Streptococcus
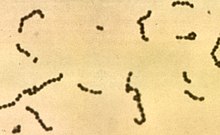
Streptococcus is a genus of gram-positive coccus (plural cocci), or spherical bacteria, that belongs to the family Streptococcaceae, within the order Lactobacillales (lactic acid bacteria), in the phylum Firmicutes.[3] Cell division in streptococci occurs along a single axis, so as they grow they tend to form pairs or chains that may appear bent or twisted. (Contrast with that of staphylococci, which divide along multiple axes, thereby generating irregular grape-like clusters of cells.)
The term was coined in 1877 by Viennese surgeon Albert Theodor Billroth (1829–1894),[4] by combining the prefix "strepto-" (from Ancient Greek: στρεπτός, romanized: streptós, lit. 'easily twisted, pliant'[5]), together with the suffix "-coccus" (from Modern Latin: coccus, from Ancient Greek: κόκκος, romanized: kókkos, lit. 'grain, seed, berry'.[6])
Most streptococci are oxidase-negative and catalase-negative, and many are facultative anaerobes (capable of growth both aerobically and anaerobically).
In 1984, many bacteria formerly grouped in the genus Streptococcus were separated out into the genera Enterococcus and Lactococcus.[7] Currently, over 50 species are recognised in this genus. This genus has been found to be part of the salivary microbiome.[8]
Pathogenesis and classification
In addition to streptococcal pharyngitis (strep throat), certain Streptococcus species are responsible for many cases of pink eye,[9] meningitis, bacterial pneumonia, endocarditis, erysipelas, and necrotizing fasciitis (the 'flesh-eating' bacterial infections). However, many streptococcal species are not pathogenic, and form part of the commensal human microbiota of the mouth, skin, intestine, and upper respiratory tract. Furthermore, streptococci are a necessary ingredient in producing Emmentaler ("Swiss") cheese.
Species of Streptococcus are classified based on their hemolytic properties.[10] Alpha-hemolytic species cause oxidization of iron in hemoglobin molecules within red blood cells, giving it a greenish color on blood agar. Beta-hemolytic species cause complete rupture of red blood cells. On blood agar, this appears as wide areas clear of blood cells surrounding bacterial colonies. Gamma-hemolytic species cause no hemolysis.
Beta-hemolytic streptococci are further classified by Lancefield grouping, a serotype classification (that is, describing specific carbohydrates present on the bacterial cell wall).[11] The 20 described serotypes are named Lancefield groups A to V (excluding I and J). This system of classification was developed by Rebecca Lancefield, a scientist at Rockefeller University.
In the medical setting, the most important groups are the alpha-hemolytic streptococci S. pneumoniae and Streptococcus viridans group, and the beta-hemolytic streptococci of Lancefield groups A and B (also known as “group A strep” and “group B strep”).
Table: Medically relevant streptococci (not all are alpha hemolytic)[10]
| Species | Host | Disease |
| S. pyogenes | human | pharyngitis, cellulitis |
| S. agalactiae | human, cattle | neonatal meningitis and sepsis |
| S. dysgalactiae | human, animals | endocarditis, bacteremia, pneumonia, meningitis, respiratory infections |
| S. bovis | human, animals | biliary or urinary tract infections, endocarditis |
| S. anginosus | human, animals | subcutaneous/organ abscesses, meningitis, respiratory infections |
| S. sanguinis | human | endocarditis, dental caries |
| S. suis | swine | meningitis |
| S. mitis | human | endocarditis |
| S. mutans | human | dental caries |
| S. pneumoniae | human | pneumonia |
Alpha-hemolytic
When alpha hemolysis (α-hemolysis) is present, the agar under the colony will appear dark and greenish due to the conversion of hemoglobin to green biliverdin. Streptococcus pneumoniae and a group of oral streptococci (Streptococcus viridans or viridans streptococci) display alpha hemolysis. Alpha-hemolysis is also termed incomplete hemolysis and partial hemolysis because the cell membrane of the red blood cells are left intact. This is also sometimes called green hemolysis because of the color change in the agar.
Pneumococci
- S. pneumoniae (sometimes called pneumococcus), is a leading cause of bacterial pneumonia and occasional etiology of otitis media, sinusitis, meningitis, and peritonitis. Inflammation is thought to be the major cause of how pneumococci cause disease, hence the tendency of diagnoses associated with them to involve inflammation.
