Swine influenza: Difference between revisions
Divert details to current 2009 swine flu outbreak and not this page. |
→1976 U.S. outbreak: expand |
||
| Line 376: | Line 376: | ||
{{main|1976 swine flu outbreak}} |
{{main|1976 swine flu outbreak}} |
||
On February 5, 1976, in the United States an army recruit at [[Fort Dix]] said he felt tired and weak. He died the next day and four of his fellow soldiers were later hospitalized. Two weeks after his death, health officials announced that |
On February 5, 1976, in the United States an army recruit at [[Fort Dix]] said he felt tired and weak. He died the next day and four of his fellow soldiers were later hospitalized. Two weeks after his death, health officials announced that the cause of death was a new strain of swine flu. The strain, a variant of [[H1N1]], is known as <!-- start -->A/New Jersey/1976 (H1N1)<!-- end -->. It was detected only from January 19 to February 9 and did not spread beyond Fort Dix.<ref name="Gaydos+2006">{{cite journal |
||
| author = Gaydos JC, Top FH, Hodder RA, Russell PK |
|||
| title = Swine influenza a outbreak, Fort Dix, New Jersey, 1976 |
|||
| journal = Emerging Infectious Diseases |
|||
| volume = 12 |
|||
| issue = 1 |
|||
| pages = 23–8 |
|||
| year = 2006 |
|||
| month = January |
|||
| pmid = 16494712 |
|||
| doi = |
|||
| url = http://www.cdc.gov/ncidod/EID/vol12no01/05-0965.htm |
|||
| issn = |
|||
}}</ref> |
|||
[[File:FordSwineFluShot1.jpg|thumb|right|President Ford receives swine flu vaccination]] |
[[File:FordSwineFluShot1.jpg|thumb|right|President Ford receives swine flu vaccination]] |
||
This new strain appeared to be closely related to the strain involved in the 1918 flu pandemic. Alarmed public-health officials decided action must be taken to head off another major [[pandemic]], and urged President [[Gerald Ford]] that every person in the U.S. be vaccinated for the disease.<ref>{{cite news |first=Harold M. |last=Schmeck |authorlink= |coauthors= |title=Ford Urges Flu Campaign To Inoculate Entire U.S. |url=http://select.nytimes.com/gst/abstract.html?res=F50A17FD3C5A167493C7AB1788D85F428785F9 |work=The New York Times |publisher= |date=March 25, 1976 |accessdate= }}</ref> |
This new strain appeared to be closely related to the strain involved in the 1918 flu pandemic. Moreover, the ensuing increased surveillance uncovered another strain in circulation in the U.S.: [[H3N2|A/Victoria/75 (H3N2)]] spread simultaneously, also caused illness, and persisted until March.<ref name="Gaydos+2006"/> Alarmed public-health officials decided action must be taken to head off another major [[pandemic]], and urged President [[Gerald Ford]] that every person in the U.S. be vaccinated for the disease.<ref>{{cite news |first=Harold M. |last=Schmeck |authorlink= |coauthors= |title=Ford Urges Flu Campaign To Inoculate Entire U.S. |url=http://select.nytimes.com/gst/abstract.html?res=F50A17FD3C5A167493C7AB1788D85F428785F9 |work=The New York Times |publisher= |date=March 25, 1976 |accessdate= }}</ref> |
||
The [[vaccination]] program was plagued by delays and public relations problems.<ref>Richard E. Neustadt and Harvey V. Fineberg. (1978). [http://www.nap.edu/catalog.php?record_id=12660 The Swine Flu Affair: Decision-Making on a Slippery Disease]. ''National Academies Press''.</ref> On October 1, 1976, the immunization program began and by October 11, approximately 40 million people, or about 24% of the population, had received swine flu immunizations. That same day, three senior citizens died soon after receiving their swine flu shots and there was a media outcry linking the deaths to the immunizations, despite the lack of positive proof. According to science writer Patrick Di Justo, however, by the time the truth was known — that the deaths were not proven to be related to the vaccine — it was too late. "The government had long feared mass panic about swine flu — now they feared mass panic about the swine flu vaccinations." This became a strong setback to the program.<ref name=DiJusto>[http://www.salon.com/env/feature/2009/04/28/1976_swine_flu/ "The Last Great Swine Flu Epidemic"], ''Salon.com'', April 28, 2009.</ref> |
