Schizophrenia: Difference between revisions
→Neural: changing section name to appropriate title |
→Neurological Pathology: change to brain chemistry, not just Dopamine |
||
| Line 81: | Line 81: | ||
===Neurological Pathology=== |
===Neurological Pathology=== |
||
[[File:Schizophrenia PET scan.jpg|thumb|Data from a [[Positron emission tomography|PET]] study<ref name="fn_25">{{vcite journal |author=Meyer-Lindenberg A |coauthors=Miletich RS, Kohn PD, Esposito G, Carson RE, Quarantelli M, Weinberger DR, Berman KF |year=2002 |title=Reduced prefrontal activity predicts exaggerated striatal dopaminergic function in schizophrenia |journal=[[Nature Neuroscience]] |volume=5 |pages=267–71 |pmid=11865311 |doi=10.1038/nn804 |issue=3}}</ref> suggests that the less the [[frontal lobe]]s are activated (<span style="color:red;">red</span>) during a [[working memory]] task, the greater the increase in abnormal [[dopamine]] activity in the [[striatum]] (<span style="color:green;">green</span>), thought to be related to the [[neurocognitive deficit]]s in schizophrenia.]] |
[[File:Schizophrenia PET scan.jpg|thumb|Data from a [[Positron emission tomography|PET]] study<ref name="fn_25">{{vcite journal |author=Meyer-Lindenberg A |coauthors=Miletich RS, Kohn PD, Esposito G, Carson RE, Quarantelli M, Weinberger DR, Berman KF |year=2002 |title=Reduced prefrontal activity predicts exaggerated striatal dopaminergic function in schizophrenia |journal=[[Nature Neuroscience]] |volume=5 |pages=267–71 |pmid=11865311 |doi=10.1038/nn804 |issue=3}}</ref> suggests that the less the [[frontal lobe]]s are activated (<span style="color:red;">red</span>) during a [[working memory]] task, the greater the increase in abnormal [[dopamine]] activity in the [[striatum]] (<span style="color:green;">green</span>), thought to be related to the [[neurocognitive deficit]]s in schizophrenia.]] |
||
Those with a diagnosis of schizophrenia have both changes in brain structure and |
Those with a diagnosis of schizophrenia have both changes in brain structure and brain chemistry.<ref name=Lancet09/> Studies using [[neuropsychological test]]s and [[brain imaging]] technologies such as [[Functional magnetic resonance imaging|fMRI]] and [[Positron emission tomography|PET]] to examine functional differences in brain activity have shown that differences seem to most commonly occur in the [[frontal lobe]]s, [[hippocampus]] and [[temporal lobe]]s.<ref>{{vcite book|year=2006|last=Kircher|first=Tilo|coauthors=Renate Thienel|title=The Boundaries of Consciousness|isbn=0444528768|page=302|url=http://books.google.com/?id=YHGacGKyVbYC&pg=PA302|chapter=Functional brain imaging of symptoms and cognition in schizophrenia|publisher=Elsevier|location=Amsterdam}}</ref> Due to the alteration in neural circuits some feel schizophrenia should be viewed as a collection of neurodevelopmental disorders.<ref name=Insel_2010>{{cite journal | last1 = Insel | first1 = TR | author-separator =, | author-name-separator= | year = 2010 | title = Rethinking Schizophrenia | url = | journal = Nature | volume = 468 | issue = | pages = 188–93 }}</ref>These differences have been linked to the [[neurocognitive deficit]]s often associated with schizophrenia.<ref name="Green2006">{{vcite journal |author=Green MF|year=2006|title=Cognitive impairment and functional outcome in schizophrenia and bipolar disorder|journal=Journal of Clinical Psychiatry |volume=67 | issue=Suppl 9 |pages=3–8|pmid=16965182}}</ref> |
||
[[File:FMRI.jpg|thumb|left|[[Functional magnetic resonance imaging]] and other [[brain imaging]] technologies allow for the study of differences in brain activity among people diagnosed with schizophrenia]] |
[[File:FMRI.jpg|thumb|left|[[Functional magnetic resonance imaging]] and other [[brain imaging]] technologies allow for the study of differences in brain activity among people diagnosed with schizophrenia]] |
||
Revision as of 02:50, 27 December 2010
| Schizophrenia | |
|---|---|
| Specialty | Psychiatry, clinical psychology |
Schizophrenia (Template:Pron-en or /ˌskɪtsɵˈfriːniə/) is a mental disorder characterized by a disintegration of the process of thinking and of emotional responsiveness.[1] It most commonly manifests as auditory hallucinations, paranoid or bizarre delusions, or disorganized speech and thinking, and it is accompanied by significant social or occupational dysfunction. The onset of symptoms typically occurs in young adulthood,[2] with a global lifetime prevalence of around 0.3–0.7%.[3] Diagnosis is based on the patient's self-reported experiences and observed behavior.
Genetics, early environment, neurobiology, psychological and social processes appear to be important contributory factors; some recreational and prescription drugs appear to cause or worsen symptoms. Current research is focused on the role of neurobiology, but this inquiry has not isolated a single organic cause. As a result of the many possible combinations of symptoms, there is debate about whether the diagnosis represents a single disorder or a number of discrete syndromes. Despite the etymology of the term from the Greek roots skhizein (σχίζειν, "to split") and phrēn, phren- (φρήν, φρεν-; "mind"), schizophrenia does not imply a "split mind" and it is not the same as dissociative identity disorder—also known as "multiple personality disorder" or "split personality"—a condition with which it is often confused in public perception.[4]
The mainstay of treatment is antipsychotic medication; which primarily works by suppressing dopamine activity. Dosages of antipsychotics are generally lower than in the early decades of their use. Psychotherapy, and vocational and social rehabilitation, are also important. In more serious cases—where there is risk to self and others—involuntary hospitalization may be necessary, although hospital stays are shorter and less frequent than they were in previous times.[5]
The disorder is thought mainly to affect cognition, but it also usually contributes to chronic problems with behavior and emotion. People with schizophrenia are likely to have additional (comorbid) conditions, including major depression and anxiety disorders;[6] the lifetime occurrence of substance abuse is around 40%. Social problems, such as long-term unemployment, poverty and homelessness, are common. Furthermore, the average life expectancy of people with the disorder is 12 to 15 years less than those without, due to increased physical health problems and a higher suicide rate (about 5%).[3]
Signs and symptoms
A person diagnosed with schizophrenia may experience hallucinations (most commonly hearing voices), delusions (often bizarre or persecutory in nature), and disorganized thinking and speech. The latter may range from loss of train of thought, to sentences only loosely connected in meaning, to incoherence known as word salad in severe cases. Social withdrawal, sloppiness about dress and hygiene, and loss of motivation and judgement are all common in schizophrenia.[7] There is often an observable pattern of emotional difficulty, for example lack of responsiveness or motivation.[8] Impairment in social cognition is associated with schizophrenia,[9] as are symptoms of paranoia; and social isolation commonly occurs.[10] In one uncommon subtype, the person may be largely mute, remain motionless in bizarre postures, or exhibit purposeless agitation; these are signs of catatonia.[11]
Late adolescence and early adulthood are peak years for the onset of schizophrenia.[3] In 40% of men and 23% of women diagnosed with schizophrenia, the condition arose before the age of 19.[12] These are critical periods in a young adult's social and vocational development. To minimize the developmental disruption associated with schizophrenia, much work has recently been done to identify and treat the prodromal (pre-onset) phase of the illness, which has been detected up to 30 months before the onset of symptoms, but may be present longer.[13] Those who go on to develop schizophrenia may experience the non-specific symptoms of social withdrawal, irritability and dysphoria in the prodromal period,[14] and transient or self-limiting psychotic symptoms in the prodromal phase before psychosis becomes apparent.[15]
Schneiderian classification

The psychiatrist Kurt Schneider (1887–1967) listed the forms of psychotic symptoms that he thought distinguished schizophrenia from other psychotic disorders. These are called first-rank symptoms or Schneider's first-rank symptoms, and they include delusions of being controlled by an external force; the belief that thoughts are being inserted into or withdrawn from one's conscious mind; the belief that one's thoughts are being broadcast to other people; and hearing hallucinatory voices that comment on one's thoughts or actions or that have a conversation with other hallucinated voices.[16] Although they have significantly contributed to the current diagnostic criteria, the specificity of first-rank symptoms has been questioned. A review of the diagnostic studies conducted between 1970 and 2005 found that these studies allow neither a reconfirmation nor a rejection of Schneider's claims, and suggested that first-rank symptoms be de-emphasized in future revisions of diagnostic systems.[17]
Positive and negative symptoms
Schizophrenia is often described in terms of positive and negative (or deficit) symptoms.[18] The term positive symptoms refers to symptoms that most individuals do not normally experience but are present in people with schizophrenia. These symptoms gererally respond well to medication.[19] They can include delusions, disordered thoughts and speech, and hallucinations such as tactile, auditory, visual, olfactory and gustatory and are typically regarded as manifestations of psychosis.[20] Hallucinations are also typically related to the content of the delusional theme.[21] Negative symptoms are symptoms that are altered or defect emotional responses that respond less successfully to medication.[7] Common negative symptoms include flat or blunted affect and emotion, poverty of speech (alogia), inability to experience pleasure (anhedonia), lack of desire to form relationships (asociality), and lack of motivation (avolition). Research suggests that negative symptoms contribute more to poor quality of life, functional disability, and the burden on others than do positive symptoms.[22] People with negative symptoms tend to respond less well to medication and can often have a history of poor adjustment before the onset of illness.[23]
Causes
A combination of genetic and environmental factors play a role in the development of schizophrenia.[3][4]
Genetic
Estimates of heritability vary owing to the difficulty of separating the effects of genetics and the environment.[24] The greatest risk for developing schizophrenia is having a first degree relative with the disease (risk is 6.5%) while more than 40% of monozygotic twins of those with schizophrenia are affected.[4]
It is likely that many genes are involved each of small effect.[4] Some have suggested that several genetic and other risk factors need to be present before a person becomes affected but this is still uncertain.[25] Candidate genes linked to an increased risk of schizophrenia and bipolar disorder as found in recent genome wide association studies appear to be partly separate and partly overlapping between the two disorders[26] Genetic linkage studies have produced evidence of chromosomal regions increasing susceptibility,[27] which interacts directly with the Disrupted in Schizophrenia 1 (DISC1) gene protein[28] more recently the zinc finger protein 804A.[29] has been implicated as well as the chromosome 6 HLA region.[30] However, a large and comprehensive genetic study found no evidence of any significant association with any of 14 previously identified candidate genes.[31] Schizophrenia, in a small minority of cases, has been associated with rare deletions or duplications of tiny DNA sequences (known as copy number variants) disproportionately occurring within genes involved in neuronal signaling and brain development/human cognitive, behavioral, and psychological variation.[32][33][34] Relations have been found between autism spectrum disorders and schizophrenia based on duplications and deletions of chromosomes; research showed that schizophrenia and autism are significantly more common in combination with 1q21.1 deletion syndrome, velo-cardio-facial syndrome and Phelan-McDermid syndrome. Duplications of parts of the chromosomes which are opposites of these syndromes show more autism-results. Research on autism/schizophrenia relations for chromosome 15 (15q13.3), chromosome 16 (16p13.1) and chromosome 17 (17p12) are inconclusive.[35]