The viridans group: alpha-hemolytic
- The viridans streptococci are a large group of commensal bacteria, that are either α-hemolytic, producing a green coloration on blood agar plates (hence the name "viridans", from Latin vĭrĭdis, green), or nonhemolytic. They possess no Lancefield antigens.[3]
Beta-hemolytic
Beta hemolysis (β-hemolysis), sometimes called complete hemolysis, is a complete lysis of red cells in the media around and under the colonies: the area appears lightened (yellow) and transparent. Streptolysin, an exotoxin, is the enzyme produced by the bacteria which causes the complete lysis of red blood cells. There are two types of streptolysin: Streptolysin O (SLO) and streptolysin S (SLS). Streptolysin O is an oxygen-sensitive cytotoxin, secreted by most Group A Streptococcus (GAS), and interacts with cholesterol in the membrane of eukaryotic cells (mainly red and white blood cells, macrophages, and platelets), and usually results in β-hemolysis under the surface of blood agar. Streptolysin S is an oxygen-stable cytotoxin also produced by most GAS strains which results in clearing on the surface of blood agar. SLS affects immune cells, including polymorphonuclear leukocytes and lymphocytes, and is thought to prevent the host immune system from clearing infection. Streptococcus pyogenes, or GAS, displays beta hemolysis.
Some weakly beta-hemolytic species cause intense beta hemolysis when grown together with a strain of Staphylococcus. This is called the CAMP test. Streptococcus agalactiae displays this property. Clostridium perfringens can be identified presumptively with this test. Listeria monocytogenes is also positive on sheep's blood agar.

Group A
Group A S. pyogenes (GAS) is the causative agent in a wide range of group A streptococcal infections. These infections may be noninvasive or invasive. The noninvasive infections tend to be more common and less severe. The most common of these infections include streptococcal pharyngitis (strep throat) and impetigo.[12] Scarlet fever is also a noninvasive infection, but has not been as common in recent years.
The invasive infections caused by group A β-hemolytic streptococci tend to be more severe and less common. This occurs when the bacterium is able to infect areas where it is not usually found, such as the blood and the organs.[13] The diseases that may be caused include streptococcal toxic shock syndrome, necrotizing fasciitis, pneumonia, and bacteremia.[12] Globally, GAS has been estimated to cause more than 500,000 deaths every year, making it one of the world's leading pathogens.[12]
Additional complications may be caused by GAS, namely acute rheumatic fever and acute glomerulonephritis. Rheumatic fever, a disease that affects the joints, kidneys, and heart valves, is a consequence of untreated strep A infection caused not by the bacterium itself. Rheumatic fever is caused by the antibodies created by the immune system to fight off the infection cross-reacting with other proteins in the body. This "cross-reaction" causes the body to essentially attack itself and leads to the damage above. A similar autoimmune mechanism initiated by Group A beta-hemolytic streptococcal (GABHS) infection is hypothesized to cause pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections (PANDAS), wherein autoimmune antibodies affect the basal ganglia, causing rapid onset of psychiatric, motor, sleep, and other symptoms in pediatric patients.
GAS infection is generally diagnosed with a rapid strep test or by culture.
Group B
S. agalactiae, or group B Streptococcus, GBS, causes pneumonia and meningitis in neonates and the elderly, with occasional systemic bacteremia. They can also colonize the intestines and the female reproductive tract, increasing the risk for premature rupture of membranes during pregnancy, and transmission of the organism to the infant. The American Congress of Obstetricians and Gynecologists (formerly the American College of Obstetricians and Gynecologists), American Academy of Pediatrics, and the Centers for Disease Control recommend all pregnant women between 35 and 37 weeks gestation to be tested for GBS. Women who test positive should be given prophylactic antibiotics during labor, which will usually prevent transmission to the infant.[14]
The United Kingdom has chosen to adopt a risk factor-based protocol, rather than the culture-based protocol followed in the US. Current guidelines state that if one or more of the following risk factors is present, then the woman should be treated with intrapartum antibiotics:
- Preterm labour (<37 weeks)
- Prolonged rupture of membranes (>18 hours)
- Intrapartum fever (>38C)[vague]
- Prior GBS affected infante[vague]
- GBS bacteriuria during this pregnancy
This protocol results in treatment[vague] of 15–20% of pregnant women and prevention of 65–70% of cases of early onset GBS sepsis.[15]
Group C
This group includes S. equi, which causes strangles in horses,[16] and S. zooepidemicus—S. equi is a clonal descendent or biovar of the ancestral S. zooepidemicus—which causes infections in several species of mammals, including cattle and horses. S. dysgalactiae[contradictory] is also a member of group C, beta-haemolytic streptococci that can cause pharyngitis and other pyogenic infections similar to group A streptococci.