The [[vaccination]] program was plagued by delays and public relations problems.<ref>Richard E. Neustadt and Harvey V. Fineberg. (1978). [http://www.nap.edu/catalog.php?record_id=12660 The Swine Flu Affair: Decision-Making on a Slippery Disease]. ''National Academies Press''.</ref> On October 1, 1976, the immunization program began and by October 11, approximately 40 million people, or about 24% of the population, had received swine flu immunizations. That same day, three senior citizens died soon after receiving their swine flu shots and there was a media outcry linking the deaths to the immunizations, despite the lack of positive proof. According to science writer Patrick Di Justo, however, by the time the truth was known — that the deaths were not proven to be related to the vaccine — it was too late. "The government had long feared mass panic about swine flu — now they feared mass panic about the swine flu vaccinations." This became a strong setback to the program.<ref name=DiJusto>[http://www.salon.com/env/feature/2009/04/28/1976_swine_flu/ "The Last Great Swine Flu Epidemic"], ''Salon.com'', April 28, 2009.</ref> |
||
Revision as of 16:10, 1 May 2009
For details of the current outbreak of Swine Flu, see 2009 swine flu outbreak. |
| Swine influenza | |
|---|---|
| Specialty | Pulmonology, infectious diseases |
| Influenza (flu) |
|---|
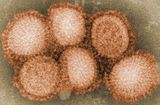 |

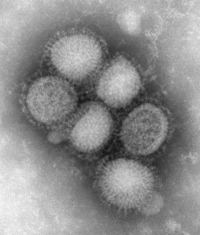
Swine influenza (also called swine flu, hog flu, and pig flu) refers to influenza caused by any strain of the influenza virus endemic in pigs (swine). Strains endemic in swine are called swine influenza virus (SIV).[1]
Of the three genera of human flu, two are endemic also in swine: Influenzavirus A is common and Influenzavirus C is rare.[2] Influenzavirus B has not been reported in swine. Within Influenzavirus A and Influenzavirus C, the strains endemic to swine and humans are largely distinct.
Swine flu is common in swine in the midwestern United States (and occasionally in other states), Mexico, Canada, South America, Europe (including the United Kingdom, Sweden, and Italy), Kenya, China, Japan, Taiwan, and other parts of eastern Asia.[1]
Swine flu is rare in humans. People who work with swine, especially people with intense exposures, are at risk of catching swine influenza if the swine carry a strain able to infect humans. However, these strains infrequently circulate between humans as SIV rarely mutates into a form able to pass easily from human to human. In humans, the symptoms of swine flu are similar to those of influenza and of influenza-like illness in general, namely chills, fever, sore throat, muscle pains, severe headache, coughing, weakness and general discomfort.
The 2009 flu outbreak in humans that is widely known as "swine flu" is due to a new strain of influenza A virus subtype H1N1 that derives by reassortment from one strain of human influenza virus, one strain of avian influenza virus, and two separate strains of swine influenza virus. The origins of this new strain are unknown, and the World Organization for Animal Health (OIE) reports that this strain has not been isolated in swine.[3] It passes with apparent ease from human to human, an ability attributed to an as-yet unidentified mutation.[4] The strain in most cases causes only mild symptoms and the infected person makes a full recovery without requiring medical attention and without the use of antiviral medicines.[5] The World Health Organization has stated that symptoms may even be less severe than seasonal influenza symptoms.