Assuming a hereditary genetic basis, one question for evolutionary psychology is why genes that increase the likelihood of the condition evolved, assuming the condition would have been maladaptive from an evolutionary/reproductive point of view. One theory implicates genes involved in the evolution of language and human nature, but so far all theories have been disproved or remain unsubstantiated.[36][37]
Environment
A number of environmental factors are associated with the development of schizophrenia including prenatal stressors, the living environment, and drug use.[3] Parenting style on the other hand has no effect on the risk.[4] Living in an urban environment either during childhood or as an adult has been consistently found to increase the risk of schizophrenia by a factor of two.[3][4] This is even after taking into account drug use, ethnic group and size of a persons social group.[38] Other factors that play an important role include: social isolation and immigration related to social adversity, racial discrimination, family dysfunction, unemployment or poor housing conditions.[39][4]
Substance abuse
A number of drugs have been associated with the developement of schizophrenia including: cocaine, amphetamines, and cannabis.[4]
Cannabis use is statistically associated with a dose-dependent increase in risk of development of psychotic disorders, including schizophrenia.[40] For example, cannabis use has increased dramatically in several countries over the past few decades, though contrary to predictions the rates of psychosis and schizophrenia have generally not increased.[41][42][43]
Psychotic individuals may also use drugs to cope with unpleasant states such as depression, anxiety, boredom and loneliness, because drugs increase "feel-good" neurotransmitters level.[44] Various studies have shown that amphetamines increases the concentrations of dopamine in the synaptic cleft, thereby heightening the response of the post-synaptic neuron.[45] However, regarding psychosis itself, it is well understood that methamphetamine and cocaine use can result in methamphetamine- or cocaine-induced psychosis that present very similar symptomatology (sometimes even misdiagnosed as schizophrenia) and may persist even when users remain abstinent.[46] The same can also be said for alcohol-induced psychosis, though to a somewhat lesser extent.[47][48][49]
Prenatal
A number of factors during fetal development may result in a small increase in the risk of schizophrenia later in life including: hypoxia and infection, stress or malnutrition in the mother.[3] People diagnosed with schizophrenia are more likely to have been born in winter or spring, (at least in the northern hemisphere).[4] This may be due to the increased rates of viral exposures in utero.[4]
Mechanisms
Psychological
A number of psychological mechanisms have been implicated in the development and maintenance of schizophrenia. Cognitive biases that have been identified in those with a diagnosis or those at risk, especially when under stress or in confusing situations, include excessive attention to potential threats, jumping to conclusions, making external attributions, impaired reasoning about social situations and mental states, difficulty distinguishing inner speech from speech from an external source, and difficulties with early visual processing and maintaining concentration.[50][51][52][53] Some cognitive features may reflect global neurocognitive deficits in memory, attention, problem-solving, executive function or social cognition, while others may be related to particular issues and experiences.[54][55]
Despite a common appearance of "blunted affect", recent findings indicate that many individuals diagnosed with schizophrenia are emotionally responsive, particularly to stressful or negative stimuli, and that such sensitivity may cause vulnerability to symptoms or to the disorder.[56][57][58] Some evidence suggests that the content of delusional beliefs and psychotic experiences can reflect emotional causes of the disorder, and that how a person interprets such experiences can influence symptomatology.[59][60][61][62] The use of "safety behaviors" to avoid imagined threats may contribute to the chronicity of delusions.[63] Further evidence for the role of psychological mechanisms comes from the effects of psychotherapies on symptoms of schizophrenia.[64]
Neurological Pathology

Those with a diagnosis of schizophrenia have both changes in brain structure and brain chemistry.[3] Studies using neuropsychological tests and brain imaging technologies such as fMRI and PET to examine functional differences in brain activity have shown that differences seem to most commonly occur in the frontal lobes, hippocampus and temporal lobes.[66] Due to the alteration in neural circuits some feel schizophrenia should be viewed as a collection of neurodevelopmental disorders.[67]These differences have been linked to the neurocognitive deficits often associated with schizophrenia.[68]
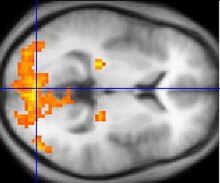
Particular focus has been placed upon the function of dopamine in the mesolimbic pathway of the brain. This focus largely resulted from the accidental finding that a drug group which blocks dopamine function, known as the phenothiazines, could reduce psychotic symptoms. It is also supported by the fact that amphetamines, which trigger the release of dopamine, may exacerbate the psychotic symptoms in schizophrenia.[69] An influential theory, known as the Dopamine hypothesis of schizophrenia, proposed that excess activation of D2 receptors was the cause of (the positive symptoms of) schizophrenia. Although postulated for about 20 years based on the D2 blockade effect common to all antipsychotics, it was not until the mid-1990s that PET and SPET imaging studies provided supporting evidence. This explanation is now thought to be simplistic, partly because newer antipsychotic medication (called atypical antipsychotic medication) can be equally effective as older medication (called typical antipsychotic medication), but also affects serotonin function and may have slightly less of a dopamine blocking effect.[70]
Interest has also focused on the neurotransmitter glutamate and the reduced function of the NMDA glutamate receptor in schizophrenia. This has largely been suggested by abnormally low levels of glutamate receptors found in postmortem brains of people previously diagnosed with schizophrenia[71] and the discovery that the glutamate blocking drugs such as phencyclidine and ketamine can mimic the symptoms and cognitive problems associated with the condition.[72] The fact that reduced glutamate function is linked to poor performance on tests requiring frontal lobe and hippocampal function and that glutamate can affect dopamine function, all of which have been implicated in schizophrenia, have suggested an important mediating (and possibly causal) role of glutamate pathways in schizophrenia.[73] Positive symptoms fail however to respond to glutamatergic medication.[74]
A commonly known side effect associated with schizo-affective patients known as akathisia (mistaken for schizophrenic symptoms) was found to be associated with increased levels of norepinephrine.[75] Data supports the efficacy of novel antipsychotics which deal with agonism of the NDMA glutamate receptors,[76] associated with regulating uptake of norepinephrine,[77] which in turn affects the trafficking of glutamate.[78] This, as well as the data noting exacerbation of positive symptoms in users of norepinephrine-agonizing amphetamine, suggests that schizophrenia may in fact have a greater association with abnormal norepinephrine-reuptake kinetics and less with dopamine, which may in fact be responsible for a large part of the mechanism of glutamate release.[78] It would be greatly beneficial for further research to be done in this area, particularly in the metabolism of various essential amino acids and their pro- and inhibitory effects on neurotransmitter balance.
There have also been findings of differences in the size and structure of certain brain areas in schizophrenia. A 2006 metaanlaysis of MRI studies found that whole brain and hippocampal volume are reduced and that ventricular volume is increased in patients with a first psychotic episode relative to healthy controls. The average volumetric changes in these studies are however close to the limit of detection by MRI methods, so it remains to be determined whether schizophrenia is a neurodegenerative process that begins at about the time of symptom onset, or whether it is better characterised as a neurodevelopmental process that produces abnormal brain volumes at an early age.[79] In first episode psychosis typical antipsychotics like haloperidol were associated with significant reductions in gray matter volume, whereas atypical antipsychotics like olanzapine were not.[80] Studies in non-human primates found gray and white matter reductions for both typical and atypical antipsychotics.[81]
A 2009 meta-analysis of diffusion tensor imaging studies identified two consistent locations of reduced fractional anisotropy (roughly the level of organization of neural connections) in schizophrenia. The authors suggest that two networks of white matter tracts may be affected in schizophrenia, with the potential for "disconnection" of the gray matter regions which they link.[82] During fMRI studies, greater connectivity in the brain's default network and task-positive network has been observed in patients diagnosed with schizophrenia, and may reflect excessive attentional orientation toward introspection and toward extrospection, respectively. The greater anti-correlation between the two networks suggests excessive rivalry between the networks.[83]
Diagnosis
Schizophrenia is diagnosed based on criteria in either the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders, version DSM-IV-TR, or the World Health Organization's International Statistical Classification of Diseases and Related Health Problems, the ICD-10.[3] These criteria use the self-reported experiences of the person, and abnormalities in behavior reported by family members, friends or co-workers, followed by a clinical assessment by a mental health professional. As of 2009 there is no objective test.[3]
Criteria
The ICD 10 criteria are typically used in European countries, while the DSM criteria are used in the United States and the rest of the world, as well as prevailing in research studies. The ICD-10 criteria put more emphasis on Schneiderian first-rank symptoms, although, in practice, agreement between the two systems is high.[84]
According to the revised fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR), to be diagnosed with schizophrenia, three diagnostic criteria must be met:[85]
- Characteristic symptoms: Two or more of the following, each present for much of the time during a one-month period (or less, if symptoms remitted with treatment).
- Delusions
- Hallucinations
- Disorganized speech, which is a manifestation of formal thought disorder
- Grossly disorganized behavior (e.g. dressing inappropriately, crying frequently) or catatonic behavior
- Negative symptoms: Blunted affect (lack or decline in emotional response), alogia (lack or decline in speech), or avolition (lack or decline in motivation)
- If the delusions are judged to be bizarre, or hallucinations consist of hearing one voice participating in a running commentary of the patient's actions or of hearing two or more voices conversing with each other, only that symptom is required above. The speech disorganization criterion is only met if it is severe enough to substantially impair communication.
- Social/occupational dysfunction: For a significant portion of the time since the onset of the disturbance, one or more major areas of functioning such as work, interpersonal relations, or self-care, are markedly below the level achieved prior to the onset.
- Duration: Continuous signs of the disturbance persist for at least six months. This six-month period must include at least one month of symptoms (or less, if symptoms remitted with treatment).
If signs of disturbance are present for more than a month but less than six months, the diagnosis of schizophreniform disorder is applied.[85] Psychotic symptoms lasting less than a month may be diagnosed as brief psychotic disorder, and various conditions may be classed as psychotic disorder not otherwise specified. Schizophrenia cannot be diagnosed if symptoms of mood disorder are substantially present (although schizoaffective disorder could be diagnosed), or if symptoms of pervasive developmental disorder are present unless prominent delusions or hallucinations are also present, or if the symptoms are the direct physiological result of a general medical condition or a substance, such as abuse of a drug or medication.
