Leukopenia
| Leukopenia | |
|---|---|
| Specialty | Hematology |
Leukopenia (also known as leukocytopenia or leucopenia, from Greek λευκός "white" and πενία "deficiency") is a decrease in the number of white blood cells (leukocytes) found in the blood, which places individuals at increased risk of infection.
Neutropenia, a subtype of leukopenia, refers to a decrease in the number of circulating neutrophil granulocytes, the most abundant white blood cells. The terms leukopenia and neutropenia may occasionally be used interchangeably, as the neutrophil count is the most important indicator of infection risk. This should not be confused with agranulocytosis.
Causes
Medical conditions
Low white cell count may be due to acute viral infections, such as with a cold or influenza. It can be associated with chemotherapy, radiation therapy, myelofibrosis and aplastic anemia (failure of white cell, red cell and platelet production). HIV and AIDS are also a threat to white cells.
Other causes of low white blood cell count include systemic lupus erythematosus, Hodgkin's lymphoma, some types of cancer, typhoid, malaria, tuberculosis, dengue, rickettsial infections, enlargement of the spleen, folate deficiencies, psittacosis, sepsis and Lyme disease. Many other causes exist, such as deficiency in certain minerals, such as copper and zinc.
Pseudoleukopenia can develop upon the onset of infection. The leukocytes (predominately neutrophils, responding to injury first) start migrating towards the site of infection and can be scanned at the site of infection. Their migration causes bone marrow to produce more WBCs to combat infection as well as to restore the leukocytes in circulation, but as the blood sample is taken upon the onset of infection, it contains low amount of WBCs, which is why it is called "pseudoleukopenia".
Medications
Some medications can have an impact on the number and function of white blood cells.
Medications which can cause leukopenia include clozapine, an antipsychotic medication with a rare adverse effect leading to the total absence of all granulocytes (neutrophils, basophils, eosinophils). The antidepressant and smoking addiction treatment drug bupropion HCl (Wellbutrin) can also cause leukopenia with long-term use. Minocycline, a commonly prescribed antibiotic, is another drug known to cause leukopenia. There are also reports of leukopenia caused by divalproex sodium or valproic acid (Depakote), a drug used for epilepsy (seizures), mania (with bipolar disorder) and migraine.
The anticonvulsant drug, lamotrigine, has been associated with a decrease in white blood cell count.[1]
The FDA monograph for metronidazole states that this medication can also cause leukopenia, and the prescriber information suggests a complete blood count, including differential cell count, before and after, in particular, high-dose therapy.
Other medications include immunosuppressive drugs, such as sirolimus, mycophenolate mofetil, tacrolimus, ciclosporin, leflunomide and TNF inhibitors.[2] Interferons used to treat multiple sclerosis, such as interferon beta-1a and interferon beta-1b, can also cause leukopenia.
Chemotherapy targets cells that grow rapidly, such as tumors, but can also affect white blood cells, because they are characterized by bone marrow as rapid growing.[3] A common side effect of cancer treatment is neutropenia, the lowering of neutrophils (a specific type of white blood cell).[4]
Decreased white blood cell count may be present in cases of arsenic toxicity.[5]
Diagnosis
Leukopenia can be identified with a complete blood count.[6]
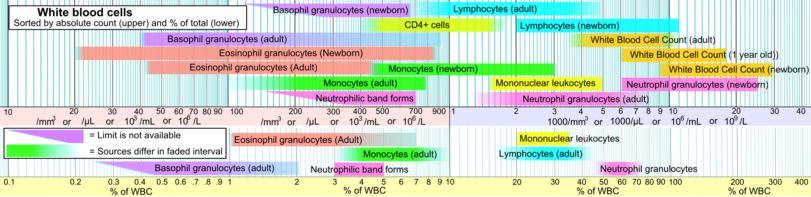
Below are blood reference ranges for various types leucocytes/WBCs.[7] The 2.5 percentile (right limits in intervals in image, showing 95% prediction intervals) is a common limit for defining leukocytosis.
References
- ^ Nicholson, R J; Kelly, K P; Grant, I S (25 February 1995). "Leucopenia associated with lamotrigine". BMJ. Retrieved 16 June 2010.
- ^ "Leukopenia and thrombocytopenia induced by etanercept: two case reports and literature review". 52 (1): 110–2. PMID 22286650.
{{cite journal}}:|access-date=requires|url=(help); Cite journal requires|journal=(help) - ^ "What causes low blood cell counts?". Retrieved March 3, 2012.
- ^ "Managing a Low White Blood Cell Count (Neutropenia)". Retrieved March 3, 2012.
- ^ http://toxsci.oxfordjournals.org/cgi/content/full/103/2/278
- ^ http://ibdcrohns.about.com/od/diagnostictesting/p/testwbc.htm
- ^ Specific references are found in article Reference_ranges_for_blood_tests#White_blood_cells_2.
External links
- . GPnotebook https://www.gpnotebook.co.uk/simplepage.cfm?ID=1355808838.
{{cite web}}: Missing or empty|title=(help) - 11-135a. at The Merck Manual of Diagnosis and Therapy Professional Edition
