Beta-lactamase
| Beta-lactamase | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
 Structure of a Streptomyces albus beta-lactamase | |||||||||||
| Identifiers | |||||||||||
| Symbol | β-lactamase domain | ||||||||||
| Pfam | PF00144 | ||||||||||
| Pfam clan | CL0013 | ||||||||||
| InterPro | IPR001466 | ||||||||||
| PROSITE | PS00146 | ||||||||||
| SCOP2 | 56601 / SCOPe / SUPFAM | ||||||||||
| |||||||||||
| β-lactamase | |||||||||
|---|---|---|---|---|---|---|---|---|---|
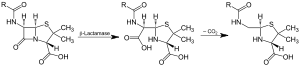 Action of β-lactamase and decarboxylation of the intermediate | |||||||||
| Identifiers | |||||||||
| EC no. | 3.5.2.6 | ||||||||
| CAS no. | 9073-60-3 | ||||||||
| Databases | |||||||||
| IntEnz | IntEnz view | ||||||||
| BRENDA | BRENDA entry | ||||||||
| ExPASy | NiceZyme view | ||||||||
| KEGG | KEGG entry | ||||||||
| MetaCyc | metabolic pathway | ||||||||
| PRIAM | profile | ||||||||
| PDB structures | RCSB PDB PDBe PDBsum | ||||||||
| Gene Ontology | AmiGO / QuickGO | ||||||||
| |||||||||


Beta-lactamases are enzymes (EC 3.5.2.6) produced by some bacteria and are responsible for their resistance to beta-lactam antibiotics like penicillins, cephamycins, and carbapenems (ertapenem). (Cephalosporins are relatively resistant to beta-lactamase.) These antibiotics have a common element in their molecular structure: a four-atom ring known as a beta-lactam. The lactamase enzyme breaks that ring open, deactivating the molecule's antibacterial properties.
Beta-lactam antibiotics are typically used to treat a broad spectrum of Gram-positive and Gram-negative bacteria. Beta-lactamases produced by Gram-negative organisms are usually secreted.
The structure of a Streptomyces β lactamase is given by 1BSG.
Penicillinase
Penicillinase is a specific type of β-lactamase, showing specificity for penicillins, again by hydrolysing the beta-lactam ring. Molecular weights of the various penicillinases tend to cluster near 50kiloDalton.
Penicillinase was the first β-lactamase to be identified: it was first isolated by Abraham and Chain in 1940 from Gram-negative E. coli even before penicillin entered clinical use[1] but penicillinase production quickly spread to bacteria that previously did not produce it or only produced it rarely. Penicillinase-resistant beta-lactams such as methicillin were developed, but there is now widespread resistance to even these.
Classification of Beta Lactamase
Functional Classification[2]
Group 1
- CEPHALOSPORINASE, Molecular Class C (not inhibited by clavulanic acid)
- Group 1 are cephalosporinases not inhibited by clavulanic acid, belonging to the molecular class C
Group 2
Group 2 are penicillinases, cephalosporinases, or both inhibited by clavulanic acid, corresponding to the molecular classes A and D reflecting the original TEM and SHV genes. However, because of the increasing number of TEM- and SHV-derived {beta}-lactamases, they were divided into two subclasses, 2a and 2b.
- GROUP 2a
- PENICILLINASE, Molecular Class A
- The 2a subgroup contains just penicillinases.
- GROUP 2b
- BROAD-SPECTRUM, Molecular Class A
- 2b Opposite to 2a , 2b are broad-spectrum {beta}-lactamases, meaning that they are capable of inactivating penicillins and cephalosporins at the same rate. Furthermore, new subgroups were segregated from subgroup 2b:
- GROUP 2be
- EXTENDED-SPECTRUM, Molecular Class A
- Subgroup 2be, with the letter "e" for extended spectrum of activity, represents the ESBLs, which are capable of inactivating third-generation cephalosporins (ceftazidime, cefotaxime, and cefpodoxime) as well as monobactams (aztreonam)
- GROUP 2br
- INHIBITOR-RESISTANT, Molecular Class A (diminished inhibition by clavulanic acid)
- The 2br enzymes, with the letter "r" denoting reduced binding to clavulanic acid and sulbactam, are also called inhibitor-resistant TEM-derivative enzymes; nevertheless, they are commonly still susceptible to tazobactam, except where an amino acid replacement exists at position met69.