Differential
Psychotic symptoms may be present in several other mental disorders, including bipolar disorder,[86] borderline personality disorder,[87] drug intoxication and drug-induced psychosis. Delusions ("non-bizarre") are also present in delusional disorder, and social withdrawal in social anxiety disorder, avoidant personality disorder and schizotypal personality disorder. Schizophrenia is complicated with obsessive-compulsive disorder (OCD) considerably more often than could be explained by pure chance, although it can be difficult to distinguish obsessions that occur in OCD from the delusions of schizophrenia.[88]
A more general medical and neurological examination may be needed to rule out medical illnesses which may rarely produce psychotic schizophrenia-like symptoms,[85] such as metabolic disturbance, systemic infection, syphilis, HIV infection, epilepsy, and brain lesions. It may be necessary to rule out a delirium, which can be distinguished by visual hallucinations, acute onset and fluctuating level of consciousness, and indicates an underlying medical illness. Investigations are not generally repeated for relapse unless there is a specific medical indication or possible adverse effects from antipsychotic medication.
"Schizophrenia" does not mean dissociative identity disorder—formerly and still widely known as "multiple personalities"—despite the etymology of the word (Greek σχίζω = "I split").[4]
Subtypes
The DSM-IV-TR contains five sub-classifications of schizophrenia, although the developers of DSM-5 are recommending they be dropped from the new classification:[89]
- Paranoid type: Where delusions and hallucinations are present but thought disorder, disorganized behavior, and affective flattening are absent. (DSM code 295.3/ICD code F20.0)
- Disorganized type: Named hebephrenic schizophrenia in the ICD. Where thought disorder and flat affect are present together. (DSM code 295.1/ICD code F20.1)
- Catatonic type: The subject may be almost immobile or exhibit agitated, purposeless movement. Symptoms can include catatonic stupor and waxy flexibility. (DSM code 295.2/ICD code F20.2)
- Undifferentiated type: Psychotic symptoms are present but the criteria for paranoid, disorganized, or catatonic types have not been met. (DSM code 295.9/ICD code F20.3)
- Residual type: Where positive symptoms are present at a low intensity only. (DSM code 295.6/ICD code F20.5)
The ICD-10 defines two additional subtypes.
- Post-schizophrenic depression: A depressive episode arising in the aftermath of a schizophrenic illness where some low-level schizophrenic symptoms may still be present. (ICD code F20.4)
- Simple schizophrenia: Insidious and progressive development of prominent negative symptoms with no history of psychotic episodes. (ICD code F20.6)
Management
The primary treatment of schizophrenia is antipsychotic medications often in combination with psychological and social supports.[3] Hospitalization may occur with severe episodes of schizophrenia. This can be voluntary or (if mental health legislation allows it) involuntary (called civil or involuntary commitment). Long-term inpatient stays are now less common due to deinstitutionalization, although can still occur.[5] Following (or in lieu of) a hospital admission, support services available can include drop-in centers, visits from members of a community mental health team or assertive community treatment team, supported employment[90] and patient-led support groups.
In many non-Western societies, schizophrenia may be treated with more informal, community-led methods only. Multiple international surveys by the World Health Organization over several decades have indicated that the outcome for people diagnosed with schizophrenia in non-Western countries is on average better there than for people in the West.[91]
Three small randomized controlled trials indicate that regular exercise has a positive effect on the physical and mental health of those with schizophrenia.[92]
Medication

The first line psychiatric treatment for schizophrenia is antipsychotic medication.[93] These can reduce the positive symptoms of psychosis. Most antipsychotics take around 7–14 days to have their main effect. Currently available antipsychotics fail, however, to significantly ameliorate the negative symptoms, and the improvements on cognition may be attributed to the practice effect.[94][95][96][97]
The choice of which antipsychotic to use is based on a number of factors including: benefits, risks, and costs.[3] It is debatable whether as a class typical or atypical antipsychotics are better.[98] Both have equal drop-out and symptom relapse rates when typicals are used at low to moderate dosages.[99] With respect to side effects typical antipsychotics are associated with extrapyramidal side effects while atypicals are associated with considerable weight gain, diabetes and risk of metabolic syndrome.[99] Clozapine is an effective treatment for the 20—30% of people who respond poorly to other drugs, but it has the potentially serious side effect of agranulocytosis in 1—4%.[3][100][4]
Research has questioned the claim that atypical antipsychotics have fewer extrapyramidal side effects than typical antipsychotics, especially when the latter are used in low doses or when low potency antipsychotics are chosen.[101] It remains unclear whether the newer antipsychotics reduce the chances of developing neuroleptic malignant syndrome, a rare but serious and potentially fatal neurological disorder most often caused by an adverse reaction.[102]
Response of symptoms to medication is variable: treatment-resistant schizophrenia is a term used for the failure of symptoms to respond satisfactorily to at least two different antipsychotics.[103] For other people who are unwilling or unable to take medication regularly, long-acting depot preparations of antipsychotics may be given every two weeks to achieve control.
Psycholosocial
Psychotherapy is also widely recommended and used in the treatment of schizophrenia, although services may often be confined to pharmacotherapy because of reimbursement problems or lack of training.[104]
Cognitive behavioral therapy (CBT) is used to target specific symptoms[105][106][107] and improve related issues such as self-esteem, social functioning, and insight. Although the results of early trials were inconclusive[108] as the therapy advanced from its initial applications in the mid 1990s, CBT has become an effective treatment to reduce positive and negative symptoms of schizophrenia, as well as improving functioning.[109][110] However, in a 2010 article in Psychological Medicine entitled, "Cognitive behavioral therapy for the major psychiatric disorder: does it really work?", Lynch, Laws and McKenna found that no trial employing both blinding and psychological placebo has found CBT to be effective in either reducing symptoms or preventing relapse in schizophrenia.[111]
Another approach is cognitive remediation, a technique aimed at remediating the neurocognitive deficits sometimes present in schizophrenia. Based on techniques of neuropsychological rehabilitation, early evidence has shown it to be cognitively effective, with some improvements related to measurable changes in brain activation as measured by fMRI.[112][113] A similar approach known as cognitive enhancement therapy, which focuses on social cognition as well as neurocognition, has shown efficacy.[114]
Family therapy or education, which addresses the whole family system of an individual with a diagnosis of schizophrenia, has been consistently found to be beneficial, at least if the duration of intervention is longer-term.[115][116][117] Aside from therapy, the effect of schizophrenia on families and the burden on carers has been recognized, with the increasing availability of self-help books on the subject.[118][119] There is also some evidence for benefits from social skills training, although there have also been significant negative findings.[120][121] Some studies have explored the possible benefits of music therapy and other creative therapies.[122][123][124]
The Soteria model is alternative to inpatient hospital treatment using a minimal medication approach. It is described as a milieu-therapeutic recovery method, characterized by its founder as "the 24 hour a day application of interpersonal phenomenologic interventions by a nonprofessional staff, usually without neuroleptic drug treatment, in the context of a small, homelike, quiet, supportive, protective, and tolerant social environment."[125] Although research evidence is limited, a 2008 systematic review found the programme equally as effective as treatment with medication in people diagnosed with first and second episode schizophrenia.[126]
Prognosis
Schizophrenia has great human and economics costs.[3] It results in a decreased life expectancy of 12—15 years primarily due to its association with obesity, little exercise, and smoking while an increased rate of suicide playing a lesser role.[3] Schizophrenia is known to be a major cause of disability with active psychosis ranked as the third-most-disabling condition after quadriplegia and dementia and ahead of paraplegia and blindness.[127] Most people however live independently with community support.[3]
There is a higher than average suicide rate associated with schizophrenia. This has been cited at 10%, but a more recent analysis of studies and statistics revises the estimate at 4.9%, most often occurring in the period following onset or first hospital admission.[128] Several times more attempt suicide.[129] There are a variety of reasons and risk factors.[130][131]
World Health Organization studies have noted that individuals diagnosed with schizophrenia have much better long-term outcomes in developing countries (India, Colombia and Nigeria) than in developed countries (United States, United Kingdom, Ireland, Denmark, Czech Republic, Slovakia, Japan, and Russia),[132] despite antipsychotic drugs not being widely available.
After long-term follow-up half of people with schizophrenia have a favourable outcome while 16% have a delayed recovery after an early unremitting course. More usually, the course in the first two years predicted the long-term course. Early social intervention was also related to a better outcome. The findings were held as important in moving patients, carers and clinicians away from the prevalent belief of the chronic nature of the condition.[133] This outcomes on average however is worse than for other psychotic and psychiatric disorders. While a moderate number of people with schizophrenia were seen to remit and remain well; the review raised the question that some may not require maintenance medication.[134]
A clinical study using strict recovery criteria (concurrent remission of positive and negative symptoms and adequate social and vocational functioning continuously for two years) found a recovery rate of 14% within the first five years.[135] A 5-year community study found that 62% showed overall improvement on a composite measure of clinical and functional outcomes.[136]
Epidemiology

Schizophrenia affects approximately 0.3—0.7% of people at some point in there life.[3] It occurs 1.4 times more frequently in males than females and typically appears earlier in men—the peak ages of onset are 20–28 years for males and 26–32 years for females.[4][2] Onset in childhood is much rarer,[137] as is onset in middle- or old age.[138] Despite the received wisdom that schizophrenia occurs at similar rates worldwide, its prevalence varies across the world,[139] within countries,[140] and at the local and neighbourhood level.[141] It causes approximately 1% of worldwide disability adjusted life years.[4] The rate of schizophrenia varies up to three fold depending on how it is defined.[3]
History
Accounts of a schizophrenia-like syndrome are thought to be rare in the historical record before the 1800s, although reports of irrational, unintelligible, or uncontrolled behavior were common. A detailed case report in 1797 concerning James Tilly Matthews, and accounts by Phillipe Pinel published in 1809, are often regarded as the earliest cases of the illness in the medical and psychiatric literature.[142] Schizophrenia was first described as a distinct syndrome affecting teenagers and young adults by Bénédict Morel in 1853, termed démence précoce (literally 'early dementia'). The term dementia praecox was used in 1891 by Arnold Pick to in a case report of a psychotic disorder. In 1893 Emil Kraepelin introduced a broad new distinction in the classification of mental disorders between dementia praecox and mood disorder (termed manic depression and including both unipolar and bipolar depression). Kraepelin believed that dementia praecox was primarily a disease of the brain,[143] and particularly a form of dementia, distinguished from other forms of dementia, such as Alzheimer's disease, which typically occur later in life.[144]
The word schizophrenia—which translates roughly as "splitting of the mind" and comes from the Greek roots schizein (σχίζειν, "to split") and phrēn, phren- (φρήν, φρεν-, "mind")[145]—was coined by Eugen Bleuler in 1908 and was intended to describe the separation of function between personality, thinking, memory, and perception. Bleuler described the main symptoms as 4 A's: flattened Affect, Autism, impaired Association of ideas and Ambivalence.[146] Bleuler realized that the illness was not a dementia as some of his patients improved rather than deteriorated and hence proposed the term schizophrenia instead.

