Global spread of H5N1: Difference between revisions
Ref cleanup. Need citation for 2003 infection in 3 flocks in Korea. |
|||
| Line 1: | Line 1: | ||
{{H5N1}}{{Flu}} |
|||
{| class="toccolours" cellpadding="0" cellspacing="0" style="float:right; clear:right; font-size:85%; width:400px; margin:0 0 1em 1em;" |
|||
:''See [http://www.who.int/wer/wer8126.pdf Epidemiology of WHO-confirmed human cases of avian influenza A(H5N1) infection].'' |
|||
|- bgcolor="FF0000" |
|||
'''H5N1 flu''' refers to the '''transmission and infection of [[H5N1]]'''. H5N1 flu is a concern due to the [[global spread of H5N1]] that constitutes a [[pandemic]] threat. This article is about the transmission of the [[H5N1]] [[virus]], infection by that virus, the resulting symptoms of that infection (having or coming down with [[influenza]] or more specifically [[avian flu]] or even more specifically H5N1 flu which can include [[pneumonia]]), and the medical response including treatment. |
|||
! colspan="2" align="center" | Highly pathogenic H5N1 |
|||
|- |
|||
| colspan="2" | [[Image:Global spread of H5N1 map.PNG|center|400px|Highly pathogenic H5N1]] |
|||
|- bgcolor=#FFEFEF |
|||
| style="width:10px; height:10px; background:#FF0000;" | || Countries with poultry or wild birds killed by H5N1. |
|||
|- bgcolor=#FFEFEF |
|||
| style="width:10px; height:5px; background:#800000;" | || Countries with human cases of H5N1. |
|||
|} |
|||
{{H5N1}} |
|||
Infected birds pass on [[H5N1]] through their [[saliva]], [[Mucus|nasal secretions]], and [[feces]]. Other birds may pick up the virus through direct contact with these excretions or when they have contact with surfaces contaminated with this material. Because migratory birds are among the carriers of the H5N1 virus it may spread to all parts of the world. Past outbreaks of avian flu have often originated in crowded conditions in [[southeast Asia|southeast]] and [[east Asia]], where humans, [[pig]]s, and poultry live in close quarters. In these conditions a virus is more likely to [[mutation|mutate]] into a form that more easily infects humans. |
|||
[[Image:Ducks in plymouth, massachusetts.jpg|thumb|right|Ducks play a key role in H5N1 spread]] |
|||
The majority of [[H5N1]] flu cases have been reported in southeast and east Asia. Once an outbreak is detected, local authorities often order a mass slaughter of birds or animals affected. If this is done promptly, an outbreak of avian flu may be prevented. However, the [[United Nations]] (UN) [[World Health Organization]] (WHO) has expressed concern that not all countries are reporting outbreaks as completely as they should. [[China]], for example, is known to have initially denied past outbreaks of [[severe acute respiratory syndrome]] (SARS) and [[HIV]], although there have been some signs of improvement regarding its openess in recent months, particularly with regard to H5N1. |
|||
[[Image:Avian influenza spread map.jpg|thumb|300px|right|The spread of avian influenza in the eastern hemisphere.]] |
|||
[[H5N1]] infections in humans are generally caused by bird to human transmission of the virus. Until May 2006, the WHO estimate of the number of human to human transmission had been "two or three cases". On [[May 24]], [[2006]], Dr. Julie L. Gerberding, director of the United States [[Centers for Disease Control and Prevention]] in [[Atlanta]], estimated that there had been "at least three." On [[May 30]], Maria Cheng, a WHO spokeswoman, said there were "probably about half a dozen," but that no one "has got a solid number."<ref>{{cite news| url=http://www.nytimes.com/2006/06/04/world/asia/04flu.html?ex=1150084800&en=595ebe1cf527875b&ei=5070&emc=eta1 | title=Human Flu Transfers May Exceed Reports | publisher=New York Times | date=[[June 4]] [[2006]] | author=Donald G. McNeil Jr.}}</ref> A few isolated cases of suspected human to human transmission exist.<ref>{{cite news |
|||
The '''global spread of (highly pathogenic) H5N1''' in [[bird]]s is considered a significant [[Influenza pandemic|pandemic]] threat. |
|||
| url=http://www.bloomberg.com/apps/news?pid=10000080&sid=aWESsJvt6CFE&refer=asia |
|||
| title=Seven Indonesian Bird Flu Cases Linked to Patients |
|||
| publisher=Bloomberg |
|||
| date=May 23, 2006 |
|||
}}</ref> with the latest such case in June 2006 (among members of a family in Sumatra).<ref>{{cite web |
|||
| url=http://www.foodconsumer.org/777/8/WHO_Confirms_Human_Transmission_In_Indonesian_Bird_Flu_Cluster.shtml |
|||
| title=WHO confirms human transmission< in Indonesian bird flu cluster |
|||
}}</ref> No [[pandemic]] strain of H5N1 has yet been found. The key point is that, at present, "the virus is not spreading efficiently or sustainably among humans."<ref>{{cite news|url=http://www.who.int/csr/don/2006_06_06/en/index.html|title=Avian influenza – situation in Indonesia – update 17|publisher=[[WHO]]|date=[[June 6]] [[2006]]}}</ref> |
|||
There is also concern, although no definitive proof, that other animals — particularly cats — may be able to act as a bridge between birds and humans. So far several cats have been confirmed to have died from H5N1 and the fact that cats have regular close contact with both birds and humans means monitoring of H5N1 in cats will need to continue. |
|||
While prior [[H5N1]] strains have been known, they were significantly different from the current H5N1 strain on a genetic level, making the global spread of this new strain unprecedented. The current H5N1 strain is a [[Mutation|fast-mutating]], highly [[Pathogen|pathogenic]] [[avian influenza]] virus (HPAI) found in multiple bird species. It is both epizootic (an epidemic in non-humans) and panzootic (a disease affecting animals of many species especially over a wide area). Unless otherwise indicated, "H5N1" in this article refers to the recent highly pathogenic strain of H5N1. |
|||
{{H5N1 case graph}} |
|||
"Since [[1997]], studies of H5N1 indicate that these viruses continue to evolve, with changes in antigenicity and internal [[gene]] constellations; an expanded host range in avian species and the ability to infect [[Felidae|felids]]; enhanced pathogenicity in experimentally infected [[mouse|mice]] and ferrets, in which they cause systemic infections; and increased environmental stability." <ref>{{cite journal |
|||
| url=http://content.nejm.org/cgi/content/full/353/13/1374 |
|||
| title=Avian Influenza A (H5N1) Infection in Humans |
|||
| author=WHO |
|||
| journal=NEJM |
|||
| volume=353 |
|||
| pages=1374 |
|||
| date=September 29, 2005 |
|||
| issue=13 |
|||
}}</ref> |
|||
[[H5N1]] vaccines for chickens exists and is sometimes used, although there are many difficulties that make deciding if it helps more or hurts more especially difficult. [[H5N1]] pre-pandemic vaccines exist in quanties sufficient to inoculate a few million people<ref>{{cite web |
|||
Tens of millions of birds have died of [[H5N1]] influenza and hundreds of millions of birds have been slaughtered and disposed of to limit the spread of H5N1. Countries that have reported one or more major highly pathogenic H5N1 outbreaks in birds (causing at least thousands but in some cases millions of dead birds) are (in order of first outbreak occurrence): [[Korea]], [[Vietnam]], [[Japan]], [[Thailand]], [[Cambodia]], [[Laos]], [[Indonesia]], [[China]], [[Malaysia]], [[Russia]], [[Kazakhstan]], [[Mongolia]], [[Turkey]], [[Romania]], [[Croatia]], [[Ukraine]], [[Cyprus]], [[Iraq]], [[Nigeria]], [[Egypt]], [[India]], [[France]], [[Niger]], [[Bosnia and Herzegovina|Bosnia]], [[Azerbaijan]], [[Albania]], [[Cameroon]], [[Myanmar]], [[Afghanistan]], [[Israel]], [[Pakistan]], [[Jordan]], [[Burkina Faso]], [[Germany]], [[Sudan]], [[Ivory Coast]], [[Djibouti]]. Highly pathogenic H5N1 has been found in birds in the wild in numerous other countries: [[Austria]], [[Bulgaria]], [[Czech Republic]], [[Denmark]], [[Greece]], [[Hungary]], [[Iran]], [[Italy]], [[Kuwait]], [[Poland]], [[Serbia and Montenegro]], [[Slovakia]], [[Slovenia]], [[Spain]], [[Sweden]], [[Switzerland]], [[United Kingdom]]. Countries with massive bird die offs that do not confirm H5N1 include: [[Ethiopia]]. Surveillance of [[H5N1]] in humans, poultry, wild birds, cats and other animals remains very weak in many parts of Asia and Africa. Much remains unknown about the exact extent of its spread. |
|||
| url=http://www.cidrap.umn.edu/cidrap/content/influenza/panflu/news/jul0506hhsreport.html |
|||
| publisher=CIDRAP |
|||
| title=HHS has enough H5N1 vaccine for 4 million people |
|||
| date=July 5, 2006 |
|||
}}</ref> and might be useful for priming to "boost the immune response to a different H5N1 vaccine tailor-made years later to thwart an emerging pandemic".<ref>{{cite web |
|||
| url=http://www.cidrap.umn.edu/cidrap/content/influenza/panflu/news/oct1306vaccines.html |
|||
| publisher=CIDRAP |
|||
| title=Study supports concept of 2-stage H5N1 vaccination |
|||
| date= October 13, 2006 |
|||
}}</ref> [[H5N1]] pandemic vaccines and technologies to rapidly create them are in the [[H5N1 clinical trials]] stage but can not be verified as useful until after there exists a pandemic strain. |
|||
==Avian flu in birds== |