- GROUP 2c
- CARBENICILLINASE, Molecular Class A
- Latersubgroup 2c was segregated from group 2 because these enzymes inactivate carbenicillin more than benzylpenicillin, with some effect on cloxacillin.
- GROUP 2d
- CLOXACILANASE, Molecular Class D or A
- Subgroup 2d enzymes inactivate cloxacillin more than benzylpenicillin, with some activity against carbenicillin; these enzymes are poorly inhibited by clavulanic acid, and some of them are ESBLs
- the correct term is "OXACILLINASE". These enzymes are able to inactivate the oxazolylpenicillins like oxacilli, cloxacilli, dicloxacillin. The enzymes belong to the molecular class D not molecular class A.
- GROUP 2e
- CEPHALOSPORINASE, Molecular Class A
- Subgroup 2e enzymes are cephalosporinases that can also hydrolyse monobactams, and they are inhibited by clavulanic acid
- GROUP 2f
- CARBAPENAMASE, Molecular Class A
- Subgroup 2f was added because these are serine-based carbapenemases, in contrast to the zinc-based carbapenemases included in group 3
Group 3
- METALLOENZYME, Molecular Class B (not inhibited by clavulanic acid)
- Group 3 are the zinc based or metallo {beta}-lactamases, corresponding to the molecular class B, which are the only enzymes acting by the metal ion zinc, as discussed above. Metallo B-lactamases are able to hydrolyse penicillins, cephalosporins, and carbapenems. Thus, carbapenems are inhibited by both group 2f (serine-based mechanism) and group 3 (zinc-based mechanism)
Group 4
- PENICILLINASE, No Molecular Class (not inhibited by clavulanic acid)
- Group 4 are penicillinases that are not inhibited by clavulanic acid, and they do not yet have a corresponding molecular class.
Molecular Classification
The molecular classification of β-lactamases is based on the nucleotide and amino acid sequences in these enzymes. To date, four classes are recognised (A-D), correlating with the functional classification. Classes A, C, and D act by a serine-based mechanism, whereas class B or metallo-β-lactamases need zinc for their action[3]
"Penicillinase" was discovered in 1940 and re-named Beta-lactamase when the structure of the Beta-lactam ring was finally elucidated.
Resistance in Gram-negative bacteria
Among Gram-negative bacteria, the emergence of resistance to expanded-spectrum cephalosporins has been a major concern. It appeared initially in a limited number of bacterial species (E. cloacae , C. freundii, S. marcescens, and P. aeruginosa ) that could mutate to hyperproduce their chromosomal class C β-lactamase. A few years later, resistance appeared in bacterial species not naturally-producing AmpC enzymes (K. pneumoniae, Salmonella spp., P. mirabilis) due to the production of TEM- or SHV-type ESBLs. Characteristically, such resistance has included oxyimino- (for example ceftizoxime, cefotaxime , ceftriaxone, and ceftazidime, as well as the oxyimino-monobactam aztreonam), but not 7-alpha-methoxy-cephalosporins (cephamycins); in other words, (cefoxitin and cefotetan) have been blocked by inhibitors such as clavulanate, sulbactam, or tazobactam, and did not involve carbapenems. Chromosomal-mediated AmpC β-lactamases represent a new threat, since they confer resistance to 7-alpha-methoxy-cephalosporins (cephamycins) such as cefoxitin or cefotetan are not affected by commercially-available β-lactamase inhibitors, and can, in strains with loss of outer membrane porins, provide resistance to carbapenems.[4]
Extended-spectrum beta-lactamase (ESBL)
Members of the family Enterobacteriaceae commonly express plasmid-encoded β-lactamases (e.g., TEM-1, TEM-2, and SHV-1). which confer resistance to penicillins but not to expanded-spectrum cephalosporins. In the mid-1980s, a new group of enzymes, the extended-spectrum b-lactamases (ESBLs), was detected. (first detected in Germany in 1983).[5] ESBLs are beta-lactamases that hydrolyze extended-spectrum cephalosporins with an oxyimino side chain. These cephalosporins include cefotaxime, ceftriaxone, and ceftazidime, as well as the oxyimino-monobactam aztreonam. Thus ESBLs confer resistance to these antibiotics and related oxyimino-beta lactams. In typical circumstances, they derive from genes for TEM-1, TEM-2, or SHV-1 by mutations that alter the amino acid configuration around the active site of these β-lactamases. This extends the spectrum of β-lactam antibiotics susceptible to hydrolysis by these enzymes. An increasing number of ESBLs not of TEM or SHV lineage have recently been described.[6] The ESBLs are frequently plasmid encoded. Plasmids responsible for ESBL production frequently carry genes encoding resistance to other drug classes (for example, aminoglycosides). Therefore, antibiotic options in the treatment of ESBL-producing organisms are extremely limited. Carbapenems are the treatment of choice for serious infections due to ESBL-producing organisms, yet carbapenem-resistant isolates have recently been reported. ESBL-producing organisms may appear susceptible to some extended-spectrum cephalosporins. However, treatment with such antibiotics has been associated with high failure rates.