Classification
SIV strains isolated to date have been classified either as Influenzavirus C or one of the various subtypes of the genus Influenzavirus A.[6]
Influenza C
Influenza A
Swine influenza is known to be caused by influenza A subtypes H1N1,[7] H1N2,[7] H3N1,[8] H3N2,[7] and H2N3.[9]
In swine, three influenza A virus subtypes (H1N1, H3N2, and H1N2) are circulating throughout the world. In the United States, the H1N1 subtype was exclusively prevalent among swine populations before 1998; however, since late August 1998, H3N2 subtypes have been isolated from pigs. As of 2004, H3N2 virus isolates in US swine and turkey stocks were triple reassortants, containing genes from human (HA, NA, and PB1), swine (NS, NP, and M), and avian (PB2 and PA) lineages.[10]
History

The H1N1 form of swine flu is one of the descendants of the Spanish flu that caused a devastating pandemic in humans in 1918–1919.[12][13] As well as persisting in pigs, the descendants of the 1918 virus have also circulated in humans through the 20th century, contributing to the normal seasonal epidemics of influenza.[12] However, direct transmission from pigs to humans is rare, with only 12 cases in the U.S. since 2005.[14]
The influenza virus constantly changes form, thereby eluding the protective antibodies that people may have developed in response to previous exposures to influenza or to influenza vaccines. Every two or three years the virus undergoes minor changes. But at intervals of roughly a decade, after the bulk of the world's population has developed some level of resistance to these minor changes, it undergoes a major change that enables it to easily infect populations around the world, often infecting hundreds of millions of people whose antibody defenses are unable to resist it.[15] The influenza virus has also been known to change form over a much shorter period of time. For instance, during the Spanish flu pandemic, the initial wave of the disease was relatively mild, while the second wave of the disease a year later was highly lethal.[13]
In 1957, an Asian flu pandemic infected some 45 million Americans and killed 70,000. It caused about 2 million deaths globally.[16] Eleven years later, lasting from 1968 to 1969, the Hong Kong flu pandemic afflicted 50 million Americans and caused 33,000 deaths, costing approximately $3.9 billion. In 1976, about 500 soldiers became infected with swine flu over a period of a few weeks. However, by the end of the month investigators found that the virus had "mysteriously disappeared."[13] In the U.S. during an average year, there are approximately 50 million cases of "normal" flu leading to around 36,000 deaths,[17] mostly to extremely young, old, or frail persons, with a large percentage of those due to complications such as pneumonia.
Medical researchers worldwide, recognizing that the swine flu virus might again mutate into something as deadly as the Spanish flu, are carefully watching the latest 2009 outbreak of swine flu and making contingency plans for a possible global pandemic. Several countries took precautionary measures to reduce the chances for a global pandemic of the disease.[18]
Signs and symptoms
In swine
In humans

See also: The Centers for Disease Control and Prevention (CDC): Symptoms of Swine Flu in YouTube
According to the Centers for Disease Control and Prevention (CDC), in humans the symptoms of swine flu are similar to those of influenza and of influenza-like illness in general. Symptoms include fever, cough, sore throat, body aches, headache, chills and fatigue. The 2009 outbreak has shown an increased percentage of patients reporting diarrhea and vomiting.[20]
Because these symptoms are not specific to swine flu, a differential diagnosis of probable swine flu requires not only symptoms but also a high likelihood of swine flu due to the person's recent history. For example, during the 2009 swine flu outbreak in the United States, CDC advised physicians to "consider swine influenza infection in the differential diagnosis of patients with acute febrile respiratory illness who have either been in contact with persons with confirmed swine flu, or who were in one of the five U.S. states that have reported swine flu cases or in Mexico during the 7 days preceding their illness onset."[21] A diagnosis of confirmed swine flu requires laboratory testing of a respiratory sample (a simple nose and throat swab).[21]
Pathophysiology
Influenza viruses bind through hemagglutinin onto sialic acid sugars on the surfaces of epithelial cells; typically in the nose, throat and lungs of mammals and intestines of birds (Stage 1 in infection figure).[22]
Swine flu in humans
People who work with poultry and swine, especially people with intense exposures, are at increased risk of zoonotic infection with influenza virus endemic in these animals, and constitute a population of human hosts in which zoonosis and reassortment can co-occur.[24] Transmission of influenza from swine to humans who work with swine was documented in a small surveillance study performed in 2004 at the University of Iowa.[25] This study among others forms the basis of a recommendation that people whose jobs involve handling poultry and swine be the focus of increased public health surveillance.[24] The 2009 swine flu outbreak is an apparent reassortment of several strains of influenza A virus subtype H1N1, including a strain endemic in humans and two strains endemic in pigs, as well as an avian influenza.[26]
Interaction with H5N1
Avian influenza virus H3N2 is endemic in pigs in China and has been detected in pigs in Vietnam, increasing fears of the emergence of new variant strains.[27] Health experts[who?] say pigs can carry human influenza viruses, which can combine (i.e. exchange homologous genome sub-units by genetic reassortment) with H5N1, passing genes and mutating into a form which can pass easily among humans.[28] H3N2 evolved from H2N2 by antigenic shift.[29] In August 2004, researchers in China found H5N1 in pigs.[30]
Nature magazine reported that Chairul Nidom, a virologist at Airlangga University's tropical disease center in Surabaya, East Java, conducted a survey of swine infections with H5N1 in 2005. He tested the blood of 10 apparently healthy pigs housed near poultry farms in West Java where avian flu had broken out. Five of the pig samples contained the H5N1 virus. The Indonesian government has since found similar results in the same region. Additional tests of 150 pigs outside the area were negative.[31][32]
The CDC reports that the symptoms and transmission of the swine flu from human to human is much like that of seasonal flu. Common symptoms include fever, lethargy, lack of appetite and coughing, while runny nose, sore throat, nausea, vomiting and diarrhea have also been reported.[33]
Prevention
Prevention of swine influenza has three components: prevention in swine, prevention of transmission to humans, and prevention of its spread among humans.