|||
H5N1 has low pathogenic varieties [[Endemic (epidemiology)|endemic]] in [[bird]]s in North America. H5N1 has a highly pathogenic variety that is endemic in dozens of species of birds throughout south [[Asia]] and is threatening to become endemic in birds in west Asia and [[Africa]]. So far, it is very difficult for [[human]]s to become infected with H5N1. The presence of highly pathogenic (deadly) H5N1 around the world in both birds in the wild (swans, magpies, ducks, geese, pigeons, eagles, etc.) and in chickens and turkeys on farms has been demonstrated in millions of cases with the [[virus]] isolate actually [[Sequencing|sequenced]] in hundreds of cases yielding definitive proof of the [[evolution]] of this strain of this subtype of the species [[Influenzavirus A]] (bird flu virus). |
|||
{{See also|Flu_vaccine#Flu vaccine for nonhumans}} |
|||
According to ''Avian Influenza'' by Timm C. Harder and Ortrud Werner: |
|||
:Following an incubation period of usually a few days (but rarely up to 21 days), depending upon the characteristics of the isolate, the dose of inoculum, the species, and age of the bird, the clinical presentation of avian influenza in birds is variable and symptoms are fairly unspecific.<ref>{{cite journal |
|||
| title=Performance of clinical signs in poultry for the detection of outbreaks during the avian influenza A (H7N7) epidemic in The Netherlands in 2003 |
|||
| author=A.R. Elbers, G. Kock and A. Bouma |
|||
| journal=Avian Pathol |
|||
| year=2005 |
|||
| page=181-7 |
|||
| volume=34 |
|||
| url=http://amedeo.com/lit.php?id=16191700 |
|||
}}</ref> Therefore, a diagnosis solely based on the clinical presentation is impossible. The symptoms following infection with low pathogenic AIV may be as discrete as ruffled feathers, transient reductions in egg production or weight loss combined with a slight respiratory disease.<ref>{{cite journal |
|||
| author=I. Capua and F. Mutinelli |
|||
| title=Low pathogenicity (LPAI) and highly pathogenic (HPAI) avian influenza in turkeys and chicken |
|||
| journal=A Colour Atlas and Text on Avian Influenza |
|||
| year=2001 |
|||
| page=13-20 |
|||
}}</ref> Some LP strains such as certain Asian H9N2 lineages, adapted to efficient replication in poultry, may cause more prominent signs and also significant mortality.<ref>{{cite journal |
|||
| author=S. Bano S, K. Naeem K, S.A. Malik |
|||
| title=Evaluation of pathogenic potential of avian influenza virus serotype H9N2 in chicken |
|||
| url=http://amedeo.com/lit.php?id=14575070 |
|||
| year=2003 |
|||
| journal=Avian Dis |
|||
| volume=47, Suppl |
|||
| page=17-22 |
|||
}}</ref><ref>{{cite journal |
|||
| author=C Li, K Yu, G TiaG, D Yu, L Liu, B Jing, J Ping, H. Chen |
|||
| title=Evolution of H9N2 influenza viruses from domestic poultry in Mainland China |
|||
| journal=Virology |
|||
| year=2005 |
|||
| volume=340 |
|||
| page=70-83 |
|||
| url=http://amedeo.com/lit.php?id=16026813 |
|||
}}</ref> In its highly pathogenic form, the illness in chickens and turkeys is characterised by a sudden onset of severe symptoms and a mortality that can approach 100% within 48 hours.<ref>{{cite journal |
|||
| author=D.E. Swayne, D.L. Suarez |
|||
| title=Highly pathogenic avian influenza |
|||
| journal=Rev Sci Tech |
|||
| year=2000 |
|||
| volume=19 |
|||
| page=463-8 |
|||
| url=http://amedeo.com/lit.php?id=10935274 |
|||
}}</ref><ref>{{cite web |
|||
| url=http://www.influenzareport.com/ir/ai.htm |
|||
| title=Avian Influenza |
|||
| author=Timm C. Harder and Ortrud Werner |
|||
| publisher=Influenza Report |
|||
}}</ref> |
|||
Poultry farming practices have changed due to H5N1: |
|||
{{H5N1 case graph}} |
|||
* killing millions of poultry |
|||
* [[Vaccination|vaccinating]] poultry against [[bird flu]] |
|||
* vaccinating poultry workers against [[human flu]] |
|||
* limiting travel in areas where H5N1 is found |
|||
* increasing farm hygiene |
|||
* reducing contact between [[livestock]] and wild birds |
|||
* reducing open-air [[wet markets]] |
|||
* limiting workers contact with [[Cockfight|cock fighting]] |
|||
* reducing purchases of live fowl |
|||
* improving veterinary [[vaccine]] availability and cost. <ref>{{cite web |
|||
| url=http://www.cfr.org/pub8198/laurie_garrett_anthony_s_fauci_michael_osterholm_rita_colwell/the_threat_of_global_pandemics.php |
|||
| publisher=Council on Foreign Relations |
|||
| title=The Threat of Global Pandemics |
|||
| accessdate=2006-09-15 |
|||
| date=June 16, 2005 |
|||
}}</ref> |
|||
For example, after nearly two years of using mainly culling to control the virus, the [[Vietnam|Vietnamese]] government in [[2005]] adopted a combination of mass poultry vaccination, disinfecting, culling, information campaigns and bans on live poultry in cities.<ref>{{cite news |
|||
==Human and bird cases== |
|||
| url=http://today.reuters.co.uk/news/newsArticle.aspx?type=worldNews&storyID=2006-04-28T080147Z_01_HAN5054_RTRUKOC_0_UK-BIRDFLU-VIETNAM.xml |
|||
{{H5N1 cases}} |
|||
| publisher=Reuters |
|||
| title=Vietnam to unveil advanced plan to fight bird flu |
|||
| date=April 28, 2006 |
|||
}}</ref> |
|||
Webster ''et al'' write |
|||
===1959-1997=== |
|||
* A highly pathogenic strain of [[H5N1]] caused [[flu]] outbreaks with significant spread to numerous farms, resulting in great economic losses in [[1959]] in [[Scotland]] in [[chicken]]s and in [[1991]] in [[England]] in [[turkey]]s. <ref>{{cite journal |
|||
| url=http://www.who.int/csr/don/2004_03_02/en/ |
|||
| title=Situation (poultry) in Asia: need for a long-term response, comparison with previous outbreaks |
|||
| journal=Disease Outbreak News: Avian influenza A(H5N1) |
|||
| date=March 2, 2004 |
|||
| author=WHO |
|||
| volume=31 |
|||
}}</ref> These strains were somewhat similar to the current pathogenic strain of H5N1 in two of its ten genes, the gene that causes it to be type H5 and the gene that causes it to be N1. The other genes can and have been [[reassortment|reassorted]] from other subtypes of the bird flu species (their ease at exchanging genes is part of what makes them all one species). [[Evolution]] by reassortment of H5N1 from [[1999]] to [[2002]] created the Z genotype which became the dominant strain of highly pathogenic H5N1 in [[2004]] and is now spreading across the entire world in both wild and domestic birds. |
|||
:Transmission of highly pathogenic H5N1 from domestic poultry back to migratory waterfowl in western China has increased the geographic spread. The spread of H5N1 and its likely reintroduction to domestic poultry increase the need for good agricultural vaccines. In fact, the root cause of the continuing H5N1 pandemic threat may be the way the pathogenicity of H5N1 viruses is masked by cocirculating influenza viruses or bad agricultural vaccines."<ref>{{cite journal |
|||
* "The precursor of the H5N1 influenza virus that spread to [[human]]s in [[1997]] was first detected in [[Guangdong]], [[China]], in [[1996]], when it caused a moderate number of deaths in [[geese]] and attracted very little attention." <ref>{{cite journal |
|||
| url=http://www.cdc.gov/ncidod/EID/vol12no01/05-1024.htm |
| url=http://www.cdc.gov/ncidod/EID/vol12no01/05-1024.htm |
||
| title=H5N1 Outbreaks and Enzootic Influenza |
| title=H5N1 Outbreaks and Enzootic Influenza |
||
| author=[[Robert G. Webster]] ''et al'' |
|||
| journal=Emerging Infectious Diseases |
| journal=Emerging Infectious Diseases |
||
| date=January, 2006 |
|||
| volume=12 |
|||
| accessdate=2006-09-15 |
|||
| issue=1 |
|||
| date=January 2006 |
|||
| author=Robert G. Webster, Malik Peiris, Honglin Chen, and Yi Guan |
|||
}}</ref> |
}}</ref> |
||
Dr. Robert Webster explains: "If you use a good vaccine you can prevent the transmission within poultry and to humans. But if they have been using vaccines now [in China] for several years, why is there so much bird flu? There is bad vaccine that stops the disease in the bird but the bird goes on pooping out virus and maintaining it and changing it. And I think this is what is going on in China. It has to be. Either there is not enough vaccine being used or there is substandard vaccine being used. Probably both. It’s not just China. We can’t blame China for substandard vaccines. I think there are substandard vaccines for influenza in poultry all over the world." <ref>{{cite news |
|||
* In [[1997]], in [[Hong Kong]], 18 humans were infected and 6 died in the first known case of H5N1 infecting humans. <ref name="timeline">{{cite web |
|||
| url=http://www. |
| url=http://www.msnbc.msn.com/id/10639567/ |
||
| title=Expert: Bad vaccines may trigger China bird flu |
|||
| title=H5N1 avian influenza: timeline |
|||
| date=December 30, 2005 |
|||
| author=WHO |
|||
| publisher=MSNBC |
|||
| date=October 28, 2005 |
|||
| accessdate=2006-09-15 |
|||
}}</ref> In response to the same concerns, Reuters reports Hong Kong infectious disease expert Lo Wing-lok saying, "The issue of vaccines has to take top priority," and Julie Hall, in charge of the WHO's outbreak response in China, saying China's vaccinations might be masking the virus." <ref> |
|||
{{cite news |
