Proton therapy
Proton therapy or proton beam therapy is a medical procedure, a type of particle therapy that uses a beam of protons to irradiate diseased tissue, most often in the treatment of cancer. Proton therapy's chief advantage over other types of external beam radiotherapy is that as a charged particle the dose is deposited over a narrow range and there is minimal exit dose.
Description

Proton therapy is a type of external beam radiotherapy that uses ionizing radiation. In proton therapy, medical personnel use a particle accelerator to target a tumor with a beam of protons.[2][3] These charged particles damage the DNA of cells, ultimately killing them or stopping their reproduction. Cancerous cells are particularly vulnerable to attacks on DNA because of their high rate of division and their reduced abilities to repair DNA damage.
Due to their relatively large mass, protons have little lateral side scatter in the tissue; the beam does not broaden much, stays focused on the tumor shape and delivers only low-dose side-effects to surrounding tissue. All protons of a given energy have a certain range; very few protons penetrate beyond that distance.[4] Furthermore, the dose delivered to tissue is maximum just over the last few millimeters of the particle’s range; this maximum is called the Bragg peak often referred to as the SOBP.[5]
To treat tumors at greater depths, the proton accelerator must produce a beam with higher energy, typically given in eV or electron volts. Proton therapy treats tumors closer to the surface of the body with lower energy protons. Accelerators used for proton therapy typically produce protons with energies in the range of 70 to 250 MeV (mega electron volts; million electron volts). Adjusting proton energy during the treatment maximizes the cell damage the proton beam causes within the tumor. Tissue closer to the surface of the body than the tumor receives reduced radiation, and therefore reduced damage. Tissues deeper in the body receive very few protons, so the dosage becomes immeasurably small.[4]
In most treatments, protons of different energies with Bragg peaks at different depths are applied to treat the entire tumor. These Bragg peaks are shown as thin blue lines in the figure to the right. The total radiation dosage of the protons is called the spread-out Bragg peak (SOBP), shown as a heavy dashed blue line in figure to the right. It is important to understand that, while tissues behind or deeper than the tumor receive no radiation from proton therapy, the tissues in front of or shallower than the tumor receive radiation dosage based on the SOBP.
History
The first suggestion that energetic protons could be an effective treatment method was made by Robert R. Wilson[6] in a paper published in 1946 while he was involved in the design of the Harvard Cyclotron Laboratory (HCL).[7] The first treatments were performed with particle accelerators built for physics research, notably Berkeley Radiation Laboratory in 1954 and at Uppsala in Sweden in 1957. In 1961, a collaboration began between HCL and the Massachusetts General Hospital (MGH) to pursue proton therapy. Over the next 41 years, this program refined and expanded these techniques while treating 9,116 patients[8] before the cyclotron was shut down in 2002. The world's first hospital-based proton therapy center was a low energy cyclotron centre for ocular tumours at the Clatterbridge Centre for Oncology in the UK, opened in 1989,[9] followed in 1990 at the Loma Linda University Medical Center (LLUMC) in Loma Linda, California. Later, The Northeast Proton Therapy Center at Massachusetts General Hospital was brought online, and the HCL treatment program was transferred to it during 2001 and 2002. By 2010 these facilities were joined by an additional seven regional hospital-based proton therapy centers in the United States alone, and many more worldwide.[10]
Application
Physicians use protons to treat conditions in two broad categories:
- Disease sites that respond well to higher doses of radiation, i.e., dose escalation. In some instances, dose escalation has demonstrated a higher probability of "cure" (i.e., local control) than conventional radiotherapy.[11] These include, among others, uveal melanoma (ocular tumors), skull base and paraspinal tumors (chondrosarcoma and chordoma), and unresectable sarcomas. In all these cases proton therapy achieves significant improvements in the probability of local control over conventional radiotherapy.[12][13][14] In treatment of ocular tumors, proton therapy also has high rates of maintaining the natural eye.[15]