Types
TEM beta-lactamases (class A)
TEM-1 is the most commonly-encountered beta-lactamase in Gram-negative bacteria. Up to 90% of ampicillin resistance in E. coli is due to the production of TEM-1[citation needed]. Also responsible for the ampicillin and penicillin resistance that is seen in H. influenzae and N. gonorrhoeae in increasing numbers. Although TEM-type beta-lactamases are most often found in E. coli and K. pneumoniae, they are also found in other species of Gram-negative bacteria with increasing frequency. The amino acid substitutions responsible for the ESBL phenotype cluster around the active site of the enzyme and change its configuration, allowing access to oxyimino-beta-lactam substrates. Opening the active site to beta-lactam substrates also typically enhances the susceptibility of the enzyme to b-lactamase inhibitors, such as clavulanic acid. Single amino acid substitutions at positions 104, 164, 238, and 240 produce the ESBL phenotype, but ESBLs with the broadest spectrum usually have more than a single amino acid substitution. Based upon different combinations of changes, currently 140 TEM-type enzymes have been described. TEM-10, TEM-12, and TEM-26 are among the most common in the United States.[7][8][9]
SHV beta-lactamases (class A)
SHV-1 shares 68 percent of its amino acids with TEM-1 and has a similar overall structure. The SHV-1 beta-lactamase is most commonly found in K. pneumoniae and is responsible for up to 20% of the plasmid-mediated ampicillin resistance in this species. ESBLs in this family also have amino acid changes around the active site, most commonly at positions 238 or 238 and 240. More than 60 SHV varieties are known. They are the predominant ESBL type in Europe and the United States and are found worldwide. SHV-5 and SHV-12 are among the most common.[10]
CTX-M beta-lactamases (class A)
These enzymes were named for their greater activity against cefotaxime than other oxyimino-beta-lactam substrates (e.g., ceftazidime, ceftriaxone, or cefepime). Rather than arising by mutation, they represent examples of plasmid acquisition of beta-lactamase genes normally found on the chromosome of Kluyvera species, a group of rarely pathogenic commensal organisms. These enzymes are not very closely related to TEM or SHV beta-lactamases in that they show only approximately 40% identity with these two commonly isolated beta-lactamases. More than 80 CTX-M enzymes are currently known. Despite their name, a few are more active on ceftazidime than cefotaxime. They have mainly been found in strains of Salmonella enterica serovar Typhimurium and E. coli, but have also been described in other species of Enterobacteriaceae and are the predominant ESBL type in parts of South America. (They are also seen in eastern Europe) CTX-M-14, CTX-M-3, and CTX-M-2 are the most widespread. CTX-M-15 is currently (2006) the most widespread type in E. coli the UK and is widely prevalent in the community.[11]
OXA beta-lactamases (class D)
OXA beta-lactamases were long recognized as a less common but also plasmid-mediated beta-lactamase variety that could hydrolyze oxacillin and related anti-staphylococcal penicillins. These beta-lactamases differ from the TEM and SHV enzymes in that they belong to molecular class D and functional group 2d . The OXA-type beta-lactamases confer resistance to ampicillin and cephalothin and are characterized by their high hydrolytic activity against oxacillin and cloxacillin and the fact that they are poorly inhibited by clavulanic acid. Amino acid substitutions in OXA enzymes can also give the ESBL phenotype. While most ESBLs have been found in E. coli, K. pneumoniae, and other Enterobacteriaceae, the OXA-type ESBLs have been found mainly in P. aeruginosa. OXA-type ESBLs have been found mainly in Pseudomonas aeruginosa isolates from Turkey and France. The OXA beta-lactamase family was originally created as a phenotypic rather than a genotypic group for a few beta-lactamases that had a specific hydrolysis profile. Therefore, there is as little as 20% sequence homology among some of the members of this family. However, recent additions to this family show some degree of homology to one or more of the existing members of the OXA beta-lactamase family. Some confer resistance predominantly to ceftazidime, but OXA-17 confers greater resistance to cefotaxime and cefepime than it does resistance to ceftazidime.