|||
| title=China H5N1 outbreak puts vaccines under spotlight |
|||
| publisher=Reuters |
|||
| date=March 19, 2006 |
|||
| accessdate=2006-09-15 |
|||
}} ''This reference is apparently no longer available online via Reuters. It is available as of 21 August, 2006 at [http://bak.flu.org.cn/news/20063196219.htm]''</ref> The BBC reported that Dr Wendy Barclay, a virologist at the University of Reading, UK said: "The Chinese have made a vaccine based on reverse genetics made with H5N1 antigens, and they have been using it. There has been a lot of criticism of what they have done, because they have protected their chickens against death from this virus but the chickens still get infected; and then you get drift - the virus mutates in response to the antibodies - and now we have a situation where we have five or six 'flavours' of H5N1 out there." <ref>{{cite web |
|||
| url=http://news.bbc.co.uk/1/hi/sci/tech/4737276.stm |
|||
| title=Bird flu vaccine no silver bullet |
|||
| publisher=BBC |
|||
| date=February 22, 2006 |
|||
| accessdate=2006-09-15 |
|||
}}</ref> |
}}</ref> |
||
==Transmission by wild birds (waterfowl)== |
|||
===2003=== |
|||
[[Image:Avian influenza spread map.jpg|thumb|300px|right|The spread of avian influenza in the eastern hemisphere.]] |
|||
* "Human disease associated with influenza A subtype H5N1 re-emerged in January [[2003]], for the first time since an outbreak in Hong Kong in 1997." Three people in one family were infected after visiting [[Fujian]] province in mainland [[China]] and 2 died. <ref>{{cite journal |
|||
| url=http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=14987888&dopt=Abstract |
|||
| title=Re-emergence of fatal human influenza A subtype H5N1 disease |
|||
| author=J.S. Peiris, W.C Yu, C.W. Leung, C.Y. Cheung, W.F. Ng, J.M. Nicholls, T.K. Ng, K.H. Chan, S.T. Lai, W.L. Lim, K.Y. Yuen, Y. Guan |
|||
| journal=Lancet |
|||
| date=February 21, 2004 |
|||
| volume=363 |
|||
| issue=9409 |
|||
| pages=617-9 |
|||
}}</ref> |
|||
According to the [[United Nations]] [[FAO]]: |
|||
* By midyear of 2003 outbreaks of poultry disease caused by H5N1 occurred in Asia, but were not recognized as such. That December animals in a [[Thailand|Thai]] zoo died after eating infected chicken carcasses. Later that month H5N1 infection was detected in 3 flocks in the [[Republic of Korea]]. <ref name="cases">{{cite web |
|||
there is no denying the fact that wild water fowl most likely play a role in the avian influenza cycle and could be the initial source for AI viruses, which may be passed on through contact with resident water fowl or domestic poultry, particularly domestic ducks. The virus undergoing mutations could circulate within the domestic and possibly resident bird populations until HPAI arises. This new virus is pathogenic to poultry and possibly to the wild birds that it arose from. Wild birds found to have been infected with HPAI were either sick or dead. This could possibly affect the ability of these birds to carry HPAI for long distances. However, the findings in [[Qinghai Lake]]-[[China]], suggest that H5N1 viruses could possibly be transmitted between migratory birds. Additionally, the new outbreaks of HPAI in poultry and wild birds in Russia, Kazakhstan, Western [[China]] and [[Mongolia]] may indicate that migratory birds probably act as carriers for the transport of HPAI over longer distances. Short distance transmission between farms, villages or contaminated local water bodies is likewise a distinct possibility. The AI virus has adapted to the environment in ways such as: 1) the use of water for survival and to spread 2) has evolved in a reservoir (ducks) strictly tied to water. The water in turn influences movement, social behaviour and migration patterns of water bird species. It is therefore of great importance to know the ecological strategy of influenza virus as well, in order to fully understand this disease and to control outbreaks when they occur. There remains a body of data and analysis missing on the collection and detection of HPAI viruses in wild birds. Finding HPAI viruses in wild birds may be a rare event, but if the contact with susceptible species occurs it can cause an outbreak at the local level or in distant areas. <ref>{{cite web |
|||
| url=http://www.who.int/csr/disease/avian_influenza/country/en/ |
|||
| url=http://www.fao.org/ag/againfo/subjects/en/health/diseases-cards/avian_HPAIrisk.html |
|||
| author=WHO |
|||
| publisher=FAO |
|||
| title=Confirmed Human Cases of Avian Influenza A(H5N1) |
|||
| title=Wild birds and Avian Influenza |
|||
| accessdate=2006-09-15 |
|||
}}</ref> |
}}</ref> |
||
==Prevention== |
|||
* H5N1 in China in this and later periods is less than fully reported. Blogs have described many discrepancies between official China government announcements concerning H5N1 and what people in China see with their own eyes. Many reports of total H5N1 cases exclude China due to widespread disbelief in China's official numbers. <ref name="timeline">Timeline ref</ref><ref>{{cite web |
|||
The current method of prevention in animal populations is to destroy infected animals, as well as animals suspected of being infected. In southeast [[Asia]], millions of domestic birds have been slaughtered to prevent the spread of the virus. |
|||
| url=http://www.who.int/csr/disease/avian_influenza/country/cases_table_2006_01_19/en/index.html |
|||
| title=Confirmed Human Cases of Avian Influenza A(H5N1) |
|||
| date=January 19, 2006 |
|||
| author=WHO |
|||
}}</ref><ref>{{cite news |
|||
| url=http://www.cbc.ca/cp/health/060621/x062128.html |
|||
| title=China had bird flu case two years earlier than Beijing admits: researchers |
|||
| publisher=CBC News |
|||
| author=Helen Branswell |
|||
| date=June 21, 2006 |
|||
}}</ref><ref>{{cite journal |
|||
| url=http://www.who.int/csr/don/2003_02_27a/en/index.html |
|||
| title=Influenza A(H5N1) in Hong Kong Special Administrative Region of China |
|||
| journal=Disease Outbreak News: Avian influenza A(H5N1) |
|||
| volume=2 |
|||
| author=WHO |
|||
| date=February 27, 2003 |
|||
}}</ref><ref>{{cite journal |
|||
| url=http://www.who.int/csr/don/2003_07_04/en/ |
|||
| author=WHO |
|||
| journal=Disease Outbreak News: SARS |
|||
| volume=95 |
|||
| title=Chronology of a serial killer |
|||
}}</ref> |
|||
The probability of a "humanized" form of H5N1 emerging through [[gene|genetic]] recombination in the body of a human co-infected with [[H5N1]] and another influenza virus type (a process called [[reassortment]]) could be reduced by [[influenza]] [[vaccine|vaccination]] of those at risk for infection by H5N1. It is not clear at this point whether vaccine production and immunization could be stepped up sufficiently to meet this demand. Additionally, vaccination of only humans would not address the possibility or reassortment in pigs, cats, or other mammal hosts. |
|||
===2004=== |
|||
{{main|Global spread of H5N1 in 2004}} |
|||
If an outbreak of [[pandemic]] flu does occur, its spread might be slowed by increasing hygiene in aircraft, and by examining airline cabin air filters for presence of [[H5N1]] [[virus]]. |
|||
In January 2004 a major new outbreak of [[H5N1]] surfaced in [[Vietnam]] and [[Thailand]]'s [[poultry]] industry, and within weeks spread to ten countries and regions in [[Asia]], including [[Indonesia]], [[South Korea]], [[Japan]] and [[China]]. In October 2004 researchers discovered [[H5N1]] is far more dangerous than previously believed because [[waterfowl]] were directly spreading the highly pathogenic strain of [[H5N1]] to [[chicken]]s, [[crow]]s, [[pigeon]]s, and other birds and that it was increasing its ability to infect mammals as well. From this point on, [[avian flu]] experts increasingly refer to containment as a strategy that can delay but not prevent a future avian flu pandemic. |
|||
The [[United States|American]] [[Centers for Disease Control and Prevention]] advises travelers to areas of Asia where outbreaks of H5N1 have occurred to avoid poultry farms and animals in live food markets <ref>{{cite web |
|||
===2005=== |
|||
| url=http://www.cdc.gov/travel/other/avian_flu_ig_americans_abroad_032405.htm |
|||
{{main|Global spread of H5N1 in 2005}} |
|||
| date=[[March 24]], [[2005]] |
|||
| title=Interim Guidance about Avian Influenza A (H5N1) for U.S. Citizens Living Abroad |
|||
| accessdate=2006-10-27 |
|||
| publisher=U.S. Centers for Disease Control and Prevention |
|||
| work=Travel Notices |
|||
| author=National Center for Infectious Diseases, Division of Global Migration and Quarantine |
|||
}}</ref>. Travelers should also avoid surfaces that appear to be contaminated by feces from any kind of animal, especially poultry. |
|||
There are several [[H5N1]] [[vaccine]]s for several of the avian H5N1 varieties. H5N1 continually mutates rendering them, so far for humans, of little use. While there can be some cross-protection against related flu strains, the best protection would be from a vaccine specifically produced for any future pandemic flu virus strain. Dr. Daniel Lucey, co-director of the Biohazardous Threats and Emerging Diseases graduate program at Georgetown University has made this point, "There is no [[H5N1]] [[pandemic]] so there can be no pandemic [[vaccine]]." <ref>{{cite news |