The second broad class are those treatments where proton therapy's increased precision reduces unwanted side effects by lessening the dose to normal tissue. In these cases, the tumor dose is the same as in conventional therapy, so there is no expectation of an increased probability of curing the disease. Instead, the emphasis is on reducing the integral dose to normal tissue, thus reducing unwanted effects.[11]
Two prominent examples are pediatric neoplasms (such as medulloblastoma) and prostate cancer. In the case of pediatric treatments, a 2004 review gave theoretical advantages but did not report any clinical benefits.[16][17]
In prostate cancer cases, the issue is less clear. Some published studies found a reduction in long term rectal and genito-urinary damage when treating with protons rather than photons (meaning X-ray or gamma ray therapy). Others showed a small difference, limited to cases where the prostate is particularly close to certain anatomical structures.[18][19] The relatively small improvement found may be the result of inconsistent patient set-up and internal organ movement during treatment, which offsets most of the advantage of increased precision.[19][20][20][21] One source suggests that dose errors around 20% can result from motion errors of just 2.5 mm,[citation needed] and another that prostate motion is between 5–10 mm.[22]
However, the number of cases of prostate cancer diagnosed each year far exceeds those of the other diseases referred to above, and this has led some, but not all, facilities to devote a majority of their treatment slots to prostate treatments. For example, two hospital facilities devote roughly 65%[23] and 50%[24] of their proton treatment capacity to prostate cancer, while a third devotes only 7.1%.[25]
Overall worldwide numbers are hard to compile, but one example in the literature shows that in 2003 roughly 26% of proton therapy treatments worldwide were for prostate cancer.[26] Proton therapy for ocular (eye) tumors is a special case since this treatment requires only comparatively low energy protons (about 70 MeV). Owing to this low energy requirement, some particle therapy centers only treat ocular tumors.[8] Proton, or more generally, hadron therapy of tissue close to the eye affords sophisticated methods to assess the alignment of the eye that can vary significantly from other patient position verification approaches in image guided particle therapy.[27] Position verification and correction must ensure that the radiation spares sensitive tissue like the optic nerve to preserve the patient’s vision.
Comparison with other treatments
The issue of when, whether, and how best to apply this technology is controversial.[28][29][30] As of 2012 there have been no controlled trials to demonstrate that proton therapy yields improved survival or other clinical outcomes (including impotence in prostate cancer) compared to other types of radiation therapy, although a five-year study of prostate cancer is underway at Massachusetts General Hospital.[31][32][33][34][34] Proton therapy is far more expensive than conventional therapy.[29][35] As of 2012[update] proton therapy required a very large capital investment (from US$100M to more than $180M).[28][30][36]
Preliminary results from a 2009 study, including high-dose treatments, showed very few side effects.[37]
NHS Choices has stated:
We cannot say with any conviction that proton beam therapy is “better” overall than radiotherapy. (...) Some overseas clinics providing proton beam therapy heavily market their services to parents who are understandably desperate to get treatment for their children. Proton beam therapy can be very costly and it is not clear whether all children treated privately abroad are treated appropriately.[38][39]
X-ray radiotherapy

The figure at the right of the page shows how beams of X-rays (IMRT; left frame) and beams of protons (right frame), of different energies, penetrate human tissue. A tumor with a sizable thickness is covered by the IMRT spread out Bragg peak (SOBP) shown as the red lined distribution in the figure. The SOBP is an overlap of several pristine Bragg peaks (blue lines) at staggered depths.
Megavoltage X-ray therapy has less "skin scarring potential" than proton therapy: X-ray radiation at the skin, and at very small depths, is lower than for proton therapy. One study estimates that passively scattered proton fields have a slightly higher entrance dose at the skin (~75%) compared to therapeutic megavoltage (MeV) photon beams (~60%).[1] X-ray radiation dose falls off gradually, unnecessarily damaging tissue deeper in the body and damaging the skin and surface tissue opposite the beam entrance. The differences between the two methods depends on the:
- Width of the SOBP
- Depth of the tumor
- Number of beams that treat the tumor
The X-ray advantage of reduced damage to skin at the entrance is partially counteracted by damage to skin at the exit point.