Prevention in swine
Methods of preventing the spread of influenza among swine include facility management, herd management, and vaccination. Because much of the illness and death associated with swine flu involves secondary infection by other pathogens, control strategies that rely on vaccination may be insufficient.
Control of swine influenza by vaccination has become more difficult in recent decades, as the evolution of the virus has resulted in inconsistent responses to traditional vaccines. Standard commercial swine flu vaccines are effective in controlling the infection when the virus strains match enough to have significant cross-protection, and custom (autogenous) vaccines made from the specific viruses isolated are created and used in the more difficult cases.[34][35] Present vaccination strategies for SIV control and prevention in swine farms, typically include the use of one of several bivalent SIV vaccines commercially available in the United States. Of the 97 recent H3N2 isolates examined, only 41 isolates had strong serologic cross-reactions with antiserum to three commercial SIV vaccines. Since the protective ability of influenza vaccines depends primarily on the closeness of the match between the vaccine virus and the epidemic virus, the presence of nonreactive H3N2 SIV variants suggests that current commercial vaccines might not effectively protect pigs from infection with a majority of H3N2 viruses.[36][37] The United States Department of Agriculture researchers say that while pig vaccination keeps pigs from getting sick, it does not block infection or shedding of the virus.[38]
Facility management includes using disinfectants and ambient temperature to control virus in the environment. The virus is unlikely to survive outside living cells for >2 wk except in cold (but above freezing) conditions, and it is readily inactivated by disinfectants.[1]
Herd management includes not adding pigs carrying influenza to herds that have not been exposed to the virus. The virus survives in healthy carrier pigs for up to 3 months and can be recovered from them between outbreaks. Carrier pigs are usually responsible for the introduction of SIV into previously uninfected herds and countries. After an outbreak, as immunity in exposed pigs wanes, new outbreaks of the same strain can occur.[1]
Prevention of transmission to humans
This section needs expansion. You can help by adding to it. (April 2009) |
The transmission from swine to human is believed to occur mainly in swine farms where farmers are in close contact with live pigs. Although strains of swine influenza are usually not able to infect humans this may occasionally happen, so farmers and veterinarians are encouraged to use a face mask when dealing with infected animals. The use of vaccines on swine to prevent their infection is a major method of limiting swine to human transmission.
Prevention of spread in humans
Influenza spreads between humans through coughing or sneezing and people touching something with the virus on it and then touching their own nose or mouth.[39] Swine flu cannot be spread by pork products, since the virus is not transmitted through food.[39] The swine flu in humans is most contagious during the first five days of the illness although some people, most commonly children, can remain contagious for up to ten days. Diagnosis can be made by sending a specimen, collected during the first five days for analysis.[40]
Recommendations to prevent spread of the virus among humans include using standard infection control against influenza. This includes frequent washing of hands with soap and water or with alcohol-based hand sanitizers, especially after being out in public.[41] Although the current trivalent influenza vaccine is unlikely to provide protection against the new 2009 H1N1 strain,[42] vaccines against the new strain are being developed and could be ready as early as June 2009.[43]
Experts agree that hand-washing can help prevent viral infections, including ordinary influenza and the swine flu virus. Influenza can spread in coughs or sneezes, but an increasing body of evidence shows small droplets containing the virus can linger on tabletops, telephones and other surfaces and be transferred via the fingers to the mouth, nose or eyes. Alcohol-based gel or foam hand sanitizers work well to destroy viruses and bacteria. Anyone with flu-like symptoms such as a sudden fever, cough or muscle aches should stay away from work or public transportation and should see a doctor to be tested.
Social distancing is another tactic. It means staying away from other people who might be infected and can include avoiding large gatherings, spreading out a little at work, or perhaps staying home and lying low if an infection is spreading in a community. Public health and other responsible authorities have action plans which social distancing actions to request or require depending on the severity of the outbreak.
