Neurofibromatosis type I: Difference between revisions
No edit summary |
|||
| Line 71: | Line 71: | ||
===Neurobehavioral developmental disorder=== |
===Neurobehavioral developmental disorder=== |
||
The most common complication in patients with NF-1 is cognitive and learning disability. These cognitive problems have been shown to be present in approximately 80% of children with NF-1 and have significant effects on their schooling and everyday life.<ref>{{cite journal |author=Hyman SL, Shores A, North KN |title=The nature and frequency of cognitive deficits in children with neurofibromatosis type 1 |journal=Neurology |volume=65 |issue=7 |pages=1037–44 |date=October 2005 |pmid=16217056 |doi=10.1212/01.wnl.0000179303.72345.ce |
The most common complication in patients with NF-1 is cognitive and learning disability. These cognitive problems have been shown to be present in approximately 80% of children with NF-1 and have significant effects on their schooling and everyday life.<ref>{{cite journal |author=Hyman SL, Shores A, North KN |title=The nature and frequency of cognitive deficits in children with neurofibromatosis type 1 |journal=Neurology |volume=65 |issue=7 |pages=1037–44 |date=October 2005 |pmid=16217056 |doi=10.1212/01.wnl.0000179303.72345.ce }}</ref> These cognitive problems have been shown to be stable into adulthood and do not get worse unlike some of the other physical symptoms of NF-1.<ref>{{cite journal |author=Hyman SL, Gill DS, Shores EA, et al. |title=Natural history of cognitive deficits and their relationship to MRI T2-hyperintensities in NF1 |journal=Neurology |volume=60 |issue=7 |pages=1139–45 |date=April 2003 |pmid=12682321 |doi=10.1212/01.WNL.0000055090.78351.C1}}</ref> The most common cognitive problems are with perception, executive functioning and attention. Disorders include: |
||
* [[Attention deficit hyperactivity disorder]] has been shown to be present in approximately 38% of children with NF-1. |
* [[Attention deficit hyperactivity disorder]] has been shown to be present in approximately 38% of children with NF-1. |
||
*Speech and language delays have also been identified in approximately 68% of preschool children with NF1.<ref>{{cite journal |author=Thompson HL, Viskochil DH, Stevenson DA, Chapman KL |title=Speech-language characteristics of children with neurofibromatosis type 1 |journal=Am. J. Med. Genet. A |volume=152A |issue=2 |pages=284–90 |date=February 2010 |pmid=20101681 |doi=10.1002/ajmg.a.33235 }}</ref> |
*Speech and language delays have also been identified in approximately 68% of preschool children with NF1.<ref>{{cite journal |author=Thompson HL, Viskochil DH, Stevenson DA, Chapman KL |title=Speech-language characteristics of children with neurofibromatosis type 1 |journal=Am. J. Med. Genet. A |volume=152A |issue=2 |pages=284–90 |date=February 2010 |pmid=20101681 |doi=10.1002/ajmg.a.33235 }}</ref> |
||
* Math deficits. |
* Math deficits. |
||
* Motor deficits are common. Motor deficits due to NF-1 are probably not [[Cerebellum|cerebellar]].<ref>{{cite journal |author=van der Vaart T, van Woerden GM, Elgersma Y, de Zeeuw CI, Schonewille M |title=Motor deficits in neurofibromatosis type 1 mice: the role of the cerebellum |journal=Genes Brain Behav. |volume=10 |issue=4 |pages=404–9 |date=June 2011 |pmid=21352477 |doi=10.1111/j.1601-183X.2011.00685.x |
* Motor deficits are common. Motor deficits due to NF-1 are probably not [[Cerebellum|cerebellar]].<ref>{{cite journal |author=van der Vaart T, van Woerden GM, Elgersma Y, de Zeeuw CI, Schonewille M |title=Motor deficits in neurofibromatosis type 1 mice: the role of the cerebellum |journal=Genes Brain Behav. |volume=10 |issue=4 |pages=404–9 |date=June 2011 |pmid=21352477 |doi=10.1111/j.1601-183X.2011.00685.x }}</ref> |
||
* Spatial deficit. [[Lovastatin]], normally used to treat [[hypercholesterolemia]], is currently in phase one of clinical trial (NCT00352599). This drug has been shown to reverse spatial deficits in [[mice]].<ref> |
* Spatial deficit. [[Lovastatin]], normally used to treat [[hypercholesterolemia]], is currently in phase one of clinical trial (NCT00352599). This drug has been shown to reverse spatial deficits in [[mice]].<ref>{{ClinicalTrialsGov|NCT00352599|Trial to Evaluate the Safety of Lovastatin in Individuals With Neurofibromatosis Type I (NF1)}}</ref> [[Simvastatin]], a drug similar to lovastatin, did not show benefit on cognitive function or behaviour in two [[randomized controlled trials]] in children with NF1.<ref>{{cite journal |author=Krab LC, de Goede-Bolder A, Aarsen FK, ''et al.'' |title=Effect of simvastatin on cognitive functioning in children with neurofibromatosis type 1: a randomized controlled trial |journal=JAMA |volume=300 |issue=3 |pages=287–94 |date=July 2008 |pmid=18632543 |pmc=2664742 |doi=10.1001/jama.300.3.287 }}</ref><ref>{{cite journal |author=van der Vaart T, Plasschaert E, Rietman AB, ''et al.'' |title=Simvastatin for cognitive deficits and behavioural problems in patients with neurofibromatosis type 1 (NF1-SIMCODA): a randomised, placebo-controlled trial |journal=Lancet Neurol |volume=12 |issue=11 |pages=1076–83 |date=November 2013 |pmid=24090588 |doi=10.1016/S1474-4422(13)70227-8 }}</ref> |
||
* [[Asperger's Syndrome]]. |
* [[Asperger's Syndrome]]. |
||
| Line 108: | Line 108: | ||
{{main|Epilepsy}} |
{{main|Epilepsy}} |
||
* '''Occurrence'''. Epileptic seizures haven been reported in up to 7% of NF-1 patients.<ref>{{cite journal |author=Vivarelli R, Grosso S, Calabrese F, et al. |title=Epilepsy in neurofibromatosis 1 |journal=J. Child Neurol. |volume=18 |issue=5 |pages=338–42 |date=May 2003 | |