Since X-ray treatments are usually done with multiple exposures from opposite sides, each section of skin is exposed to both entering and exiting X-rays. In proton therapy, skin exposure at the entrance point is higher, but tissues on the opposite side of the body to the tumor receive no radiation. Thus, X-ray therapy causes slightly less damage to the skin and surface tissues, and proton therapy causes less damage to deeper tissues in front of and beyond the target.[3]
An important consideration in comparing these treatments is whether the equipment delivers protons via the scattering method (historically, the most common) or a spot scanning method. Spot scanning can adjust the width of the SOBP on a spot-by-spot basis, which reduces the volume of normal (healthy) tissue inside the high dose region. Also, spot scanning allows for intensity modulated proton therapy (IMPT), which determines individual spot intensities using an optimization algorithm that lets the user balance the competing goals of irradiating tumors while sparing normal tissue. Spot scanning availability depends on the machine and the institution. Spot scanning is more commonly known as pencil-beam scanning and is available on IBA, Hitachi, Mevion (known as hyperscan [40] and Not USFDA approved as of 2015) and Varian.
Surgery
Physicians base the decision to use surgery or proton therapy (or any radiation therapy) on the tumor type, stage, and location. In some instances, surgery is superior (e.g. cutaneous melanoma), in some instances radiation is superior (e.g., skull base chondrosarcoma), and in some instances they are comparable (e.g., prostate cancer). In some instances, they are used together (e.g., rectal cancer or early stage breast cancer). The benefit of external beam proton radiation lies in the dosimetric difference from external beam X-ray radiation and brachytherapy in cases where the use of radiation therapy is already indicated, rather than as a direct competition with surgery.[11] However, in the case of prostate cancer, the most common indication for proton beam therapy, no clinical study directly comparing proton therapy to surgery, brachytherapy, or other treatments has shown any clinical benefit for proton beam therapy. Indeed, the largest study to date showed that IMRT compared with proton therapy was associated with less gastrointestinal morbidity.[41]
Side effects and risks
Proton therapy is a type of external beam radiotherapy, and shares risks and side effects of other forms of radiation therapy. However the dose outside of the treatment region can be significantly less for deep-tissue tumors than X-ray therapy, because proton therapy takes full advantage of the Bragg peak. Proton therapy has been in use for over 40 years, and is a mature treatment technology. However, as with all medical knowledge, understanding of the interaction of radiation (proton, X-ray, etc.) with tumor and normal tissue is still imperfect.[28]
Costs
Historically, proton therapy has been expensive. Goitein & Jermann's[42] analysis had previously determined the relative cost of proton therapy is approximately 2.4 times that of X-ray therapies. However, newer, more compact proton beam sources can be four to five times cheaper and offer more accurate three-dimensional targeting.[43][44] Thus the cost is expected to reduce as better proton technology becomes more widely available. A similar analysis by Lievens & Van den Bogaert[45] determined that the cost of proton therapy is not unrealistic and should not be the reason for denying patients access to this technology. In some clinical situations, proton beam therapy is clearly superior to the alternatives.[46][47] Another study in 2007 expressed concerns about the effectiveness of proton therapy for treating prostate cancer.[48] Although, with the advent of new developments in proton beam technology, such as improved scanning techniques and more precise dose delivery ('pencil beam scanning'), this situation may change considerably.[49] Amitabh Chandra, a health economist at Harvard University, has been quoted as saying that "Proton-beam therapy is like the death star of American medical technology... It's a metaphor for all the problems we have in American medicine.”[50] However, another study has shown that proton therapy in fact brings cost savings.[51] The advent of second generation, and much less expensive, proton therapy equipment now being installed at various sites may change this picture significantly.[52]
