Eosinophil cationic protein
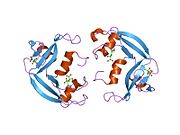
Eosinophil Cationic Protein (ECP) also known as ribonuclease 3 is a basic protein located in the eosinophil primary matrix.[1] In humans, the eosinophil cationic protein is encoded by the RNASE3 gene.[2]
ECP is released during degranulation of eosinophils. This protein is related to inflammation and asthma because in these cases, there are increased levels of ECP in the body. There are three glycosolated forms of ECP and consequently ECP has a range of molecular weights from 18-22 kDa.[3]
Function
Eosinophil cationic protein and the sequence related eosinophil-derived neurotoxin are both members of the ribonuclease a superfamily. Both proteins possess neurotoxic, helmintho-toxic, and ribonucleo-lytic activities. Eosinophil cationic protein is localized to the granule matrix of the eosinophil.[4]
Ribonuclease activity and cytotoxicity
The ribonuclease activity of ECP is not essential for cytotoxicity.[5]
When the two known ribonuclease active-site residues are modified to non-functional counterparts (Lysine at position 38 to Arginine and Histidine at position 128 to Aspartate)[6] and compared to the wild-type ECP, the mutated ECP retains its cytotoxicity but no longer has its ribonuclease activity. The experiment confirmed that converting the two amino acids to non-functional counter parts did inhibit ECP’s ribonuclease activity. However, ECP retained its anti-parasitic activity. Also, it did not change the production and transportation of ECP in bacteria.
ECP is a potent cytotoxic protein capable of killing cells of guinea pig tracheal epithelium,[7] mammalian leukemia,[8] epidermis carcinoma,[7] and breast carcinoma,[9] as well as non-mammalian cells such as parasites, bacteria, and viruses.[10]
Mature ECP is cytotoxic to human bronchial epithelial (BEAS-2B) cells by specific binding to cell surface heparan sulfate proteoglycans (HSPGs) followed by endocytosis.[11]
ECP-induced apoptosis

Studies show that ECP, along with other RNases including EDN, had been reported to induce apoptosis in cells. A latest study indicated that ECP caused cytotoxicity in HL-60 and HeLa cells via caspase-3 like activity.[13] Accordingly, cytotoxic RNases play an important role in cell death. However, the mechanism of ECP-induced apoptosis is still not fully verified. Recent studies have shown that eosinophils can induce epithelial cell death via apoptosis and necrosis.[14]
ECP triggers apoptosis by caspase-8 activation through mitochondria-independent pathway.[12] Increases in chromatin condensation, sub-G1 population, PARP cleavage, and DNA fragmentation indicate that ECP induces apoptosis in human bronchial epithelial (BEAS-2B) cells.[12]
Clinical significance
Eosinophil granulocytes appear in large numbers in inflammation sites and in response to certain parasitic infections. These cytoplasmic granulocytes contain positively charged proteins that characterize the cells. ECP is one of the four highly basic proteins that enter the surrounding tissues when activated eosinophils degranulate. Although circulating ECP levels can vary widely among patients, some studies show that serum ECP measurements are useful in monitoring many active inflammatory diseases.[15] ECP concentrations in plasma and other body fluids increase during inflammatory reactions marked by activated eosinophils.[16]
Serum ECP levels are also a useful, objective measurement for asthma severity. Increased ECP levels correspond to symptom onset. In seasonal asthmatic patients, ECP measurement reflected changes in disease activity throughout the year.[17]
There are several mechanisms that can be combined to generate an asthma attack, including specific IgE antibodies, activated inflammatory cells, neurogenic mechanisms, hyperresponsiveness and individual hormonal imbalances. Allergic reactions in the lung typically have two phases. The late phase typically occurs several hours after exposure, upon which eosinophils accumulate in the bronchus and release granule proteins that cause bronchial irritability. ECP is also toxic to neurons, some epithelial cell lines, and isolated myocardial cells.[18] This could be a reason for itching disorders of the skin.