Group D (enterococci)
Many former group D streptococci have been reclassified and placed in the genus Enterococcus (including E. faecalis, E. faecium, E. durans, and E. avium).[17] For example, Streptococcus faecalis is now Enterococcus faecalis. E. faecalis is sometimes alpha hemolytic and E. faecium is sometimes beta hemolytic.[18]
The remaining nonenterococcal group D strains include Streptococcus bovis and Streptococcus equinus.
Nonhemolytic streptococci rarely cause illness. However, weakly hemolytic group D beta-hemolytic streptococci and Listeria monocytogenes (which is actually a Gram-positive bacillus) should not be confused with nonhemolytic streptococci.
Group F streptococci
Group F streptococci were first described in 1934 by Long and Bliss amongst the "minute haemolytic streptococci".[19] They are also known as Streptococcus anginosus (according to the Lancefield classification system) or as members of the S. milleri group (according to the European system).
Group G streptococci
These streptococci are usually, but not exclusively, beta-hemolytic. Streptococcus dysgalactiae[contradictory] is the predominant species encountered, particularly in human disease. S. canis is an example of a GGS which is typically found on animals, but can cause infection in humans. S. phocae is a GGS subspecies that has been found in marine mammals and marine fish species. In marine mammals it has been mainly associated with meningoencephalitis, septicemia, and endocarditis, but is also associated with many other pathologies. Its environmental reservoir and means of transmission in marine mammals is not well characterized.
Group H streptococci
Group H streptococci cause infections in medium-sized canines. Group H streptococci rarely cause illness unless a human has direct contact with the mouth of a canine. One of the most common ways this can be spread is human-to-canine, mouth-to-mouth contact. However, the canine may lick the human's hand and infection can be spread, as well.[20]
Molecular taxonomy and phylogenetics
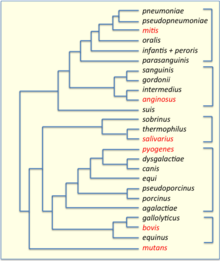
Streptococci have been divided into six groups on the basis of their 16S rDNA sequences: S. anginosus, S.bovis, S. mitis, S. mutans, S. pyogenes and S. salivarius.[22] The 16S groups have been confirmed by whole genome sequencing (see figure). The important pathogens S. pneumoniae and S. pyogenes belong to the S. mitis and S. pyogenes groups, respectively,[23] while the causative agent of dental caries, Streptococcus mutans, is basal to the Streptococcus group.
Genomics

The genomes of hundreds of species have been sequenced.[25] Most Streptococcus genomes are 1.8 to 2.3 Mb in size and encode 1,700 to 2,300 proteins. Some important genomes are listed in the table.[26] The four species shown in the table (S. pyogenes, S. agalactiae, S. pneumoniae, and S. mutans) have an average pairwise protein sequence identity of about 70%.[26]
| feature | S. pyogenes | S. agalactiae | S. pneumoniae | S. mutans |
|---|---|---|---|---|
| base pairs | 1,852,442 | 2,211,488 | 2,160,837 | 2,030,921 |
| ORFs | 1792 | 2118 | 2236 | 1963 |
| prophages | yes | no | no | no |
Bacteriophage
Bacteriophages have been described for many species of Streptococcus. 18 prophages have been described in S. pneumoniae that range in size from 38 to 41 kb in size, encoding from 42 to 66 genes each.[citation needed] Some of the first Streptococcus phages discovered were Dp-1[27] and ω1.[28][29] In 1981 the Cp (Complutense phage) family was discovered with Cp-1 as its first member.[30] Dp-1 and Cp-1 infect both S. pneumoniae and S. mitis.[31] However, the host ranges of most Streptococcus phages have not been investigated systematically.