Treatment centers

As of January 2016, there are 58 particle therapy facilities worldwide. This represents a total of more than 121 treatment rooms available to patients.[53] More than 96,537 patients had been treated.[54]
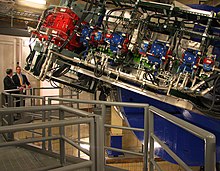
One hindrance to universal use of the proton in cancer treatment is the size and cost of the cyclotron or synchrotron equipment necessary. Several industrial teams are working on development of comparatively small accelerator systems to deliver the proton therapy to patients.[55] Among the technologies being investigated are superconducting synchrocyclotrons (also known as FM Cyclotrons), ultra-compact synchrotrons, dielectric wall accelerators,[55] and linear particle accelerators.[44]
United States
Proton treatment centers in the United States as of 2014[update] (in chronological order of first treatment date) include:[9][56]
| Institution | Location | Year of first treatment | Comments |
|---|---|---|---|
| University of California, Davis, Crocker Nuclear Laboratory[57] | Davis, CA | 1994 | Ocular treatments only (low energy accelerator) |
| Loma Linda University Medical Center[58] | Loma Linda, CA | 1990 | First hospital-based facility in USA It uses the Spread Out Bragg's Peak (SOBP) shown in the above illustration. |
| Francis H. Burr Proton Center (formerly NPTC) at Massachusetts General Hospital (MGH) | Boston, MA | 2001 | Continuation of Harvard Cyclotron Laboratory/MGH treatment program that began in 1961 |
| SCCA Proton Therapy Center at Seattle Cancer Care Alliance | Seattle, WA | 2001 | Part of Fred Hutchinson Cancer Research Center |
| Indiana University Health Proton Therapy Center | Bloomington, IN | 2004 | Formerly MPRI (Closed 4December 2014) |
| University of Florida Health Proton Therapy Institute-Jacksonville[59] | Jacksonville, FL | 2006 | The UF Health Proton Therapy Institute is a part of a non-profit academic medical research facility. It is the first treatment center in the Southeast U.S. to offer proton therapy. |
| University of Texas MD Anderson Cancer Center[60] | Houston, TX | 2006 | |
| INTEGRIS Cancer Institute of Oklahoma[61] | Oklahoma City, OK | 2009 | First of a number of planned ProCure facilities |
| CDH Proton Center[62] | Warrenville, IL | 2010 | Second of a number of planned ProCure facilities |
| Roberts Proton Therapy Center, University of Pennsylvania Health System[63] | Philadelphia, PA | 2010 | The largest proton therapy center in the world, the Roberts Proton Therapy Center, which is a part of Penn's Abramson Cancer Center, is also part of a medical complex that includes the Hospital of the University of Pennsylvania, the Perelman Center for Advanced Medicine, and the Children's Hospital of Philadelphia. |
| Hampton University Proton Therapy Institute | Hampton, VA | 2010 | |
| ProCure Proton Therapy Center[64] | Somerset, NJ | 2012 | Third of a number of planned ProCure facilities |
| Siteman Cancer Center[43] | St. Louis, MO | 2013 | First of the new single suite, ultra-compact,superconducting synchrocyclotron,[65] lower cost facilities to treat a patient using the Mevion Medical system's S250.[66] |
| Provision Proton Therapy Center[67] | Knoxville, TN | 2014 | |
| Scripps Health Scripps Proton Therapy Center [68] | San Diego, CA | 2014 | (5 suites, all using pencil-beam scanning precision also called IMPT) Manufactured by Varian Medical Systems [69] |
| Ackerman Cancer Center | Jacksonville, FL | 2015 | Ackerman Cancer Center is the world's first private, physician-owned practice to provide proton therapy, in addition to conventional radiation therapy and on-site diagnostic services. |
| The Laurie Proton Therapy Center, Robert Wood Johnson University Hospital | New Brunswick, NJ | 2015 | The Laurie Proton Therapy Center is home to the world’s third MEVION S250 Proton Therapy System. |
| Texas Center for Proton Therapy | Dallas Fort Worth, Texas | 2015 | TCPT is a joint venture between Baylor, McKesson, and Texas Oncology. It has three pencil beam rooms and cone beam CT imaging. |
| Mayo Clinic Cancer Center | Phoenix, Arizona | 2016 | Mayo Clinic Cancer Center Officially opened its doors in February 2016. |
| The Marjorie and Leonard Williams Center for Proton Therapy | Orlando, Florida | 2016 | http://www.ufhealthcancerorlando.com/centers/proton-therapy-center Opened its doors in April 2016. |
