition (Burbank, Los Angeles County, Calif.). 26 (2): 156–67. doi:10.1016/j.nut.2009.11.017. PMID 20122539.
- ^ Kristof, Nicholas D. (December 4, 2008). "Raising the world's IQ". The New York Times.
- ^ a b c d e f g The Treatment of Diarrhoea: A manual for physicians and other senior health workers, World Health Organization, 2005. See especially Ch. 4 "Management of Acute Diarrhoea (Without Blood)" and Ch. 8 "Management of Diarrhoea With Severe Malnutrition."
- ^ Victora, Cesar; Bryce, Jennifer (January 2000). "Reducing deaths from diarrhoea through oral rehydration therapy". Bulletin of the World Health Organization (10).
- ^ a b "4. Management of acute diarrhoea without blood". The Treatment of diarrhoea : a manual for physicians and other senior health workers (PDF) (4 ed.). Geneva: World Health Organization. 2005. pp. 8–16. ISBN 924159318 0.
- ^ WHO Drug Information Vol. 16, No. 2, 2002.
- ^ Low-osmolarity oral rehydration solution (ORS), Rehydrate Project, updated: April 23, 2014.
- ^ The Treatment of Diarrhoea: A manual for physicians and other senior health workers, WHO, 2005. Specifically, 45 milliliters of potassium chloride solution from a stock solution containing 100g KCl per liter, along with one packet of ORS, two liters of water, and 50 grams of sucrose. And please remember, sucrose has approximately twice the molecular weight of glucose, with one mole of glucose weighing 180 g and one mole of sucrose weighing 342 g.
- ^ "Guidelines for the control of shigellosis, including epidemics due to Shigella dysenteriae type 1". World Health Organization, 2005, Annex 12 - Preparation of Home Made Oral Rehydration Solution, page 51 (57 in PDF): "Ingredients: Half a teaspoon of salt (2.5 grams), six level teaspoons of sugar (30 grams) and one litre of safe drinking water".
- ^ "Dehydration, treatments and drugs." Mayo Clinic January 7, 2011. "In an emergency situation where a pre-formulated solution is unavailable, you can make your own oral rehydration solution by mixing half teaspoon salt, six level teaspoons of sugar and one litre (about 1 quart) of safe drinking water."
- ^ Family Practice Notebook, Oral Rehydration Solution, Scott Moses, MD, February 1, 2014.
- ^ National Guidelines for the Management of Severely Malnourished Children in Bangladesh recommends, for initial hypoglycemia, a 50 milliliter bolus of 10% glucose or sucrose. This can also be achieved by added 1 rounded teaspoon of sugar to 10.5 teaspoons of water (which is 3.5 tablespoons of water).
- ^ "Mortality and Burden of Disease Estimates for WHO Member States in 2002" (xls). World Health Organization. 2002.
- ^ Jean Ziegler. "Promotion And Protection Of All Human Rights, Civil, Political, Economic, Social And Cultural Rights, Including The Right To Development: Report of the Special Rapporteur on the right to food, Jean Ziegler". Human Rights Council of the United Nations, January 10, 2008."According to the Food and Agriculture Organization of the United Nations (FAO), the world already produces enough food to feed every child, woman and man and could feed 12 billion people, or double the current world population."
- ^ a b "The State of Food Insecurity in the World 2015". Food and Agricultural Organization of the United Nations. Retrieved December 27, 2015.
- ^ Food and Agriculture Organization Economic and Social Development Department. "The State of Food Insecurity in the World, 2008 : High food prices and food security — threats and opportunities". Food and Agriculture Organization of the United Nations, 2008, p. 48.
- ^ Food and Agriculture Organization Agricultural and Development Economics Division. "The State of Food Insecurity in the World, 2006 : Eradicating world hunger – taking stock ten years after the World Food Summit". Food and Agriculture Organization of the United Nations, 2006, p. 8. "Because of population growth, the very small decrease in the number of hungry people has nevertheless resulted in a reduction in the proportion of undernourished people in the developing countries by 3 percentage points – from 20 percent in 1990–92 to 17 percent in 2001–03. (...) the prevalence of undernourishment declined by 9 percent (from 37 percent to 28 percent) between 1969–71 and 1979–81 and by a further 8 percentage points (to 20 percent) between 1979–81 and 1990–92.".
- ^ Food and Agriculture Organization Economic and Social Development Department. "The State of Food Insecurity in the World, 2008 : High food prices and food security — threats and opportunities". Food and Agriculture Organization of the United Nations, 2008, p. 6. "Good progress in reducing the share of hungry people in the developing world had been achieved – down from almost 20 percent in 1990–92 to less than 18 percent in 1995–97 and just above 16 percent in 2003–05. The estimates show that rising food prices have thrown that progress into reverse, with the proportion of undernourished people worldwide moving back towards 17 percent.".
- ^ http://www.savethechildren.org/atf/cf/%7B9def2ebe-10ae-432c-9bd0-df91d2eba74a%7D/STATE-OF-THE-WORLDS-MOTHERS-REPORT-2012-FINAL.PDF Archived May 23, 2012, at the Wayback Machine
- ^ Ziegler, Jean (2007). L'Empire de la honte. Fayard. p. 130. ISBN 978-2-253-12115-2.
- ^ a b Lozano R, Naghavi M, Foreman K, et al. (December 2012). "Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010". Lancet. 380 (9859): 2095–128. doi:10.1016/S0140-6736(12)61728-0. hdl:10536/DRO/DU:30050819. PMID 23245604.