|||
In January 2005 an outbreak of avian influenza affected thirty three out of sixty four cities and provinces in [[Vietnam]], leading to the forced killing of nearly 1.2 million poultry. Up to 140 million birds are believed to have died or been killed because of the outbreak. In April 2005 there begins an unprecedented die-off of over 6,000 migratory birds at [[Qinghai Lake]] in central [[China]] over three months. This strain of H5N1 is the same strain as is spread west by migratory birds over at least the next ten months. In August 2005 H5N1 spread to [[Kazakhstan]], [[Mongolia]] and [[Russia]]. On [[September 29]] [[2005]], [[David Nabarro]], the newly appointed Senior United Nations System Coordinator for Avian and Human Influenza, warned the world that an outbreak of avian influenza could kill 5 to 150 million people. David Nabarro later stated that as the virus had spread to migratory birds, an outbreak could start in [[Africa]] or the [[Middle East]]. Later in [[2005]] H5N1 spread to [[Turkey]], [[Romania]], [[Croatia]] and [[Kuwait]]. |
|||
| url-http://www.upi.com/ConsumerHealthDaily/view.php?StoryID=20051128-054641-9412r |
|||
| title=Bird flu vaccine won't precede pandemic |
|||
| author=Jennifer Schultz |
|||
| publisher=[[United Press International]] |
|||
| date=[[November 28]] [[2005]] |
|||
| accessdate=2006-10-27 |
|||
}}</ref> However, "pre-pandemic vaccines" have been created; are being refined and tested; and do have some promise both in furthering research and preparedness for the next pandemic <ref>Promising research into vaccines includes: |
|||
* {{cite journal |
|||
| title=Avian Influenza: 'Pandemic Vaccine' Appears to Protect Only at High Doses |
|||
| author=Martin Enserink |
|||
| journal=[[Science (journal)|Science]] |
|||
| volume=309 |
|||
| pages=996 |
|||
| date=[[August 12]] [[2005]] |
|||
| doi=10.1126/science.309.5737.996b |
|||
}} |
|||
* {{cite news |
|||
| url=http://www.gsk.ca/en/media_room/news/20060330.pdf |
|||
| title=GlaxoSmithKline Initiates Human Trial Programme With Two H5N1 Pandemic Flu Vaccines |
|||
| date=[[March 30]] [[2006]] |
|||
| accessdate=2006-10-27 |
|||
}} |
|||
* {{cite news |
|||
| url=http://pittsburghlive.com/x/tribune-review/trib/pittsburgh/s_418036.html |
|||
| source=Tribune-Review |
|||
| title=Murtha eager to speed vaccine |
|||
| date=[[January 28]] [[2006]] |
|||
| accessdate=2006-10-27 |
|||
}} A promising new bird flu vaccine developed by [[University of Pittsburgh]] researchers could provide better protection and be made more quickly than other experimental vaccines.</ref>. [[Vaccine]] manufacturing companies are being encouraged to increase capacity so that if a [[pandemic]] [[vaccine]] is needed, facilities will be available for rapid production of large amounts of a vaccine specific to a new pandemic strain. |
|||
It is not likely that use of [[antiviral drug]]s could prevent the evolution of a pandemic flu virus. <ref name="tamiflu">{{cite web |
|||
| title=Oseltamivir (Tamiflu) |
|||
| url=http://www.nlm.nih.gov/medlineplus/druginfo/uspdi/500062.html |
|||
| publisher=[[National Institutes of Health]] |
|||
| date=January 13, 2000 |
|||
}} Revised on January 10, 2001. |
|||
</ref> |
|||
==Environmental survival== |
|||
===2006=== |
|||
Avian flu virus can last forever at a temperature dozens of degrees below freezing, as is found in the northern most areas that migratory birds frequent. |
|||
{{main|Global spread of H5N1 in 2006}} |
|||
Heat kills [[H5N1]] (i.e. inactivates the virus): |
|||
* In January, scientists announced the development of a vaccine for H5N1 that proved 100 percent effective in mice and chickens.<ref>{{cite news |
|||
* Over 30 days at 0ºC (32.0ºF) (over one month at freezing temperature) |
|||
| url=http://www.physorg.com/news10302.html |
|||
* 6 days at 37ºC (98.6ºF) (one week at human body temperature) |
|||
| title=Scientists develop bird flu vaccine |
|||
* 30 minutes 60ºC (140.0ºF) (half hour at a temperature that causes first and second degree burns in humans in ten seconds)<ref>{{cite web |
|||
| publisher=physorg.com |
|||
| url=http://www.accuratebuilding.com/services/legal/charts/hot_water_burn_scalding_graph.html |
|||
| date=January 26, 2006 |
|||
| title=Hot Water Burn & Scalding Graph |
|||
| accessdate=2006-10-08 |
|||
| accessdate=2006-09-15 |
|||
}}</ref> |
}}</ref> |
||
* In the first two months of [[2006]] H5N1 spread to [[Africa]] and [[Europe]] in wild bird populations possibly signaling the beginning of [[H5N1]] being endemic in wild migratory bird populations on multiple continents for decades, permanently changing the way [[poultry]] are [[farm]]ed. In addition, the spread of highly pathogenic H5N1 to wild birds, birds in zoos and even sometimes to mammals (example: pet cats) raises many unanswered questions concerning best practices for threat mitigation, trying to balance reducing risks of human and nonhuman deaths from the current nonpandemic strain with reducing possible pandemic deaths by limiting its chances of mutating into a pandemic strain. Not using vaccines can result in the need to kill significant numbers of farm and zoo birds, while using vaccines can increase the chance of a pandemic. |
|||
Inactivation of the virus also occurs under the following conditions: |
|||
* By April 2006 scientists had concluded that containment had failed due to the role of wild birds in transmitting the virus and were now emphasizing far more comprehensive risk mitigation and management measures. <ref>{{cite journal |
|||
* [[Acid]]ic [[pH]] conditions |
|||
| journal=Avian Influenza & Wild Birds Bulletin |
|||
* Presence of [[oxidizing agent]]s such as [[sodium dodecyl sulfate]], lipid [[solvent]]s, and [[B-propiolactone]] |
|||
| volume=123 |
|||
* Exposure to [[disinfectant]]s: [[formalin]], [[iodine]] compounds <ref>{{cite web |
|||
| issue=1 |
|||
| url=http://www. |
| url=http://www.cidrap.umn.edu/cidrap/content/influenza/avianflu/biofacts/avflu_human.html |
||
| title=Avian flu biofacts |
|||
| author=International Institute for Sustainable Development (IISD) |
|||
| publisher=CIDRAP |
|||
| title=Scientific Seminar on Avian Influenza, the Environment and Migratory Birds |
|||
| date=April 14, 2006 |
|||
}}</ref> |
}}</ref> |
||
==Incubation== |
|||
* In June 2006 WHO predicted an upsurge in human deaths due to H5N1 during late 2006. In July and August 2006 significantly increased numbers of bird deaths due to H5N1 were recorded in Cambodia, China, Laos, Nigeria, and Thailand while continuing unabated a rate unparalleled in Indonesia. |
|||
The human incubation period of avian influenza A (H5N1) is 2 to 17 days<ref name="nejm">Full text article online: {{cite journal |
|||
| url=http://content.nejm.org/cgi/content/full/353/13/1374 |
|||
| title=Avian Influenza A (H5N1) Infection in Humans |
|||
| author=The Writing Committee of the World Health Organization (WHO) Consultation on Human Influenza A/H5 |
|||
| journal=[[New England Journal of Medicine]] |
|||
| date=[[September 29]] [[2005]] |
|||
| volume=353 |
|||
| pages=1374-1385 |
|||
}}</ref>. Once infected, the virus can spread by cell-to-cell contact, bypassing receptors. So even if a strain is very hard to initially catch, once infected, it spreads rapidly within a body.<ref>{{cite web |
|||
| url=http://www.epw.org.in/showArticles.php?root=2005&leaf=11&filename=9325&filetype=html |
|||
| title=Bird Flu: Public Health Implications for India |
|||
| author=T Jacob John |
|||
| date=November 12, 2005 |
|||
| publisher=Economic and Political Weekly |
|||
}}</ref> |
|||
==Symptoms== |
|||
* In September, Egypt and Sudan joined the list of nations seeing a resurgence of bird deaths due to H5N1. |
|||
:''See also [[Pneumonia]].'' |
|||
Avian influenza HA bind alpha 2-3 [[sialic acid]] receptors while human influenza HA bind alpha 2-6 sialic acid receptors. Usually other differences also exist. There is as yet no human form of H5N1, so all humans who have caught it so far have caught '''avian''' H5N1. |
|||
[[Human flu]] symptoms usually include |
|||
==Pig cases== |
|||
[[fever]], [[cough]], [[sore throat]], [[myalgia|muscle aches]], [[conjunctivitis]] and, in severe cases, severe breathing problems and [[pneumonia]] that may be fatal. The severity of the infection will depend to a large part on the state of the infected person's [[immune system]] and if the victim has been exposed to the strain before, and is therefore partially immune. No one knows if these or other symptoms will be the symptoms of a humanized H5N1 flu. |
|||
[[image:Sow with piglet.jpg|thumb|right|Pigs can harbor influenza viruses adapted to humans and others that are adapted to birds, allowing the viruses to exchange genes and create a pandemic strain.]] |
|||