Outside the USA
United Kingdom
In 2013 the British government announced that £250 million had been budgeted to establish two centers for advanced radiotherapy, to open in 2018 at the Christie Hospital NHS Foundation Trust in Manchester and University College London Hospitals NHS Foundation Trust. These would offer high-energy proton therapy, currently unavailable in the UK, as well as other types of advanced radiotherapy, including intensity modulated radiotherapy (IMRT) and image guided radiotherapy (IGRT).[72] In 2014, only low-energy proton therapy was available in the UK, at the Clatterbridge Cancer Centre NHS Foundation Trust in Merseyside. But NHS England has paid to have suitable cases treated abroad, mostly in the US. Such cases have risen from 18 in 2008 to 122 in 2013, 99 of whom were children. The cost to the National Health Service averaged around £100,000 per case.[73]
In January 2015, it was announced the UK would get its first high energy proton beam therapy centre a year earlier than expected.[74] A company named Advanced Oncotherapy signed a deal with Howard de Walden Estates to install a machine in Harley Street, the heart of private medicine in London, to be ready by 2017. Advanced Oncotherapy’s system allows for more rapid movement and energy variation of the proton beam.[75] The technological advance also allows the company to build proton therapy facilities one-third smaller and one-fifth the cost of facilities based on the NHS first-generation machines which will come on stream a year later. The NHS has been criticised by leading doctors for buying old equipment.[76]
See also
- Particle therapy, Charged particle therapy, Hadron, Microbeam
- Fast neutron therapy
- Boron neutron capture therapy
- Linear energy transfer, Electromagnetic radiation and health
- Dosimetry, Dosimeter, Ionizing radiation
- List of oncology-related terms
References
- ^ a b Adapted from "Proton beam therapy" W P Levin, H Kooy, J S Loeffler and T F DeLaney British Journal of Cancer (2005) 93, 849–854 [1]
- ^ O. Jakel: State of the art in hadron therapy. AIP Conference Proceedings, vol. 958, no.1, 2007, pp. 70-77
- ^ a b "Zap! You're not dead." Economist, 8 September 2007. 384 (8545):13-14
- ^ a b Metz, James (2006-07-31). "Differences Between Protons and X-rays". The Abramson Cancer Center of the University of Pennsylvania. Retrieved 2008-02-04.
the beam then stops, resulting in virtually no radiation to the tissue beyond the target- or no "exit dose"
- ^ Camphausen KA, Lawrence RC. "Principles of Radiation Therapy" in Pazdur R, Wagman LD, Camphausen KA, Hoskins WJ (Eds) Cancer Management: A Multidisciplinary Approach. 11 ed. 2008.
- ^ "Radiological Use of Fast Protons", R. R. Wilson, Radiology, 47:487-491 (1946)
- ^ Richard Wilson, "A Brief History of the Harvard University Cyclotrons", Harvard University Press, 2004, pp 9
- ^ a b "PTCOG: Particle Therapy Co-Operative Group". Ptcog.web.psi.ch. Retrieved 2009-09-03.
- ^ a b c "Particle therapy facilities in operation". Particle Therapy Co-Operative Group. 2013-08-27. Retrieved 2014-09-01.
- ^ "Particle therapy facilities in operation". Particle Therapy Co-Operative Group. Retrieved 2010-04-27.
- ^ a b c R. P. Levy et al., The current status and future directions of heavy charged particle therapy in medicine, AIP Journal, March 2009
- ^ Hug E. B.; et al. (1999). ": Proton radiation therapy for chordomas and chondrosarcomas of the skull base". J. Neurosurgery. 91: 432–439. doi:10.3171/jns.1999.91.3.0432.
- ^ E. Gragoudas et al., Evidence-based estimates of outcomes in patients treated for intraocular melenoma", Arch. Ophthalmol.120, 1665-1671 (2002)
- ^ Munzenrider J. E., Liebsch N. J. (1999). "Proton radiotherapy for tumors of the skull base". Strahnlenther. Onkol. 175: 57–63. doi:10.1007/bf03038890.
- ^ "Proton Therapy for Ocular Tumors".
- ^ W. H. St. Clair et al, Advantage of protons compared to conventional X-ray or IMRT in the treatment of a pediatric patient with medulloblastoma, Int. J. Radiat. Oncol. Biol. Phys.58, 727-734 (2004)
- ^ D.G. Kirsch and N. J. Tarbell, Conformal radiation therapy for childhood CNS tumors, The Oncologist 9(4), 442-450 (2004)
- ^ Slater J. D.; et al. (2004). ", Proton therapy for prostate cancer; the initial Loma Linda University experience". Int. J. Radiat. Oncol. Biol. Phys. 59: 348–352. doi:10.1016/j.ijrobp.2003.10.011.