Natural genetic transformation
Natural genetic transformation involves the transfer of DNA from one bacterium to another through the surrounding medium. Transformation is a complex process dependent on expression of numerous genes. To be capable of transformation a bacterium must enter a special physiologic state referred to as competence. S. pneumoniae, S. mitis and S. oralis can become competent, and as a result actively acquire homologous DNA for transformation by a predatory fratricidal mechanism [32] This fratricidal mechanism mainly exploits non-competent siblings present in the same niche [33] Among highly competent isolates of S. pneumoniae, Li et al.[34] showed that nasal colonization fitness and virulence (lung infectivity) depend on an intact competence system. Competence may allow the streptococcal pathogen to use external homologous DNA for recombinational repair of DNA damages caused by the hosts oxidative attack [35]
See also
References
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad ae af ag ah ai aj ak al am an ao ap aq ar as at au av aw ax ay az ba bb bc bd be bf bg bh bi bj bk bl bm bn bo bp bq br bs bt Parte, A.C. "Streptococcus". www.bacterio.net.
- ^ LPSN entry for Streptococcus
- ^ a b Ryan KJ, Ray CG, eds. (2004). Sherris Medical Microbiology (4th ed.). McGraw Hill. pp. 293–4. ISBN 0-8385-8529-9.
- ^ "streptococcus". Online Etymology Dictionary. Retrieved 25 July 2018.
{{cite web}}: Cite has empty unknown parameter:|dead-url=(help) - ^ στρεπτός in Liddell, Henry George; Scott, Robert (1940) A Greek–English Lexicon, revised and augmented throughout by Jones, Sir Henry Stuart, with the assistance of McKenzie, Roderick. Oxford: Clarendon Press. In the Perseus Digital Library, Tufts University.
- ^ κόκκος in Liddell and Scott
- ^ Facklam R (October 2002). "What happened to the streptococci: overview of taxonomic and nomenclature changes". Clin. Microbiol. Rev. 15 (4): 613–30. doi:10.1128/CMR.15.4.613-630.2002. PMC 126867. PMID 12364372.
- ^ Wang, Kun; Lu, Wenxin; Tu, Qichao; Ge, Yichen; He, Jinzhi; Zhou, Yu; Gou, Yaping; Nostrand, Joy D Van; Qin, Yujia; Li, Jiyao; Zhou, Jizhong; Li, Yan; Xiao, Liying; Zhou, Xuedong (10 March 2016). "Preliminary analysis of salivary microbiome and their potential roles in oral lichen planus". Scientific Reports. 6 (1). doi:10.1038/srep22943. PMC 4785528. PMID 26961389. Retrieved 6 May 2017.
- ^ http://www.medicinenet.com/pink_eye/article.htm
- ^ a b Patterson MJ (1996). Baron S; et al. (eds.). Streptococcus. In: Baron's Medical Microbiology (4th ed.). Univ of Texas Medical Branch. (via NCBI Bookshelf) ISBN 0-9631172-1-1.
- ^ Facklam R (2002). "What happened to the streptococci: overview of taxonomic and nomenclature changes". Clin Microbiol Rev. 15 (4): 613–30. doi:10.1128/CMR.15.4.613-630.2002. PMC 126867. PMID 12364372.
- ^ a b c Cohen-Poradosu R, Kasper DL (2007). "Group A streptococcus epidemiology and vaccine implications". Clin. Infect. Dis. 45 (7): 863–5. doi:10.1086/521263. PMID 17806050.
- ^ "Streptococcal Infections (Invasive Group A Strep)". New York City Department of Health and Mental Hygiene. Retrieved 21 November 2012.
- ^ Schrag S, Gorwitz R, Fultz-Butts K, Schuchat A (2002). "Prevention of perinatal group B streptococcal disease. Revised guidelines from CDC". MMWR Recomm Rep. 51 (RR-11): 1–22. PMID 12211284.
- ^ Norwitz, E.R.; Schorge, J.O. (2013). Obstetrics and Gynaecology at a Glance (4th ed.). John Wiley & Sons LTD.
- ^ Harrington DJ, Sutcliffe IC, Chanter N (2002). "The molecular basis of Streptococcus equi infection and disease". Microbes Infect. 4 (4): 501–10. doi:10.1016/S1286-4579(02)01565-4. PMID 11932201.
- ^ Köhler W (June 2007). "The present state of species within the genera Streptococcus and Enterococcus". International Journal of Medical Microbiology. 297 (3): 133–50. doi:10.1016/j.ijmm.2006.11.008. PMID 17400023.
- ^ Holt et al. (1994). Bergey's Manual of Determinative Bacteriology (9th ed.). Lippincott Williams & Wilkins. ISBN 0-683-00603-7
- ^ Whitworth JM (November 1990). "Lancefield group F and related streptococci" (PDF). J. Med. Microbiol. 33 (3): 135–51. doi:10.1099/00222615-33-3-135. PMID 2250284.