Others
Other plasmid-mediated ESBLs, such as PER, VEB, GES, and IBC beta-lactamases, have been described but are uncommon and have been found mainly in P. aeruginosa and at a limited number of geographic sites. PER-1 in isolates in Turkey, France, and Italy; VEB-1 and VEB-2 in strains from Southeast Asia; and GES-1, GES-2, and IBC-2 in isolates from South Africa, France, and Greece. PER-1 is also common in multiresistant acinetobacter species in Korea and Turkey. Some of these enzymes are found in Enterobacteriaceae as well, whereas other uncommon ESBLs (such as BES-1, IBC-1, SFO-1, and TLA-1) have been found only in Enterobacteriaceae.
Treatment
While ESBL-producing organisms were previously associated with hospitals and institutional care, these organisms are now increasingly found in the community. CTX-M-15-positive E. coli are a cause of community-acquired urinary infections in the UK,[12] and tend to be resistant to all oral β-lactam antibiotics, as well as quinolones and sulfonamides. Treatment options may include nitrofurantoin, fosfomycin, mecillinam and chloramphenicol. In desperation, once-daily ertapenem or gentamicin injections may also be used.
Inhibitor-resistant β-lactamases
Although the inhibitor-resistant β-lactamases are not ESBLs, they are often discussed with ESBLs because they are also derivatives of the classical TEM- or SHV-type enzymes. These enzymes were at first given the designation IRT for inhibitor-resistant TEM β-lactamase; however, all have subsequently been renamed with numerical TEM designations. There are at least 19 distinct inhibitor-resistant TEM β-lactamases. Inhibitor-resistant TEM β-lactamases have been found mainly in clinical isolates of E. coli, but also some strains of K. pneumoniae, Klebsiella oxytoca, P. mirabilis, and Citrobacter freundii .Although the inhibitor-resistant TEM variants are resistant to inhibition by clavulanic acid and sulbactam, thereby showing clinical resistance to the beta-lactam—lactamase inhibitor combinations of amoxicillin-clavulanate (Co-amoxiclav), ticarcillin-clavulanate, and ampicillin/sulbactam, they normally remain susceptible to inhibition by tazobactam and subsequently the combination of piperacillin/tazobactam, although resistance has been described. To date, these beta-lactamases have primarily been detected in France and a few other locations within Europe.[13]
AmpC-type β-lactamases (Class C)
AmpC type β-lactamases are commonly isolated from extended-spectrum cephalosporin-resistant Gram-negative bacteria. AmpC β-lactamases (also termed class C or group 1) are typically encoded on the chromosome of many Gram-negative bacteria including Citrobacter, Serratia and Enterobacter species where its expression is usually inducible; it may also occur on Escherichia coli but is not usually inducible, although it can be hyperexpressed. AmpC type β-lactamases may also be carried on plasmids.[14] AmpC β-lactamases, in contrast to ESBLs, hydrolyse broad and extended-spectrum cephalosporins (cephamycins as well as to oxyimino-β-lactams) but are not inhibited by β-lactamase inhibitors such as clavulanic acid.
Carbapenemases
Carbapenems are famously stable to AmpC β-lactamases and extended-spectrum-β-lactamases. Carbapenemases are a diverse group of b-lactamases that are active not only against the oxyimino-cephalosporins and cephamycins but also against the carbapenems. Aztreonam is stable to the metallo-β-lactamases but many IMP and VIM producers are resistant, owing to other mechanisms. Carbapenemases were formerly believed to derive only from classes A, B, and D, but a class C carbapenemase has been described.
IMP-type carbapenemases (one of the metallo-β-lactamases)
Plasmid-mediated IMP-type carbapenemases, 17 varieties of which are currently known, became established in Japan in the 1990s in both enteric Gram-negative organisms and in Pseudomonas and Acinetobacter species. IMP enzymes spread slowly to other countries in the Far East, were reported from Europe in 1997, and have been found in Canada and Brazil.