Avian influenza virus [[H3N2]] is endemic in [[pig]]s ("[[swine flu]]") in [[China]] and has been detected in pigs in Vietnam, increasing fears of the emergence of new variant strains. Health experts say pigs can carry human [[influenza]] viruses, which can combine (i.e. exchange homologous genome sub-units by genetic [[reassortment]]) with [[H5N1]], passing [[gene]]s and mutating into a form which can pass easily among humans. [[H3N2]] evolved from [[H2N2]] by [[antigenic shift]] and caused the [[Hong Kong Flu]] pandemic of [[1968]] and [[1969]] that killed up to 750,000 humans. The dominant strain of annual [[flu]] in humans in January 2006 is [[H3N2]]. Measured resistance to the standard antiviral drugs [[amantadine]] and [[rimantadine]] in H3N2 in humans has increased to 91% in [[2005]]. A combination of these two subtypes of the species known as the [[avian flu]] virus in a country like [[China]] is a worst case scenario. In August 2004, researchers in [[China]] found [[H5N1]] in pigs. <ref name="timeline"/> |
|||
Highly pathogenic [[H5N1]] [[avian flu]] in a human is far worse, killing over 50% of humans that catch it. In one case, a boy with H5N1 experienced [[diarrhea]] followed rapidly by a [[coma]] without developing respiratory or flu-like symptoms. <ref>{{cite journal |
|||
==''[[Felidae]]'' (cats)== |
|||
| url=http://content.nejm.org/cgi/content/short/352/7/686 |
|||
[[Image:Cat_outside.jpg|thumb|right|Domestic cats can get H5N1 from eating birds, and can transmit it to other cats.]] |
|||
| journal=New England Journal of Medicine |
|||
| volume=352 |
|||
| pages=686-691 |
|||
| date=[[February 17]] [[2005]] |
|||
| issue=7 |
|||
| title=Fatal Avian Influenza A (H5N1) in a Child Presenting with Diarrhea Followed by Coma |
|||
}}</ref> |
|||
There have been studies of the levels of [[cytokine]]s in humans infected by the H5N1 flu virus. Of particular concern is elevated levels of [[Tumor necrosis factor|tumor necrosis factor alpha]] (TNF?), a [[protein]] that is associated with tissue destruction at sites of infection and increased production of other cytokines. Flu virus-induced increases in the level of cytokines is also associated with flu symptoms including fever, chills, vomiting and headache. Tissue damage associated with pathogenic flu virus infection can ultimately result in death <ref>{{cite journal |
|||
October 2004 |
|||
| url=http://www.scs.carleton.ca/~soma/biosec/readings/influenza/influenza.html |
|||
| title=Influenza: The world is teetering on the edge of a pandemic that could kill a large fraction of the human population |
|||
* Variants have been found in a number of domestic cats, [[leopard]]s and [[tiger]]s in [[Thailand]], with high lethality. <ref>{{cite journal |
|||
| author=Robert G. Webster and Elizabeth Jane Walker |
|||
| url=http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=pubmed&dopt=Abstract&list_uids=16318716&query_hl=1 |
|||
| journal= |
| journal=American Scientist |
||
| date=2003 |
|||
| title=Highly pathogenic avian influenza H5N1, Thailand, 2004 |
|||
| volume=91 |
|||
| author=T. Tiensin, P. Chaitaweesub, T. Songserm, A. Chaisingh, W. Hoonsuwan, C. Buranathai, T. Parakamawongsa, S. Premashthira, A. Amonsin, M. Gilbert, M. Nielen, A. Stegeman |
|||
| pages=122 |
|||
| date=November, 2005 |
|||
}}</ref>. The [[Inflammation|inflammatory]] cascade triggered by H5N1 has been called a '[[cytokine storm]]' by some, because of what seems to be a [[positive feedback]] process of damage to the body resulting from [[immune system]] stimulation. H5N1 type flu virus induces higher levels of cytokines than the more common flu virus types such as H1N1 <ref>{{cite journal |
|||
| volume=11 |
|||
| url=http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=pubmed&dopt=Abstract&list_uids=16283933 |
|||
| issue=11 |
|||
| title=Proinflammatory cytokine responses induced by influenza A (H5N1) viruses in primary human alveolar and bronchial epithelial cells |
|||
| pages=1664-72 |
|||
| author=M. C. Chan et al |
|||
}}</ref> "The Thailand Zoo tiger outbreak killed more than 140 tigers, causing health officials to make the decision to cull all the sick tigers in an effort to stop the zoo from becoming a reservoir for H5N1 influenza (ProMED-mail, 2004i; ProMED-mail, 2004w). A study of domestic cats showed H5N1 virus infection by ingestion of infected poultry and also by contact with other infected cats (Kuiken et al., 2004)." <ref>{{cite book |
|||
| journal=Respiratory Research |
|||
| url=http://www.nap.edu/books/0309095042/html/15.html |
|||
| year=2005 |
|||
| title=The Threat of Pandemic Influenza: Are We Ready? Workshop Summary |
|||
| volume=6 |
|||
| author=Board on Global Health (BGH) |
|||
| |
| page=135 |
||
}}</ref> Other important mechanisms also exist "in the acquisition of virulence in [[Influenzavirus A|avian influenza viruses]]" according to the [[CDC]].<ref>{{cite journal |
|||
| date=2005 |
|||
| url=http://www.cdc.gov/ncidod/EID/vol10no12/04-0743.htm |
|||
| publisher=NAP |
|||
| title=Novel Avian Influenza H7N3 Strain Outbreak, British Columbia |
|||
}} |
|||
| author=Martin Hirst, Caroline R. Astell, Malachi Griffith, Shaun M. Coughlin, Michelle Moksa, Thomas Zeng ''et al'' |
|||
</ref> The initial [[OIE]] report reads: "the clinical manifestations began on 11 October 2004 with weakness, lethargy, respiratory distress and high fever (about 41-42 degrees Celsius). There was no response to any antibiotic treatment. Death occurred within three days following the onset of clinical signs with severe pulmonary lesions." <ref>{{cite web |
|||
| date=December 2004 |
|||
| url=http://www.oie.int/eng/info/hebdo/AIS_22.HTM#Sec4 |
|||
| journal=Emerg Infect Dis |
|||
| publisher=OIE |
|||
| title=Avian Influenza in Jordan: Followup Report No. 2 |
|||
| author=Fares Bakhit Naser |
|||
| date=April 13, 2006 |
|||
| accessdate=2006-10-08 |
|||
}}</ref> |
}}</ref> |
||
The NS1 [[protein]] of the highly pathogenic avian [[H5N1]] [[virus]]es circulating in [[poultry]] and [[waterfowl]] in Southeast [[Asia]] is currently believed to be responsible for the enhanced proinflammatory [[cytokine]] response. H5N1 NS1 is characterized by a single [[amino acid]] change at position 92. By changing the amino acid from [[glutamic acid]] to [[aspartic acid]], researchers were able to abrogate the effect of the H5N1 NS1. This single amino acid change in the NS1 gene greatly increased the [[pathogenicity]] of the H5N1 influenza virus. |
|||
[[February 28]] [[2006]] |
|||
In short, this one amino acid difference in the NS1 protein produced by the NS [[RNA]] molecule of the [[H5N1]] virus is believed to be largely responsible for an increased [[pathogenicity]] (on top of the already increased pathogenicity of its hemagglutinin type which allows it to grow in organs other than lungs) that can manifest itself by causing a [[cytokine storm]] in a patient's body, often causing [[pneumonia]] and [[death]]. |
|||
* A dead cat infected with the [[H5N1]] bird flu virus was found in [[Germany]]. <ref>{{cite news |
|||
| title=German cat gets deadly bird flu |
|||
| url=http://news.bbc.co.uk/2/hi/europe/4758632.stm |
|||
| publisher=BBC News |
|||
| date=February 28, 2006 |
|||
| accessdate=2006-10-08 |
|||
}}</ref> |
|||
==Treatment== |
|||
[[March 6]] [[2006]] |
|||
Neuraminidase inhibitors are a class of drugs that includes [[zanamivir]] and [[oseltamivir]], the latter being licensed for [[prophylaxis]] treatment in the [[United Kingdom]]. Oseltamivir inhibits the influenza virus from spreading inside the user's body <ref name="tamiflu" />. It is marketed by [[Hoffmann-La Roche|Roche]] as ''[[Tamiflu]]''. This drug has become a focus for some governments and organizations trying to be seen as making preparations for a possible H5N1 pandemic. In August [[2005]], Roche agreed to donate three million courses of o be deployed by the WHO to contain a pandemic in its region of origin. Although ''Tamiflu'' is patented, international law gives governments wide freedom to issue [[compulsory licenses]] for life-saving drugs. |
|||
A second class of drugs, which include [[amantadine]] and [[rimantadine]], target the M2 protein, but are ineffective against [[H5N1]]. Unlike zanamivir and oseltamivir, these drugs are inexpensive and widely available and the WHO had initially planned to use them in efforts to combat an [[H5N1]] pandemic. However, the potential of these drugs was considerably lessened when it was discovered that farmers in China have been administering amantadine to poultry with government encouragement and support since the early [[1990s]], against international livestock regulations; the result has been that the strain of the virus now circulating in South East Asia is largely resistant to these medications and hence significantly more dangerous to humans<ref>{{cite news |
|||
* Hans Seitinger, the top agriculture official in the southern state of [[Styria]], [[Austria]] announced that several still living cats in Styria have tested positive for H5N1: <ref>{{cite news |
|||
| url=http:// |
| url=http://www.washingtonpost.com/wp-dyn/content/article/2005/06/17/AR2005061701214.html |
||
| title=Bird Flu Drug Rendered Useless: Chinese Chickens Given Medication Made for Humans |
|||
| publisher=ABC News |
|||
| author=Alan Sipress |
|||
| title=Austrian Cats Test Positive for Bird Flu |
