Portal hypertension
| Portal hypertension | |
|---|---|
| Specialty | Gastroenterology, digestive system surgery |
Portal hypertension is hypertension (high blood pressure) in the hepatic portal system, which are the portal vein and its branches, which draining from most of the intestines to the liver. Portal hypertension is defined as a hepatic venous pressure gradient equal to or greater than 6 mmHg.[1] Cirrhosis (a form of chronic liver failure) is the most common cause of portal hypertension; other, less frequent causes are therefore grouped as non-cirrhotic portal hypertension. When it becomes severe enough to cause symptoms or complications, treatment may be given to decrease portal hypertension itself or to manage its complications.[citation needed]
Signs and symptoms
Signs and symptoms of portal hypertension include:
Causes
The causes for portal hypertension are classified as originating in the portal venous system before it reaches the liver (prehepatic causes), within the liver (intrahepatic) or between the liver and the heart (post-hepatic). The most common causes is cirrhosis (chronic liver failure). Other causes include:[2][5][6]
| Conditions associated with non-cirrhotic portal hypertension | |
|---|---|
| Prehepatic causes | Portal vein thrombosis or splenic vein thrombosis |
| Arteriovenous fistula | |
| Splenomegaly (increased portal blood flow) | |
| Hepatic causes | Any cause of cirrhosis, e.g. alcohol abuse, chronic viral hepatitis, biliary atresia, etc. |
| Primary biliary cirrhosis | |
| Primary sclerosing cholangitis | |
| Chronic pancreatitis | |
| Hereditary haemorrhagic telangiectasia | |
| Schistosomiasis | |
| Congenital hepatic fibrosis | |
| Nodular regenerative hyperplasia | |
| Fibrosis of space of Disse | |
| Granulomatous or infiltrative liver diseases (Gaucher, mucopolysaccharidosis, sarcoidosis, lymphoproliferative malignancies, amyloid deposition, …) | |
| Toxicity (from arsenic, copper, vinyl chloride monomers, mineral oil, vitamin A, azathioprine, dacarbazine, methotrexate, amiodarone, …) | |
| Viral hepatitis | |
| Fatty liver disease | |
| Veno-occlusive disease | |
| Budd-Chiari syndrome | |
| Posthepatic causes | Inferior vena cava obstruction |
| (Right-sided) heart failure, e.g. from constrictive pericarditis | |
| hepatic vein thrombosis |
Pathophysiology

The pathophysiology of portal hypertension is indicated by increasing vascular resistance via different etiologies; additionally, stellate cells and myofibroblasts are activated. Increased endogenous vasodilators in turn promote more blood flow in the portal veins.[2][7]
Nitric oxide is an endogenous vasodilator and it regulates intrahepatic vascular tone (it is produced from L-arginine). According to Maruyama, et al., in laboratory studies nitric oxide inhibition increases portal hypertension and hepatic response to norepinephrine is increased.[8]
Diagnosis

The diagnosis of portal hypertension can be done via HVPG (hepatic venous pressure gradient) measurement has been accepted as the gold standard for assessing the severity of portal hypertension. Portal hypertension is defined as HVPG greater than or equal to 5 mm Hg and is considered to be clinically significant when HVPG exceeds 10 to 12 mm Hg.[9]
In clinical practice the pressure is not measured directly until the decision to take a liver biopsy for suspected cirrhosis (chronic liver failure), or to place a transjugular intrahepatic portosystemic shunt has been made. Part of the procedure, a hepatic vein wedge pressure is measured with the assumption of no pressure drop across the liver yielding portal vein pressure.[medical citation needed]
Treatment
The treatment of portal hypertension is divided into:
Portosystemic shunts
Selective shunts select non-intestinal flow to be shunted to the systemic venous drainage while leaving the intestinal venous drainage to continue to pass through the liver. The most well known of this type is the splenorenal.[10] This connects the splenic vein to the left renal vein thus reducing portal system pressure while minimizing any encephalopathy. In an H-shunt, which could be mesocaval (from the superior mesenteric vein to the inferior vena cava) or could be, portocaval (from the portal vein to the inferior vena cava) a graft, either synthetic or the preferred vein harvested from somewhere else on the patient's body, is connected between the superior mesenteric vein and the inferior vena cava. The size of this shunt will determine how selective it is.[11][12]
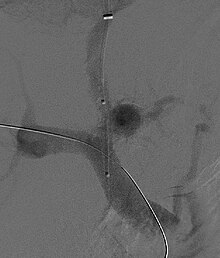
It should be noted that with the advent of transjugular intrahepatic portosystemic shunting (TIPS), portosystemic shunts are less performed. TIPS has the advantage of being easier to perform and doesn't disrupt the liver's vascularity.[13]
Prevention of bleeding
Both pharmacological (non-specific β-blockers, nitrate isosorbide mononitrate, vasopressin such as terlipressin) and endoscopic (banding ligation) treatment have similar results. TIPS (transjugular intrahepatic portosystemic shunting) is effective at reducing the rate of rebleeding.[14]
The management of active variceal bleeding includes administering vasoactive drugs (somatostatin, octreotide), endoscopic banding ligation, balloon tamponade and TIPS.[14][15]
Ascites
This should be gradual to avoid sudden changes in systemic volume status which can precipitate hepatic encephalopathy, renal failure and death. The management includes salt restriction, diuretics (spironolactone), paracentesis, and transjugular intrahepatic portosystemic shunt.[16]
Hepatic encephalopathy
A treatment plan may involve lactulose, enemas, and use of antibiotics such as rifaximin, neomycin, vancomycin, and the quinolones. Restriction of dietary protein was recommended but this is now refuted by a clinical trial which shows no benefit. Instead, the maintenance of adequate nutrition is now advocated.[17]
References
- ^ "Portal hypertension | Disease | Overview | Genetic and Rare Diseases Information Center (GARD) – an NCATS Program". rarediseases.info.nih.gov. Retrieved 2016-01-08.