- ^ a b A. L. Zietman et al, Comparisons of conventional-dose vs. high-dose conformal radiation therapy in clinically localized adenocarcinoma of the prostate: a randomized controlled trial, J. A. M. A. 294(10) 1233-1239 (2005)
- ^ a b R. deCrevoisier et al, "Increased risk of biochemical and local failure in patients with distended rectum on the planning CT for prostate cancer radiotherapy," Int. J. Radiat. Oncol. Biol. Phys. 62(4) 965-973 (2005)
- ^ Lambert; et al. (2005). "Intrafractional motion during proton beam scanning". Phys. Med. Biol. 50: 4853–4862. doi:10.1088/0031-9155/50/20/008.
- ^ Byrne Thomas E (2005). "A Review of Prostate Motion with Considerations for the Treatment of Prostate Cancer". Medical Dosimerty. 30 (3): 155–161. doi:10.1016/j.meddos.2005.03.005.
- ^ Dyk, Jacob, Van (1999). The modern technology of radiation oncology: A Compendium for Medical Physicists and Radiation Oncologists. p. 826: Medical Physics Publishing Corporation. p. 1072. ISBN 9780944838389.
Proton Patient Summary - Inception Through December 1998...Prostate...2591 64.3%
{{cite book}}: CS1 maint: location (link) - ^ "The Promise of Proton-Beam Therapy". U.S. News and World Report. 2008-04-16. Retrieved 2008-02-20.
- ^ "Francis H. Burr Proton Therapy Center" (PDF).
- ^ J. Sisterson, Ion beam therapy in 2004, Nuclear Instruments and Methods in Physics Research B 241 713-716 (2005)
- ^ Boris Peter Selby et al., "Pose estimation of eyes for particle beam treatment of tumors.", Bildverarbeitung für die Medizin (Medical Image Processing); Munich, 2007 pp. 368-373.
- ^ a b c Joel E. Tepper, MD, and A. William Blackstock, MD (20 October 2009). "EDITORIAL: Randomized Trials and Technology Assessment". Annals of Internal Medicine. 151 (8): 583–584. doi:10.7326/0003-4819-151-8-200910200-00146. PMID 19755346.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b BOULTON, GUY (March 30, 2008). "High cost; of high tech; Outlay vs. benefit of expensive medical devices questioned". Milwaukee Journal Sentinel. Retrieved 2009-09-03.
Despite that controversy, roughly a dozen proton therapy centers have been proposed throughout the country, including northern Illinois
- ^ a b David Whelan and Robert Langreth (March 16, 2009). "The $150 Million Zapper:Does every cancer patient really need proton-beam therapy?". Forbes. Retrieved 2009-09-03.
- ^ Terasawa, T; Teruhiko Terasawa, MD; Tomas Dvorak, MD; Stanley Ip, MD; Gowri Raman, MD; Joseph Lau, MD; Thomas A. Trikalinos, MD, PhD (20 October 2009). "Systematic Review: Charged-Particle Radiation Therapy for Cancer". Annals of Internal Medicine. 151 (8): 556–565. doi:10.7326/0003-4819-151-8-200910200-00145. PMID 19755348.
{{cite journal}}: CS1 maint: multiple names: authors list (link)[FREE] - ^ Proton beams vs. radiation: 5-year MGH study seeks definitive answers about costly prostate cancer treatment, By Carolyn Y. Johnson, Boston Globe, May 14, 2012
- ^ "Particle Beam Radiation Therapies for Cancer: Policymaker Summary Guide". U.S. Department of Health and Human Services. September 14, 2009. Retrieved 2009-10-09.
- ^ a b "Particle Beam Radiation Therapies for Cancer Final Research Review". U.S. Department of Health and Human Services Federal Agency for Healthcare Research and Quality. September 14, 2009.
- ^ Feldstein, Dan (Oct 23, 2005). "M.D. Anderson private venture raises questions/ Proton-therapy benefits at center won't merit costs of care, some say". Houston Chronicle. Retrieved 2009-10-01.