* '''Occurrence'''. Epileptic seizures haven been reported in up to 7% of NF-1 patients.<ref>{{cite journal |author=Vivarelli R, Grosso S, Calabrese F, et al. |title=Epilepsy in neurofibromatosis 1 |journal=J. Child Neurol. |volume=18 |issue=5 |pages=338–42 |date=May 2003 |pmid=12822818 |doi=10.1177/08830738030180050501}}</ref> |
||
* '''Diagnosis'''. Electroencephalograph, magnetic resonance imaging, computed tomographic scan, single-photon emission CT and positron emission tomographic scan. |
* '''Diagnosis'''. Electroencephalograph, magnetic resonance imaging, computed tomographic scan, single-photon emission CT and positron emission tomographic scan. |
||
* '''Etiology'''. Due to cerebral tumors, cortical malformation, mesial temporal sclerosis. |
* '''Etiology'''. Due to cerebral tumors, cortical malformation, mesial temporal sclerosis. |
||
| Line 131: | Line 131: | ||
===Mental disorder=== |
===Mental disorder=== |
||
Children with NF-1 can experience social problems, attention problems, social anxiety, depression, withdrawal, thought problems, somatic complaints, and aggressive behavior.<ref>{{cite journal |author=Johnson NS, Saal HM, Lovell AM, Schorry EK |title=Social and emotional problems in children with neurofibromatosis type 1: evidence and proposed interventions |journal=J. Pediatr. |volume=134 |issue=6 |pages=767–72 |date=June 1999 |pmid=10356149 |
Children with NF-1 can experience social problems, attention problems, social anxiety, depression, withdrawal, thought problems, somatic complaints, and aggressive behavior.<ref>{{cite journal |author=Johnson NS, Saal HM, Lovell AM, Schorry EK |title=Social and emotional problems in children with neurofibromatosis type 1: evidence and proposed interventions |journal=J. Pediatr. |volume=134 |issue=6 |pages=767–72 |date=June 1999 |pmid=10356149 |doi=10.1016/S0022-3476(99)70296-9}}</ref> Treatments include [[psychotherapy]], [[antidepressants]] and [[cognitive behavioral therapy]]. |
||
===Cancer=== |
===Cancer=== |
||
| Line 138: | Line 138: | ||
* '''Diagnosis'''. [[Magnetic resonance imaging|MRI]]. |
* '''Diagnosis'''. [[Magnetic resonance imaging|MRI]]. |
||
* '''Treatment'''. Surgery (primary) +/- radiation therapy. |
* '''Treatment'''. Surgery (primary) +/- radiation therapy. |
||
* '''Mortality'''. Malignant nerve sheath tumor was the main cause of death (60%) in a study of 1895 patients with NF-1 from France in the time period 1980-2006 indicated excess mortality in NF-1 patients compared to the general population.<ref> |
* '''Mortality'''. Malignant nerve sheath tumor was the main cause of death (60%) in a study of 1895 patients with NF-1 from France in the time period 1980-2006 indicated excess mortality in NF-1 patients compared to the general population.<ref>{{cite journal |last1=Duong |first1=Tu |last2=Sbidian |first2=Emilie |last3=Valeyrie-Allanore |first3=Laurence |last4=Vialette |first4=Cédric |last5=Ferkal |first5=Salah |last6=Hadj-Rabia |first6=Smaïl |last7=Glorion |first7=Christophe |last8=Lyonnet |first8=Stanislas |last9=Zerah |first9=Michel |last10=Kemlin |first10=Isabelle |last11=Rodriguez |first11=Diana |last12=Bastuji-Garin |first12=Sylvie |last13=Wolkenstein |first13=Pierre |title=Mortality Associated with Neurofibromatosis 1: A Cohort Study of 1895 Patients in 1980-2006 in France |journal=Orphanet Journal of Rare Diseases |volume=6 |issue= |pages=18 |year=2011 |pmid=21542925 |pmc=3095535 |doi=10.1186/1750-1172-6-18 }}</ref> The cause of death was available for 58 (86.6%) patients. The study found excess mortality occurred among patients aged 10 to 40 years. Significant excess mortality was found in both males and females. |
||
==Cause== |
==Cause== |
||
| Line 146: | Line 146: | ||
NF-1 is a [[microdeletion syndrome]] caused by a [[mutation]] of a [[gene]] located on chromosomal segment 17q11.2 on the long arm of [[chromosome 17]] which encodes a protein known as [[neurofibromin 1|neurofibromin]]<ref name="pmid2134734">{{cite journal|last1=Wallace|first1=MR|last2=Marchuk|first2=DA|last3=Andersen|first3=LB|last4=Letcher|first4=R|last5=Odeh|first5=HM|last6=Saulino|first6=AM|last7=Fountain|first7=JW|last8=Brereton|first8=A|last9=Nicholson|first9=J|last10=Mitchell|first10=AL|title=Type 1 neurofibromatosis gene: identification of a large transcript disrupted in three NF1 patients.|journal=Science (New York, N.Y.)|date=13 July 1990|volume=249|issue=4965|pages=181-6|pmid=2134734|doi=10.1126/science.2134734}}</ref> (not to be confused with the disorder itself) which plays a role in [[cell signaling]].<ref>[http://www.genecards.org/cgi-bin/carddisp.pl?gene=NF1 "neurofibromin 1" [[GeneCards]]]</ref><ref>[http://genome.ucsc.edu/cgi-bin/hgGene?hgg_gene=uc002hgf.1&org=human "Human Gene NF1 (uc002hgf.1) Description and Page Index"]</ref> The [[Neurofibromin 1]] gene is a negative regulator of the [[Ras (protein)|Ras]] [[oncogene]] [[signal transduction]] pathway. It stimulates the [[GTPase]] activity of [[Ras (protein)|Ras]]. It shows greater [[Chemical affinity|affinity]] for [[RAS p21 protein activator 1]], but lower [[Enzyme assay#Specific activity|specific activity]]. The [[Messenger RNA|mRNA]] for this gene is subject to [[RNA editing]] ([[Chorionic gonadotropin alpha|CGA]]->UGA->Arg1306Term) resulting in premature translation termination. [[Alternative splicing|Alternatively spliced transcript variants]] encoding different [[Protein isoform|isoforms]] have also been described for this gene. |