- ^ a b c d "Malnutrition The Starvelings". The Economist. January 24, 2008.
- ^ "U.N. chief: Hunger kills 17,000 kids daily". CNN. November 17, 2009.
- ^ Alina Paul Bossuet, Nourishing Communities Through Holistic Farming "Archived copy". Archived from the original on April 2, 2015. Retrieved January 26, 2014.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help)CS1 maint: archived copy as title (link). ICRISAT. Downloaded January 26, 2014. - ^ Jere R. Behrman (February 1996). "The Impact of Health and Nutrition on Education". The World Bank Research Observer. 11 (1): 23–37. doi:10.1093/wbro/11.1.23. JSTOR 3986477.
- ^ Manary, Mark J.; Indi Trehan; Hayley S. Goldbach; Lacey N. LaGrone; Guthrie J. Meuli; Richard J. Wang; Kenneth M. Maleta (January 31, 2013). "Antibiotics as Part of the Management of Severe Acute Malnutrition". The New England Journal of Medicine. 368 (5): 425–435. doi:10.1056/NEJMoa1202851. PMC 3654668. PMID 23363496. Retrieved January 31, 2013.
The addition of antibiotics to therapeutic regimens for uncomplicated severe acute malnutrition was associated with a significant improvement in recovery and mortality rates.
- ^ a b c Prüss-Üstün, A., Bos, R., Gore, F., Bartram, J. (2008). Safer water, better health - Costs, benefits and sustainability of interventions to protect and promote health. World Health Organization (WHO), Geneva, Switzerland
- ^ a b c d e f g Nubé, M.; Van Den Boom, G. J. M. (2003). "Gender and adult undernutrition in developing countries". Annals of Human Biology. 30 (5): 520–537. doi:10.1080/0301446031000119601. PMID 12959894.
- ^ a b c Dewan, Manju (2008). "Malnutrition in Women" (PDF). Stud. Home Comm. Sci. 2 (1): 7–10. Retrieved March 3, 2014.
- ^ Najma Rizvi (March 2013). "Enduring misery". dandc.eu.
- ^ Carter, Rachel Bonham. "Survey Reveals High Malnutrition Rates Among Pregnant Women in Kenya". UNICEF. Retrieved March 3, 2014.
- ^ a b c d e "Gender and Nutrition 2001". Food and Agriculture of the United Nations. Retrieved August 22, 2016.
- ^ Bhutta, Z. A.; Ahmed, T.; Black, R. E.; Cousens, S.; Dewey, K.; Giugliani, E.; Haider, B. A.; Kirkwood, B.; Morris, S. S.; Sachdev, H. P. S.; Shekar, M.; Maternal Child Undernutrition Study Group (2008). "What works? Interventions for maternal and child undernutrition and survival". The Lancet. 371 (9610): 417–440. doi:10.1016/S0140-6736(07)61693-6. PMID 18206226.
- ^ Denis Campbell (October 14, 2014). "Folic acid to be added to UK flour in effort to reduce birth defects". The Guardian. Retrieved October 15, 2018.
- ^ a b Kvamme, Jan–Magnus; Olsen, Jan Abel; Florholmen, Jon; Jacobsen, Bjarne K. (2011). "Risk of malnutrition and health-related quality of life in community-living elderly men and women: The Tromsø study". Quality of Life Research. 20 (4): 575–582. doi:10.1007/s11136-010-9788-0. PMC 3075394. PMID 21076942.
- ^ a b c d Wellman, N.S; Weddle, D.O; Kranz, S; Brain, C.T (October 1997). "Elder Insecurities: Poverty, Hunger, and Malnutrition". Journal of the American Dietetic Association. 97 (10): S120–S122. doi:10.1016/S0002-8223(97)00744-X. PMID 9336570.
- ^ a b c Bulent Saka; Omer Kaya; Gulistan Bahat Ozturk; Nilgun Erten; M. Akif Karan (2010). "Malnutrition in the elderly and its relationship with other geriatric syndromes". Clinical Nutrition. 29 (6): 745–748. doi:10.1016/j.clnu.2010.04.006. PMID 20627486.
- ^ a b Volkert, Dorothee (2002). "Malnutrition in the elderly — prevalence, causes and corrective strategies". Clinical Nutrition. 21: 110–112. doi:10.1016/S0261-5614(02)80014-0.
- ^ Volkert, D. (2002). "Malnutrition in the elderly — prevalence, causes and corrective strategies". Clinical Nutrition. 21: 110–112. doi:10.1016/S0261-5614(02)80014-0.
- ^ a b Milne, AC; Potter, J; Vivanti, A; Avenell, A (April 15, 2009). "Protein and energy supplementation in elderly people at risk from malnutrition". The Cochrane Database of Systematic Reviews (2): CD003288. doi:10.1002/14651858.CD003288.pub3. PMID 19370584.
- ^ Mamhidir, Anna-Greta; Kihlgren, Mona; Soerlie, Venke (2010). "Malnutrition in elder care: qualitative analysis of ethical perceptions of politicians and civil servants". BMC Medical Ethics. 11: 11. doi:10.1186/1472-6939-11-11. PMC 2927875. PMID 20553607.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Bolin, T.; Bare, M.; Caplan, G.; Daniells, S.; Holyday, M. (2010). "Malabsorption may contribute to malnutrition in the elderly". Nutrition. 26 (7–8): 852–853. doi:10.1016/j.nut.2009.11.016. PMID 20097534.