VIM (Verona integron-encoded metallo-β-lactamase)
A second growing family of carbapenemases, the VIM family, was reported from Italy in 1999 and now includes 10 members, which have a wide geographic distribution in Europe, South America, and the Far East and have been found in the United States. VIM-1 was discovered in P. aeruginosa in Italy in 1996; since then, VIM-2 - now the predominant variant - was found repeatedly in Europe and the Far East; VIM-3 and -4 are minor variants of VIM-2 and -1, respectively. VIM enzymes occur mostly in P. aeruginosa, also P. putidaand, very rarely, Enterobacteriaceae.
Amino acid sequence diversity is up to 10% in the VIM family, 15% in the IMP family, and 70% between VIM and IMP. Enzymes of both the families, nevertheless, are similar. Both are integron-associated, sometimes within plasmids. Both hydrolyse all β-lactams except monobactams, and evade all β-lactam inhibitors.
OXA (oxacillinase) group of β-lactamases (Class D)
The OXA group of β-lactamases occur mainly in Acinetobacter species and are divided into two clusters. OXA carbapenemases hydrolyse carbapenems very slowly in vitro, and the high MICs seen for some Acinetobacter hosts (>64 mg/L) may reflect secondary mechanisms. They are sometimes augmented in clinical isolates by additional resistance mechanisms, such as impermeability or efflux. OXA carbapenemases also tend to have a reduced hydrolytic efficiency towards penicillins and cephalosporins.[15]
KPC (K. pneumoniae carbapenemase) (Class A)
A few class A enzymes, most noted the plasmid-mediated KPC enzymes, are effective carbapenemases as well. Ten variants, KPC-2 through KPC-11 are known, and they are distinguished by one or two amino-acid substitutions (KPC-1 was re-sequenced in 2008 and found to be 100% homologous to published sequences of KPC-2). KPC-1 was found in North Carolina, KPC-2 in Baltimore and KPC-3 in New York. They have only 45% homology with SME and NMC/IMI enzymes and, unlike them, can be encoded by self-transmissible plasmids.
The class A Klebsiella pneumoniae carbapenemase (KPC) is currently the most common carbapenemase, which was first detected in North Carolina, USA, in 1996 and has since spread worldwide.[16] A later publication indicated that Enterobacteriaceae that produce KPC were becoming common in the United States.[17]
CMY (Class C)
The first class C carbapenemase was described in 2006 and was isolated from a virulent strain of Enterobacter aerogenes.[18] It is carried on a plasmid, pYMG-1, and is therefore transmissible to other bacterial strains.[19]
SME, IMI, NMC and CcrA
In general, these are of little clinical significance.
CcrA (CfiA). Its gene occurs in c. 1-3% of B. fragilis isolates, but fewer produce the enzyme since expression demands appropriate migration of an insertion sequence. CcrA was known before imipenem was introduced, and producers have shown little subsequent increase.
NDM-1 (New Delhi metallo-β-lactamase)
Originally described from New Delhi in 2009, this gene is now widespread in Escherichia coli and Klebsiella pneumoniae from India and Pakistan. As of mid-2010, NDM-1 carrying bacteria have been introduced to other countries (including the USA and UK), presumably by medical tourists undergoing surgery in India.
Treatment of ESBL/AmpC/carbapenemases
General Overview
In general, an isolate is suspected to be an ESBL producer when it shows in vitro susceptibility to the second-generation cephalosporins (cefoxitin, cefotetan) but resistance to the third-generation cephalosporins and to aztreonam. Moreover, one should suspect these strains when treatment with these agents for Gram-negative infections fails despite reported in vitro susceptibility. Once an ESBL-producing strain is detected, the laboratory should report it as "resistant" to all penicillins, cephalosporins, and aztreonam, even if it is tested (in vitro) as susceptible.[citation needed] Associated resistance to aminoglycosides and trimethoprim-sulfamethoxazole, as well as high frequency of co-existence of fluoroquinolone resistance, creates problems. Beta-lactamase inhibitors such as clavulanate, sulbactam, and tazobactam in vitro inhibit most ESBLs, but the clinical effectiveness of beta-lactam/beta-lactamase inhibitor combinations cannot be relied on consistently for therapy. Cephamycins (cefoxitin and cefotetan) are not hydrolyzed by majority of ESBLs, but are hydrolyzed by associated AmpC-type β-lactamase. Also, β-lactam/β-lactamase inhibitor combinations may not be effective against organisms that produce AmpC-type β-lactamase. Sometimes these strains decrease the expression of outer membrane proteins, rendering them resistant to cephamycins. In vivo studies have yielded mixed results against ESBL-producing K. pneumoniae. (Cefepime, a fourth-generation cephalosporin, has demonstrated in vitro stability in the presence of many ESBL/AmpC strains.) Currently, carbapenems are, in general, regarded as the preferred agent for treatment of infections due to ESBL-producing organisms. Carbapenems are resistant to ESBL-mediated hydrolysis and exhibit excellent in vitro activity against strains of Enterobacteriaceae expressing ESBLs.[citation needed]
According to genes
ESBLs
Strains producing only ESBLs are susceptible to cephamycins and carbapenems in vitro and show little if any inoculum effect with these agents.