In the early 1970s, the diagnostic criteria for schizophrenia was the subject of a number of controversies which eventually led to the operational criteria used today. It became clear after the 1971 US-UK Diagnostic Study that schizophrenia was diagnosed to a far greater extent in America than in Europe.[147] This was partly due to looser diagnostic criteria in the US, which used the DSM-II manual, contrasting with Europe and its ICD-9. David Rosenhan's 1972 study, published in the journal Science under the title On being sane in insane places, concluded that the diagnosis of schizophrenia in the US was often subjective and unreliable.[148] These were some of the factors in leading to the revision not only of the diagnosis of schizophrenia, but the revision of the whole DSM manual, resulting in the publication of the DSM-III in 1980.{subscription required}[149]
The term schizophrenia is commonly misunderstood to mean that affected persons have a "split personality". Although some people diagnosed with schizophrenia may hear voices and may experience the voices as distinct personalities, schizophrenia does not involve a person changing among distinct multiple personalities. The confusion arises in part due to the literal interpretation of Bleuler's term schizophrenia. The first known misuse of the term to mean "split personality" was in an article by the poet T. S. Eliot in 1933.[150] Treatment was revolutionized in the mid-1950s with the development and introduction of chlorpromazine.[151]
Society and culture
Schizophrenia has increasingly gained attention among the general public and the scientific community. Indeed, the November 11, 2010 issue of Nature was devoted to the theme of schizophrenia.[152]
Stigma
Social stigma has been identified as a major obstacle in the recovery of patients with schizophrenia.[153] In a large, representative sample from a 1999 study, 12.8% of Americans believed that individuals with schizophrenia were "very likely" to do something violent against others, and 48.1% said that they were "somewhat likely" to. Over 74% said that people with schizophrenia were either "not very able" or "not able at all" to make decisions concerning their treatment, and 70.2% said the same of money management decisions.[154] The perception of individuals with psychosis as violent has more than doubled in prevalence since the 1950s, according to one meta-analysis.[155]
In 2002, the Japanese Society of Psychiatry and Neurology changed the term for schizophrenia from Seishin-Bunretsu-Byō 精神分裂病 (mind-split-disease) to Tōgō-shitchō-shō 統合失調症 (integration disorder) to reduce stigma,[156] The new name was inspired by the biopsychosocial model, and it increased the percentage of cases in which patients were informed of the diagnosis from 36.7% to 69.7% over three years.[157]
Economic burden
In the United States alone, the overall cost of schizophrenia was estimated to be $62.7 billion in 2002.[158] These estimates include health care costs (e.g. outpatient, inpatient, drugs, and long-term care) and non-health care costs (e.g. law enforcement, reduced workplace productivity, and unemployment).
Cultural depictions
The book and film A Beautiful Mind chronicled the life of John Forbes Nash, a Nobel Prize-winning mathematician who was diagnosed with schizophrenia. The Marathi film Devrai (featuring Atul Kulkarni) is a presentation of a patient with schizophrenia. The film, set in Western India, shows the behavior, mentality, and struggle of the patient as well as his loved-ones. Other factual books have been written by relatives on family members; Australian journalist Anne Deveson told the story of her son's battle with schizophrenia in Tell Me I'm Here,[159] later made into a movie. The book The Eden Express by Mark Vonnegut recounts his struggle with schizophrenia and his recovering journey.
Research
Prevention
There is some evidence that early interventions in those with a psychotic episode may improve short term outcomes but that there is little benefit after 5 years.[3]
There are no reliable markers for the later development of schizophrenia although research is being conducted into how well a combination of genetic risk plus non-disabling psychosis-like experience predicts later diagnosis.[160] People who fulfill the 'ultra high-risk mental state' criteria, that include a family history of schizophrenia plus the presence of transient or self-limiting psychotic experiences, have a 20–40% chance of being diagnosed with the condition after one year.[161] The use of psychological treatments and medication has been found effective in reducing the chances of people who fulfill the 'high-risk' criteria from developing full-blown schizophrenia.[162] However, the treatment of people who may never develop schizophrenia is controversial,[163] in light of the side-effects of antipsychotic medication; particularly with respect to the potentially disfiguring tardive dyskinesia and the rare but potentially lethal neuroleptic malignant syndrome.[164] The most widely used form of preventative health care for schizophrenia takes the form of public education campaigns that provide information on risk factors and early symptoms, with the aim to improve detection and provide treatment earlier for those experiencing delays.[165] The new clinical approach early intervention in psychosis is a secondary prevention strategy to prevent further episodes and prevent the long term disability associated with schizophrenia.
Diagnostic controversies
The scientific validity of schizophrenia, and its defining symptoms such as delusions and hallucinations, have been criticised.[166][167] In 2006, a group of consumers and mental health professionals from the UK, under the banner of Campaign for Abolition of the Schizophrenia Label, argued for a rejection of the diagnosis of schizophrenia based on its heterogeneity and associated stigma, and called for the adoption of a biopsychosocial model. Other UK psychiatrists opposed the move arguing that the term schizophrenia is a useful, even if provisional concept.[168][169]
Similarly, there is an argument that the underlying issues would be better addressed as a spectrum of conditions[170] or as individual dimensions along which everyone varies rather than by a diagnostic category based on an arbitrary cut-off between normal and ill.[171] This approach appears consistent with research on schizotypy, and with a relatively high prevalence of psychotic experiences, mostly non-distressing delusional beliefs, among the general public.[172][173][174] In concordance with this observation, psychologist Edgar Jones, and psychiatrists Tony David and Nassir Ghaemi, surveying the existing literature on delusions, pointed out that the consistency and completeness of the definition of delusion have been found wanting by many; delusions are neither necessarily fixed, nor false, nor involve the presence of incontrovertible evidence.[175][176][177]
Nancy Andreasen, a leading figure in schizophrenia research, has criticized the current DSM-IV and ICD-10 criteria for sacrificing diagnostic validity for the sake of artificially improving reliability. She argues that overemphasis on psychosis in the diagnostic criteria, while improving diagnostic reliability, ignores more fundamental cognitive impairments that are harder to assess due to large variations in presentation.[178][179] This view is supported by other psychiatrists.[180] In the same vein, Ming Tsuang and colleagues argue that psychotic symptoms may be a common end-state in a variety of disorders, including schizophrenia, rather than a reflection of the specific etiology of schizophrenia, and warn that there is little basis for regarding DSM’s operational definition as the "true" construct of schizophrenia.[170] Neuropsychologist Michael Foster Green went further in suggesting the presence of specific neurocognitive deficits may be used to construct phenotypes that are alternatives to those that are purely symptom-based. These deficits take the form of a reduction or impairment in basic psychological functions such as memory, attention, executive function and problem solving.[181][182]
The exclusion of affective components from the criteria for schizophrenia, despite their ubiquity in clinical settings, has also caused contention. This exclusion in the DSM has resulted in a "rather convoluted" separate disorder—schizoaffective disorder.[180] Citing poor interrater reliability, some psychiatrists have totally contested the concept of schizoaffective disorder as a separate entity.[183][184] The categorical distinction between mood disorders and schizophrenia, known as the Kraepelinian dichotomy, has also been challenged by data from genetic epidemiology.[185]
An approach broadly known as the anti-psychiatry movement, most active in the 1960s, opposes the orthodox medical view of schizophrenia as an illness.[186][page needed] Psychiatrist Thomas Szasz argues that psychiatric patients are individuals with unconventional thoughts and behavior that society diagnoses as a method of social control, and therefore the diagnosis of "schizophrenia" is merely a form of social construction.[187] The Hearing Voices Movement argues that many people diagnosed as psychotic need their experiences to be accepted and valued rather than medicalized.
References
- ^ "Schizophrenia" Concise Medical Dictionary. Oxford University Press, 2010. Oxford Reference Online. Maastricht University Library. 29 June 2010 prepaid subscription only
- ^ a b Castle D, Wessely S, Der G, Murray RM. The incidence of operationally defined schizophrenia in Camberwell, 1965-84. The British Journal of Psychiatry. 1991;159:790–4. doi:10.1192/bjp.159.6.790. PMID 1790446.
- ^ a b c d e f g h i j k l m n o p q r s van Os J, Kapur S (2009). "Schizophrenia". Lancet. 374 (9690): 635–45. doi:10.1016/S0140-6736(09)60995-8. PMID 19700006.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ a b c d e f g h i j k l m n Picchioni MM, Murray RM (2007). "Schizophrenia". BMJ. 335 (7610): 91–5. doi:10.1136/bmj.39227.616447.BE. PMC 1914490. PMID 17626963.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ a b Becker T, Kilian R. Psychiatric services for people with severe mental illness across western Europe: what can be generalized from current knowledge about differences in provision, costs and outcomes of mental health care?. Acta Psychiatrica Scandinavica Supplement. 2006;429(429):9–16. doi:10.1111/j.1600-0447.2005.00711.x. PMID 16445476.
- ^ Sim K, Chua TH, Chan YH, Mahendran R, Chong SA. Psychiatric comorbidity in first episode schizophrenia: a 2 year, longitudinal outcome study. Journal of Psychiatric Research. 2006;40(7):656–63. doi:10.1016/j.jpsychires.2006.06.008. PMID 16904688.
- ^ a b Carson VB (2000). Mental health nursing: the nurse-patient journey W.B. Saunders. ISBN 9780721680538. pp 638.
- ^ Hirsch SR; Weinberger DR (2003). Schizophrenia. Wiley-Blackwell. p. 21. ISBN 9780632063888.
- ^ Brunet-Gouet E, Decety J. Social brain dysfunctions in schizophrenia: a review of neuroimaging studies. Psychiatry Res. 2006;148(2-3):75–92. doi:10.1016/j.pscychresns.2006.05.001. PMID 17088049.
- ^ Hirsch SR; WeinbergerDR (2003). Schizophrenia. Wiley-Blackwell. p. 481. ISBN 9780632063888.
- ^ Ungvari GS, Caroff SN, Gerevich J. The catatonia conundrum: evidence of psychomotor phenomena as a symptom dimension in psychotic disorders. Schizophr Bull. 2010;36(2):231–8. doi:10.1093/schbul/sbp105. PMID 19776208.
- ^ Cullen KR, Kumra S, Regan J et al.. Atypical Antipsychotics for Treatment of Schizophrenia Spectrum Disorders. Psychiatric Times. 2008;25(3).
- ^ Addington J. North American prodrome longitudinal study: a collaborative multisite approach to prodromal schizophrenia research. Schizophrenia Bulletin. 2007;33(3):665–72. doi:10.1093/schbul/sbl075. PMID 17255119.
- ^ Parnas J. Pre-morbid psychopathology in schizophrenia spectrum. British Journal of Psychiatry. 1989;115:623–7. PMID 2611591.