- ^ a b c d e "Portal Hypertension. Learn about Portal Hypertension | Patient". Patient. Retrieved 2016-01-08.
- ^ "Spontaneous Bacterial Peritonitis". www.karger.com. Retrieved 2016-01-08.
- ^ Sun, Z; Migaly, J (March 2016). "Review of Hemorrhoid Disease: Presentation and Management". Clinics in colon and rectal surgery. 29 (1): 22–9. doi:10.1055/s-0035-1568144. PMID 26929748.
- ^ Bloom, S.; Kemp, W.; Lubel, J. (2015-01-01). "Portal hypertension: pathophysiology, diagnosis and management". Internal Medicine Journal. 45 (1): 16–26. doi:10.1111/imj.12590. ISSN 1445-5994.
- ^ Perkins, [edited by] Vinay Kumar, Abul K. Abbas, Jon C. Aster ; artist, James A. Robbins basic pathology (9th ed.). Philadelphia, PA: Elsevier/Saunders. p. 608. ISBN 978-1-4377-1781-5.
{{cite book}}:|first=has generic name (help)CS1 maint: multiple names: authors list (link)2013 - ^ "Portal Hypertension: Practice Essentials, Background, Anatomy".
{{cite journal}}: Cite journal requires|journal=(help) - ^ Maruyama, Hitoshi; Yokosuka, Osamu (2012). "Pathophysiology of Portal Hypertension and Esophageal Varices". International Journal of Hepatology. 2012: 1–7. doi:10.1155/2012/895787.
{{cite journal}}:|access-date=requires|url=(help)CS1 maint: unflagged free DOI (link) - ^ Al-Busafi SA, McNabb-Baltar J, Farag A, Hilzenrat N (2012). "Clinical manifestations of portal hypertension". Int J Hepatol. 2012: 203794. doi:10.1155/2012/203794. PMC 3457672. PMID 23024865.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Shah, Omar Javed; Robbani, Irfan (2005-01-01). "A Simplified Technique of Performing Splenorenal Shunt (Omar's Technique)". Texas Heart Institute Journal / from the Texas Heart Institute of St. Luke's Episcopal Hospital, Texas Children's Hospital. 32 (4): 549–554. ISSN 0730-2347. PMC 1351828. PMID 16429901.
- ^ Moore, Wesley S. (2012-11-23). Vascular and Endovascular Surgery: A Comprehensive Review. Elsevier Health Sciences. p. 851. ISBN 1455753866.
- ^ Yin, Lanning; Liu, Haipeng; Zhang, Youcheng; Rong, Wen (2013). "The Surgical Treatment for Portal Hypertension: A Systematic Review and Meta-Analysis". ISRN Gastroenterology. 2013: 1–10. doi:10.1155/2013/464053.
{{cite journal}}:|access-date=requires|url=(help)CS1 maint: unflagged free DOI (link) - ^ Pomier-Layrargues, Gilles; Bouchard, Louis; Lafortune, Michel; Bissonnette, Julien; Guérette, Dave; Perreault, Pierre (2012). "The Transjugular Intrahepatic Portosystemic Shunt in the Treatment of Portal Hypertension: Current Status". International Journal of Hepatology. 2012: 1–12. doi:10.1155/2012/167868.
{{cite journal}}:|access-date=requires|url=(help)CS1 maint: unflagged free DOI (link) - ^ a b Bari, Khurram; Garcia-Tsao, Guadalupe (2012-03-21). "Treatment of portal hypertension". World Journal of Gastroenterology : WJG. 18 (11): 1166–1175. doi:10.3748/wjg.v18.i11.1166. ISSN 1007-9327. PMC 3309905. PMID 22468079.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ "Portal Hypertension Medication: Somatostatin Analogs, Beta-Blockers, Nonselective, Vasopressin-Related, Vasodilators". emedicine.medscape.com. Retrieved 2016-01-08.
- ^ Dib, Nina; Oberti, Frédéric; Calès, Paul (2006-05-09). "Current management of the complications of portal hypertension: variceal bleeding and ascites". Canadian Medical Association Journal. 174 (10): 1433–1443. doi:10.1503/cmaj.051700. ISSN 0820-3946. PMC 1455434. PMID 16682712.
- ^ http://www.patient.info/doctor/Hepatic-Encephalopathy.htm