NF-1 is a [[microdeletion syndrome]] caused by a [[mutation]] of a [[gene]] located on chromosomal segment 17q11.2 on the long arm of [[chromosome 17]] which encodes a protein known as [[neurofibromin 1|neurofibromin]]<ref name="pmid2134734">{{cite journal|last1=Wallace|first1=MR|last2=Marchuk|first2=DA|last3=Andersen|first3=LB|last4=Letcher|first4=R|last5=Odeh|first5=HM|last6=Saulino|first6=AM|last7=Fountain|first7=JW|last8=Brereton|first8=A|last9=Nicholson|first9=J|last10=Mitchell|first10=AL|title=Type 1 neurofibromatosis gene: identification of a large transcript disrupted in three NF1 patients.|journal=Science (New York, N.Y.)|date=13 July 1990|volume=249|issue=4965|pages=181-6|pmid=2134734|doi=10.1126/science.2134734}}</ref> (not to be confused with the disorder itself) which plays a role in [[cell signaling]].<ref>[http://www.genecards.org/cgi-bin/carddisp.pl?gene=NF1 "neurofibromin 1" [[GeneCards]]]</ref><ref>[http://genome.ucsc.edu/cgi-bin/hgGene?hgg_gene=uc002hgf.1&org=human "Human Gene NF1 (uc002hgf.1) Description and Page Index"]</ref> The [[Neurofibromin 1]] gene is a negative regulator of the [[Ras (protein)|Ras]] [[oncogene]] [[signal transduction]] pathway. It stimulates the [[GTPase]] activity of [[Ras (protein)|Ras]]. It shows greater [[Chemical affinity|affinity]] for [[RAS p21 protein activator 1]], but lower [[Enzyme assay#Specific activity|specific activity]]. The [[Messenger RNA|mRNA]] for this gene is subject to [[RNA editing]] ([[Chorionic gonadotropin alpha|CGA]]->UGA->Arg1306Term) resulting in premature translation termination. [[Alternative splicing|Alternatively spliced transcript variants]] encoding different [[Protein isoform|isoforms]] have also been described for this gene. |
||
In 1989, through linkage and cross over analyses, neurofibromin was localized to chromosome 17.<ref name=autogenerated1>{{cite journal |author=Goldberg NS, Collins FS |title=The hunt for the neurofibromatosis gene |journal=Arch Dermatol |volume=127 |issue=11 |pages=1705–7 |date=November 1991 | |
In 1989, through linkage and cross over analyses, neurofibromin was localized to chromosome 17.<ref name=autogenerated1>{{cite journal |author=Goldberg NS, Collins FS |title=The hunt for the neurofibromatosis gene |journal=Arch Dermatol |volume=127 |issue=11 |pages=1705–7 |date=November 1991 |pmid=1952978 |doi=10.1001/archderm.1991.01680100105014}}</ref> It was localized to the long arm of chromosome 17 by chance when researchers discovered chromosome exchanges between chromosome 17 with chromosome 1 and 22.<ref name=autogenerated1 /> This exchange of genetic material presumably caused a mutation in the neurofibromin gene, leading to the NF1 phenotype. Two recurrent microdeletion types with microdeletion breakpoints located in paralogous regions flanking NF1 (proximal NF1-REP-a and distal NF1-REP-c for the 1.4 Mb type-1 microdeletion, and SUZ12 and SUZ12P for the 1.2 Mb type-2 microdeletion), are found in most cases.<ref>{{cite journal|last1=Pasmant|first1=E|last2=Sabbagh|first2=A|last3=Spurlock|first3=G|last4=Laurendeau|first4=I|last5=Grillo|first5=E|last6=Hamel|first6=MJ|last7=Martin|first7=L|last8=Barbarot|first8=S|last9=Leheup|first9=B|last10=Rodriguez|first10=D|last11=Lacombe|first11=D|last12=Dollfus|first12=H|last13=Pasquier|first13=L|last14=Isidor|first14=B|last15=Ferkal|first15=S|last16=Soulier|first16=J|last17=Sanson|first17=M|last18=Dieux-Coeslier|first18=A|last19=Bièche|first19=I|last20=Parfait|first20=B|last21=Vidaud|first21=M|last22=Wolkenstein|first22=P|last23=Upadhyaya|first23=M|last24=Vidaud|first24=D|last25=members of the NF France|first25=Network|title=NF1 microdeletions in neurofibromatosis type 1: from genotype to phenotype.|journal=Human mutation|date=June 2010|volume=31|issue=6|pages=E1506-18|pmid=20513137}}</ref> |
||
===Structure of the Neurofibromin gene=== |
===Structure of the Neurofibromin gene=== |
||
The Neurofibromin gene was soon sequenced and found to be 350,000 base pairs in length.<ref name="autogenerated3">{{cite journal |author=Marchuk DA, Saulino AM, Tavakkol R, et al. |title=cDNA cloning of the type 1 neurofibromatosis gene: complete sequence of the NF1 gene product |journal=Genomics |volume=11 |issue=4 |pages=931–40 |date=December 1991 |pmid=1783401 |
The Neurofibromin gene was soon sequenced and found to be 350,000 base pairs in length.<ref name="autogenerated3">{{cite journal |author=Marchuk DA, Saulino AM, Tavakkol R, et al. |title=cDNA cloning of the type 1 neurofibromatosis gene: complete sequence of the NF1 gene product |journal=Genomics |volume=11 |issue=4 |pages=931–40 |date=December 1991 |pmid=1783401 |doi=10.1016/0888-7543(91)90017-9}}</ref> However, the protein is 2818 amino acids long leading to the concept of splice variants.<ref name=autogenerated2>{{cite journal |author=Gutmann DH, Giovannini M |title=Mouse models of neurofibromatosis 1 and 2 |journal=Neoplasia |volume=4 |issue=4 |pages=279–90 |year=2002 |pmid=12082543 |pmc=1531708 |doi=10.1038/sj.neo.7900249 }}</ref> For example, exon 9a, 23a and 48a are expressed in the neurons of the forebrain, muscle tissues and adult neurons respectively.<ref name="autogenerated2" /> |
||
Homology studies have shown that neurofibromin is 30% similar to proteins in the GTPase Activating Protein (GAP) Family.<ref name="autogenerated3" /> This homologous sequence is in the central portion of neurofibromin and being similar to the GAP family is recognized as a negative regulator of the [[Ras (protein)|Ras]] kinase.<ref>{{cite journal |author=Feldkamp MM, Angelov L, Guha A |title=Neurofibromatosis type 1 peripheral nerve tumors: aberrant activation of the Ras pathway |journal=Surg Neurol |volume=51 |issue=2 |pages=211–8 |date=February 1999 |pmid=10029430 |
Homology studies have shown that neurofibromin is 30% similar to proteins in the GTPase Activating Protein (GAP) Family.<ref name="autogenerated3" /> This homologous sequence is in the central portion of neurofibromin and being similar to the GAP family is recognized as a negative regulator of the [[Ras (protein)|Ras]] kinase.<ref>{{cite journal |author=Feldkamp MM, Angelov L, Guha A |title=Neurofibromatosis type 1 peripheral nerve tumors: aberrant activation of the Ras pathway |journal=Surg Neurol |volume=51 |issue=2 |pages=211–8 |date=February 1999 |pmid=10029430 |doi=10.1016/S0090-3019(97)00356-X}}</ref> |