- ^ Amminger GP. Early onset of symptoms predicts conversion to non-affective psychosis in ultra-high risk individuals. Schizophrenia Research. 2006;84(1):67–76. doi:10.1016/j.schres.2006.02.018. PMID 16677803.
- ^ Clinical Psychopathology. 5 ed. New York: Grune & Stratton; 1959.
- ^ Nordgaard J, Arnfred SM, Handest P, Parnas J. The diagnostic status of first-rank symptoms. Schizophrenia Bulletin. 2008;34(1):137–54. doi:10.1093/schbul/sbm044. PMID 17562695.
- ^ Sims A. Symptoms in the mind: an introduction to descriptive psychopathology. Philadelphia: W. B. Saunders; 2002. ISBN 0-7020-2627-1.
- ^ American Psychiatric Association. Task Force on DSM-IV. (2000). Diagnostic and statistical manual of mental disorders: DSM-IV-TR. American Psychiatric Pub. ISBN 9780890420256. pp 299
- ^ Kneisl C. and Trigoboff E.(2009). Contemporary Psychiatric- Mental Health Nursing. 2nd edition. London: Pearson Prentice Ltd. pp.371
- ^ American Psychiatric Association. Task Force on DSM-IV. (2000). Diagnostic and statistical manual of mental disorders: DSM-IV-TR. American Psychiatric Pub. ISBN 9780890420256. pp 299.
- ^ Velligan DI and Alphs LD. Negative Symptoms in Schizophrenia: The Importance of Identification and Treatment. Psychiatric Times. March 1, 2008;25(3).
- ^ Carson VB (2000). Mental health nursing: the nurse-patient journey W.B. Saunders. ISBN 9780721680538. pp638.
- ^ O'Donovan MC, Williams NM, Owen MJ. Recent advances in the genetics of schizophrenia. Hum. Mol. Genet.. 2003;12 Spec No 2:R125–33. doi:10.1093/hmg/ddg302. PMID 12952866.
- ^ Owen MJ, Craddock N, O'Donovan MC. Schizophrenia: genes at last?. Trends Genet.. 2005;21(9):518–25. doi:10.1016/j.tig.2005.06.011. PMID 16009449.
- ^ Craddock N, O'Donovan MC, Owen MJ. Genes for schizophrenia and bipolar disorder? Implications for psychiatric nosology. Schizophr Bull. 2006;32(1):9–16. doi:10.1093/schbul/sbj033. PMID 16319375.
- ^ Datta SR, McQuillin A, Rizig M, et al.. A threonine to isoleucine missense mutation in the pericentriolar material 1 gene is strongly associated with schizophrenia. Mol. Psychiatry. 2010;15(6):615–28. doi:10.1038/mp.2008.128. PMID 19048012.
- ^ Hennah W, Thomson P, McQuillin A, et al.. DISC1 association, heterogeneity and interplay in schizophrenia and bipolar disorder. Mol. Psychiatry. 2009;14(9):865–73. doi:10.1038/mp.2008.22. PMID 18317464.
- ^ O'Donovan MC, Craddock NJ, Owen MJ. Genetics of psychosis; insights from views across the genome. Hum. Genet.. 2009;126(1):3–12. doi:10.1007/s00439-009-0703-0. PMID 19521722.
- ^ Purcell SM, Wray NR, Stone JL, et al.. Common polygenic variation contributes to risk of schizophrenia and bipolar disorder. Nature. 2009;460(7256):748–52. doi:10.1038/nature08185. PMID 19571811.
- ^ Sanders AR, Duan J, Levinson DF, et al.. No significant association of 14 candidate genes with schizophrenia in a large European ancestry sample: implications for psychiatric genetics. Am J Psychiatry. 2008;165(4):497–506. doi:10.1176/appi.ajp.2007.07101573. PMID 18198266.
- ^ Walsh T, McClellan JM, McCarthy SE et al.. Rare structural variants disrupt multiple genes in neurodevelopmental pathways in schizophrenia. Science. 2008;320(5875):539–43. doi:10.1126/science.1155174. PMID 18369103.
- ^ Kirov G, Grozeva D, Norton N et al.. Support for the involvement of large CNVs in the pathogenesis of schizophrenia. Hum Mol Genet. 2009;18(8):1497. doi:10.1093/hmg/ddp043. PMID 19181681.
- ^ The International Schizophrenia Consortium. Rare chromosomal deletions and duplications increase risk of schizophrenia. Nature. 11 September 2008;455(7210):237–41. doi:10.1038/nature07239. PMID 18668038.
- ^ Crespi B, Stead P, Elliot M. Evolution in health and medicine Sackler colloquium: Comparative genomics of autism and schizophrenia. Proc. Natl. Acad. Sci. U.S.A.. 2010;107 Suppl 1:1736–41. doi:10.1073/pnas.0906080106. PMID 19955444.
- ^ Crow TJ. The 'big bang' theory of the origin of psychosis and the faculty of language. Schizophrenia Research. 2008;102(1–3):31–52. doi:10.1016/j.schres.2008.03.010. PMID 18502103.
- ^ Mueser KT, Jeste DV. Clinical Handbook of Schizophrenia. New York: Guilford Press; 2008. ISBN 1593856520. p. 22–23.
- ^ Van Os J. Does the urban environment cause psychosis?. British Journal of Psychiatry. 2004;184(4):287–288. doi:10.1192/bjp.184.4.287. PMID 15056569.
- ^ Selten JP, Cantor-Graae E, Kahn RS. Migration and schizophrenia. Current Opinion in Psychiatry. 2007 [Retrieved 2008-07-06];20(2):111–115. doi:10.1097/YCO.0b013e328017f68e. PMID 17278906.
- ^ Moore THM, Zammit S, Lingford-Hughes A et al.. Cannabis use and risk of psychotic or affective mental health outcomes: a systematic review. Lancet. 2007;370(9584):319–328. doi:10.1016/S0140-6736(07)61162-3. PMID 17662880.
- ^ Degenhardt L, Hall W, Lynskey M. Comorbidity between cannabis use and psychosis: Modelling some possible relationships. [PDF]. 2001 [Retrieved 2006-08-19].
- ^ Frisher M, Crome I, Martino O, Croft P. Assessing the impact of cannabis use on trends in diagnosed schizophrenia in the United Kingdom from 1996 to 2005. Schizophr. Res.. 2009;113(2-3):123–8. doi:10.1016/j.schres.2009.05.031. PMID 19560900.
- ^ http://www.nhsconfed.org/Publications/Documents/MHN_factsheet_August_2009_FINAL_2.pdf Key facts and trends in mental health, National Health Service, 2009
- ^ Gregg L, Barrowclough C, Haddock G. Reasons for increased substance use in psychosis. Clin Psychol Rev. 2007;27(4):494–510. doi:10.1016/j.cpr.2006.09.004. PMID 17240501.
- ^ Kuczenski R, Segal DS. Effects of methylphenidate on extracellular dopamine, serotonin, and norepinephrine: comparison with amphetamine. J. Neurochem.. 1997;68(5):2032–7. doi:10.1046/j.1471-4159.1997.68052032.x. PMID 9109529.
- ^ Mahoney JJ, Kalechstein AD, De La Garza R, Newton TF. Presence and persistence of psychotic symptoms in cocaine- versus methamphetamine-dependent participants. The American Journal on Addictions. 2008;17(2):83–98. doi:10.1080/10550490701861201. PMID 18393050.
- ^ Larson, Michael (2006-03-30). "Alcohol-Related Psychosis". eMedicine. WebMD. Retrieved September 27, 2006.
- ^ Soyka, M. Psychopathological characteristics in alcohol hallucinosis and paranoid schizophrenia. Acta Psychiatrica Scandinavica. 1990;81(3):255–9. doi:10.1111/j.1600-0447.1990.tb06491.x. PMID 2343749.
- ^ Gossman, William. WebMD. Delirium Tremens; November 19, 2005 [Retrieved October 16, 2006].
- ^ Broome MR, Woolley JB, Tabraham P, et al.. What causes the onset of psychosis?. Schizophr. Res.. 2005;79(1):23–34. doi:10.1016/j.schres.2005.02.007. PMID 16198238.
- ^ Lewis R. Should cognitive deficit be a diagnostic criterion for schizophrenia?. Journal of Psychiatry and Neuroscience. 2004;29(2):102–113. PMID 15069464.
- ^ Brüne M, Abdel-Hamid M, Lehmkämper C, Sonntag C. Mental state attribution, neurocognitive functioning, and psychopathology: what predicts poor social competence in schizophrenia best?. Schizophr. Res.. 2007;92(1-3):151–9. doi:10.1016/j.schres.2007.01.006. PMID 17346931.
- ^ Sitskoorn MM. Cognitive deficits in relatives of patients with schizophrenia: a meta-analysis. Schizophrenia Research. 2004;71(2):285–295. doi:10.1016/j.schres.2004.03.007. PMID 15474899.
- ^ Bentall RP. Prospects for a cognitive-developmental account of psychotic experiences. Br J Clin Psychol. 2007;46(Pt 2):155–73. doi:10.1348/014466506X123011. PMID 17524210.
- ^ Kurtz MM. Neurocognitive impairment across the lifespan in schizophrenia: an update. Schizophrenia Research. 2005;74(1):15–26. doi:10.1016/j.schres.2004.07.005. PMID 15694750.
- ^ Cohen AS. Affective reactivity of speech and emotional experience in patients with schizophrenia. Schizophrenia Research. 2004;69(1):7–14. doi:10.1016/S0920-9964(03)00069-0. PMID 15145465.
- ^ Horan WP. Emotional responses to psychosocial stress in schizophrenia: the role of individual differences in affective traits and coping. Schizophrenia Research. 2003;60(2–3):271–83. doi:10.1016/S0920-9964(02)00227-X. PMID 12591589.
- ^ Barrowclough C. Self-esteem in schizophrenia: relationships between self-evaluation, family attitudes, and symptomatology. J Abnorm Psychol. 2003;112(1):92–9. doi:10.1037/0021-843X.112.1.92. PMID 12653417.
- ^ Birchwood M. The power and omnipotence of voices: subordination and entrapment by voices and significant others. Psychol Med. 2000;30(2):337–44. doi:10.1017/S0033291799001828. PMID 10824654.
- ^ Smith B, Fowler DG, Freeman D, et al.. Emotion and psychosis: links between depression, self-esteem, negative schematic beliefs and delusions and hallucinations. Schizophr. Res.. 2006;86(1-3):181–8. doi:10.1016/j.schres.2006.06.018. PMID 16857346.
- ^ Beck, AT. A Cognitive Model of Schizophrenia. Journal of Cognitive Psychotherapy. 2004;18(3):281–88. doi:10.1891/jcop.18.3.281.65649.
- ^ Bell V. Explaining delusions: a cognitive perspective. Trends in Cognitive Science. 2006;10(5):219–26. doi:10.1016/j.tics.2006.03.004. PMID 16600666.