M.D. Anderson officials estimate that when patients on all types of insurance and payment plans are mixed together, proton delivery will cost an average of $37,000 per patient for prostate treatment, compared with $29,000 for IMRT and $21,000 for standard radiation. The amount excludes doctor fees, which will be roughly the same for each.
- ^ Emanuel EJ; Pearson SD (2012-01-02). "It Costs More, but Is It Worth More?". The Opinion Pages. New York: The New York Times. Retrieved 2012-01-03.
- ^ Cox, Jeremy (2009-11-23). "UF Proton Therapy Institute study shows positive outcomes". Jacksonville.com. Retrieved 2009-12-22.
- ^ Ashya King: This story isn't quite what it seems
- ^ What is proton beam therapy?
- ^ "Introducing Hyperscan". Mevion Medical Systems. 2015-04-19.
- ^ Sheets, NC; Goldin, GH; Meyer, AM; Wu, Y; Chang, Y; Stürmer, T; Holmes, JA; Reeve, BB; Godley, PA; Carpenter, WR; Chen, RC (Apr 18, 2012). "Intensity-modulated radiation therapy, proton therapy, or conformal radiation therapy and morbidity and disease control in localized prostate cancer". JAMA: The Journal of the American Medical Association. 307 (15): 1611–20. doi:10.1001/jama.2012.460. PMID 22511689.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Goitein, M., & Jermann, M. 2003. "The Relative Costs of Proton and X-ray Radiation Thearpy. (2003)". Clinical Oncology, 15, S37–50. 15: S37–S50. doi:10.1053/clon.2002.0174.
{{cite journal}}: Italic or bold markup not allowed in:|journal=(help)CS1 maint: multiple names: authors list (link) CS1 maint: numeric names: authors list (link) - ^ a b "Siteman Cancer Center Treats First Patient With First-of-Its-Kind Proton Therapy System". PRWeb. Retrieved 2014-01-09.
- ^ a b "God particle technology to cancer patients".
- ^ Lievens, Y., & Van den Bogaert, W. 2005. Proton beam therapy: Too expensive to become true? Radiotherapy and Oncology, 75, 131–3.
- ^ St Clair, W. H., Adams, J. A., Bues, M., Fullerton, B. C., La Shell, S., Kooy, H. M., Loeffler, J. S., and Tarbell, N. J. (2004). Advantage of protons compared to conventional X-ray or IMRT in the treatment of a pediatric patient with medulloblastoma. Int. J. Radiat. Oncol. Biol. Phys. 58, 727–734.
- ^ Merchant, T. E., Hua, C. H., Shukla, H., Ying, X., Nill, S., and Oelfke, U. (2008). Proton versus photon radiotherapy for common pediatric brain tumors: comparison of models of dose characteristics and their relationship to cognitive function. Pediatr. Blood Cancer 51, 110–117.
- ^ Konski A., Speier W., Hanlon A., Beck J. R., Pollack A. (2007). "Is proton beam therapy cost effective in the treatment of adenocarcinoma of the prostate?". J. Clin. Oncol. 25: 3603–3608. doi:10.1200/jco.2006.09.0811.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ NGUYEN P., TROFIMOV A.; et al. (2008). "Proton-Beam vs. Intensity-Modulated Radiation Therapy, Which Is Best for Treating Prostate Cancer?". Oncology. 22: 7.
- ^ Langreth, Robert (March 26, 2012). "Prostate Cancer Therapy Too Good to Be True Explodes Health Cost". Bloomberg. Retrieved May 16, 2013.
- ^ Lundkvist J., Ekman M., Ericsson S. R., Jönsson B., Glimelius B. (2005a). "Cost-effectiveness of proton radiation in the treatment of childhood medulloblastoma". Cancer. 103: 793–801. doi:10.1002/cncr.20844.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ "Mevion Medical Systems continues Manufacturing Ramp Up". Marketwatch.com. 2012-11-01. Archived from the original on October 29, 2013. Retrieved 2012-11-29.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ "Operating clinical proton centres". http://www.proton-cancer-treatment.com/. Retrieved 23 January 2016.
{{cite web}}: External link in|website= - ^ "Hadron Therapy Patient Statistics" (PDF). Particle Therapy Co-Operative Group. Retrieved 2012-03-30.