Treatment
In swine
In humans
If a person becomes sick with swine flu, antiviral drugs can make the illness milder and make the patient feel better faster. They may also prevent serious flu complications. For treatment, antiviral drugs work best if started soon after getting sick (within 2 days of symptoms). Beside antivirals, palliative care, at home or in the hospitals, focuses on controlling fevers and maintaining fluid balance. The U.S. Centers for Disease Control and Prevention recommends the use of Tamiflu (oseltamivir) or Relenza (zanamivir) for the treatment and/or prevention of infection with swine influenza viruses, however, the majority of people infected with the virus make a full recovery without requiring medical attention or antiviral drugs.[44] The virus isolates in the 2009 outbreak have been found resistant to amantadine and rimantadine.[45]
In the U.S., on April 27, 2009, the FDA issued Emergency Use Authorizations to make available Relenza and Tamiflu antiviral drugs to treat the swine influenza virus in cases for which they are currently unapproved. The agency issued these EUAs to allow treatment of patients younger than the current approval allows and to allow the widespread distribution of the drugs, including by non-licensed volunteers.[46]
Epidemiology : outbreaks in swine
2007 Philippine outbreak
On August 20, 2007 Department of Agriculture officers investigated the outbreak (epizootic) of swine flu in Nueva Ecija and Central Luzon, Philippines. The mortality rate is less than 10% for swine flu, unless there are complications like hog cholera. On July 27, 2007, the Philippine National Meat Inspection Service (NMIS) raised a hog cholera "red alert" warning over Metro Manila and 5 regions of Luzon after the disease spread to backyard pig farms in Bulacan and Pampanga, even if these tested negative for the swine flu virus.[47][48]
Epidemiology: Outbreaks in humans
Swine flu has been reported numerous times as a zoonosis in humans, usually with limited distribution, rarely with a widespread distribution. The 1918 flu pandemic in humans was associated with H1N1,[12] thus may reflect a zoonosis either from swine to humans or from humans to swine. Evidence available from that time is not sufficient to resolve this question. The "Spanish" influenza pandemic of 1918–19 infected one third of the world's population (or around 500 million persons at that time) and caused around 50 million deaths.[12]
1976 U.S. outbreak
On February 5, 1976, in the United States an army recruit at Fort Dix said he felt tired and weak. He died the next day and four of his fellow soldiers were later hospitalized. Two weeks after his death, health officials announced that the cause of death was a new strain of swine flu. The strain, a variant of H1N1, is known as A/New Jersey/1976 (H1N1). It was detected only from January 19 to February 9 and did not spread beyond Fort Dix.[49]

This new strain appeared to be closely related to the strain involved in the 1918 flu pandemic. Moreover, the ensuing increased surveillance uncovered another strain in circulation in the U.S.: A/Victoria/75 (H3N2) spread simultaneously, also caused illness, and persisted until March.[49] Alarmed public-health officials decided action must be taken to head off another major pandemic, and urged President Gerald Ford that every person in the U.S. be vaccinated for the disease.[50]
The vaccination program was plagued by delays and public relations problems.[51] On October 1, 1976, the immunization program began and by October 11, approximately 40 million people, or about 24% of the population, had received swine flu immunizations. That same day, three senior citizens died soon after receiving their swine flu shots and there was a media outcry linking the deaths to the immunizations, despite the lack of positive proof. According to science writer Patrick Di Justo, however, by the time the truth was known — that the deaths were not proven to be related to the vaccine — it was too late. "The government had long feared mass panic about swine flu — now they feared mass panic about the swine flu vaccinations." This became a strong setback to the program.[15]
There were reports of Guillain-Barré syndrome, a paralyzing neuromuscular disorder, affecting some people who had received swine flu immunizations. This syndrome is a rare side-effect of modern influenza vaccines, with an incidence of about one case per million vaccinations.[52] As a result, Di Justo writes that "the public refused to trust a government-operated health program that killed old people and crippled young people." In total, less than 33 percent of the population had been immunized by the end of 1976. The National Influenza Immunization Program was effectively halted on Dec. 16.
Overall, about 500 cases of Guillain-Barré syndrome (GBS), resulting in death from severe pulmonary complications for 25 people, which, according to Dr. P. Haber, were probably caused by an immunopathological reaction to the 1976 vaccine. Other influenza vaccines have not been linked to GBS, though caution is advised for certain individuals, particularly those with a history of GBS.[53][54] Still, as observed by a participant in the immunization program, the vaccine killed more Americans than the disease did.[55]
1988 swine flu outbreak
In September 1988, a swine flu virus killed one woman in Wisconsin, and infected at least hundreds of others. 32-year old Barbara Ann Wieners was eight months pregnant when she and her husband, Ed, became ill after visiting the hog barn at the Walworth County Fair. Barbara died eight days later, though doctors were able to induce labor and deliver a healthy daughter before she passed away. Her husband recovered from his symptoms.