Serum ECP concentrations have also been linked to atopic dermatitis (AD) activity. ECP correlates with the symptoms (lichenification, sleep deprivation, erythema, papules, pruritus and excoriations) for AD and also correlates with the total clinical score.[18]
Serum ECP measurement for assessing asthma severity, monitoring therapy, and indicating severity of certain inflammatory skin conditions present an advantage over subjective clinical measures that are prone to inconsistencies due to broad variability of individual investigator and patient assessments, especially in young children.
The normal reference range for blood tests for eosinophil cationic protein is between 2.3 and 16 µg/L.[19]
See also
References
- ^ Boix E, Carreras E, Nikolovski Z, Cuchillo CM, Nogués MV (June 2001). "Identification and characterization of human eosinophil cationic protein by an epitope-specific antibody". J. Leukoc. Biol. 69 (6): 1027–35. PMID 11404391.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Mastrianni DM, Eddy RL, Rosenberg HF, Corrette SE, Shows TB, Tenen DG, Ackerman SJ (May 1992). "Localization of the human eosinophil Charcot-Leyden crystal protein (lysophospholipase) gene (CLC) to chromosome 19 and the human ribonuclease 2 (eosinophil-derived neurotoxin) and ribonuclease 3 (eosinophil cationic protein) genes (RNS2 and RNS3) to chromosome 14". Genomics. 13 (1): 240–2. doi:10.1016/0888-7543(92)90237-M. PMID 1577491.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Lee BioSolutions, Inc. http://www.leebio.com/eosinophil-cationic-protein-human-P359.html
- ^ Hamann KJ, Ten RM, Loegering DA, Jenkins RB, Heise MT, Schad CR, Pease LR, Gleich GJ, Barker RL (August 1990). "Structure and chromosome localization of the human eosinophil-derived neurotoxin and eosinophil cationic protein genes: evidence for intronless coding sequences in the ribonuclease gene superfamily". Genomics. 7 (4): 535–46. doi:10.1016/0888-7543(90)90197-3. PMID 2387583.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Rosenberg HF (April 1995). "Recombinant human eosinophil cationic protein. Ribonuclease activity is not essential for cytotoxicity". J. Biol. Chem. 270 (14): 7876–81. doi:10.1074/jbc.270.14.7876. PMID 7713881.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Lehrer RI, Szklarek D, Barton A, Ganz T, Hamann KJ, Gleich GJ (June 1989). "Antibacterial properties of eosinophil major basic protein and eosinophil cationic protein". Journal of Immunology. 142 (12): 4428–34. PMID 2656865.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Motojima S, Frigas E, Loegering DA, Gleich GJ (March 1989). "Toxicity of eosinophil cationic proteins for guinea pig tracheal epithelium in vitro". Am. Rev. Respir. Dis. 139 (3): 801–5. doi:10.1164/ajrccm/139.3.801. PMID 2923379.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Carreras E, Boix E, Navarro S, Rosenberg HF, Cuchillo CM, Nogués MV (April 2005). "Surface-exposed amino acids of eosinophil cationic protein play a critical role in the inhibition of mammalian cell proliferation". Mol. Cell. Biochem. 272 (1–2): 1–7. doi:10.1007/s11010-005-4777-2. PMID 16010966.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Ali S, Kaur J, Patel KD (July 2000). "Intercellular Cell Adhesion Molecule-1, Vascular Cell Adhesion Molecule-1, and Regulated on Activation Normal T Cell Expressed and Secreted Are Expressed by Human Breast Carcinoma Cells and Support Eosinophil Adhesion and Activation". Am. J. Pathol. 157 (1): 313–21. doi:10.1016/S0002-9440(10)64542-7. PMC 1850201. PMID 10880401.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Venge P (January 2004). "Monitoring the allergic inflammation". Allergy. 59 (1): 26–32. doi:10.1046/j.1398-9995.2003.00386.x. PMID 14674929.