- ^ a b J.N.A. Matthews: "Accelerators shrink to meet growing demand for proton therapy", Physics Today, March 2009, p. 22
- ^ "N.J. proton therapy center opens today". DotMed.com. Retrieved 2012-03-30.
- ^ http://cyclotron.crocker.ucdavis.edu/
- ^ "Proton Therapy Treatment and Research Center". Loma Linda University Medical Center. Retrieved 2013-11-05.
- ^ "Proton Therapy Jacksonville | Cancer Treatment". University of Florida Proton Therapy Institute. Retrieved 2013-11-05.
- ^ "Proton Therapy Center". University of Texas MD Anderson Cancer Center. Retrieved 2013-11-05.
- ^ "Oklahoma Proton Therapy Treatment Center". ProCure. Retrieved 2013-11-05.
- ^ "Illinois Proton Therapy Treatment Center". ProCure. Retrieved 2013-11-05.
- ^ "Proton Therapy at Penn Medicine". Perelman Center for Advanced Medicine. Retrieved 2013-11-05.
- ^ "New Jersey Proton Therapy Treatment Center". ProCure. Retrieved 2013-11-05.
- ^ "Elegant and Precise". Mevion Medical Systems. Retrieved 2015-04-19.
- ^ "Introducing the Mevion S250". Mevion. Retrieved 2015-04-19.
- ^ "Proton therapy cancer treatment center opens, first of its kind in Tennessee". WATE TV. Retrieved 2014-01-25.
- ^ "Scripps Proton Therapy Center". Scripps Health. Retrieved 2015-03-28.
- ^ "Oncology, Solutions, Proton Therapy". Varian Medical Systems. Retrieved 2015-04-19.
- ^ TRIUMF Proton Therapy
- ^ Clatterbridge Cancer Centre NHS Foundation Trust
- ^ "Manchester and London proton beam therapy units confirmed", Press release, Press Association, Cancer Research UK, 1 August 2013
- ^ "Ashya King case: What is proton beam therapy?" BBC news story with NHS England figures, 31 August 2014
- ^ http://www.lse.co.uk/AllNews.asp?code=dqaddbqb&headline=Advanced_Oncotherapy_Signs_Lease_Deal_To_Establish_UK_LIGHT_Centre
- ^ "NeoStem (Amex: NBS) 15M units Prices at $0.40 per unit for $6M Public Offering". www.proactiveinvestors.co.uk. Retrieved 11 August 2015.
- ^ "Brain tumor boy Ashya King 'could soon be walking unaided'... as NHS is blasted for buying 'old' equipment". The Mail on Sunday. Retrieved 11 August 2015.
Further reading
- Greco C., Wolden S. (Apr 2007). "Current status of radiotherapy with proton and light ion beams". Cancer. 109 (7): 1227–38. doi:10.1002/cncr.22542. PMID 17326046.
- "Use of Protons for Radiotherapy", A.M. Koehler, Proc. of the Symposium on Pion and Proton Radiotherapy, Nat. Accelerator Lab., (1971).
- A.M. Koehler, W.M. Preston, "Protons in Radiation Therapy: comparative Dose Distributions for Protons, Photons and Electrons Radiology 104(1):191–195 (1972).
- "Bragg Peak Proton Radiosurgery for Arteriovenous Malformation of the Brain" R.N. Kjelberg, presented at First Int. Seminar on the Use of Proton Beams in Radiation Therapy, Moskow (1977).
- Austin-Seymor, M.J. Munzenrider, et al. "Fractionated Proton Radiation Therapy of Cranial and Intracrainial Tumors" Am. J. of Clinical Oncology 13(4):327–330 (1990).
- "Proton Radiotherapy", Hartford, Zietman, et al. in Radiotheraputic Management of Carcinoma of the Prostate, A. D'Amico and G.E. Hanks. London,UK, Arnold Publishers: 61–72 (1999).
External links
- Proton therapy—MedlinePlus Medical Encyclopedia
- Proton Therapy
- "Proton therapy is coming to the UK, but what does it mean for patients?", Arney, Kat, Science blog, Cancer Research UK, 16 September 2013
- CERN - AVO
- Proton Therapy in Korea