Influenza-like illnesses were reportedly widespread among the pigs at the fair they had visited, and 76% of the swine exhibitors there tested positive for the swine flu antibody but no serious illnesses were detected among this group. Additional studies suggested between one and three health care personnel who had contact with the patient developed mild influenza-like illnesses with antibody evidence of swine flu infection.[56][57]
2009 flu outbreak
The new strain of swine influenza A (H1N1) involved in the 2009 flu outbreak in humans is a reassortment of several strains of influenza A virus subtype H1N1 that are, separately, endemic in humans, endemic in birds, and endemic in swine. Preliminary genetic characterization found that the hemagglutinin (HA) gene was similar to that of swine flu viruses present in United States pigs since 1999, but the neuraminidase (NA) and matrix protein (M) genes resembled versions present in European swine flu isolates. Viruses with this genetic makeup had not previously been found to be circulating in humans or pigs, but there is no formal national surveillance system to determine what viruses are circulating in pigs in the United States.[58] The origins of this new strain remain unknown.
The 2009 strain of swine influenza A (H1N1) has a more efficient human-to-human transmission than previous swine H1N1 strains. It is currently listed by the United States and World Health Organization as a Phase 5 pandemic virus.[59]
See also
References
- ^ a b c d "Swine influenza". The Merck Veterinary Manual. 2008. Retrieved April 30, 2009.
- ^ Heinen PP (15 September 2003). "Swine influenza: a zoonosis". Veterinary Sciences Tomorrow. ISSN 1569-0830.
Influenza B and C viruses are almost exclusively isolated from man, although influenza C virus has also been isolated from pigs and influenza B has recently been isolated from seals.
- ^ Maria Zampaglione (April 29, 2009). "Press Release: A/H1N1 influenza like human illness in Mexico and the USA: OIE statement". World Organisation for Animal Health. Retrieved April 29, 2009.
- ^ http://www.who.int/mediacentre/news/statements/2009/h1n1_20090427/en/index.html
- ^ http://www.who.int/csr/disease/swineflu/faq/en/index.html
- ^
Heinen PP (15 September 2003). "Swine influenza: a zoonosis". Veterinary Sciences Tomorrow. ISSN 1569-0830.
Influenza B and C viruses are almost exclusively isolated from man, although influenza C virus has also been isolated from pigs and influenza B has recently been isolated from seals.
- ^ a b c "Swine Influenza". Swine Diseases (Chest). Iowa State University College of Veterinary Medicine.
- ^
Shin JY, Song MS, Lee EH, Lee YM, Kim SY, Kim HK, Choi JK, Kim CJ, Webby RJ, Choi YK (2006). "Isolation and characterization of novel H3N1 swine influenza viruses from pigs with respiratory diseases in Korea". Journal of Clinical Microbiology. 44 (11): 3923–7. doi:10.1128/JCM.00904-06. PMID 16928961.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^
Ma W, Vincent AL, Gramer MR, Brockwell CB, Lager KM, Janke BH, Gauger PC, Patnayak DP, Webby RJ, Richt JA (26 December 2007). "Identification of H2N3 influenza A viruses from swine in the United States". Proc Nat Acad Sci USA. 104 (52): 20949–54. doi:10.1073/pnas.0710286104. PMC 2409247. PMID 18093945.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^
Yassine HM, Al-Natour MQ, Lee CW, Saif YM (2007). "Interspecies and intraspecies transmission of triple reassortant H3N2 influenza A viruses". Virol J. 28 (4): 129. doi:10.1186/1743-422X-4-129. PMC 2228287. PMID 18045494.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - ^ Palese P (2004). "Influenza: old and new threats". Nat. Med. 10 (12 Suppl): S82–7. doi:10.1038/nm1141. PMID 15577936.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ a b c d Taubenberger JK, Morens DM (2006). "1918 Influenza: the mother of all pandemics". Emerg Infect Dis. 12 (1): 15–22. PMID 16494711.
- ^ a b c "Soft evidence and hard sell". New York Times. 5 September 1976.
- ^ "U.S. pork groups urge hog farmers to reduce flu risk". Reuters. 26 April 2009.
- ^ a b "The Last Great Swine Flu Epidemic", Salon.com, April 28, 2009.
- ^ Q&A: Swine flu. BBC News. April 27, 2009.
