Vaccination: Difference between revisions
| [pending revision] | [pending revision] |
m Reverted edits by 193.110.107.251 (talk) to last version by Mathiaseu |
|||
| Line 104: | Line 104: | ||
{{Commons category|Vaccinations}} |
{{Commons category|Vaccinations}} |
||
* [http://www.vrc.nih.gov Vaccine Research Center]: Information regarding preventative vaccine research studies |
* [http://www.vrc.nih.gov Vaccine Research Center]: Information regarding preventative vaccine research studies |
||
* [http://healthmad.com/children/side-effects-of-vaccines-in-kids Side Effects of Vaccines in Kids] |
|||
* [http://vaccines.org/ The Vaccine Page] links to resources in many countries. |
* [http://vaccines.org/ The Vaccine Page] links to resources in many countries. |
||
* [http://www.immunisation.nhs.uk/article.php?id=97 Immunisation] Immunisation schedule for children in the UK. Published by the UK Department of Health. |
* [http://www.immunisation.nhs.uk/article.php?id=97 Immunisation] Immunisation schedule for children in the UK. Published by the UK Department of Health. |
||
Revision as of 08:57, 26 November 2009

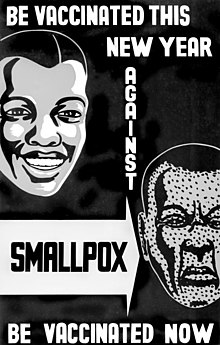
Vaccination is the administration of antigenic material (the vaccine) to produce immunity to a disease. Vaccines can prevent or ameliorate the effects of infection by a pathogen. Vaccination is generally considered to be the most effective and cost-effective method of preventing infectious diseases. The material administrated can either be live but weakened forms of pathogens (bacteria or viruses), killed or inactivated forms of these pathogens, or purified material such as proteins. Smallpox was the first disease people tried to prevent by purposely inoculating themselves with other types of infections; smallpox inoculation was started in China or India before 200 BC.[1] In 1718, Lady Mary Wortley Montagu reported that the Turks had a habit of deliberately inoculating themselves with fluid taken from mild cases of smallpox, and that she had inoculated her own children.[2] Before 1796 when British physician Edward Jenner tested the possibility of using the cowpox vaccine as an immunisation for smallpox in humans for the first time, at least six people had done the same several years earlier: a person whose identity is unknown, England, (about 1771); a Mrs. Sevel, Germany (about 1772); a Mr. Jensen, Germany (about 1770); Benjamin Jesty, England, in 1774; a Mrs. Rendall, England (about 1782); and Peter Plett, Germany, in 1791.[3]
The word vaccination was first used by Edward Jenner in 1796. Louis Pasteur furthered the concept through his pioneering work in microbiology. Vaccination (Template:Lang-la) is so named because the first vaccine was derived from a virus affecting cows—the relatively benign cowpox virus—which provides a degree of immunity to smallpox, a contagious and deadly disease. In common speech, 'vaccination' and 'immunization' generally have the same colloquial meaning. This distinguishes it from inoculation which uses unweakened live pathogens, although in common usage either is used to refer to an immunization. The word "vaccination" was originally used specifically to describe the injection of smallpox vaccine.[1][3]
Vaccination efforts have been met with some controversy since their inception, on ethical, political, medical safety, religious, and other grounds. In rare cases, vaccinations can injure people and they may receive compensation for those injuries. Early success and compulsion brought widespread acceptance, and mass vaccination campaigns were undertaken which are credited with greatly reducing the incidence of many diseases in numerous geographic regions.
Triggering immune sensitization
In the generic sense, the process of artificial induction of immunity, in an effort to protect against infectious disease, works by 'priming' the immune system with an 'immunogen'. Stimulating immune response, via use of an infectious agent, is known as immunization. Vaccinations involve the administration of one or more immunogens, which can be administered in several forms.
Some modern vaccines are administered after the patient already has contracted a disease, as in the cases of experimental AIDS, cancer and Alzheimer's disease vaccines. Vaccinia given after exposure to smallpox, within the first four days, is reported to attenuate the disease considerably, and vaccination within the first week is known to be beneficial to a degree. The first rabies immunization was given by Louis Pasteur to a child bitten by a rabid dog, subsequently post-exposure immunization to rabies has generally been followed by survival. The essential empiricism behind such immunizations is that the vaccine triggers an immune response more rapidly than the natural infection itself.
