Torasemide
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Demadex, Tortas, Wator, others |
| Other names | Torsemide |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a601212 |
| License data | |
| Routes of administration | By mouth, IV |
| Drug class | Loop diuretic |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 80-90% |
| Protein binding | Highly bound (>99%). |
| Metabolism | Hepatic (80%) |
| Elimination half-life | 3.5 hours; Cirrhosis: 7-8 hours |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.164.924 |
| Chemical and physical data | |
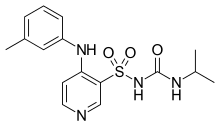
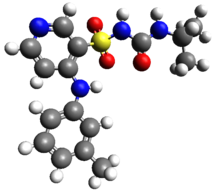
| Formula | C16H20N4O3S |
| Molar mass | 348.42 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| | |
Torasemide, also known as torsemide, is a diuretic medication used to treat fluid overload due to heart failure, kidney disease, and liver disease and high blood pressure.[1] It is a less preferred treatment for high blood pressure.[1] It is taken by mouth or by injection into a vein.[1]
Common side effects include headache, increased urination, diarrhea, cough, and dizziness.[1] Other side effects may include hearing loss and low blood potassium.[1] Torasemide is a sulfonamide and loop diuretic.[1] Use is not recommended in pregnancy or breastfeeding.[2] It works by decreasing the reabsorption of sodium by the kidneys.[1]
Torasemide was patented in 1974 and came into medical use in 1993.[3] It is available as a generic medication.[2] In 2017, it was the 264th most commonly prescribed medication in the United States, with more than one million prescriptions.[4][5]
Medical uses
It is used to treat fluid overload due to heart failure and high blood pressure.[1] Compared with furosemide, torasemide is associated with a lower risk of rehospitalization for heart failure and an improvement in New York Heart Association class of heart failure.[6][7][8] In heart failure it may be safer and more effective than furosemide.[9][10][11]
Adverse effects
No evidence of torasemide-induced ototoxicity has been demonstrated in humans.[12] Loop diuretics, including torsemide, may decrease total body thiamine, particularly in people with poor thiamine intake, and this depletion may worsen heart failure. It is therefore reasonable to either also give thiamine supplements or to check blood thiamine levels in those being treated with chronic loop diuretics.[13]
Chemistry
Compared with other loop diuretics, torasemide has a more prolonged diuretic effect than equipotent doses of furosemide and relatively decreased potassium loss.
Names
Torasemide is the recommended name of the drug (rINN) according to the (INN), which is the drug naming system coordinated by the World Health Organization. Torsemide is the official name of the drug according to the (USAN), which is the drug naming system coordinated by the USAN Council, which is co-sponsored by the American Medical Association (AMA), the United States Pharmacopeial Convention (USP), and the American Pharmacists Association (APhA).
References
- ^ a b c d e f g h "Torsemide Monograph for Professionals". Drugs.com. American Society of Health-System Pharmacists. Retrieved 18 March 2019.
- ^ a b British national formulary : BNF 76 (76 ed.). Pharmaceutical Press. 2018. pp. 227–228. ISBN 9780857113382.
- ^ Fischer, Jnos; Ganellin, C. Robin (2006). Analogue-based Drug Discovery. John Wiley & Sons. p. 458. ISBN 9783527607495.
- ^ "The Top 300 of 2020". ClinCalc. Retrieved 11 April 2020.
- ^ "Torsemide - Drug Usage Statistics". ClinCalc. Retrieved 11 April 2020.
- ^ Abraham B, Megaly M, Sous M, Fransawyalkomos M, Saad M, Fraser R, Topf J, Goldsmith S, Simegn M, Bart B, Azzo Z, Mesiha N, Sharma R (January 2020). "Meta-Analysis Comparing Torsemide Versus Furosemide in Patients With Heart Failure". Am. J. Cardiol. 125 (1): 92–99. doi:10.1016/j.amjcard.2019.09.039. PMID 31699358.
- ^ Täger T, Fröhlich H, Seiz M, Katus HA, Frankenstein L (March 2019). "READY: relative efficacy of loop diuretics in patients with chronic systolic heart failure-a systematic review and network meta-analysis of randomised trials". Heart Fail Rev. doi:10.1007/s10741-019-09771-8. PMID 30874955.
- ^ Miles JA, Hanumanthu BK, Patel K, Chen M, Siegel RM, Kokkinidis DG (June 2019). "Torsemide versus furosemide and intermediate-term outcomes in patients with heart failure: an updated meta-analysis". J Cardiovasc Med (Hagerstown). 20 (6): 379–388. doi:10.2459/JCM.0000000000000794. PMID 30950982.
- ^ Wargo KA, Banta WM (November 2009). "A comprehensive review of the loop diuretics: should furosemide be first line?". Ann Pharmacother. 43 (11): 1836–47. doi:10.1345/aph.1M177. PMID 19843838.
- ^ Roush GC, Kaur R, Ernst ME (2014). "Diuretics: a review and update". J. Cardiovasc. Pharmacol. Ther. 19 (1): 5–13. doi:10.1177/1074248413497257. PMID 24243991.
- ^ Buggey J, Mentz RJ, Pitt B, Eisenstein EL, Anstrom KJ, Velazquez EJ, O'Connor CM (2015). "A reappraisal of loop diuretic choice in heart failure patients". Am. Heart J. 169 (3): 323–33. doi:10.1016/j.ahj.2014.12.009. PMC 4346710. PMID 25728721.
- ^ Dunn CJ, Fitton A, Brogden RN (January 1995). "Torasemide. An update of its pharmacological properties and therapeutic efficacy". Drugs. 49 (1): 121–42. doi:10.2165/00003495-199549010-00009. PMID 7705212.
- ^ Kattoor AJ, Goel A, Mehta JL (August 2018). "Thiamine Therapy for Heart Failure: a Promise or Fiction?". Cardiovasc Drugs Ther. 32 (4): 313–317. doi:10.1007/s10557-018-6808-8. PMID 30022355.
External links
- "Torasemide". Drug Information Portal. U.S. National Library of Medicine.