||
Additionally, being such a large protein, more active domains of the protein have been identified. One such domain interacts with the protein [[Adenylate cyclase|adenylyl cyclase]],<ref>{{cite journal |author=Hannan F, Ho I, Tong JJ, Zhu Y, Nurnberg P, Zhong Y |title=Effect of neurofibromatosis type I mutations on a novel pathway for adenylyl cyclase activation requiring neurofibromin and Ras |journal=Hum. Mol. Genet. |volume=15 |issue=7 |pages=1087–98 |date=April 2006 |pmid=16513807 |pmc=1866217 |doi=10.1093/hmg/ddl023 |
Additionally, being such a large protein, more active domains of the protein have been identified. One such domain interacts with the protein [[Adenylate cyclase|adenylyl cyclase]],<ref>{{cite journal |author=Hannan F, Ho I, Tong JJ, Zhu Y, Nurnberg P, Zhong Y |title=Effect of neurofibromatosis type I mutations on a novel pathway for adenylyl cyclase activation requiring neurofibromin and Ras |journal=Hum. Mol. Genet. |volume=15 |issue=7 |pages=1087–98 |date=April 2006 |pmid=16513807 |pmc=1866217 |doi=10.1093/hmg/ddl023 }}</ref> and a second with [[CRMP1|collapsin response mediator protein]].<ref>{{cite journal |author=Ozawa T, Araki N, Yunoue S, et al. |title=The neurofibromatosis type 1 gene product neurofibromin enhances cell motility by regulating actin filament dynamics via the Rho-ROCK-LIMK2-cofilin pathway |journal=J. Biol. Chem. |volume=280 |issue=47 |pages=39524–33 |date=November 2005 |pmid=16169856 |doi=10.1074/jbc.M503707200 }}</ref> Together, likely with domains yet to be discovered, neurofibromin regulates many of the pathways responsible for overactive cell proliferation, learning impairments, skeletal defects and plays a role in neuronal development.<ref>{{cite journal |author=Le LQ, Parada LF |title=Tumor microenvironment and neurofibromatosis type I: connecting the GAPs |journal=Oncogene |volume=26 |issue=32 |pages=4609–16 |date=July 2007 |pmid=17297459 |pmc=2760340 |doi=10.1038/sj.onc.1210261 }}</ref> |
||
===Inheritance and spontaneous mutation=== |
===Inheritance and spontaneous mutation=== |
||
| Line 169: | Line 169: | ||
===Post-natal testing=== |
===Post-natal testing=== |
||
The National Institutes of Health (NIH) has created specific criteria for the diagnosis of NF-1. Two of these seven "Cardinal Clinical Features" are required for positive diagnosis.<ref>{{cite book |author=Huson, Susan Mary; Hughes, Richard Anthony Cranmer |title=The neurofibromatoses: a pathogenetic and clinical overview |publisher=Chapman & Hall |location=London |year=1994 |isbn=0-412-38920-7 |at=1.3.2:9}}</ref> There is practical flowchart to distinguish between NF1, NF2 and schwannomatosis |
The National Institutes of Health (NIH) has created specific criteria for the diagnosis of NF-1. Two of these seven "Cardinal Clinical Features" are required for positive diagnosis.<ref>{{cite book |author=Huson, Susan Mary; Hughes, Richard Anthony Cranmer |title=The neurofibromatoses: a pathogenetic and clinical overview |publisher=Chapman & Hall |location=London |year=1994 |isbn=0-412-38920-7 |at=1.3.2:9}}</ref> There is practical flowchart to distinguish between NF1, NF2 and schwannomatosis.<ref>{{cite journal |last1=Rodrigues |first1=Luiz Oswaldo Carneiro |last2=Batista |first2=Pollyanna Barros |last3=Goloni-Bertollo |first3=Eny Maria |last4=Souza-Costa |first4=Danielle de |last5=Eliam |first5=Lucas |last6=Eliam |first6=Miguel |last7=Cunha |first7=Karin Soares Gonçalves |last8=Darrigo Junior |first8=Luiz Guilherme |last9=Ferraz Filho |first9=José Roberto Lopes |last10=Geller |first10=Mauro |last11=Gianordoli-Nascimento |first11=Ingrid F. |last12=Madeira |first12=Luciana Gonçalves |last13=Malloy-Diniz |first13=Leandro Fernandes |last14=Mendes |first14=Hérika Martins |last15=Miranda |first15=Débora Marques de |last16=Pavarino |first16=Erika Cristina |last17=Baptista-Pereira |first17=Luciana |last18=Rezende |first18=Nilton A. |last19=Rodrigues |first19=Luíza de Oliveira |last20=Silva |first20=Carla Menezes da |last21=Souza |first21=Juliana Ferreira de |last22=Souza |first22=Márcio Leandro Ribeiro de |last23=Stangherlin |first23=Aline |last24=Valadares |first24=Eugênia Ribeiro |last25=Vidigal |first25=Paula Vieira Teixeira |title=Neurofibromatoses: part 1 – diagnosis and differential diagnosis |journal=Arquivos de Neuro-Psiquiatria |volume=72 |issue=3 |pages=241–50 |year=2014 |pmid=24676443 |doi=10.1590/0004-282X20130241 }}</ref> |
||
*Six or more [[café-au-lait spot]]s over 5 mm in greatest diameter in pre-pubertal individuals and over 15 mm in greatest diameter in post-pubertal individuals. Note that multiple café-au-lait spots alone are not a definitive diagnosis of NF-1 as these spots can be caused by a number of other conditions. |
*Six or more [[café-au-lait spot]]s over 5 mm in greatest diameter in pre-pubertal individuals and over 15 mm in greatest diameter in post-pubertal individuals. Note that multiple café-au-lait spots alone are not a definitive diagnosis of NF-1 as these spots can be caused by a number of other conditions. |
||
Revision as of 15:52, 23 August 2015
| Neurofibromatosis type I | |
|---|---|
| Specialty | Medical genetics, neurology |
| Frequency | 0.026998%, 0.0128%, 0.0217%, 0.0241%, 0.0457%, 0.0149%, 0.02691% |
Neurofibromatosis type I (NF-1) is a tumor disorder that is caused by the mutation of a gene on chromosome 17 that is responsible for control of cell division. NF-1 causes tumors along the nervous system. Common symptoms of NF-1 include scoliosis (curvature of the spine), learning disabilities, vision disorders, and epilepsy.