- ^ Freeman D, Garety PA, Kuipers E, Fowler D, Bebbington PE, Dunn G. Acting on persecutory delusions: the importance of safety seeking. Behav Res Ther. 2007;45(1):89–99. doi:10.1016/j.brat.2006.01.014. PMID 16530161.
- ^ Kuipers E, Garety P, Fowler D, Freeman D, Dunn G, Bebbington P. Cognitive, emotional, and social processes in psychosis: refining cognitive behavioral therapy for persistent positive symptoms. Schizophr Bull. 2006;32 Suppl 1:S24–31. doi:10.1093/schbul/sbl014. PMID 16885206.
- ^ Meyer-Lindenberg A. Reduced prefrontal activity predicts exaggerated striatal dopaminergic function in schizophrenia. Nature Neuroscience. 2002;5(3):267–71. doi:10.1038/nn804. PMID 11865311.
- ^ The Boundaries of Consciousness. Amsterdam: Elsevier; 2006. ISBN 0444528768. Functional brain imaging of symptoms and cognition in schizophrenia. p. 302.
- ^ Insel, TR (2010). "Rethinking Schizophrenia". Nature. 468: 188–93.
{{cite journal}}: Cite has empty unknown parameter:|author-name-separator=(help); Unknown parameter|author-separator=ignored (help) - ^ Green MF. Cognitive impairment and functional outcome in schizophrenia and bipolar disorder. Journal of Clinical Psychiatry. 2006;67(Suppl 9):3–8. PMID 16965182.
- ^ Laruelle M, Abi-Dargham A, van Dyck CH, et al.. Single photon emission computerized tomography imaging of amphetamine-induced dopamine release in drug-free schizophrenic subjects. Proc. Natl. Acad. Sci. U.S.A.. 1996;93(17):9235–40. doi:10.1073/pnas.93.17.9235. PMID 8799184.
- ^ Jones HM. Dopamine and antipsychotic drug action revisited. British Journal of Psychiatry. 2002;181:271–275. doi:10.1192/bjp.181.4.271. PMID 12356650.
- ^ Konradi C. Molecular aspects of glutamate dysregulation: implications for schizophrenia and its treatment. Pharmacology and Therapeutics. 2003;97(2):153–79. doi:10.1016/S0163-7258(02)00328-5. PMID 12559388.
- ^ Lahti AC. Effects of ketamine in normal and schizophrenic volunteers. Neuropsychopharmacology. 2001;25(4):455–67. doi:10.1016/S0893-133X(01)00243-3. PMID 11557159.
- ^ Coyle JT. Converging evidence of NMDA receptor hypofunction in the pathophysiology of schizophrenia. Annals of the New York Academy of Sciences. 2003;1003:318–27. doi:10.1196/annals.1300.020. PMID 14684455.
- ^ Tuominen HJ. Glutamatergic drugs for schizophrenia: a systematic review and meta-analysis. Schizophrenia Research. 2005;72(2-3):225–34. doi:10.1016/j.schres.2004.05.005. PMID 15560967.
- ^ http://books.google.com/books?id=AQeQa5AtpXoC&pg=PA215&lpg=PA215&source=bl&ots=_AZBdDkZOg&sig=cyrLwQRUUijGlvTRNVpmKoLJmpc&hl=en&ei=C9HMTI3mJ5DSsAPbhNzzDg&sa=X&oi=book_result&ct=result&resnum=2&ved=0CBcQ6AEwAQ#v=onepage&q&f=false
- ^ http://www.nature.com/npp/journal/v31/n4/abs/1300838a.html
- ^ http://www.sciencedirect.com/science?_ob=ArticleURL&_udi=B6WN4-4CCGGN1-9P&_user=10&_coverDate=11%2F30%2F1984&_rdoc=1&_fmt=high&_orig=search&_origin=search&_sort=d&_docanchor=&view=c&_searchStrId=1520587233&_rerunOrigin=scholar.google&_acct=C000050221&_version=1&_urlVersion=0&_userid=10&md5=5e43884bdf1f204eb2356e02096708bc&searchtype=a
- ^ a b http://sciencelinks.jp/j-east/article/200707/000020070707A0194475.php
- ^ Steen RG, Mull C, McClure R, Hamer RM, Lieberman JA. Brain volume in first-episode schizophrenia: systematic review and meta-analysis of magnetic resonance imaging studies. Br J Psychiatry. 2006;188:510–8. doi:10.1192/bjp.188.6.510. PMID 16738340.
- ^ Lieberman JA, Bymaster FP, Meltzer HY, et al.. Antipsychotic drugs: comparison in animal models of efficacy, neurotransmitter regulation, and neuroprotection. Pharmacol. Rev.. 2008;60(3):358–403. doi:10.1124/pr.107.00107. PMID 18922967.
- ^ DeLisi LE. The concept of progressive brain change in schizophrenia: implications for understanding schizophrenia. Schizophr Bull. 2008;34(2):312–21. doi:10.1093/schbul/sbm164. PMID 18263882. PMC 2632405.
- ^ Ellison-Wright I, Bullmore E. Meta-analysis of diffusion tensor imaging studies in schizophrenia. Schizophr. Res.. 2009;108(1–3):3–10. doi:10.1016/j.schres.2008.11.021. PMID 19128945.
- ^ Broyd SJ, Demanuele C, Debener S, Helps SK, James CJ, Sonuga-Barke EJS. Default-mode brain dysfunction in mental disorders: a systematic review. Neurosci Biobehav Rev. 2008;33(3):279. doi:10.1016/j.neubiorev.2008.09.002. PMID 18824195.
- ^ Jakobsen KD. Reliability of clinical ICD-10 schizophrenia diagnoses. Nordic Journal of Psychiatry. 2005;59(3):209–12. doi:10.1080/08039480510027698. PMID 16195122.
- ^ a b c American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-IV. Washington, DC: American Psychiatric Publishing, Inc.; 2000 [Retrieved 2008-07-04]. ISBN 0-89042-024-6. Schizophrenia.
- ^ Pope HG. Distinguishing bipolar disorder from schizophrenia in clinical practice: guidelines and case reports [PDF]. Hospital and Community Psychiatry. 1983 [Retrieved 2008-02-24];34:322–28.
- ^ McGlashan TH. Testing DSM-III symptom criteria for schizotypal and borderline personality disorders. Archives of General Psychiatry. 1987 [Retrieved 2008-07-03];44(2):143–8. PMID 3813809.
- ^ Bottas A. Comorbidity: Schizophrenia With Obsessive-Compulsive Disorder. Psychiatric Times. April 15, 2009;26(4).
- ^ American Psychiatric Association DSM-5 Work Groups (2010) Proposed Revisions - Schizophrenia and Other Psychotic Disorders. Retrieved 17 February 2010.
- ^ Cognitive training for supported employment: 2-3 year outcomes of a randomized controlled trial.. American Journal of Psychiatry. 2007;164(3):437–41. doi:10.1176/appi.ajp.164.3.437. PMID 17329468.
- ^ Outcome of schizophrenia: some transcultural observations with particular reference to developing countries.. Eur Arch Psychiatry Clin Neurosci. 1994;244(5):227–35. doi:10.1007/BF02190374. PMID 7893767.
- ^ Gorczynski P, Faulkner G (2010). "Exercise therapy for schizophrenia". Cochrane Database Syst Rev (5): CD004412. doi:10.1002/14651858.CD004412.pub2. PMID 20464730.
- ^ National Collaborating Centre for Mental Health. Gaskell and the British Psychological Society. Schizophrenia: Full national clinical guideline on core interventions in primary and secondary care [PDF]; 2009-03-25 [Retrieved 2009-11-25].
- ^ Murphy BP, Chung YC, Park TW, McGorry PD. Pharmacological treatment of primary negative symptoms in schizophrenia: a systematic review. Schizophrenia Research. 2006;88(1–3):5–25. doi:10.1016/j.schres.2006.07.002. PMID 16930948.
- ^ Gray JA, Roth BL. The pipeline and future of drug development in schizophrenia. Molecular Psychiatry. 2007;12(10):904–22. doi:10.1038/sj.mp.4002062. PMID 17667958.
- ^ Jarskog LF, Miyamoto S, Lieberman JA. Schizophrenia: new pathological insights and therapies. Annu. Rev. Med.. 2007;58:49–61. doi:10.1146/annurev.med.58.060904.084114. PMID 16903799.
- ^ Tandon R, Keshavan MS, Nasrallah HA. Schizophrenia, "Just the Facts": what we know in 2008 part 1: overview. Schizophrenia Research. 2008;100(1-3):4–19. doi:10.1016/j.schres.2008.01.022. PMID 18291627.
- ^ Kane JM, Correll CU (2010). "Pharmacologic treatment of schizophrenia". Dialogues Clin Neurosci. 12 (3): 345–57. PMID 20954430.
- ^ a b Schultz SH, North SW, Shields CG (2007). "Schizophrenia: a review". Am Fam Physician. 75 (12): 1821–9. PMID 17619525.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Wahlbeck K, Cheine MV, Essali A. Clozapine versus typical neuroleptic medication for schizophrenia. The Cochrane Database of Systematic Reviews. 2007;(2):CD000059. doi:10.1002/14651858.CD000059. PMID 10796289.
- ^ Leucht S, Wahlbeck K, Hamann J, Kissling W. New generation antipsychotics versus low-potency conventional antipsychotics: a systematic review and meta-analysis. Lancet. 2003 [Retrieved 2008-07-04];361(9369):1581–89. doi:10.1016/S0140-6736(03)13306-5. PMID 12747876.
- ^ Ananth J, Parameswaran S, Gunatilake S, Burgoyne K, Sidhom T. Neuroleptic malignant syndrome and atypical antipsychotic drugs. Journal of Clinical Psychiatry. 2004 [Retrieved 2008-07-04];65(4):464–70. doi:10.4088/JCP.v65n0403. PMID 15119907.
- ^ Meltzer HY. Treatment-resistant schizophrenia—the role of clozapine. Current Medical Research and Opinion. 1997;14(1):1–20. doi:10.1185/03007999709113338. PMID 9524789.
- ^ Moran, M. Psychosocial Treatment Often Missing From Schizophrenia Regimens. Psychiatric News. 18 November 2005 [Retrieved 17 May 2007];40(22):24.
- ^ Sensky T, Turkington D, Kingdon D, Scott JL, Scott J, Siddle R, O'Carroll M, Barnes TR. A randomized controlled trial of cognitive-behavioral therapy for persistent symptoms in schizophrenia resistant to medication. Archives of General Psychiatry. 2000;57(2):165–72. doi:10.1001/archpsyc.57.2.165. PMID 10665619.
- ^ Kuipers E, Garety P, Fowler D, Dunn G, Bebbington P, Freeman D, Hadley C. London-East Anglia randomised controlled trial of cognitive-behavioural therapy for psychosis. I: effects of the treatment phase. Br J Psychiatry. 1997;171:319–27. doi:10.1192/bjp.171.4.319. PMID 9373419.