- ^ Fan TC, Chang HT, Chen IW, Wang HY, Chang MD (December 2007). "A heparan sulfate-facilitated and raft-dependent macropinocytosis of eosinophil cationic protein". Traffic. 8 (12): 1778–95. doi:10.1111/j.1600-0854.2007.00650.x. PMID 17944807.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b c Chang KC, Lo CW, Fan TC, Chang MD, Shu CW, Chang CH, Chung CT, Fang SL, Chao CC, Tsai JJ, Lai YK (2010). "TNF-α Mediates Eosinophil Cationic Protein-induced Apoptosis in BEAS-2B Cells". BMC Cell Biol. 11: 6. doi:10.1186/1471-2121-11-6. PMC 2819994. PMID 20089176.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - ^ Navarro S, Aleu J, Jiménez M, Boix E, Cuchillo CM, Nogués MV (January 2008). "The cytotoxicity of eosinophil cationic protein/ribonuclease 3 on eukaryotic cell lines takes place through its aggregation on the cell membrane". Cell. Mol. Life Sci. 65 (2): 324–37. doi:10.1007/s00018-007-7499-7. PMID 18087674.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Trautmann A, Schmid-Grendelmeier P, Krüger K, Crameri R, Akdis M, Akkaya A, Bröcker EB, Blaser K, Akdis CA (February 2002). "T cells and eosinophils cooperate in the induction of bronchial epithelial cell apoptosis in asthma". The Journal of Allergy and Clinical Immunology. 109 (2): 329–37. doi:10.1067/mai.2002.121460. PMID 11842305.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Wardlaw AJ (August 1994). "Eosinophils in the 1990s: new perspectives on their role in health and disease". Postgrad Med J. 70 (826): 536–52. doi:10.1136/pgmj.70.826.536. PMC 2397687. PMID 7937446.
- ^ D'Amato G, Liccardi G, Russo M, Saggese M, D'Amato M (April 1996). "Measurement of serum levels of eosinophil cationic protein to monitor patients with seasonal respiratory allergy induced by Parietaria pollen (treated and untreated with specific immunotherapy)". Allergy. 51 (4): 245–50. doi:10.1111/j.1398-9995.1996.tb00075.x. PMID 8792921.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Tomassini M, Magrini L, De Petrillo G, Adriani E, Bonini S, Balsano F, Bonini S (June 1996). "Serum levels of eosinophil cationic protein in allergic diseases and natural allergen exposure". The Journal of Allergy and Clinical Immunology. 97 (6): 1350–5. doi:10.1016/S0091-6749(96)70204-X. PMID 8648032.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Czech W, Krutmann J, Schöpf E, Kapp A (April 1992). "Serum eosinophil cationic protein (ECP) is a sensitive measure for disease activity in atopic dermatitis". Br. J. Dermatol. 126 (4): 351–5. doi:10.1111/j.1365-2133.1992.tb00677.x. PMID 1571256.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Reference range list from Uppsala University Hospital ("Laborationslista"). Artnr 40284 Sj74a. Issued on April 22, 2008
Further reading
- Plager DA, Davis MD, Andrews AG; et al. (2009). "Eosinophil Ribonucleases and Their Cutaneous Lesion-Forming Activity". Journal of Immunology. 183 (6): 4013–20. doi:10.4049/jimmunol.0900055. PMC 2852253. PMID 19717523.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Nielsen LP, Peterson CG, Dahl R (2009). "Serum eosinophil granule proteins predict asthma risk in allergic rhinitis". Allergy. 64 (5): 733–7. doi:10.1111/j.1398-9995.2008.01869.x. PMID 19133919.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Behnecke A, Mayr S, Schick B; et al. (2008). "Evaluation of ECP release from intact tissue biopsies from patients with nasal polyps". Inflamm. Res. 57 Suppl 1: S65–6. doi:10.1007/s00011-007-0632-0. PMID 18345486.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Eberlein B, Gulyas A, Schultz K; et al. (2009). "Benefits of alpine mountain climate of Bavaria in patients with allergic diseases and chronic obstructive pulmonary disease: results from the AURA* study". J Investig Allergol Clin Immunol. 19 (2): 159–61. PMID 19476022.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Torrent M, Navarro S, Moussaoui M; et al. (2008). "Eosinophil cationic protein high-affinity binding to bacteria-wall lipopolysaccharides and peptidoglycans". Biochemistry. 47 (11): 3544–55. doi:10.1021/bi702065b. PMID 18293932.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Parwez Q, Stemmler S, Epplen JT, Hoffjan S (2008). "Variation in genes encoding eosinophil granule proteins in atopic dermatitis patients from Germany". J Negat Results Biomed. 