For organisms producing TEM and SHV type ESBLs, apparent in vitro sensitivity to cefepime and to piperacillin/tazobactam is common, but both drugs show an inoculum effect, with diminished susceptibility as the size of the inoculum is increased from 105to 107organisms.
Strains with some CTX-M–type and OXA-type ESBLs are resistant to cefepime on testing, despite the use of a standard inoculum.
Inhibitor-Resistant β-Lactamases
Although the inhibitor-resistant TEM variants are resistant to inhibition by clavulanic acid and sulbactam, thereby showing clinical resistance to the beta-lactam—lactamase inhibitor combinations of amoxicillin-clavulanate (Co-amoxiclav), ticarcillin-clavulanate, and ampicillin/sulbactam, they remain susceptible to inhibition by tazobactam and subsequently the combination of piperacillin/tazobactam.
AmpC
AmpC-producing strains are typically resistant to oxyimino-beta lactams and to cephamycins and are susceptible to carbapenems; however, diminished porin expression can make such a strain carbapenem-resistant as well.
Carbapenemases
Strains with IMP-, VIM-, and OXA-type carbapenemases usually remain susceptible to aztreonam. Resistance to non–b-lactam antibiotics is common in strains making any of these enzymes, such that alternative options for non–b-lactam therapy need to be determined by direct susceptibility testing. Resistance to fluoroquinolones and aminoglycosides is especially high.
According to Species
Escherichia coli or Klebsiella
For infections caused by ESBL-producing Escherichia coli or Klebsiella species, treatment with imipenem or meropenem has been associated with the best outcomes in terms of survival and bacteriologic clearance. Cefepime and piperacillin/tazobactam have been less successful. Ceftriaxone, cefotaxime, and ceftazidime have failed even more often, despite the organism's susceptibility to the antibiotic in vitro. Several reports have documented failure of cephamycin therapy as a result of resistance due to porin loss. Some patients have responded to aminoglycoside or quinolone therapy, but in a recent comparison of ciprofloxacin and imipenem for bacteremia involving an ESBL-producing K. pneumoniae, imipenem produced the better outcome.
Pseudomonas aeruginosa
There have been few clinical studies to define the optimal therapy for infections caused by ESBL producing Pseudomonas aeruginosa strains.
See also
References
- ^ Abraham EP, Chain E (1940). "An enzyme from bacteria able to destroy penicillin". Nature. 46 (3713): 837–837. doi:10.1038/146837a0.
- ^ *Bush K, Jacoby GA, Medeiros AA.1995. "A functional classification scheme for beta-lactamases and its correlation with molecular structure." Antimicrob Agents Chemother.. 1995;39: 1211-33
- ^ *Ambler RP.1980. "The structure of beta-lactamases." Philos Trans R Soc Lond B Biol Sci.. 1980;289: 321-31
- ^ *Philippon A, Arlet B, Jacoby GA.2002. "Plasmid-determined AmpC-type β-lactamases" Antimicrob Agents Chemother.. 2002; 46: 1-11
- ^ *Knothe H; Shah P. Kremery V; et al. (1983). "Transferable resistance to cefotaxime, cefoxitin, cefamandole and cefuroxime in clinical isolates of Klebsiella pneumoniae and [[Serratia marcescens]]". Infection. 11 (6): 315–317. doi:10.1007/BF01641355. PMID 6321357.
{{cite journal}}: URL–wikilink conflict (help); Unknown parameter|author-separator=ignored (help) - ^ *Emery C. L., Weymouth L. A. (1997). "Detection and clinical significance of extended-spectrum β-lactamases in a tertiary-care medical center". J. Clin. Microbiol. 35 (8): 2061–7. PMC 229903. PMID 9230382.