Most vaccines are given by hypodermic injection as they are not absorbed reliably through the intestines. Live attenuated polio, some typhoid and some cholera vaccines are given orally in order to produce immunity based in the bowel.
Types of vaccinations
All vaccinations work by presenting a foreign antigen to the immune system in order to evoke an immune response, but there are several ways to do this. The four main types that are currently in clinical use are as follows:
- An inactivated vaccine consists of virus particles which are grown in culture and then killed using a method such as heat or formaldehyde. The virus particles are destroyed and cannot replicate, but the virus capsid proteins are intact enough to be recognized and remembered by the immune system and evoke a response. When manufactured correctly, the vaccine is not infectious, but improper inactivation can result in intact and infectious particles. Since the properly produced vaccine does not reproduce, booster shots are required periodically to reinforce the immune response.
- In an attenuated vaccine, live virus particles with very low virulence are administered. They will reproduce, but very slowly. Since they do reproduce and continue to present antigen beyond the initial vaccination, boosters are required less often. These vaccines are produced by passaging virus in cell cultures, in animals, or at suboptimal temperatures, allowing selection of less virulent strains, or by mutagenesis or targeted deletions in genes required for virulence. There is a small risk of reversion to virulence, this risk is smaller in vaccines with deletions. Attenuated vaccines also cannot be used by immunocompromised individuals.
- Virus-like particle vaccines consist of viral protein(s) derived from the structural proteins of a virus. These proteins can self-assemble into particles that resemble the virus from which they were derived but lack viral nucleic acid, meaning that they are not infectious. Because of their highly repetitive, multivalent structure, virus-like particles are typically more immunogenic than subunit vaccines (described below). The human papillomavirus and Hepatitis B virus vaccines are two virus-like particle-based vaccines currently in clinical use.
- A subunit vaccine presents an antigen to the immune system without introducing viral particles, whole or otherwise. One method of production involves isolation of a specific protein from a virus or bacteria (such as a bacterial toxin) and administering this by itself. A weakness of this technique is that isolated proteins may have a different three-dimensional structure than the protein in its normal context, and will induce antibodies that may not recognize the infectious organism. In addition, subunit vaccines often elicit weaker antibody responses than the other classes of vaccines.
A number of other vaccine strategies are under experimental investigation. These include DNA vaccination and recombinant viral vectors.
History

Early forms of vaccination were developed in ancient China as early as 200 B.C.[1] Scholar Ole Lund comments: "The earliest documented examples of vaccination are from India and China in the 17th century, where vaccination with powdered scabs from people infected with smallpox was used to protect against the disease. Smallpox used to be a common disease throughout the world and 20% to 30% of infected persons died from the disease. Smallpox was responsible for 8 to 20% of all deaths in several European countries in the 18th century. The tradition of vaccination may have originated in India in AD 1000."[4] The mention of vaccination in the Sact'eya Grantham, an Ayurvedic text, was noted by the French scholar Henri Marie Husson in the journal Dictionaire des sciences me`dicales.[5] Almroth Wright, the professor of pathology at Netley, further helped shape the future of vaccination by conducting limited experiments on the professional staff at Netly, including himself. The outcome of these experiments resulted in further development of vaccination in Europe.[6] The Anatolian Ottoman Turks knew about methods of vaccination about a hundred years before Edward Jenner to whom the discovery is attributed. They called vaccination Ashi or engrafting, which they used to apply to their children with cowpox taken from the breast of cattle. This kind of vaccination and other forms of variolation were introduced into England by Lady Montagu, a famous English letter-writer and wife of the English ambassador at Istanbul between 1716 and 1718, who'd almost died from smallpox as a young adult and was physically scarred from it. She came across the Turkish methods of vaccination, consenting to have her son inoculated by the Embassy surgeon Charles Maitland in the Turkish way. Lady Montagu wrote to her sister and friends in England describing the process in details. On her return to England she continued to propagate the Turkish tradition of vaccination and had many of her relatives inoculated. The breakthrough came when a scientific description of the vaccination operation was submitted to the Royal Society in 1724 by Dr Emmanual Timoni, who had been the Montagu’s family physician in Istanbul. Inoculation was adopted both in England and in France nearly half a century before Jenner's famous smallpox vaccine of 1796.[7]
Since then vaccination campaigns have spread throughout the globe, sometimes prescribed by law or regulations (See Vaccination Acts). Vaccines are now used to fight a wide variety of disease threats besides smallpox. Louis Pasteur further developed the technique during the 19th century, extending its use to protecting against bacterial anthrax and viral rabies. The method Pasteur used entailed treating the infectious agents for those diseases so they lost the ability to cause serious disease. Pasteur adopted the name vaccine as a generic term in honor of Jenner's discovery, which Pasteur's work built upon.