7: 9. doi:10.1186/1477-5751-7-9. PMC 2596079. PMID 19014520.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - Zagai U, Lundahl J, Klominek J; et al. (2009). "Eosinophil cationic protein stimulates migration of human lung fibroblasts in vitro". Scand. Journal of Immunology. 69 (4): 381–6. doi:10.1111/j.1365-3083.2009.02233.x. PMID 19284504.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Torrent M, de la Torre BG, Nogués VM; et al. (2009). "Bactericidal and membrane disruption activities of the eosinophil cationic protein are largely retained in an N-terminal fragment". Biochem. J. 421 (3): 425–34. doi:10.1042/BJ20082330. PMID 19450231.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Fukuda T, Iwata M, Kitazoe M; et al. (2009). "Human eosinophil cationic protein enhances stress fiber formation in Balb/c 3T3 fibroblasts and differentiation of rat neonatal cardiomyocytes". Growth Factors. 27 (4): 228–36. doi:10.1080/08977190902987149. PMID 19521893.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Torrent M, Sánchez D, Buzán V; et al. (2009). "Comparison of the membrane interaction mechanism of two antimicrobial RNases: RNase 3/ECP and RNase 7". Biochim. Biophys. Acta. 1788 (5): 1116–25. doi:10.1016/j.bbamem.2009.01.013. PMID 19366593.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Domínguez-Ortega J, Pérez-Bedmar J, Rodríguez-Jiménez B; et al. (2009). "Eosinophilic esophagitis due to profilin allergy". J Investig Allergol Clin Immunol. 19 (4): 338–9. PMID 19639743.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Fan TC, Fang SL, Hwang CS; et al. (2008). "Characterization of molecular interactions between eosinophil cationic protein and heparin". J. Biol. Chem. 283 (37): 25468–74. doi:10.1074/jbc.M803516200. PMID 18593710.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - Kang I, An XH, Oh YK; et al. (2010). "Identification of polymorphisms in the RNase3 gene and the association with allergic rhinitis". Eur Arch Otorhinolaryngol. 267 (3): 391–5. doi:10.1007/s00405-009-1103-8. PMID 19760211.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Yuksel H, Yilmaz O, Sogut A; et al. (2009). "Correlation of quality of life with clinical parameters and eosinophilic cation protein levels in children with allergic rhinoconjunctivitis". Int. Arch. Allergy Immunol. 148 (1): 18–22. doi:10.1159/000151501. PMID 18716399.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Rubin J, Zagai U, Blom K; et al. (2009). "The coding ECP 434(G>C) gene polymorphism determines the cytotoxicity of ECP but has minor effects on fibroblast-mediated gel contraction and no effect on RNase activity". Journal of Immunology. 183 (1): 445–51. doi:10.4049/jimmunol.0803912. PMID 19542456.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Laurents DV, Bruix M, Jiménez MA; et al. (2009). "The (1)H, (13)C, (15)N resonance assignment, solution structure, and residue level stability of eosinophil cationic protein/RNase 3 determined by NMR spectroscopy". Biopolymers. 91 (12): 1018–28. doi:10.1002/bip.21152. PMID 19189375.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Peona V, De Amici M, Quaglini S; et al. (2010). "Serum eosinophilic cationic protein: is there a role in respiratory disorders?". J Asthma. 47 (2): 131–4. doi:10.3109/02770900903497170. PMID 20170318.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Shin SY, Choi SJ, Hur GY; et al. (2009). "Local production of total IgE and specific antibodies to the house dust mite in adenoid tissue". Pediatr Allergy Immunol. 20 (2): 134–41. doi:10.1111/j.1399-3038.2008.00756.x. PMID 18657051.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Woschnagg C, Rubin J, Venge P (2009). "Eosinophil cationic protein (ECP) is processed during secretion". Journal of Immunology. 183 (6): 3949–54. doi:10.4049/jimmunol.0900509. PMID 19692640.
{{cite journal}}: CS1 maint: multiple names: authors list (link)
External links
- Eosinophil+Cationic+Protein at the U.S. National Library of Medicine Medical Subject Headings (MeSH)
- RNASE3+protein,+human at the U.S. National Library of Medicine Medical Subject Headings (MeSH)