- ^ *Paterson DL; Hujer KM; Hujer AM; et al. (2003). "Extended-spectrum b-lactamases in Klebsiella pneumoniae bloodstream isolates from seven countries: dominance and widespread prevalence of SHV- and CTX-M-type b-lactamases". Antimicrob Agents Chemother. 47 (11): 3554–3560. doi:10.1128/AAC.47.11.3554-3560.2003. PMC 253771. PMID 14576117.
{{cite journal}}: Unknown parameter|author-separator=ignored (help) - ^ *Bradford PA.2001. "Extended-spectrum β-lactamases in the 21st century:characterization, epidemiology, and detection of this important resistance threat." Clin Microbiol Rev.. 2001; 48:933-51
- ^ Jacoby George A., Luisa Silvia Munoz-Price (2005). "mechanisms of disease: The New beta-Lactamases" (PDF). N Engl J Med. 352 (4): 380–391. doi:10.1056/NEJMra041359. PMID 15673804.
- ^ *Paterson DL; Hujer KM; Hujer AM; et al. (2003). "Extended-spectrum b-lactamases in Klebsiella pneumoniae bloodstream isolates from seven countries: dominance and widespread prevalence of SHV- and CTX-M-type b-lactamases". Antimicrob Agents Chemother. 47 (11): 3554–3560. doi:10.1128/AAC.47.11.3554-3560.2003. PMC 253771. PMID 14576117.
{{cite journal}}: Unknown parameter|author-separator=ignored (help) - ^ Woodford N, Ward E, Kaufmann ME; et al. "Molecular characterisation of Escherichia coli isolates producing CTX-M-15 extended-spectrum β-lactamase (ESBL) in the United Kingdom" (PDF). Health Protection Agency. Retrieved 2006-11-19.
{{cite web}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Woodford N, Ward E, Kaufmann ME; et al. "Molecular characterisation of Escherichia coli isolates producing CTX-M-15 extended-spectrum βlactamase (ESBL) in the United Kingdom" (PDF). Retrieved 2006-11-08.
{{cite web}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ *Bradford PA.2001. "Extended-spectrum β-lactamases in the 21st century:characterization, epidemiology, and detection of this important resistance threat." "Clin Microbiol Rev.. 2001; 48:933-51
- ^ *Philippon A, Arlet B, Jacoby GA.2002. "Plasmid-determined AmpC-type β-lactamases" Antimicrob Agents Chemother.. 2002; 46:
- ^ Santillana; et al. (2007). "Crystal structure of the carbapenemase OXA-24 reveals insights into the mechanism of carbapenem hydrolysis". PNAS. 104 (13): 5354–5359. doi:10.1073/pnas.0607557104. PMC 1838445. PMID 17374723.
- ^ Nordmann P, Cuzon G, Naas T (2009). "The real threat of Klebsiella pneumoniae carbapenemase-producing bacteria". Lancet Infect Dis. 9 (4): 228–236. doi:10.1016/S1473-3099(09)70054-4. PMID 19324295.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Cuzon G, Naas T, Nordmann P (2010 Feb). "KPC carbapenemases: what is at stake in clinical microbiology?". Pathol Biol (Paris) (in French). 58 (1): 39–45. doi:10.1016/j.patbio.2009.07.026. PMID 19854586.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|trans_title=ignored (|trans-title=suggested) (help)CS1 maint: multiple names: authors list (link) - ^ Kim JY; Jung HI; An YJ; et al. (2006). "Structural basis for the extended substrate spectrum of CMY-10, a plasmid-encoded class C beta-lactamase". Mol Microbiol. 60 (4): 907–16. doi:10.1111/j.1365-2958.2006.05146.x. PMID 16677302.
{{cite journal}}: Unknown parameter|author-separator=ignored (help) - ^ Lee JH; Jung HI; Jung JH (2004). "Dissemination of transferable AmpC-type β-lactamase (CMY-10) in a Korean hospital". Microbiol Drug Resist. 10: 224–30.
{{cite journal}}: Invalid|display-authors=3(help); Unknown parameter|author-separator=ignored (help)
External links
- Online ESBL genotyping tool (EGT)
- Online Amino Acid Sequences for ESBL enzymes
- beta-Lactamases at the U.S. National Library of Medicine Medical Subject Headings (MeSH)