- ^ http://www.cdc.gov/flu/about/qa/disease.htm
- ^ "World takes drastic steps to contain swine flu". 30 April 2009.
- ^ Centers for Disease Control and Prevention > Key Facts about Swine Influenza (Swine Flu) Retrieved on April 27, 2009.
- ^ "Swine Flu and You". CDC. 2009-04-26. Retrieved 2009-04-26.
- ^ a b Centers for Disease Control and Prevention (April 26, 2009). "CDC Health Update: Swine Influenza A (H1N1) Update: New Interim Recommendations and Guidance for Health Directors about Strategic National Stockpile Materiel". Health Alert Network. Retrieved April 27, 2009.
- ^ Wagner, R (2002). "Functional balance between haemagglutinin and neuraminidase in influenza virus infections". Reviews in Medical Virology. 12 (3): 159–66. doi:10.1002/rmv.352. PMID 11987141.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|journapi9juuj9il=ignored (help); Unknown parameter|month=ignored (help) - ^ International Committee on Taxonomy of Viruses. "The Universal Virus Database, version 4: Influenza A".
- ^ a b Gray GC, Kayali G (2009). "Facing pandemic influenza threats: the importance of including poultry and swine workers in preparedness plans". Poultry Science. 88 (4): 880–4. doi:10.3382/ps.2008-00335. PMID 19276439.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Gray GC, McCarthy T, Capuano AW, Setterquist SF, Olsen CW, Alavanja MC (2007). "Swine workers and swine influenza virus infections". Emerging Infectious Diseases. 13 (12): 1871–8. PMID 18258038.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ "Deadly new flu virus in US and Mexico may go pandemic". New Scientist. 2009-04-24. Retrieved 2009-04-26.
- ^ Yu, H. (2008). "Genetic evolution of swine influenza A (H3N2) viruses in China from 1970 to 2006". Journal of Clinical Microbiology. 46 (3): 1067. doi:10.1128/JCM.01257-07. PMID 18199784.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ "Bird flu and pandemic influenza: what are the risks?". UK Department of Health.
- ^ Lindstrom Stephen E, Cox Nancy J, Klimov Alexander (15 October 2004). "Genetic analysis of human H2N2 and early H3N2 influenza viruses, 1957–1972: evidence for genetic divergence and multiple reassortment events". Virology. 328 (1): 101–19. doi:10.1016/j.virol.2004.06.009. PMID 15380362.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ World Health Organization (28 October 2005). "H5N1 avian influenza: timeline" (PDF).
- ^ "Indonesian pigs have avian flu virus; bird cases double in China". University of Minnesota: Center for Infectious Disease Research & Policy. 27 May 2005. Retrieved 2009-04-26.
- ^ Roos Robert, ed. (31 March 2009). "H5N1 virus may be adapting to pigs in Indonesia". University of Minnesota: Center for Infectious Disease Research & Policy. Retrieved 2009-04-26. report on pigs as carriers.
- ^ "Q & A: Key facts about swine influenza (swine flu) - Symptoms". Centers for Disease Control and Prevention. 24 April 2009. Retrieved 2009-04-26.
- ^ "Swine flu virus turns endemic". National Hog Farmer. 15 September 2007.
- ^ "Swine". Custom Vaccines. Novartis.
- ^ Gramer Marie René, Lee Jee Hoon, Choi Young Ki, Goyal Sagar M, Joo Han Soo (July 2007). "Serologic and genetic characterization of North American H3N2 swine influenza A viruses". Canadian Journal of Veterinary Research. 71 (3): 201–206. PMID 1899866.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^
Myers KP, Olsen CW, Gray GC (2007). "Cases of swine influenza in humans: a review of the literature". Clin Infect Dis. 44 (8): 1084–8. doi:10.1086/512813. PMC 1973337. PMID 17366454.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ "Swine flu: The predictable pandemic?". 2009-04-29.
- ^ a b "Q & A: Key facts about swine influenza (swine flu) – Spread of Swine Flu". Centers for Disease Control and Prevention. 24 April 2009. Retrieved 2009-04-26.
- ^ "Q & A: Key facts about swine influenza (swine flu) – Diagnosis". Centers for Disease Control and Prevention. 24 April 2009. Retrieved 2009-04-26.
- ^ "CDC - Influenza (Flu) | Swine Influenza (Flu) Investigation". Cdc.gov. Retrieved 2009-04-27.