|||
| publisher=Washington Post |
|||
| date=March 6, 2006 |
|||
|date=June 18, 2005 |
|||
| accessdate=2006-10-08 |
|||
}}</ref>. |
|||
:However, recent data suggest that some strains of H5N1 are susceptible to the older drugs. An analysis of more than 600 H5N1 viruses collected in Southeast Asia showed that most samples from China and Indonesia lacked genetic characteristics signaling resistance to amantadine, whereas most samples from Vietnam, Thailand, and Cambodia had those characteristics. The report was published by the Journal of Infectious Diseases. The new WHO guidelines were drawn up by an international group of clinicians with experience treating H5N1 patients, along with other experts, at a meeting in late March. The panel systematically reviewed and graded the evidence for the drugs' effectiveness. Since no results from controlled trials of medication use in H5N1 cases are available, "Overall, the quality of the underlying evidence for all recommendations was very low," the 138-page WHO report states. The evidence includes results of lab and animal studies and indirect evidence from studies of antiviral use in patients with seasonal influenza. The recommendations are classified as "strong" or "weak," depending on the quality of the relevant evidence. The WHO says that if a patient has a confirmed or strongly suspected H5N1 case and NIs are available, "Clinicians should administer oseltamivir treatment (strong recommendation); zanamivir might be used as an alternative (weak recommendation)." Oseltamivir comes in capsule form, whereas zanamivir is taken with an inhaler. The WHO says zanamivir has lower bioavailability outside the respiratory tract than oseltamivir, but it may be active against some strains of oseltamivir-resistant H5N1 virus.<ref> |
|||
{{cite news |
|||
| url=http://www.cidrap.umn.edu/cidrap/content/influenza/avianflu/news/may2206antivirals.html |
|||
| title=WHO sees role for older antivirals in some H5N1 cases |
|||
| publisher=CIDRAP |
|||
| date=May 22, 2006 |
|||
}}</ref> |
}}</ref> |
||
==Mortality rate== |
|||
August 2006 |
|||
{{H5N1 Human Mortality}} |
|||
A strain of [[H5N1]] killed [[chicken]]s in [[1959]] in [[Scotland]] and [[turkey]]s in [[1991]] in [[England]]. This strain was "highly pathogenic" (deadly to birds) but caused neither illness nor death in humans.<ref>{{cite news |
|||
| url=http://www.who.int/csr/don/2004_03_02/en/ |
|||
| work=Disease Outbreak News: Avian influenza A(H5N1) |
|||
| title=Situation (poultry) in Asia: need for a long-term response, comparison with previous outbreaks |
|||
| date=[[March 2]] [[2004]] |
|||
| accessdate=2006-10-27 |
|||
| publisher=WHO |
|||
}} |
|||
</ref> "The precursor of the H5N1 influenza virus that spread to [[human]]s in [[1997]] was first detected in [[Guangdong]], [[China]], in [[1996]], when it caused a moderate number of deaths in [[geese]] and attracted very little attention." <ref>{{cite web |
|||
| url=http://www.cdc.gov/ncidod/EID/vol12no01/05-1024.htm |
|||
| title=H5N1 Outbreaks and Enzootic Influenza |
|||
| author=Robert G. Webster, Malik Peiris, Honglin Chen, and Yi Guan |
|||
| date=January 2006 |
|||
| accessdate=2006-10-28 |
|||
| journal=Emerg Infect Dis |
|||
| publisher=CDC |
|||
| volume=12 |
|||
| issue=1 |
|||
}}</ref> In [[1997]], in [[Hong Kong]], 18 humans were infected and 6 died in the first known case of H5N1 infecting humans. <ref name="timeline">{{cite web |
|||
| url=http://www.who.int/csr/disease/avian_influenza/Timeline_28_10a.pdf |
|||
| title=H5N1 avian influenza: timeline |
|||
| author=WHO |
|||
| date=October 28, 2005 |
|||
}}</ref> H5N1 had evolved from a zero mortality rate to a 33% mortality rate. |
|||
By 2003 H5N1 infection was detected in three flocks in the [[Republic of Korea]].{{fact}} This strain caused asymptomatic infections in humans and has died out, meaning that its low mortality level is no more relevant than the 1959 strain's low mortality rate.<ref>{{cite news |
|||
<ul> |
|||
| url=http://www.cidrap.umn.edu/cidrap/content/influenza/avianflu/news/sep2106korea.html |
|||
<li>It was announced in the August 2006 CDC EID journal that while literature describing HPAI H5N1 infection in cats had been limited to a subset of clade I viruses; a Qinghai-like virus (they are genetically distinct from other clade II viruses) killed up to five cats and 51 chickens from February 3 to February 5, 2006 in Grd Jotyar (~10 km north of [[Arbil|Erbil City]], Iraq). Two of the cats were available for examination. |
|||
| publisher=CIDRAP |
|||
| title=Five Koreans had H5N1 virus but no illness |
|||
| date=September 21, 2006 |
|||
}}</ref> <ref name="Tree of Life">{{cite web |
|||
| url=http://www.who.int/csr/disease/avian_influenza/guidelines/recommendationvaccine.pdf |
|||
| author=WHO |
|||
| date=[[August 18]] [[2006]] |
|||
| title=Antigenic and genetic characteristics of H5N1 viruses and candidate H5N1 vaccine viruses developed for potential use as pre-pandemic vaccines |
|||
}} Contains latest Evolutionary "Tree of Life" for H5N1</ref> The apparently extinct strain that caused Vietnam's human deaths from H5N1 in 2003, 2004 and 2005 also had a lower case mortality rate than the currently existing strains.<ref name="Tree of Life"/> Changes are occurring in H5N1 that are increasing its pathogenicity in mammals.<ref name="Chen">{{cite journal |
|||
| author=Chen H, Deng G, Li Z, Tian G, Li Y, Jiao P, Zhang L, Liu Z, Webster RG, Yu K. | title=The evolution of H5N1 influenza viruses in ducks in southern China | journal=Proc. Natl. Acad. Sci. U. S. A. | year=2004 | pages=10452-10457 | volume=101 | issue=28 | id={{PMID|15235128}}}} [http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pubmed&pubmedid=15235128 Full Text]</ref> |
|||
In [[2005]], 42 of 97 people confirmed by the [[WHO]] to be infected with [[H5N1]] died -- or 43%. From [[January 1]] [[2006]] to [[October 16]] [[2006]], the case fatality ratio has been higher, with 73 deaths among 109 [[WHO]]-confirmed cases |
|||
:"An influenza A H5 virus was present in multiple organs in all species from the outbreak site in Grd Jotyar (Table). cDNA for sequencing was amplified directly from RNA extracts from pathologic materials without virus isolation. On the basis of sequence analysis of the full HA1 gene and 219 amino acids of the HA2 gene, the viruses from the goose and 1 cat from Grd Jotyar and from the person who died from Sarcapcarn (sequence derived from PCR amplification from first-passage egg material) are >99% identical at the nucleotide and amino acid levels (GenBank nos. DQ435200–02). Thus, no indication of virus adaptation to cats was found. The viruses from Iraq are most closely related to currently circulating Qinghai-like viruses, but when compared with A/bar-headed goose/Qinghai/65/2005 (H5N1) (GenBank no. DQ095622), they share only 97.4% identity at the nucleic acid level with 3 amino acid substitutions of unknown significance. On the other hand, the virus from the cat is only 93.4% identical to A/tiger/Thailand/CU-T4/2004(H5N1) (GenBank no. AY972539). These results are not surprising, given that these strains are representative of different clades (8,9). Sequencing of 1,349 bp of the N gene from cat 1 and the goose (to be submitted to GenBank) show identity at the amino acid level, and that the N genes of viruses infecting the cat and goose are >99% identical to that of A/bar-headed goose/Qinghai/65/2005(H5N1). These findings support the notion that cats may be broadly susceptible to circulating H5N1 viruses and thus may play a role in reassortment, antigenic drift, and transmission."<ref>{{cite journal |
|||
<ref>{{cite web |
|||
| url=http://www.cdc.gov/ncidod/EID/vol12no08/06-0264.htm |
|||
| url=http://www.who.int/csr/disease/avian_influenza/country/cases_table_2006_10_16/en/index.html |
|||
| title=Centers for Disease Control and Prevention (CDC) |
|||
| title=Cumulative Number of Confirmed Human Cases of Avian Influenza A/(H5N1) Reported to WHO |
|||
| journal=Emerging Infectious Diseases (EID) Journal |
|||
| |
| publisher=WHO |
||
| date=October 16, 2006 |
|||
| issue=8 |
|||
}}</ref>-- or 67%. This has been interpreted by some to mean that the virus itself is becoming more deadly over time. <ref>{{cite web |
|||
| date=August, 2006 |
|||
| url=http://www.dymaxionweb.com/h5n1/archives/2006/05/h5n1_getting_de.html |
|||
| title=Qinghai-like H5N1 from Domestic Cats, Northern Iraq |
|||
| title=H5N1 Getting Deadlier |
|||
| author=Samuel L. Yingst, Magdi D. Saad, and Stephen A. Felt |
|||
}} based on the article {{cite web |
|||
}} Authors all part of US Naval Medical Research Unit No. 3, Cairo, Egypt |
|||
| url=http://www.bloomberg.com/apps/news?pid=10000080&sid=a7CJ0uPPpg.g |
|||
</ref> |
|||
| title=Bird Flu Fatality Rate in Humans Climbs to 64% as Virus Spreads |
|||
}}</ref> The global case fatality ratio is, nonetheless, a crude summary of a complex situation with many contributing factors. In particular, if an [[influenza pandemic]] arises from one of the currently circulating strains of [[H5N1|Asian lineage HPAI A(H5N1)]], the mortality rates for the resulting human adapted [[influenza]] strain cannot be predicted with any confidence. |