- ^ Lewis S, Tarrier N, Haddock G, Bentall R, Kinderman P, Kingdon D, Siddle R, Drake R, Everitt J, Leadley K, Benn A, Grazebrook K, Haley C, Akhtar S, Davies L, Palmer S, Faragher B, Dunn G. Randomised controlled trial of cognitive-behavioural therapy in early schizophrenia: acute-phase outcomes. Br J Psychiatry Suppl. 2002;43:s91–7. PMID 12271807.
- ^ Cormac I, Jones C, Campbell C. Cognitive behaviour therapy for schizophrenia. Cochrane Database of systematic reviews. 2002 [Retrieved 2008-07-03];(1):CD000524. doi:10.1002/14651858.CD000524. PMID 11869579.
- ^ Wykes T, Steel C, Everitt B, Tarrier N. Cognitive behavior therapy for schizophrenia: effect sizes, clinical models, and methodological rigor. Schizophr Bull. 2008;34(3):523–37. doi:10.1093/schbul/sbm114. PMID 17962231.
- ^ Zimmermann G, Favrod J, Trieu VH, Pomini V. The effect of cognitive behavioral treatment on the positive symptoms of schizophrenia spectrum disorders: a meta-analysis. Schizophrenia Research. 2005 [Retrieved 2008-07-03];77(1):1–9. doi:10.1016/j.schres.2005.02.018. PMID 16005380.
- ^ Lynch D, Laws KR, McKenna PJ. Cognitive behavioural therapy for major psychiatric disorder: does it really work? A meta-analytical review of well-controlled trials. Psychol Med. 2010;40(1):9–24. doi:10.1017/S003329170900590X. PMID 19476688.
- ^ Wykes T, Brammer M, Mellers J, et al.. Effects on the brain of a psychological treatment: cognitive remediation therapy: functional magnetic resonance imaging in schizophrenia. British Journal of Psychiatry. 2002 [Retrieved 2008-07-03];181:144–52. doi:10.1192/bjp.181.2.144. PMID 12151286.
- ^ Medalia A. Cognitive Remediation for Psychiatric Patients: Improving Functional Outcomes for Patients With Schizophrenia. Psychiatric Times. 2009;26(3).
- ^ Hogarty GE, Flesher S, Ulrich R, et al.. Cognitive enhancement therapy for schizophrenia: effects of a 2-year randomized trial on cognition and behavior. Archives of General Psychiatry. 2004 [Retrieved 2008-07-03];61(9):866–76. doi:10.1001/archpsyc.61.9.866. PMID 15351765.
- ^ McFarlane WR, Dixon L, Lukens E, Lucksted A. Family psychoeducation and schizophrenia: a review of the literature. J Marital Fam Ther. 2003;29(2):223–45. doi:10.1111/j.1752-0606.2003.tb01202.x. PMID 12728780.
- ^ Glynn SM, Cohen AN, Niv N. New challenges in family interventions for schizophrenia. Expert Review of Neurotherapeutics. 2007 [Retrieved 2008-07-03];7(1):33–43. doi:10.1586/14737175.7.1.33. PMID 17187495.
- ^ Family intervention for schizophrenia.. Cochrane Database Syst Rev. 2006;(4):CD000088. doi:10.1002/14651858.CD000088.pub2. PMID 17054127.
- ^ Jones S, Hayward P. Coping with Schizophrenia: A Guide for Patients, Families and Caregivers. Oxford, England: Oneworld Pub.; 2004. ISBN 1-85168-344-5.
- ^ Torrey EF. Surviving Schizophrenia: A Manual for Families, Consumers, and Providers. 5th ed. HarperCollins; 2006. ISBN 0-06-084259-8.
- ^ Kopelowicz A, Liberman RP, Zarate R. Recent advances in social skills training for schizophrenia. Schizophrenia Bulletin. 2006 [Retrieved 2008-07-03];32 Suppl 1:S12–23. doi:10.1093/schbul/sbl023. PMID 16885207. PMC 2632540.
- ^ American Psychiatric Association (2004). "Practice Guideline for the Treatment of Patients With Schizophrenia. Second Edition". USA: National Guideline Clearinghouse.
{{cite web}}: Unknown parameter|month=ignored (help) - ^ Talwar N, Crawford MJ, Maratos A, Nur U, McDermott O, Procter S. Music therapy for in-patients with schizophrenia: exploratory randomised controlled trial. The British Journal of Psychiatry. 2006 [Retrieved 2008-07-03];189:405–9. doi:10.1192/bjp.bp.105.015073. PMID 17077429.
- ^ Art therapy for schizophrenia or schizophrenia-like illnesses.. Cochrane Database Syst Rev. 2005;(4):CD003728. doi:10.1002/14651858.CD003728.pub2. PMID 16235338.
- ^ Drama therapy for schizophrenia or schizophrenia-like illnesses.. Cochrane Database Syst Rev. 2007;(1):CD005378. doi:10.1002/14651858.CD005378.pub2. PMID 17253555.
- ^ Mosher LR. Soteria and other alternatives to acute psychiatric hospitalization: a personal and professional review. Journal of Nervous and Mental Disease. 1999 [Retrieved 2008-07-03];187(3):142–9. doi:10.1097/00005053-199903000-00003. PMID 10086470.
- ^ Calton T, Ferriter M, Huband N, Spandler H. A systematic review of the Soteria paradigm for the treatment of people diagnosed with schizophrenia. Schizophrenia Bulletin. 2008 [Retrieved 2008-07-03];34(1):181–92. doi:10.1093/schbul/sbm047. PMID 17573357. PMC 2632384.
- ^ Ustun TB. Multiple-informant ranking of the disabling effects of different health conditions in 14 countries. The Lancet. 1999;354(9173):111–15. doi:10.1016/S0140-6736(98)07507-2. PMID 10408486.
- ^ Palmer BA, Pankratz VS, Bostwick JM. The lifetime risk of suicide in schizophrenia: a reexamination. Archives of General Psychiatry. 2005;62(3):247–53. doi:10.1001/archpsyc.62.3.247. PMID 15753237.
- ^ Radomsky ED, Haas GL, Mann JJ, Sweeney JA. Suicidal behavior in patients with schizophrenia and other psychotic disorders. American Journal of Psychiatry. 1 October 1999 [Retrieved 2008-07-04];156(10):1590–5. PMID 10518171.
- ^ Caldwell CB, Gottesman II. Schizophrenics kill themselves too: a review of risk factors for suicide. Schizophr Bull. 1990;16(4):571–89. PMID 2077636.
- ^ Dalby JT, Williams RJ. Depression in schizophrenics. New York: Plenum Press; 1989. ISBN 0-306-43240-4.
- ^ Hopper K, Wanderling J. Revisiting the developed versus developing country distinction in course and outcome in schizophrenia: results from ISoS, the WHO collaborative followup project. International Study of Schizophrenia. Schizophrenia Bulletin. 1 January 2000 [Retrieved 2008-07-04];26(4):835–46. PMID 11087016.
- ^ Harrison G, Hopper K, Craig T, et al.. Recovery from psychotic illness: a 15- and 25-year international follow-up study. British Journal of Psychiatry. 2001 [Retrieved 2008-07-04];178:506–17. doi:10.1192/bjp.178.6.506. PMID 11388966.
- ^ Jobe TH, Harrow M. Long-term outcome of patients with schizophrenia: a review [PDF]. Canadian Journal of Psychiatry. 2005 [Retrieved 2008-07-05];50(14):892–900. PMID 16494258.
- ^ Robinson DG, Woerner MG, McMeniman M, Mendelowitz A, Bilder RM. Symptomatic and functional recovery from a first episode of schizophrenia or schizoaffective disorder. American Journal of Psychiatry. 2004 [Retrieved 2008-07-04];161(3):473–9. doi:10.1176/appi.ajp.161.3.473. PMID 14992973.
- ^ Harvey CA, Jeffreys SE, McNaught AS, Blizard RA, King MB. The Camden Schizophrenia Surveys III: Five-Year Outcome of a Sample of Individuals From a Prevalence Survey and the Importance of Social Relationships. International Journal of Social Psychiatry. 2007 [Retrieved 2008-07-04];53(4):340–356. doi:10.1177/0020764006074529. PMID 17703650.
- ^ Kumra S. Childhood-onset schizophrenia: research update. Canadian Journal of Psychiatry. 2001;46(10):923–30. PMID 11816313.
- ^ Psychosis in the Elderly. London: Taylor and Francis.; 2005. ISBN 1841843946. p. 6.
- ^ Jablensky A. Schizophrenia: manifestations, incidence and course in different cultures. A World Health Organization ten-country study. Psychological Medicine Monograph Supplement. 1992;20:1–97. doi:10.1017/S0264180100000904. PMID 1565705.
- ^ Kirkbride JB, Fearon P, Morgan C, et al.. Heterogeneity in incidence rates of schizophrenia and other psychotic syndromes: findings from the 3-center AeSOP study. Archives of General Psychiatry. 2006;63(3):250–8. doi:10.1001/archpsyc.63.3.250. PMID 16520429.
- ^ Kirkbride JB. Neighbourhood variation in the incidence of psychotic disorders in Southeast London. Social Psychiatry and Psychiatric Epidemiology. 2007;42(6):438–45. doi:10.1007/s00127-007-0193-0. PMID 17473901.
- ^ Heinrichs RW. Historical origins of schizophrenia: two early madmen and their illness. Journal of the History of the Behavioral Sciences. 2003;39(4):349–63. doi:10.1002/jhbs.10152. PMID 14601041.
- ^ Kraepelin E, Diefendorf AR. Text book of psychiatry. 7 ed. London: Macmillan; 1907.
- ^ Hansen RA, Atchison B. Conditions in occupational therapy: effect on occupational performance. Hagerstown, MD: Lippincott Williams & Wilkins; 2000. ISBN 0-683-30417-8.
- ^ Kuhn R;. Eugen Bleuler's concepts of psychopathology. History of Psychiatry. 2004;15(3):361–6. doi:10.1177/0957154X04044603. PMID 15386868.
- ^ Stotz-Ingenlath G. Epistemological aspects of Eugen Bleuler's conception of schizophrenia in 1911 [PDF]. Medicine, Health Care and Philosophy. 2000 [Retrieved 2008-07-03];3(2):153–9. doi:10.1023/A:1009919309015. PMID 11079343.
- ^ Wing JK. International comparisons in the study of the functional psychoses. British Medical Bulletin. 1971;27(1):77–81. PMID 4926366.
- ^ Rosenhan D. On being sane in insane places. Science. 1973;179(70):250–8. doi:10.1126/science.179.4070.250. PMID 4683124.