NF-1 was formerly known as von Recklinghausen disease after the researcher (Friedrich Daniel von Recklinghausen) who first documented the disorder. Neurofibromatosis type 1 is one of the most common single-gene disorders affecting neurological function in humans.[1]
NF-1 is not to be confused with Proteus syndrome.[2] NF-1 is a developmental syndrome caused by germline mutations in neurofibromin, a gene that is involved in the RAS pathway (RASopathy). In diagnosis it may also be confused with Legius syndrome.
Signs and symptoms


The following is a list of conditions and complications associated with NF-1, and, where available, age range of onset and progressive development, occurrence percentage of NF-1 population, method of earliest diagnosis, and treatments and related medical specialties.[3][4] The progression of the condition is roughly as follows:
- Congenital musculoskeletal disorders may or may not be present
- Cutaneous conditions may be observed in early infancy
- Small tumors may arise in the retina which can eventually lead to blindness
- Learning disabilities may arise in preschool children
- Neurofibromas may occur and cause many dependent neurological conditions and cutaneous and skeletal disfigurement
- Depression and social anxiety may occur as a result of disabilities caused by the condition
- Neurofibromas may transition into cancer which can be fatal
The NF Clinical Program at St. Louis Children's Hospital maintains a comprehensive list of current NF research studies.
Musculoskeletal disorder
Musculoskeletal abnormalities affecting the skull include Sphenoid bone dysplasia, Congenital Hydrocephalus and associated neurologic impairment. These abnormalities are non-progressive and may be diagnosed in the fetus or at birth.
Disorders affecting the spine include:
- In NF-1, there can be a generalized abnormality of the soft tissues in the fetus, which is referred to as mesodermal dysplasia, resulting in maldevelopment of skeletal structures.
- Meningoceles and formation of cystic diverticula of the dura of the spine, unrelated to Spina bifida
- Radiographically, Dural ectasia can lead to scalloping of the posterior vertebral bodies and to the formation of cystic diverticula of the dura of the spine (termed meningoceles. This meningocele is not related to spina bifida).
- Focal scoliosis and/or kyphosis are the most common skeletal manifestation of NF-1, occurring in 20% of affected patients. Approximately 25% of patients will require corrective surgery.
Facial bones and limbs
- Bowing of a long bone with a tendency to fracture and not heal, yielding a pseudarthrosis. The most common bone to be affected is the tibia, causing congenital pseudarthrosis of the tibia or CPT. CPT occurs in 2-4% of individuals with NF-1. Treatment includes limb amputation or correction by Ilizarov method .
- Malformation of the facial bones or of the eye sockets (lambdoid suture defects, sphenoid dysplasia)
- Unilateral overgrowth of a limb. When a plexiform neurofibroma manifests on a leg or arm, it will cause extra blood circulation, and may thus accelerate the growth of the limb. This may cause considerable difference in length between left and right limbs. To equalize the difference during childhood, there is an orthopedic surgery called epiphysiodesis, where growth at the epiphyseal (growth) plate is halted. It can be performed on one side of the bone to help correct an angular deformity, or on both sides to stop growth of that bone completely. The surgery must also be carefully planned with regard to timing, as it is non-reversible. The goal is that the limbs are at near-equal length at end of growth.
Skin
- Flat pigmented lesions of the skin called café au lait spots.[5] These spots can grow from birth to 16 years and are nonprogressive after that.
- Freckling of the axillae or inguinal regions.
- Dermal neurofibroma, manifested as single or multiple firm, rubbery bumps of varying sizes on a person's skin. Age of onset is puberty. Progressive in number and size. Not malignant. Can be treated with CO2 lasers.
Eye disease
- Lisch nodules in the iris.
- Optic gliomas along one or both optic nerves or the optic chiasm can cause bulging of the eyes, involuntary eye movement, squinting, and / or vision loss. Treatment may include surgery, radiation +/- steroids, or chemotherapy (in children).[6]
Neurobehavioral developmental disorder
The most common complication in patients with NF-1 is cognitive and learning disability. These cognitive problems have been shown to be present in approximately 80% of children with NF-1 and have significant effects on their schooling and everyday life.[7] These cognitive problems have been shown to be stable into adulthood and do not get worse unlike some of the other physical symptoms of NF-1.[8] The most common cognitive problems are with perception, executive functioning and attention. Disorders include:
- Attention deficit hyperactivity disorder has been shown to be present in approximately 38% of children with NF-1.
- Speech and language delays have also been identified in approximately 68% of preschool children with NF1.[9]
- Math deficits.
- Motor deficits are common. Motor deficits due to NF-1 are probably not cerebellar.[10]
- Spatial deficit. Lovastatin, normally used to treat hypercholesterolemia, is currently in phase one of clinical trial (NCT00352599). This drug has been shown to reverse spatial deficits in mice.[11] Simvastatin, a drug similar to lovastatin, did not show benefit on cognitive function or behaviour in two randomized controlled trials in children with NF1.[12][13]
- Asperger's Syndrome.
Nervous system disease
The primary neurologic involvement in NF-1 is of the peripheral nervous system, and secondarily of the central nervous system.
Peripheral neuropathy
Neurofibroma
A neurofibroma is a lesion of the peripheral nervous system. Its cellular lineage is uncertain, and may derive from Schwann cells, other perineural cell lines, or fibroblasts. Neurofibromas may arise sporadically, or in association with NF-1. A neurofibroma may arise at any point along a peripheral nerve. A number of drugs have been studied to treat this condition.
Neurofibroma conditions are progressive and include:
- Plexiform neurofibroma: Often congenital. Lesions are composed of sheets of neurofibromatous tissue that may infiltrate and encase major nerves, blood vessels, and other vital structures. These lesions are difficult and sometimes impossible to routinely resect without causing any significant damage to surrounding nerves and tissue. However, early intervention may be beneficial:a 2004 study in Germany concluded "Early surgical intervention of small superficial PNFs is uncomplicated, without burden for even the youngsters and enables total resection of the tumors. It may be considered as a preventive strategy for later disfigurement and functional deficits." [14][15]
- Solitary neurofibroma, affecting 8–12% of patients with NF-1. This occurs in a deep nerve trunk. Diagnosis by cross-sectional imaging (e.g., computed tomography or magnetic resonance) as a fusiform enlargement of a nerve.