- ^ "Bacterial Infection (Streptococcus) in Dogs". petmd.com. Retrieved 12 December 2014.
- ^ "Bacteria-Firmicutes-Bacilli-Lactobacillales-Streptococcaceae-Streptococcus". PATRIC, University of Chicago. Retrieved 12 December 2014.
- ^ Kawamura Y, Hou XG, Sultana F, Miura H, Ezaki T (1995). "Determination of 16S rRNA sequences of Streptococcus mitis and Streptococcus gordonii and phylogenetic relationships among members of the genus Streptococcus". Int J Syst Bacteriol. 45: 406–408. doi:10.1099/00207713-45-2-406. PMID 7537076.
- ^ Liu, D., Molecular Detection of Human Bacterial Pathogens (Boca Raton: CRC Press, 2011), p. 324.
- ^ Xu, P; Alves, J. M.; Kitten, T; Brown, A; Chen, Z; Ozaki, L. S.; Manque, P; Ge, X; Serrano, M. G.; Puiu, D; Hendricks, S; Wang, Y; Chaplin, M. D.; Akan, D; Paik, S; Peterson, D. L.; MacRina, F. L.; Buck, G. A. (2007). "Genome of the opportunistic pathogen Streptococcus sanguinis". Journal of Bacteriology. 189 (8): 3166–75. doi:10.1128/JB.01808-06. PMC 1855836. PMID 17277061.
- ^ Streptococcus genomes and related information at PATRIC
- ^ a b Ferretti JJ, Ajdic D, McShan WM (2004). "Comparative genomics of streptococcal species". The Indian journal of medical research. 119 Suppl: 1–6. PMID 15232152.
- ^ McDonnell M, Ronda C, Tomasz A (1975) “Diplophage”: a bacteriophage of Diplococcus pneumoniae. Virology 63:577–582
- ^ Tiraby JG, Tiraby E, Fox MS (1975) Pneumococcal bacteriophages. Virology 68:566–569
- ^ López R (2004). "Streptococcus pneumoniae and its bacteriophages: one long argument". Int. Microbiol. 7 (3): 163–71. PMID 15492930.
- ^ Ronda C, López R, García E (1981). "Isolation and characterization of a new bacteriophage, Cp-1, infecting Streptococcus pneumoniae". J. Virol. 40 (2): 551–9. PMC 256658. PMID 6275103.
- ^ Ouennane S, Leprohon P, Moineau S (2015). "Diverse virulent pneumophages infect Streptococcus mitis". PLoS ONE. 10 (2): e0118807. doi:10.1371/journal.pone.0118807. PMC 4334900. PMID 25692983.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Johnsborg O, Eldholm V, Bjørnstad ML, Håvarstein LS (2008). "A predatory mechanism dramatically increases the efficiency of lateral gene transfer in Streptococcus pneumoniae and related commensal species". Mol. Microbiol. 69 (1): 245–53. doi:10.1111/j.1365-2958.2008.06288.x. PMID 18485065.
- ^ Claverys JP, Håvarstein LS (2007). "Cannibalism and fratricide: mechanisms and raisons d'être". Nat. Rev. Microbiol. 5 (3): 219–29. doi:10.1038/nrmicro1613. PMID 17277796.
- ^ Li G, Liang Z, Wang X, Yang Y, Shao Z, Li M, Ma Y, Qu F, Morrison DA, Zhang JR (2016). "Addiction of Hypertransformable Pneumococcal Isolates to Natural Transformation for In Vivo Fitness and Virulence". Infect. Immun. 84 (6): 1887–901. doi:10.1128/IAI.00097-16. PMC 4907133. PMID 27068094.
- ^ Michod RE, Bernstein H, Nedelcu AM (2008). "Adaptive value of sex in microbial pathogens". Infect. Genet. Evol. 8 (3): 267–85. doi:10.1016/j.meegid.2008.01.002. PMID 18295550.
External links
- Streptococcus genomes and related information at PATRIC, a Bioinformatics Resource Center funded by NIAID
- "Adoption of perinatal group B streptococcal disease prevention recommendations by prenatal-care providers—Connecticut and Minnesota, 1998". MMWR Morb. Mortal. Wkly. Rep. 49 (11): 228–32. March 2000. PMID 10763673.
- The Canadian Strep B Foundation
- The UK Group B Strep Support charity