- ^ "Q & A: Key facts about swine influenza (swine flu) – Virus Strains". Centers for Disease Control and Prevention. 24 April 2009. Retrieved 2009-04-26.
- ^ Lauren Petty (April 28, 2009). "Swine Flu Vaccine Could Be Ready in 6 Weeks". NBC Connecticut. Retrieved April 28, 2009.
- ^ http://www.who.int/csr/disease/swineflu/faq/en/index.html
- ^ "Antiviral Drugs and Swine Influenza". Centers for Disease Control. Retrieved 2009-04-27.
- ^ FDA Authorizes Emergency Use of Influenza Medicines, Diagnostic Test in Response to Swine Flu Outbreak in Humans. FDA News, April 27, 2009.
- ^ "DA probes reported swine flu 'outbreak' in N. Ecija". Gmanews.tv. Retrieved 2009-04-25.
- ^ "Gov't declares hog cholera alert in Luzon". Gmanews.tv. Retrieved 2009-04-25.
- ^ a b Gaydos JC, Top FH, Hodder RA, Russell PK (2006). "Swine influenza a outbreak, Fort Dix, New Jersey, 1976". Emerging Infectious Diseases. 12 (1): 23–8. PMID 16494712.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Schmeck, Harold M. (March 25, 1976). "Ford Urges Flu Campaign To Inoculate Entire U.S." The New York Times.
{{cite news}}: Cite has empty unknown parameter:|coauthors=(help) - ^ Richard E. Neustadt and Harvey V. Fineberg. (1978). The Swine Flu Affair: Decision-Making on a Slippery Disease. National Academies Press.
- ^ Vellozzi C, Burwen DR, Dobardzic A, Ball R, Walton K, Haber P (2009). "Safety of trivalent inactivated influenza vaccines in adults: Background for pandemic influenza vaccine safety monitoring". Vaccine. 27 (15): 2114–2120. doi:10.1016/j.vaccine.2009.01.125. PMID 19356614.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^
Haber P, Sejvar J, Mikaeloff Y, Destefano F (2009). "Vaccines and Guillain-Barré syndrome". Drug Saf. 32 (4): 309–23. doi:10.2165/00002018-200932040-00005. PMID 19388722.
{{cite journal}}: Unknown parameter|doi_brokendate=ignored (|doi-broken-date=suggested) (help)CS1 maint: multiple names: authors list (link) - ^ "Influenza / Flu Vaccine". University of Illinois at Springfield. Retrieved 26 April 2009.
- ^ BBC: The World; April 28, 2009.
- ^ http://www.cdc.gov/swineflu/key_facts.htm Key Facts About Swine Flu (CDC).
- ^ Jason George (April 28, 2009). "Swine flu: Last U.S. swine flu death in 1988 in Wisconsin". Chicago Tribune.
- ^ "Swine influenza A (H1N1) infection in two children --- Southern California, March--April 2009". Morbidity and Mortality Weekly Report. Centers for Disease Control. 22 April 2009.
- ^ "WHO raises H1N1 Virus to Phase 5 -Pandemic Imminent". 2009-04-29.
Further reading
- Alexander DJ (1982). "Ecological aspects of influenza A viruses in animals and their relationship to human influenza: a review". J R Soc Med. 75 (10): 799–811. PMC 1438138. PMID 6752410.
{{cite journal}}: Unknown parameter|month=ignored (help)
- Hampson AW, Mackenzie JS (2006). "The influenza viruses". Med. J. Aust. 185 (10 Suppl): S39–43. PMID 17115950.
{{cite journal}}: Unknown parameter|month=ignored (help)
- Lipatov AS, Govorkova EA, Webby RJ; et al. (2004). "Influenza: emergence and control". J. Virol. 78 (17): 8951–9. doi:10.1128/JVI.78.17.8951-8959.2004. PMC 506949. PMID 15308692.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link)
- Van Reeth K (2007). "Avian and swine influenza viruses: our current understanding of the zoonotic risk". Vet. Res. 38 (2): 243–60. doi:10.1051/vetres:2006062. PMID 17257572.
- Webster RG, Bean WJ, Gorman OT, Chambers TM, Kawaoka Y (1992). "Evolution and ecology of influenza A viruses". Microbiol. Rev. 56 (1): 152–79. PMC 372859. PMID 1579108.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link)
- Winkler WG (1970). "Influenza in animals: its possible public health significance". J. Wildl. Dis. 6 (4): 239–42, discussion 247–8. PMID 16512120.
{{cite journal}}: Unknown parameter|month=ignored (help)