- Schwannomas, peripheral nerve-sheath tumors which are seen with increased frequency in NF-1. The major distinction between a schwannoma and a solitary neurofibroma is that a schwannoma can be resected while sparing the underlying nerve, whereas resection of a neurofibroma requires the sacrifice of the underlying nerve.
- Nerve root neurofibroma.
- Bones, especially the ribs, can develop chronic erosions (pits) from the constant pressure of adjacent neurofibroma or Schwannoma. Similarly, the neural foramen of the spine can be widened due to the presence of a nerve root neurofibroma or schwannoma. Surgery may be needed when NF-1 related tumors compress organs or other structures.
Nerve sheath tumor

- Peripheral nerve sheath tumor.
- Chronic pain, numbness, and/or paralysis due to peripheral nerve sheath tumor.
Other complications
- Renal artery anomalies or pheochromocytoma and associated chronic hypertension
- Schwannoma
Central nervous system disease
Epilepsy
- Occurrence. Epileptic seizures haven been reported in up to 7% of NF-1 patients.[16]
- Diagnosis. Electroencephalograph, magnetic resonance imaging, computed tomographic scan, single-photon emission CT and positron emission tomographic scan.
- Etiology. Due to cerebral tumors, cortical malformation, mesial temporal sclerosis.
- Therapy. Drug therapy (57% amenable) where not resistant (29%).
Glial tumors
Intracranially, NF-1 patients have a predisposition to develop glial tumors of the central nervous system, primarily:
- Optic nerve gliomas and associated blindness.[17]
- Astrocytoma
Focally degenerative myelin
Another CNS manifestation of NF-1 is the so-called "unidentified bright object" or UBO, which is a lesion which has increased signal on a T2 weighted sequence of a magnetic resonance imaging examination of the brain. These UBOs are typically found in the Cerebral peduncle, pons, midbrain, globus pallidus, thalamus, and optic radiations. Their exact identity remains a bit of a mystery since they disappear over time (usually, by age 16), and they are not typically biopsied or resected. They may represent a focally degenerative bit of myelin.
Dural ectasia
Within the CNS, NF-1 manifests as a weakness of the dura, which is the tough covering of the brain and spine. Weakness of the dura leads to focal enlargement terms dural ectasia due to chronic exposure to the pressures of CSF pulsation.
Acetazolamide has shown promise as a treatment for this condition.
Mental disorder
Children with NF-1 can experience social problems, attention problems, social anxiety, depression, withdrawal, thought problems, somatic complaints, and aggressive behavior.[18] Treatments include psychotherapy, antidepressants and cognitive behavioral therapy.
Cancer
Cancer can arise in the form of Malignant peripheral nerve sheath tumor resulting from malignant degeneration of a plexiform neurofibroma.[15][19]
- Frequency. A plexiform neurofibroma has a lifetime risk of 8–12% of transformation into a malignant tumor.
- Diagnosis. MRI.
- Treatment. Surgery (primary) +/- radiation therapy.
- Mortality. Malignant nerve sheath tumor was the main cause of death (60%) in a study of 1895 patients with NF-1 from France in the time period 1980-2006 indicated excess mortality in NF-1 patients compared to the general population.[20] The cause of death was available for 58 (86.6%) patients. The study found excess mortality occurred among patients aged 10 to 40 years. Significant excess mortality was found in both males and females.
Cause
Neurofibromin 1 gene
NF-1 is a microdeletion syndrome caused by a mutation of a gene located on chromosomal segment 17q11.2 on the long arm of chromosome 17 which encodes a protein known as neurofibromin[21] (not to be confused with the disorder itself) which plays a role in cell signaling.[22][23] The Neurofibromin 1 gene is a negative regulator of the Ras oncogene signal transduction pathway. It stimulates the GTPase activity of Ras. It shows greater affinity for RAS p21 protein activator 1, but lower specific activity. The mRNA for this gene is subject to RNA editing (CGA->UGA->Arg1306Term) resulting in premature translation termination. Alternatively spliced transcript variants encoding different isoforms have also been described for this gene.
In 1989, through linkage and cross over analyses, neurofibromin was localized to chromosome 17.[24] It was localized to the long arm of chromosome 17 by chance when researchers discovered chromosome exchanges between chromosome 17 with chromosome 1 and 22.[24] This exchange of genetic material presumably caused a mutation in the neurofibromin gene, leading to the NF1 phenotype. Two recurrent microdeletion types with microdeletion breakpoints located in paralogous regions flanking NF1 (proximal NF1-REP-a and distal NF1-REP-c for the 1.4 Mb type-1 microdeletion, and SUZ12 and SUZ12P for the 1.2 Mb type-2 microdeletion), are found in most cases.[25]
Structure of the Neurofibromin gene
The Neurofibromin gene was soon sequenced and found to be 350,000 base pairs in length.[26] However, the protein is 2818 amino acids long leading to the concept of splice variants.[27] For example, exon 9a, 23a and 48a are expressed in the neurons of the forebrain, muscle tissues and adult neurons respectively.[27]
Homology studies have shown that neurofibromin is 30% similar to proteins in the GTPase Activating Protein (GAP) Family.[26] This homologous sequence is in the central portion of neurofibromin and being similar to the GAP family is recognized as a negative regulator of the Ras kinase.[28]
Additionally, being such a large protein, more active domains of the protein have been identified. One such domain interacts with the protein adenylyl cyclase,[29] and a second with collapsin response mediator protein.[30] Together, likely with domains yet to be discovered, neurofibromin regulates many of the pathways responsible for overactive cell proliferation, learning impairments, skeletal defects and plays a role in neuronal development.[31]
Inheritance and spontaneous mutation
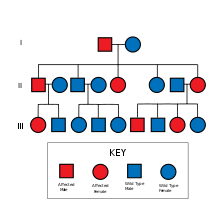
The mutant gene is transmitted with an autosomal dominant pattern of inheritance, but up to 50% of NF-1 cases arise due to spontaneous mutation. The incidence of NF-1 is about 1 in 3500 live births.[32]
Related medical conditions
Mutations in the NF1 gene have been linked to NF-1, Juvenile myelomonocytic leukemia and Watson syndrome. A condition with a separate gene mutation but similar Café au lait spots is Legius syndrome which has a mutation on the SPRED1 gene.
