Respiratory failure
| Respiratory failure | |
|---|---|
 | |
| Respiratory system | |
| Specialty | Pulmonology, Intensive care medicine |
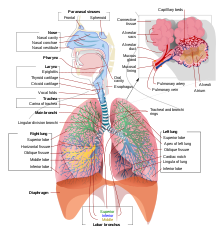
Respiratory failure results from inadequate gas exchange by the respiratory system, meaning that the arterial oxygen, carbon dioxide, or both cannot be kept at normal levels. A drop in the oxygen carried in the blood is known as hypoxemia; a rise in arterial carbon dioxide levels is called hypercapnia. Respiratory failure is classified as either Type 1 or Type 2, based on whether there is a high carbon dioxide level, and can be acute or chronic. In clinical trials, the definition of respiratory failure usually includes increased respiratory rate, abnormal blood gases (hypoxemia, hypercapnia, or both), and evidence of increased work of breathing. Respiratory failure causes an altered mental status due to ischemia in the brain.
The typical partial pressure reference values are oxygen Pa O
2 more than 80 mmHg (11 kPa) and carbon dioxide Pa CO2 less than 45 mmHg (6.0 kPa).[1]
Cause
A variety of conditions that can potentially result in respiratory failure.[1] The etiologies of each type of respiratory failure (see below) may differ, as well. Different types of conditions may cause respiratory failure:
- Conditions that reduce the flow of air into and out of the lungs, including physical obstruction by foreign bodies or masses and reduced breathing due to drugs or changes to the chest.[1]
- Conditions that impair the lungs' blood supply. These include thromboembolic conditions and conditions that reduce the output of the right heart, such as right heart failure and some myocardial infarctions.
- Conditions that limit the ability of the lung tissue to exchange oxygen and carbon dioxide between the blood and the air within the lungs. Any disease which can damage the lung tissue can fit into this category. The most common causes are (in no particular order) infections, interstitial lung disease, and pulmonary edema.

Types
Respiratory failure is generally organized into 4 types.[1] Below is a diagram that provides a general overview of the 4 types of respiratory failure, their distinguishing characteristics, and major causes of each.

Type 1
Type 1 respiratory failure is characterized by a low level of oxygen in the blood (hypoxemia) (PaO2) < 60 mmHg with a normal (normocapnia) or low (hypocapnia) level of carbon dioxide (PaCO2) in the blood.[1]
The fundamental defect in type 1 respiratory failure is a failure of oxygenation characterized by:
PaO2 decreased (< 60 mmHg (8.0 kPa)) PaCO2 normal or decreased (<50 mmHg (6.7 kPa)) PA-aO2 increased
Type I respiratory failure is caused by conditions that affect oxygenation and therefore lead to lower-than-normal oxygen in the blood. These include:
- Low ambient oxygen (e.g. at high altitude).[1]
- Ventilation-perfusion mismatch (parts of the lung receive oxygen but not enough blood to absorb it, e.g. pulmonary embolism, Acute respiratory distress syndrome, Chronic obstructive pulmonary disease, Congestive heart failure.[1]
- Alveolar hypoventilation (decreased minute volume due to reduced respiratory muscle activity, e.g. in acute neuromuscular disease); this form can also cause type 2 respiratory failure if severe.
- Diffusion problem (oxygen cannot enter the capillaries due to parenchymal disease, e.g. in pneumonia or ARDS).
- Right-to-left shunt (oxygenated blood mixes with non-oxygenated blood from the venous system, e.g. Arteriovenous malformation, Complete atelectasis, Severe pneumonia, Severe pulmonary edema).
Type 2