|||
[[H5N1]] is currently much better adapted to [[bird]]s than to other hosts, which is why the disease it causes is called a [[bird flu]]. No [[pandemic]] strain of H5N1 has yet been found. The precise nature and extent of the genetic alterations that might change one of the currently circulating [[avian flu]] strains into a [[human flu]] strain cannot be known in advance. While many of the current H5N1 strains circulating in birds can generate a dangerous [[cytokine storm]] in healthy adult humans <ref>{{cite web |
|||
The spread to more and more types and populations of birds and the ability of [[felidae]] (cats) to catch [[H5N1]] from eating this natural prey means the creation of a reservoir for H5N1 in cats where the virus can adapt to mammals is one of the many possible pathways to a [[pandemic]]. |
|||
| url=http://www.cidrap.umn.edu/cidrap/content/influenza/panflu/news/sep1106storm.html |
|||
</li> |
|||
| title=Clinical study points to cytokine storm in H5N1 cases |
|||
</ul> |
|||
| date=September 11, 2006 |
|||
| publisher=CIDRAP News |
|||
}}</ref><ref>{{cite journal |
|||
| url=http://www.nature.com/nm/journal/vaop/ncurrent/abs/nm1477.html |
|||
| title=Fatal outcome of human influenza A (H5N1) is associated with high viral load and hypercytokinemia |
|||
| journal=Nature |
|||
| author=Menno D de Jong ''et al'' |
|||
| date=September 10, 2006 |
|||
}} Published online.</ref>, the ultimate pandemic strain might arise from a less-lethal strain, or its current level of lethality might be lost in the adaptation to a human host. |
|||
The global case fatality ratio looks only to the official tally of cases confirmed by the [[WHO]]. It takes no account of other cases, such as those appearing in press reports. Nor does it reflect any estimate of the global extent of mild, asymptomatic, or other cases which are undiagnosed, unreported by national governments to the [[WHO]], or for any reason cannot be confirmed by the [[WHO]]. While the [[WHO]]'s case count is clearly the most authoritative, these unavoidable limitations result in an unknown number of cases being omitted from it. The problem of overlooked but genuine cases is emphasized by occasional reports in which later serology reveals antibodies to the H5N1 infection in the blood of persons who were never known to have bird flu, and who then are confirmed by the [[WHO]] only retroactively as "cases." Press reports of such cases, often poultry handlers, have appeared in various countries. The largest number of asymptomatic cases was recently confirmed among Korean workers who had assisted in massive culls of H5N1-infected poultry.<ref> |
|||
==Mammals in general== |
|||
{{cite web |
|||
[[Image:marten.jpg|thumb|right|Martens and an unknown number of other mammals can catch H5N1, illustrating the unprecedented ability of H5N1 to survive and spread.]] |
|||
| url=http://www.cidrap.umn.edu/cidrap/content/influenza/avianflu/news/sep2106korea.html |
|||
[[H5N1]] has been transmitted in laboratories to many species including [[mouse|mice]] and [[ferret]]s to study its effects. |
|||
| title=Five Koreans had H5N1 virus but no illness (Sep 21,2006) |
|||
| publisher=CIDRAP |
|||
| accessdate=2006-08-23 |
|||
}}</ref> This relatively benign Korean strain of H5N1 has died out, and the remaining strains of H5N1 have a higher case fatality rate in humans. |
|||
Unconfirmed cases have a potentially huge impact on the case fatality ratio. This mathematical impact is well-understood by epidemiologists, and is easy to see in theory. For example, if for each confirmed case reported by the WHO we assume that there has been another mild and unreported case, the actual global number of cases would be double the current number of [[WHO]]-confirmed cases. The fatality ratio for H5N1 infections would then be calculated as the same number of deaths, but divided by a doubled number for total cases, resulting in a hypothetical death ratio of half the currently-reported fatality ratio. Such a result would indicate to epidemiologists that the world was confronting an H5N1 virus that is less-lethal than currently assumed, although possibly one that was more contagious and difficult to track. |
|||
H5N1 was transmitted in the wild to three [[Civet|civet cats]] in [[Vietnam]] in August 2005 and a [[Marten|stone marten]] in [[Germany]] in March 2006. <ref>{{cite news |
|||
| url=http://news.bbc.co.uk/2/hi/asia-pacific/4186620.stm |
|||
| title=Bird flu kills Vietnam civet cats |
|||
| publisher=BBC News |
|||
| date=August 26, 2005 |
|||
| accessdate=2006-10-07 |
|||
}}</ref> |
|||
A case-fatality ratio based on an accurate and all-inclusive count of cases would be invaluable, but unfortunately it is impossible to attain. The ability to diagnose every case of H5N1 as it arises does not exist. A few reported studies have attempted to gather preliminary data on this crucial statistic, by carrying out systematic blood testing of neighbors and contacts of fatal cases in villages where there had been confirmed H5N1 fatalities. This testing failed to turn up any overlooked mild cases. <ref> |
|||
The [[BBC]] reported that a stray [[dog]] in [[Azerbaijan]] died from the disease on [[March 15]] [[2006]]. <ref>{{cite news |
|||
{{cite news |
|||
| url=http://news.bbc.co.uk/1/hi/world/europe/4811284.stm |
|||
| url=http://www.cidrap.umn.edu/cidrap/content/influenza/avianflu/news/mar2706cases.html |
|||
| publisher=BBC News |
|||
| title=Mild H5N1 cases weren’t found missed in Cambodian outbreak study |
|||
| title=Bird flu 'causes first dog death' |
|||
| date=March |
| date=March 27, 2006 |
||
| publisher=CIDRAP |
|||
| accessdate=2006-10-08 |
|||
}}</ref> <ref>{{cite news |
|||
}} |
|||
| url=http://www.cidrap.umn.edu/cidrap/content/influenza/avianflu/news/sep0706cambodia.html |
|||
</ref> |
|||
| title=Cambodian study suggests mild H5N1 cases are rare |
|||
| date=September 7, 2006 |
|||
| publisher=CIDRAP |
|||
}}</ref> These methodical studies of contacts provide significant evidence that the high death rate among confirmed cases in the villages where these studies were carried out cannot be simply attributed to a wholesale failure to detect mild cases. Unfortunately, these studies are likely to remain too few and sketchy to define the complex situation worldwide regarding the lethality of the varying H5N1 clades. The testing and reporting necessary for mass serology studies to determine the incidence of overlooked cases for each existing clade and strain of H5N1 worldwide would be prohibitively costly. |
|||
Hence the precise allocation of infections by the various H5N1 clades across the spectrum including lethal, serious, mild, and asymptomatic cases is likely to remain unknown in both humans and the hundreds of other species it can infect. Scientists are very concerned about what we do know about [[H5N1]]; but even more concerned about the vast amount of important data that we don't know about H5N1 and its future mutations. |
|||
Experts believe more work is needed to determine the role of [[mammal]]s in the [[epidemiology]] of [[H5N1]]. Officials are not doing enough to monitor cats, dogs and other carnivores for their possible role in transmitting [[H5N1]]. People living in areas where the A(H5N1) virus has infected birds are advised to keep their cats indoors. "Cats can be infected through the respiratory tract. Cats can also be infected when they ingest the virus, which is a novel route for influenza transmission in mammals. But cats excrete only one-thousandth the amount of virus that chickens do [...] The concern is that if large numbers of felines and other carnivores become infected, the virus might mutate in a series of events that could lead to an epidemic among humans. Dogs, foxes, seals and other carnivores may be vulnerable to A(H5N1) virus infection, Dr. Osterhaus said. Tests in Thailand have shown that the virus has infected dogs without causing apparent symptoms." <ref>{{cite news |
|||
| url=http://www.nytimes.com/2006/04/06/world/europe/06cat.html |
|||
| publisher=New York Times |
|||
| title=Article on Bird Flu Criticizes Effort to Monitor Cats and Dogs |
|||
| author=Lawrence K. Altman |
|||
| date=April 6, 2006 |
|||
| accessdate=2006-10-08 |
|||
}} (Free subscription required to access article.) |
|||
</ref> |
|||
A case fatality ratio of over 50% provides a grim backdrop for the fact that the currently circulating H5N1 strains have certain genetic similarities with the [[Spanish Influenza]] pandemic virus. In that pandemic, 50 million to 100 million people worldwide were killed during about a year in [[1918]] and [[1919]] <ref> |
|||
==Expected mortality from pandemic== |
|||
{{cite web |
|||
{{seealso|Transmission and infection of H5N1#Mortality rate}} |
|||
| url=http://www.nap.edu/books/0309095042/html/7.html |
|||
| title=The Threat of Pandemic Influenza: Are We Ready? Workshop Summary (2005) |
|||
| publisher=NAP |
|||
| accessdate=2006-08-21 |
|||
}}</ref>. |
|||