Diagnosis
Prenatal testing
Prenatal testing may be used to identify the existence of NF-1 in the fetus. For embryos produced via in vitro fertilisation, it is possible via preimplantation genetic diagnosis to screen for NF-1.[33]
Chorionic villus sampling or amniocentesis can be used to detect NF-1 in the fetus.[34]
Post-natal testing
The National Institutes of Health (NIH) has created specific criteria for the diagnosis of NF-1. Two of these seven "Cardinal Clinical Features" are required for positive diagnosis.[35] There is practical flowchart to distinguish between NF1, NF2 and schwannomatosis.[36]
- Six or more café-au-lait spots over 5 mm in greatest diameter in pre-pubertal individuals and over 15 mm in greatest diameter in post-pubertal individuals. Note that multiple café-au-lait spots alone are not a definitive diagnosis of NF-1 as these spots can be caused by a number of other conditions.
- Two or more neurofibromas of any type or 1 plexiform neurofibroma
- Freckling in the axillary (Crowe sign) or inguinal regions
- Optic glioma
- Two or more Lisch nodules (pigmented iris hamartomas)
- A distinctive osseous lesion such as sphenoid dysplasia, or thinning of the long bone cortex with or without pseudarthrosis.
- A first degree relative (parent, sibling, or offspring) with NF-1 by the above criteria.
Prognosis
NF-1 is a progressive and diverse condition, making the prognosis difficult to predict. The NF-1 gene mutations manifest the disorder differently even amongst people of the same family. This phenomenon is called variable expressivity. For example, some individuals have no symptoms, while others may have a manifestation that is rapidly more progressive and severe.
For many NF-1 patients, a primary concern is the disfigurement caused by cutaneous/dermal neurofibromas, pigmented lesions, and the occasional limb abnormalities. However, there are many more severe complications caused by NF-1, although most of them are quite rare. Many NF patients live perfectly normal and uninterrupted lives.
Treatment
There is no cure for the disorder itself. Instead, people with neurofibromatosis are followed by a team of specialists to manage symptoms or complications. In progress and recently concluded medical studies on NF-1 can be found by searching the official website of the National Institutes of Health.
See also
External links
- Understanding NF1, Harvard Medical School
- GeneReviews/NCBI/NIH/UW entry on Neurofibromatosis 1
- GeneReviews/NIH/NCBI/UW entry on Legius syndrome SPRED1 Sprouty-related, EVH1 domain-containing protein 1
- NF KONTAKT.be (a nonprofit organization providing information and resources for families, Schools and Health Care workers dealing with NF1, NF2, and tumour-related neurofibromatosis in Belgium and providing awareness and support of Neurofibromatosis in Europe)
References
- ^ Costa, R. M.; Silva, A. J. (2002). "Molecular and cellular mechanisms underlying the cognitive deficits associated with neurofibromatosis 1". Journal of child neurology. 17 (8): 622–626, discussion 626–9, 626–51. doi:10.1177/088307380201700813. PMID 12403561.
- ^ Legendre, Claire-Marie; Catherine Charpentier-Côté; Régen Drouin; Chantal Bouffard (February 9, 2011). Skoulakis, Efthimios (ed.). "Neurofibromatosis Type 1 and the "Elephant Man's" Disease: The Confusion Persists: An Ethnographic Study". PLoS ONE. 6 (2): e16409. doi:10.1371/journal.pone.0016409. PMC 3036577. PMID 21347399.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ "Neurofibromatosis 1: Current Issues in Diagnosis, Therapy, and Patient Management", by David Viskochil MD PhD, Mountain States Genetic Foundation, Denver 2010
- ^ "Current Therapies for Neurofibromatosis Type 1", by Laura Klesse MD PhD, Mountain States Genetic Foundation, Denver 2010
- ^ "Neurofibromatosis, giant cafe-au-lait spot". AllRefer.com Health. Retrieved 2010-07-27.
- ^ MedlinePlus Encyclopedia: Optic glioma
- ^ Hyman SL, Shores A, North KN (October 2005). "The nature and frequency of cognitive deficits in children with neurofibromatosis type 1". Neurology. 65 (7): 1037–44. doi:10.1212/01.wnl.0000179303.72345.ce. PMID 16217056.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Hyman SL, Gill DS, Shores EA; et al. (April 2003). "Natural history of cognitive deficits and their relationship to MRI T2-hyperintensities in NF1". Neurology. 60 (7): 1139–45. doi:10.1212/01.WNL.0000055090.78351.C1. PMID 12682321.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Thompson HL, Viskochil DH, Stevenson DA, Chapman KL (February 2010). "Speech-language characteristics of children with neurofibromatosis type 1". Am. J. Med. Genet. A. 152A (2): 284–90. doi:10.1002/ajmg.a.33235. PMID 20101681.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ van der Vaart T, van Woerden GM, Elgersma Y, de Zeeuw CI, Schonewille M (June 2011). "Motor deficits in neurofibromatosis type 1 mice: the role of the cerebellum". Genes Brain Behav. 10 (4): 404–9. doi:10.1111/j.1601-183X.2011.00685.x. PMID 21352477.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Clinical trial number NCT00352599 for "Trial to Evaluate the Safety of Lovastatin in Individuals With Neurofibromatosis Type I (NF1)" at ClinicalTrials.gov
- ^ Krab LC, de Goede-Bolder A, Aarsen FK; et al. (July 2008). "Effect of simvastatin on cognitive functioning in children with neurofibromatosis type 1: a randomized controlled trial". JAMA. 300 (3): 287–94. doi:10.1001/jama.300.3.287. PMC 2664742. PMID 18632543.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ van der Vaart T, Plasschaert E, Rietman AB; et al. (November 2013). "Simvastatin for cognitive deficits and behavioural problems in patients with neurofibromatosis type 1 (NF1-SIMCODA): a randomised, placebo-controlled trial". Lancet Neurol. 12 (11): 1076–83. doi:10.1016/S1474-4422(13)70227-8. PMID 24090588.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Friedrich, Reinhard. "Resection of small plexiform neurofibromas in neurofibromatosis type 1 children". World Journal of Surgical Oncology. Retrieved March 10, 2015.
- ^ a b Korf, BR (26 March 1999). "Plexiform neurofibromas". American journal of medical genetics. 89 (1): 31–7. PMID 10469434.
- ^ Vivarelli R, Grosso S, Calabrese F; et al. (May 2003). "Epilepsy in neurofibromatosis 1". J. Child Neurol. 18 (5): 338–42. doi:10.1177/08830738030180050501. PMID 12822818.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Listernick, R; Charrow, J; Gutmann, DH (26 March 1999). "Intracranial gliomas in neurofibromatosis type 1". American journal of medical genetics. 89 (1): 38–44. PMID 10469435.