Prior to vaccination with cowpox, the only known protection against smallpox was inoculation or variolation (Variola - the Smallpox viruses) where a small amount of live smallpox virus was administered to the patient; this carried the serious risk that the patient would be killed or seriously ill. The death rate from variolation was reported to be around a tenth of that from natural infection with Variola, and the immunity provided was considered quite reliable. Factors contributing to the efficacy of variolation probably include the choices of Variola Minor strains used, the relatively low number of cells infected in the first phase of multiplication following initial exposure, and the exposure route used, via the skin or nasal lining rather than inhalation of droplets into the lungs.
Consistency would suggest the activity should have predated Jenner's description of an effective vaccination system, and there is some history relating to opposition to the older and more hazardous procedure of variolation [citation needed].
In modern times, the first vaccine-preventable disease targeted for eradication was smallpox. The World Health Organization (WHO) coordinated the global effort to eradicate this disease. The last naturally occurring case of smallpox occurred in Somalia in 1977.
In 1988, the governing body of WHO targeted polio for eradication by the year 2000. Although the target was missed, eradication is very close. The next eradication target would most likely be measles, which has declined since the introduction of measles vaccination in 1963.
In 2000, the Global Alliance for Vaccines and Immunization was established to strengthen routine vaccinations and introduce new and under-used vaccines in countries with a per capita GDP of under US$1000. GAVI is now entering its second phase of funding, which extends through 2014.
Policies and enforcement
In an attempt to eliminate the risk of outbreaks of some diseases, at various times several governments and other institutions have instituted policies requiring vaccination for all people. For example, an 1853 law required universal vaccination against smallpox in England and Wales, with fines levied on people who did not comply. Common contemporary U.S. vaccination policies require that children receive common vaccinations before entering school. Most other countries also have some compulsory vaccinations.
Beginning with early vaccination in the nineteenth century, these policies led to resistance from a variety of groups, collectively called anti-vaccinationists, who objected on ethical, political, medical safety, religious, and other grounds. Common objections are that compulsory vaccination represents excessive government intervention in personal matters, or that the proposed vaccinations are not sufficiently safe.[8] Many modern vaccination policies allow exemptions for people who have compromised immune systems, allergies to the components used in vaccinations or strongly-held objections.[9]
Allegations of vaccine injuries in recent decades have appeared in litigation in the U.S. Some families have won substantial awards from sympathetic juries, even though most public health officials believed that the claims of injuries were unfounded.[10] In response, several vaccine makers stopped production, threatening public health, and laws were passed to shield makers from liabilities stemming from vaccine injury claims.[10]
Adjuvants and preservatives
Vaccines typically contain one or more adjuvants, used to boost the immune response. Tetanus toxoid, for instance, is usually adsorbed onto alum. This presents the antigen in such a way as to produce a greater action than the simple aqueous tetanus toxoid. People who get an excessive reaction to adsorbed tetanus toxoid may be given the simple vaccine when time for a booster occurs.
In the preparation for the 1990 Gulf campaign, Pertussis vaccine (not acellular) was used as an adjuvant for Anthrax vaccine. This produces a more rapid immune response than giving only the Anthrax, which is of some benefit if exposure might be imminent.