- ^ Wilson M. DSM-III and the transformation of American psychiatry: a history. American Journal of Psychiatry. 1993 [Retrieved 2008-07-03];150(3):399–410. PMID 8434655.{subscription required}
- ^ Porter, Roy; Berrios, G. E.. A history of clinical psychiatry: the origin and history of psychiatric disorders. London: Athlone Press; 1995. ISBN 0-485-24211-7.
- ^ Turner T.. Unlocking psychosis. British Medical Journal. 2007;334(suppl):s7. doi:10.1136/bmj.39034.609074.94. PMID 17204765.
- ^ Editor (2010). "Combating Schizophrenia". Nature. 468: 133.
{{cite journal}}:|last1=has generic name (help); Cite has empty unknown parameter:|author-name-separator=(help); Unknown parameter|author-separator=ignored (help) - ^ Maj, Mario and Sartorius N.. Schizophrenia. Chichester: Wiley; 15 September 1999. ISBN 978-0-471-99906-5. p. 292.
- ^ Pescosolido BA, Monahan J, Link BG, Stueve A, Kikuzawa S. The public's view of the competence, dangerousness, and need for legal coercion of persons with mental health problems. American Journal of Public Health. 1999 [Retrieved 2008-07-03];89(9):1339–45. doi:10.2105/AJPH.89.9.1339. PMID 10474550. PMC 1508769.
- ^ Phelan JC, Link BG, Stueve A, Pescosolido BA. Public Conceptions of Mental Illness in 1950 and 1996: What Is Mental Illness and Is It to be Feared?. Journal of Health and Social Behavior. 2000;41(2):188–207. doi:10.2307/2676305.
- ^ Kim Y, Berrios GE. Impact of the term schizophrenia on the culture of ideograph: the Japanese experience. Schizophr Bull. 2001;27(2):181–5. PMID 11354585.
- ^ Sato M. Renaming schizophrenia: a Japanese perspective. World Psychiatry. 2004;5(1):53–55. PMID 16757998.
- ^ Wu EQ. The economic burden of schizophrenia in the United States in 2002. J Clin Psychiatry. 2005;66(9):1122–9. PMID 16187769.
- ^ Deveson A. Tell Me I'm Here. Penguin; 1991. ISBN 0-14-027257-7.
- ^ Cannon TD, Cornblatt B, McGorry P. The empirical status of the ultra high-risk (prodromal) research paradigm. Schizophrenia Bulletin. 2007 [Retrieved 2008-07-06];33(3):661–4. doi:10.1093/schbul/sbm031. PMID 17470445. PMC 2526144.
- ^ Drake RJ, Lewis SW. Early detection of schizophrenia. Current Opinion in Psychiatry. 2005 [Retrieved 2008-07-06];18(2):147–50. doi:10.1097/00001504-200503000-00007. PMID 16639167.
- ^ Van Os J, Delespaul P. Toward a world consensus on prevention of schizophrenia. Dialogues Clin Neurosci. 2005;7(1):53–67. PMID 16060596.
- ^ Ethics and early intervention in psychosis: keeping up the pace and staying in step.. Schizophr Res. 2001;51(1):17–29. doi:10.1016/S0920-9964(01)00235-3. PMID 11479062.
- ^ Haroun N, Dunn L, Haroun A, Cadenhead KS. Risk and protection in prodromal schizophrenia: ethical implications for clinical practice and future research. Schizophrenia Bulletin. 2006 [Retrieved 2008-07-06];32(1):166–78. doi:10.1093/schbul/sbj007. PMID 16207892. PMC 2632176.
- ^ Häfner H, Maurer K, Ruhrmann S, et al.. Early detection and secondary prevention of psychosis: facts and visions. European Archives of Psychiatry and Clinical Neuroscience. 2004 [Retrieved 2008-07-06];254(2):117–28. doi:10.1007/s00406-004-0508-z. PMID 15146341.
- ^ Boyle, Mary. Schizophrenia: a scientific delusion?. New York: Routledge; 2002. ISBN 0-415-22718-6.
- ^ Bentall, Richard P.; Read, John E; Mosher, Loren R.. Models of Madness: Psychological, Social and Biological Approaches to Schizophrenia. Philadelphia: Brunner-Routledge; 2004. ISBN 1-58391-906-6.
- ^ Schizophrenia term use 'invalid'. BBC News online (United Kingdom). 9 October 2006 [Retrieved 16 May 2007].
- ^ CASL Biography [Retrieved 2009-02-01].[dead link] and CASL History [Retrieved 2009-02-01].[dead link]
- ^ a b Tsuang MT. Toward reformulating the diagnosis of schizophrenia. American Journal of Psychiatry. 2000;157(7):1041–50. doi:10.1176/appi.ajp.157.7.1041. PMID 10873908.
- ^ Peralta V, Cuesta MJ. A dimensional and categorical architecture for the classification of psychotic disorders. World Psychiatry. 2007;6(2):100–1. PMID 18235866.
- ^ Verdoux H. Psychotic symptoms in non-clinical populations and the continuum of psychosis. Schizophrenia Research. 2002;54(1–2):59–65. doi:10.1016/S0920-9964(01)00352-8. PMID 11853979.
- ^ Johns LC. The continuity of psychotic experiences in the general population. Clinical Psychology Review. 2001;21(8):1125–41. doi:10.1016/S0272-7358(01)00103-9. PMID 11702510.
- ^ Peters ER. Measuring delusional ideation: the 21-item Peters et al. Delusions Inventory (PDI). Schizophrenia Bulletin. 2005;30(4):1005–22. PMID 15954204.
- ^ Edgar Jones. The Phenomenology of Abnormal Belief: A Philosophical and Psychiatric Inquiry. Philosophy, Psychiatry and Psychology. 1999 [Retrieved 2008-02-24];6(1):1–16.
- ^ David AS. On the impossibility of defining delusions. Philosophy, Psychiatry and Psychology. 1999 [Retrieved 2008-02-24];6(1):17–20.
- ^ S. Nassir Ghaemi. An Empirical Approach to Understanding Delusions. Philosophy, Psychiatry and Psychology. 1999 [Retrieved 2008-02-24];6(1):21–24.
- ^ Andreasen NC. Schizophrenia: the fundamental questions. Brain Res. Brain Res. Rev.. 2000;31(2–3):106–12. doi:10.1016/S0165-0173(99)00027-2. PMID 10719138.
- ^ Andreasen NC. A unitary model of schizophrenia: Bleuler's "fragmented phrene" as schizencephaly. Archives of General Psychiatry. 1999;56(9):781–7. doi:10.1001/archpsyc.56.9.781. PMID 12884883.
- ^ a b Jansson LB, Parnas J. Competing definitions of schizophrenia: what can be learned from polydiagnostic studies?. Schizophr Bull. 2007;33(5):1178–200. doi:10.1093/schbul/sbl065. PMID 17158508.
- ^ Green MF, Nuechterlein KH. Should schizophrenia be treated as a neurocognitive disorder?. Schizophr Bull. 1999;25(2):309–19. PMID 10416733.
- ^ Green, Michael. Schizophrenia revealed: from neurons to social interactions. New York: W.W. Norton; 2001. ISBN 0-393-70334-7.
- ^ Lake CR, Hurwitz N. Schizoaffective disorder merges schizophrenia and bipolar disorders as one disease—there is no schizoaffective disorder. Curr Opin Psychiatry. 2007;20(4):365–79. doi:10.1097/YCO.0b013e3281a305ab. PMID 17551352.
- ^ Malhi GS, Green M, Fagiolini A, Peselow ED, Kumari V. Schizoaffective disorder: diagnostic issues and future recommendations. Bipolar Disorders. 2008;10(1 Pt 2):215–30. doi:10.1111/j.1399-5618.2007.00564.x. PMID 18199238.
- ^ Craddock N, Owen MJ. The beginning of the end for the Kraepelinian dichotomy. Br J Psychiatry. 2005;186:364–6. doi:10.1192/bjp.186.5.364. PMID 15863738.
- ^ Cooper, David A.. The Dialectics of Liberation (Pelican). London, England: Penguin Books Ltd; 1969. ISBN 0-14-021029-6.
- ^ Szasz, Thomas Stephen. The myth of mental illness: foundations of a theory of personal conduct. San Francisco: Harper & Row; 1974. ISBN 0-06-091151-4.
Further reading
- Bentall, Richard. Madness explained: psychosis and human nature. London: Allen Lane; 2003. ISBN 0-7139-9249-2.
- Dalby, J. Thomas. Mental disease in history: a selection of translated readings. Bern: Peter Lang; 1996. ISBN 0-8204-3056-0.
- Fallon, James H.. The Neuroanatomy of Schizophrenia: Circuitry and Neurotransmitter Systems. Clinical Neuroscience Research. 2003 [Retrieved 2008-07-07];3:77–107. doi:10.1016/S1566-2772(03)00022-7.
- Fleck, Stephen; Theodore Lidz; and Alice Cornelison. Schizophrenia and the family. New York: International Universities Press; 1985. ISBN 0-8236-6001-X.
- Keen TM. Schizophrenia: orthodoxy and heresies. A review of alternative possibilities. Journal of Psychiatric and Mental Health Nursing. 1999;6(6):415–24. doi:10.1046/j.1365-2850.1999.00237.x. PMID 10818864.
- Laing, Ronald D.. The divided self: an existential study in sanity and madness. New York: Penguin Books; 1990. ISBN 0-14-013537-5.
- Lenzenweger, M.F. (2010). Schizotypy and schizophrenia: The view from experimental psychopathology. New York: Guilford Press. ISBN 978-1-60623-865-3
- Noll, Richard. The Encyclopedia of Schizophrenia And Other Psychotic Disorders (Facts on File Library of Health and Living). New York: Facts on File; 2006. ISBN 0-8160-6405-9.
- Roazen, Paul nd Victor Tausk. Sexuality, war, and schizophrenia: collected psychoanalytic papers. New Brunswick, N.J., U.S.A: Transaction Publishers; 1991. ISBN 0-88738-365-3. (On the Origin of the 'Influencing Machine' in Schizophrenia.)
- Shaner A, Miller G, Mintz J. Schizophrenia as one extreme of a sexually selected fitness indicator [PDF]. Schizophr. Res.. 2004 [Retrieved 2008-07-07];70(1):101–9. doi:10.1016/j.schres.2003.09.014. PMID 15246469.
- Schizophrenia: the sacred symbol of psychiatry. New York: Basic Books; 1976. ISBN 0-465-07222-4.
- Walker Elaine, et al. Schizophrenia: Etiology and Course. Annual Review of Psychology. 2004;55:401–30. doi:10.1146/annurev.psych.55.090902.141950. PMID 14744221.
External links
- Schizophrenia at Curlie
- NPR: the sight and sounds of schizophrenia
- The current World Health Organisation definition of Schizophrenia
- Symptoms in Schizophrenia Film made in 1940 showing some of the symptoms of Schizophrenia.
Template:Link GA Template:Link GA Template:Link GA Template:Link GA Template:Link GA Template:Link FA Template:Link FA