- ^ Johnson NS, Saal HM, Lovell AM, Schorry EK (June 1999). "Social and emotional problems in children with neurofibromatosis type 1: evidence and proposed interventions". J. Pediatr. 134 (6): 767–72. doi:10.1016/S0022-3476(99)70296-9. PMID 10356149.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Matsui, I; Tanimura, M; Kobayashi, N; Sawada, T; Nagahara, N; Akatsuka, J (1 November 1993). "Neurofibromatosis type 1 and childhood cancer". Cancer. 72 (9): 2746–54. doi:10.1002/1097-0142(19931101)72:9<2746::AID-CNCR2820720936>3.0.CO;2-W. PMID 8402499.
- ^ Duong, Tu; Sbidian, Emilie; Valeyrie-Allanore, Laurence; Vialette, Cédric; Ferkal, Salah; Hadj-Rabia, Smaïl; Glorion, Christophe; Lyonnet, Stanislas; Zerah, Michel; Kemlin, Isabelle; Rodriguez, Diana; Bastuji-Garin, Sylvie; Wolkenstein, Pierre (2011). "Mortality Associated with Neurofibromatosis 1: A Cohort Study of 1895 Patients in 1980-2006 in France". Orphanet Journal of Rare Diseases. 6: 18. doi:10.1186/1750-1172-6-18. PMC 3095535. PMID 21542925.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Wallace, MR; Marchuk, DA; Andersen, LB; Letcher, R; Odeh, HM; Saulino, AM; Fountain, JW; Brereton, A; Nicholson, J; Mitchell, AL (13 July 1990). "Type 1 neurofibromatosis gene: identification of a large transcript disrupted in three NF1 patients". Science (New York, N.Y.). 249 (4965): 181–6. doi:10.1126/science.2134734. PMID 2134734.
- ^ "neurofibromin 1" GeneCards
- ^ "Human Gene NF1 (uc002hgf.1) Description and Page Index"
- ^ a b Goldberg NS, Collins FS (November 1991). "The hunt for the neurofibromatosis gene". Arch Dermatol. 127 (11): 1705–7. doi:10.1001/archderm.1991.01680100105014. PMID 1952978.
- ^ Pasmant, E; Sabbagh, A; Spurlock, G; Laurendeau, I; Grillo, E; Hamel, MJ; Martin, L; Barbarot, S; Leheup, B; Rodriguez, D; Lacombe, D; Dollfus, H; Pasquier, L; Isidor, B; Ferkal, S; Soulier, J; Sanson, M; Dieux-Coeslier, A; Bièche, I; Parfait, B; Vidaud, M; Wolkenstein, P; Upadhyaya, M; Vidaud, D; members of the NF France, Network (June 2010). "NF1 microdeletions in neurofibromatosis type 1: from genotype to phenotype". Human mutation. 31 (6): E1506-18. PMID 20513137.
- ^ a b Marchuk DA, Saulino AM, Tavakkol R; et al. (December 1991). "cDNA cloning of the type 1 neurofibromatosis gene: complete sequence of the NF1 gene product". Genomics. 11 (4): 931–40. doi:10.1016/0888-7543(91)90017-9. PMID 1783401.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ a b Gutmann DH, Giovannini M (2002). "Mouse models of neurofibromatosis 1 and 2". Neoplasia. 4 (4): 279–90. doi:10.1038/sj.neo.7900249. PMC 1531708. PMID 12082543.
- ^ Feldkamp MM, Angelov L, Guha A (February 1999). "Neurofibromatosis type 1 peripheral nerve tumors: aberrant activation of the Ras pathway". Surg Neurol. 51 (2): 211–8. doi:10.1016/S0090-3019(97)00356-X. PMID 10029430.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Hannan F, Ho I, Tong JJ, Zhu Y, Nurnberg P, Zhong Y (April 2006). "Effect of neurofibromatosis type I mutations on a novel pathway for adenylyl cyclase activation requiring neurofibromin and Ras". Hum. Mol. Genet. 15 (7): 1087–98. doi:10.1093/hmg/ddl023. PMC 1866217. PMID 16513807.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Ozawa T, Araki N, Yunoue S; et al. (November 2005). "The neurofibromatosis type 1 gene product neurofibromin enhances cell motility by regulating actin filament dynamics via the Rho-ROCK-LIMK2-cofilin pathway". J. Biol. Chem. 280 (47): 39524–33. doi:10.1074/jbc.M503707200. PMID 16169856.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - ^ Le LQ, Parada LF (July 2007). "Tumor microenvironment and neurofibromatosis type I: connecting the GAPs". Oncogene. 26 (32): 4609–16. doi:10.1038/sj.onc.1210261. PMC 2760340. PMID 17297459.
- ^ Online Mendelian Inheritance in Man (OMIM): NEUROFIBROMATOSIS, TYPE I; NF1 - 162200
- ^ "British couple successfully screens out genetic disorder using NHS-funded PGD" by Antony Blackburn-Starza, June 9, 2008, BioNews 461
- ^ "Are there any prenatal tests for the neurofibromatoses?"
- ^ Huson, Susan Mary; Hughes, Richard Anthony Cranmer (1994). The neurofibromatoses: a pathogenetic and clinical overview. London: Chapman & Hall. 1.3.2:9. ISBN 0-412-38920-7.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ^ Rodrigues, Luiz Oswaldo Carneiro; Batista, Pollyanna Barros; Goloni-Bertollo, Eny Maria; Souza-Costa, Danielle de; Eliam, Lucas; Eliam, Miguel; Cunha, Karin Soares Gonçalves; Darrigo Junior, Luiz Guilherme; Ferraz Filho, José Roberto Lopes; Geller, Mauro; Gianordoli-Nascimento, Ingrid F.; Madeira, Luciana Gonçalves; Malloy-Diniz, Leandro Fernandes; Mendes, Hérika Martins; Miranda, Débora Marques de; Pavarino, Erika Cristina; Baptista-Pereira, Luciana; Rezende, Nilton A.; Rodrigues, Luíza de Oliveira; Silva, Carla Menezes da; Souza, Juliana Ferreira de; Souza, Márcio Leandro Ribeiro de; Stangherlin, Aline; Valadares, Eugênia Ribeiro; Vidigal, Paula Vieira Teixeira (2014). "Neurofibromatoses: part 1 – diagnosis and differential diagnosis". Arquivos de Neuro-Psiquiatria. 72 (3): 241–50. doi:10.1590/0004-282X20130241. PMID 24676443.