They may also contain preservatives, which are used to prevent contamination with bacteria or fungi. Until recent years, the preservative thiomersal was used in many vaccines that did not contain live virus. As of 2005[update], the only childhood vaccine in the U.S. that contains thiomersal in greater than trace amounts is the influenza vaccine [1], which is currently recommended only for children with certain risk factors.[11] The UK is considering Influenza immunisation in children perhaps as soon as in 2006-7. Single-dose Influenza vaccines supplied in the UK do not list Thiomersal (its UK name) in the ingredients. Preservatives may be used at various stages of production of vaccines, and the most sophisticated methods of measurement might detect traces of them in the finished product, as they may in the environment and population as a whole [2].
Methods of administration
A vaccine administration may be oral, by injection (intramuscular, intradermal, subcutaneous), by puncture, transdermal or intranasal.[12]
Research
Some major contemporary research in vaccination focuses on development of vaccinations for diseases including HIV and malaria.
Vaccine is an international peer-reviewed journal for vaccination researchers, indexed in Medline pISSN: 0264-410X.
See also
- Influenza vaccine
- H5N1 flu vaccine clinical trials
- Vaccine trial
- Vaccination of dogs
- Feline vaccination
- Immunization during pregnancy
References
- ^ a b c Lombard M, Pastoret PP, Moulin AM (2007). "A brief history of vaccines and vaccination". Rev. - Off. Int. Epizoot. 26 (1): 29–48. PMID 17633292.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Behbehani AM (1983). "The smallpox story: life and death of an old disease". Microbiol. Rev. 47 (4): 455–509. PMID 6319980.
- ^ a b Plett PC (2006). "[Peter Plett and other discoverers of cowpox vaccination before Edward Jenner]". Sudhoffs Arch (in German). 90 (2): 219–32. PMID 17338405. Retrieved 2008-03-12.
- ^ Lund, Ole; Nielsen, Morten Strunge and Lundegaard, Claus (2005). Immunological Bioinformatics. MIT Press. ISBN 0262122804
- ^ Chaumeton, F.P.; F.V. Me`rat de Vaumartoise. Dictionaire des sciences me`dicales. Paris: C.L.F. Panckoucke, 1812-1822, lvi (1821).
- ^ Curtin, Phillip (1998). "Disease and Empire: The Health of European Troops in the Conquest of Africa". Cambridge University Press. ISBN 0521598354
- ^ Anthony Henricy (ed.) (1796). Lady Mary Wortley Montagu,Letters of the Right Honourable Lady Mary Wortley Montagu:Written During her Travels in Europe,Asia and Africa. Vol. 1. pp. 167–169.
{{cite book}}:|author=has generic name (help) - ^ Wolfe R, Sharp L (2002). "Anti-vaccinationists past and present". BMJ. 325 (7361): 430–2. doi:10.1136/bmj.325.7361.430. PMID 12193361.
- ^ Salmon DA, Teret SP, MacIntyre CR, Salisbury D, Burgess MA, Halsey NA (2006). "Compulsory vaccination and conscientious or philosophical exemptions: past, present, and future". Lancet. 367 (9508): 436–42. doi:10.1016/S0140-6736(06)68144-0. PMID 16458770.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Sugarman SD (2007). "Cases in vaccine court—legal battles over vaccines and autism". N Engl J Med. 357 (13): 1275–7. doi:10.1056/NEJMp078168. PMID 17898095.
- ^ Melinda Wharton. National Vaccine Advisory committee U.S.A. national vaccine plan
- ^ Plotkin, Stanley A. (2006). Mass Vaccination: Global Aspects - Progress and Obstacles (Current Topics in Microbiology & Immunology). Springer-Verlag Berlin and Heidelberg GmbH & Co. K. ISBN 978-3540293828.
External links
- Vaccine Research Center: Information regarding preventative vaccine research studies
- Side Effects of Vaccines in Kids
- The Vaccine Page links to resources in many countries.
- Immunisation Immunisation schedule for children in the UK. Published by the UK Department of Health.
- CDC.gov - 'National Immunization Program: leading the way to healthy lives', US Centers for Disease Control (CDC information on vaccinations)
- CDC.gov - 'Mercury and Vaccines (Thimerosal)', US Centers for Disease Control
- Immunize.org - Immunization Action Coalition' (nonprofit working to increase immunization rates)
- WHO.int - 'Immunizations, vaccines and biologicals: Towards a World free of Vaccine Preventable Diseases', World Health Organization (WHO's global vaccination campaign website)
- Health-EU Portal Vaccinations in the EU