Hypoxemia (PaO2 <8kPa or normal) with hypercapnia (PaCO2 >6.0kPa).
The basic defect in type 2 respiratory failure is characterized by:
PaO2 decreased (< 60 mmHg (8.0 kPa))or normal PaCO2 increased (> 50 mmHg (6.7 kPa)) PA-aO2 normal pH <7.35
Type 2 respiratory failure is caused by inadequate alveolar ventilation; both oxygen and carbon dioxide are affected. Defined as the buildup of carbon dioxide levels (PaCO2) that has been generated by the body but cannot be eliminated. The underlying causes include:
- Increased airways resistance (chronic obstructive pulmonary disease, asthma, suffocation)
- Reduced breathing effort (drug effects, brain stem lesion, extreme obesity)
- A decrease in the area of the lung available for gas exchange (such as in chronic bronchitis)
- Neuromuscular problems (Guillain–Barré syndrome,[2] motor neuron disease)
- Deformed (kyphoscoliosis), rigid (ankylosing spondylitis), or flail chest.[2]
Type 3
Type 3 respiratory failure is a type of Type 1 respiratory failure, with decreased PaO2 (hypoxemia) and either normal or decreased PaCO2.[1] However, because of its prevalence, it has been given its own category. Type 3 respiratory failure is often referred to as peri-operative respiratory failure, because it is distinguished by being a Type 1 respiratory failure that is specifically associated with an operation, procedure, or surgery. [3]
The pathophysiology of type 3 respiratory failure often includes lung atelectasis, which is a term used to describe a collapsing of the functional units of the lung that allow for gas exchange. Because atelectasis occurs so commonly in the perioperative period, this form is also called perioperative respiratory failure. After general anesthesia, decreases in functional residual capacity leads to collapse of dependent lung units.[1]
Type 4
Type 4 respiratory failure occurs when metabolic (oxygen) demands exceed what the cardiopulmonary system can provide.[1] It often results from hypoperfusion of respiratory muscles as in patients in shock, such as cardiogenic shock or hypovolemic shock. Patients in shock often experience respiratory distress due to pulmonary edema (e.g., in cardiogenic shock). Lactic acidosis and anemia can also result in type 4 respiratory failure.[1] However, type 1 and 2 are the most widely accepted.[1][4][5]
Most common conditions causing Type 4 respiratory failure involve hypoperfusion of respiratory muscles as in patients in shock, such as cardiogenic shock or hypovolemic shock.
Patients in shock often experience respiratory distress due to pulmonary edema (e.g., in cardiogenic shock). Lactic acidosis and anemia can also result in type 4 respiratory failure.[6] However, type 1 and 2 are the most widely accepted.[1][7][8]
Physical exam
Physical exam findings often found in patients with respiratory failure include findings indicative of impaired oxygenation (low blood oxygen level). These include, but are not limited to, the following:
- Accessory muscle use in breathing or other signs of respiratory distress[9]
- Altered mental status (eg. confusion, lethargy)[9]
- Clubbing of fingertips (see image right)[9]
- Peripheral cyanosis (eg. bluish color on mucosal membranes or fingers and/or toes)
- Tachypnea (faster breathing rate)[9]
- Pale conjunctiva[9]
People with respiratory failure often exhibit other signs or symptoms that are associated with the underlying cause of their respiratory failure. For instance, if respiratory failure is caused by cardiogenic shock (decreased perfusion due to heart dysfunction, symptoms of heart dysfunction (e.g., pitting edema) are also expected.

Diagnosis
Arterial blood gas (ABG) assessment is considered the gold standard diagnostic test for establishing a diagnosis of respiratory failure.[1] This is because ABG can be used to measure blood oxygen levels (PaO2), and respiratory failure (all types) is characterized by a low blood oxygen level.[1]
Alternative or supporting diagnostic methods include the following:
- Capnometry: measures the amount of carbon dioxide in exhaled air.[1]
- Pulse Oximetry: measures the fraction of hemoglobin saturated with oxygen (SpO2).[1]
Imaging (eg. ultrasonography, radiography) may be used to assist in the diagnostic workup. For example, it may be utilized to determine the etiology of a person's respiratory failure.

Treatment

Treatment of the underlying cause is required, if possible. The treatment of acute respiratory failure may involve medication such as bronchodilators (for airways disease),[10][11] antibiotics (for infections), glucocorticoids (for numerous causes), diuretics (for pulmonary oedema), amongst others.[1][12][13] Respiratory failure resulting from an overdose of opioids may be treated with the antidote naloxone. In contrast, most benzodiazepine overdose does not benefit from its antidote, flumazenil.[14] Respiratory therapy/respiratory physiotherapy may be beneficial in some cases of respiratory failure.[15][16]
Type 1 respiratory failure may require oxygen therapy to achieve adequate oxygen saturation.[17] Lack of oxygen response may indicate other modalities such as heated humidified high-flow therapy, continuous positive airway pressure or (if severe) endotracheal intubation and mechanical ventilation. .[citation needed]
Type 2 respiratory failure often requires non-invasive ventilation (NIV) unless medical therapy can improve the situation.[18] Mechanical ventilation is sometimes indicated immediately or otherwise if NIV fails.[18] Respiratory stimulants such as doxapram are now rarely used.[19]
There is tentative evidence that in those with respiratory failure identified before arrival in hospital, continuous positive airway pressure can be helpful when started before conveying to hospital.[20]
Prognosis
Prognosis is highly variable and dependent on etiology and availability of appropriate treatment and management.[21] One of three hospitalized cases of acute respiratory failure is fatal.[21]
See also
References
- ^ a b c d e f g h i j k l m n o p q r Mirabile, Vincent S.; Shebl, Eman; Sankari, Abdulghani; Burns, Bracken (2023), "Respiratory Failure", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 30252383, retrieved 2023-11-15
- ^ a b Arrowsmith J, Burt C (1 November 2009). "Respiratory failure". Surgery. 27 (11). Oxford: 475–479. doi:10.1016/j.mpsur.2009.09.007.
- ^ "Acute respiratory failure". Department of Critical Care. Retrieved 2023-10-28.
- ^ Katyal P, Gajic O. "Critical Care Medicine, Acute respiratory failure" (PDF). Mayo Clinic. Rochester, MN, USA. Archived from the original (PDF) on 9 April 2021 – via McGill University.
- ^ Melanson P. "Acute respiratory failure". Critical Care Medicine. McGill University.
- ^ Harrison’s principles of internal medicine
- ^ Katyal P, Gajic O. "Critical Care Medicine, Acute respiratory failure" (PDF). Mayo Clinic. Rochester, MN, USA. Archived from the original (PDF) on 9 April 2021 – via McGill University.
- ^ Melanson P. "Acute respiratory failure". Critical Care Medicine. McGill University.
- ^ a b c d e "Respiratory Failure - Diagnosis". National Heart, Lung and Blood Institute, US National Institutes of Health. 2022-03-24. Retrieved 2023-11-15.
- ^ Artigas A, Camprubí-Rimblas M, Tantinyà N, Bringué J, Guillamat-Prats R, Matthay MA (July 2017). "Inhalation therapies in acute respiratory distress syndrome". Annals of Translational Medicine. 5 (14): 293. doi:10.21037/atm.2017.07.21. PMC 5537120. PMID 28828368.
- ^ Budinger GR, Mutlu GM (March 2014). "β2-agonists and acute respiratory distress syndrome". American Journal of Respiratory and Critical Care Medicine. 189 (6): 624–5. doi:10.1164/rccm.201401-0170ED. PMC 3983843. PMID 24628310.
- ^ Yin J, Bai CX (May 2018). "Pharmacotherapy for Adult Patients with Acute Respiratory Distress Syndrome". Chinese Medical Journal. 131 (10): 1138–1141. doi:10.4103/0366-6999.231520. PMC 5956763. PMID 29722332.
- ^ Lewis SR, Pritchard MW, Thomas CM, Smith AF (2019). "Pharmacological agents for adults with acute respiratory distress syndrome". Cochrane Database of Systematic Reviews. 7 (7): CD004477. doi:10.1002/14651858.CD004477.pub3. PMC 6646953. PMID 31334568. CD004477.
- ^ Sivilotti ML (March 2016). "Flumazenil, naloxone and the 'coma cocktail'". British Journal of Clinical Pharmacology. 81 (3): 428–36. doi:10.1111/bcp.12731. PMC 4767210. PMID 26469689.
- ^ Wong WP (July 2000). "Physical therapy for a patient in acute respiratory failure". Physical Therapy. 80 (7): 662–70. doi:10.1093/ptj/80.7.662. PMID 10869128.
- ^ Gai L, Tong Y, Yan B (July 2018). "The Effects of Pulmonary Physical Therapy on the Patients with Respiratory Failure". Iranian Journal of Public Health. 47 (7): 1001–1006. PMC 6119578. PMID 30181999.
- ^ O'Driscoll BR, Howard LS, Earis J, Mak V (May 2017). "British Thoracic Society Guideline for oxygen use in adults in healthcare and emergency settings". BMJ Open Respiratory Research. 4 (1): e000170. doi:10.1136/bmjresp-2016-000170. PMC 5531304. PMID 28883921.
- ^ a b Rochwerg B, Brochard L, Elliott MW, Hess D, Hill NS, Nava S, et al. (August 2017). "Official ERS/ATS clinical practice guidelines: noninvasive ventilation for acute respiratory failure". The European Respiratory Journal. 50 (2): 1602426. doi:10.1183/13993003.02426-2016. PMID 28860265.
- ^ Greenstone M, Lasserson TJ (2003). "Doxapram for ventilatory failure due to exacerbations of chronic obstructive pulmonary disease". The Cochrane Database of Systematic Reviews (1): CD000223. doi:10.1002/14651858.CD000223. PMID 12535393.
- ^ Bakke SA, Botker MT, Riddervold IS, Kirkegaard H, Christensen EF (November 2014). "Continuous positive airway pressure and noninvasive ventilation in prehospital treatment of patients with acute respiratory failure: a systematic review of controlled studies". Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine. 22 (1): 69. doi:10.1186/s13049-014-0069-8. PMC 4251922. PMID 25416493.
- ^ a b "Respiratory failure". Cleveland Clinic. 15 March 2023. Retrieved 15 November 2023.