Review of patient ages and outcomes reveals that H5N1 attacks are especially lethal in pre-adults and young adults, while older victims tend to have milder attacks and to survive. <ref>{{cite web |
|||
If H5N1 mutates so that it can jump from human to human, while maintaining a relatively high level of mortality, how many people could die? Risk communication analysts Peter M. Sandman and Jody Lanard give a round-up of the various estimates: |
|||
| url=http://www.wpro.who.int/NR/rdonlyres/299B9BDC-67D8-40AC-81BE-0BC8D38E296A/0/S2_0814.jpg |
|||
| title=Human Avian Influenza A(H5N1) Cases by Age Group and Country |
|||
}}</ref> This is consistent with the frequent development of a [[cytokine storm]] in the afflicted.<ref>{{cite news |
|||
| url=http://www.nytimes.com/2006/09/11/world/11flu.html |
|||
| title=Immediate Treatment Needed for Bird Flu Cases, Study Says |
|||
| publisher=New York Times |
|||
| date=September 11, 2006 |
|||
}}</ref> Very few persons over 50 years of age died after suffering a H5N1 attack. Instead, the age-fatality curve of H5N1 influenza attacks in humans resembles that of the 1918 Spanish pandemic flu, and is the opposite of the mortality curve of seasonal flu strains, since seasonal influenza preferentially kills the elderly and does not kill by [[cytokine storm]]. |
|||
Another factor complicating any attempt to predict lethality of an eventual pandemic strain is that many human victims of the current H5N1 influenza have been blood relatives (but rarely spouses) of other victims. This data suggests that the victims' genetic susceptibility may have played a role in the human cases registered to date. |
|||
<blockquote style="padding:1em; border:1px dashed #2f6fab; color:black; background-color:#f9f9f9;">Worldwide mortality estimates range all the way from 2-7.4 million deaths (the “conservatively low” pandemic influenza calculation of a flu modeling expert at the U.S. Centers for Disease Control and Prevention) to 1000 million deaths (the bird flu pandemic prediction of one Russian virologist). The estimates of most H5N1 experts range less widely but still widely. In an H5N1 pandemic, the experts guess that somewhere between a quarter of us and half of us would get sick, and somewhere between one percent and five percent of those who got sick would die — the young and hale as well as the old and frail. If it's a quarter and one percent, that's 16 million dead; if it's a half and five percent, it's 160 million dead. Either way it's a big number. <ref>{{cite web |
|||
| url=http://www.psandman.com/col/pandemic.htm |
|||
| title=Pandemic Influenza Risk Communication: The Teachable Moment |
|||
| author=Peter M. Sandman, Jody Lanard |
|||
| date=December 4, 2004 |
|||
| accessdate=2006-10-08 |
|||
}}</ref></blockquote> |
|||
=== Mortality rate in planning reports === |
|||
Perhaps the most extreme maximum has come from renowned virus expert, [[Robert Webster]], who believes H5N1 has the capacity to mutate into a form that could kill a third of the human population.<ref>{{cite journal |
|||
Governments and other organisations at many levels and in many places have produced "planning" reports that, among other things, offer speculation on the mortality rate of an eventual pandemic. One such report states that "over half a million Americans could die and over 2.3 million could be hospitalized if a moderately severe strain of a pandemic flu virus hits the U.S."<ref>{{cite web |
|||
| url=http://www.scs.carleton.ca/~soma/biosec/readings/influenza/influenza.html |
|||
| publisher=Senior Journal |
|||
| title= The world is teetering on the edge of a pandemic that could kill a large fraction of the human population |
|||
| date=June 24, 2005 |
|||
| author=[[Robert Webster]], Elizabeth Jane Walker |
|||
| title=Pandemic Flu Projection Says More Than Half Million Could Die in U.S. |
|||
| date=March-April 2003 |
|||
| url=http://www.seniorjournal.com/Spotlights/FLU2005-06/5-06-24PandemicProjections.htm |
|||
| accessdate=2006-10-08 |
|||
}}</ref>. No one knows if "moderately severe" is an accurate guess or not. This report entitled ''A Killer Flu?''<ref>{{cite web |
|||
| journal=American Scientist |
|||
| url=http://healthyamericans.org/reports/flu/Flu2005.pdf |
|||
| volume=91 |
|||
| title=Healthy Americans Full report PDF |
|||
| issue=2 |
|||
}}</ref> shows an assumed (guessed) contraction rate of 25% and a severity similar to low severity flu pandemics causing 180 thousand deaths in the US and a 1918 level severity rate causing one million deaths in the US. There is no evidence an H5N1 flu pandemic would be between these figures<ref>{{cite web |
|||
| pages=122 |
|||
| url=http://www.msnbc.msn.com/id/12610942/site/newsweek/ |
|||
}}</ref> In March, 2006, he is quoted as saying "Society just can't accept the idea that 50 percent of the population could die. And I think we have to face that possibility".<ref>{{cite news |
|||
| publisher=Newsweek |
|||
| url=http://abcnews.go.com/WNT/AvianFlu/story?id=1724801 |
|||
| title=A Dramatic Disconnect |
|||
| publisher=ABC News |
|||
}} estimates two million dead in the US, for example</ref> as no data is available reflecting similar virulance in any earlier flu strain as it emerged. The relatively low mortality rate in these and other such reports can not, therefore, be taken as reliable predictions of what the mortality rate of an H5N1 pandemic might be. The low assumed mortality rate does, however, serve the purpose of the reports, which is to show that we are not prepared ''even'' for severity levels that have occurred in the past<ref>Dr. Martin Meltzer of the Centers for Disease Control, an expert on the societal impact of diseases, warns that “There is no healthcare system anywhere in the world that can cope with even a mild pandemic like the one in 1968.” Meltzer MI, Lancet Asia Forum, Singapore, May 2006</ref>, let alone the much higher case fatality ratios seen more recently. |
|||
| date=March 14, 2006 |
|||
| title=Renowned Bird Flu Expert Warns: Be Prepared |
|||
| accessdate=2006-10-08 |
|||
}}</ref> |
|||
==Notes and references== |
|||
==Sources== |
|||
<div class="references-small" style="-moz-column-count:2; column-count:2;"> |
<div class="references-small" style="-moz-column-count:2; column-count:2;"><references/></div> |
||
<references/> |
|||
</div> |
|||
==See also== |
==See also== |
||
*[[Reporting disease cases]] |
*[[Reporting disease cases]] |
||
*[[Severe acute respiratory syndrome]] |
|||
*[[Progress of the SARS outbreak]] |
|||
==Further reading== |
==Further reading== |
||
{{wikinews|Category:Avian Flu}} |
|||
* {{cite web | url=http://www.who.int/csr/disease/avian_influenza/en/ | title=WHO Avian influenza resource (updated)}} |
|||
=== General information === |
|||
* {{cite web | url=http://www.cdc.gov/flu/avian/gen-info/facts.htm CDC | title=Facts About Avian Influenza (Bird Flu) and Avian Influenza A (H5N1) Virus}} |
|||
{{wikinews|Category:Avian Flu}} |
|||
* {{cite web | url=http://www.fao.org/ag/avian.html | title=FAO information on Avian Influenza - Latest news, Disease Card, Maps, Animations}} |
|||
*{{cite web |
|||
* {{cite web |
|||
| url=http://www.birdflubeacon.com |
|||
| url=http://www.cidrap.umn.edu/cidrap/content/biosecurity/ag-biosec/anim-disease/avianflu.html |
|||
| title=Birdflubeacon.com for news, maps, stats, symptoms, treatment, pandemic preparation. |
|||
| title=Avian Influenza (Bird Flu): Agricultural and Wildlife Considerations |
|||
| accessdate=2006-10-13 }} |
|||
| publisher=CIDRAP |
|||
*{{cite web |
|||
| url=http://www.nature.com/nature/focus/avianflu/index.html |
|||
| title=Nature Magazine focus on the global spread of H5N1 |
|||
| accessdate=2006-10-09 }} |
|||
*{{cite web |
|||
| url=http://www.cepr.net/publications/intellectual_property_2005_10.pdf |
|||
| title=Bird Flu Fears: Is There a Better Way to Develop Drugs? |
|||
| publisher=Center for Economic and Policy Research |
|||
| date=October 2005 |
|||
| accessdate=2006-10-09 |
|||
| author=Dean Baker |
|||
}} |
}} |
||
*{{cite web |
* {{cite web |
||
| url=http://www. |
| url=http://www.aafp.org/afp/20060901/783.html |
||
| publisher=American Family Physician |
|||
| title=Q&A: What is Bird Flu and Who's At Risk? |
|||
| title=Avian Influenza: Preparing for a Pandemic |
|||
| author=Robert Siegel and Melissa Block |
|||
| publisher=NPR |
|||
| date=October 20, 2005 |
|||
| accessdate=2006-10-09 |
|||
}} |
}} |
||
*{{cite journal |
|||
| url=http://www.nature.com/nature/journal/v435/n7041/full/435400a.html |
|||
| journal=Nature Magazine |
|||
| title=Avian flu special: The flu pandemic: were we ready? |
|||
| date=May 26, 2005 |
|||
| accessdate=2006-10-09 |
|||
| volume=435 |
|||
| pages=400-402 |
|||
| author=Declan Butler |
|||
}} Fictional account of flu epidemic. |
|||
*{{cite book |
|||
| url=http://www.nap.edu/openbook/0309095042/html/R1.html |
|||
| title=The Threat of Pandemic Influenza: Are We Ready? Workshop Summary (2005) |
|||
| author=Board on Global Health (BGH) |
|||
| publisher=Institute of Medicine of The National Academies |
|||
}} |
|||
*{{cite web |
|||
| url=http://www.time.com/time/asia/magazine/article/0,13673,501050207-1022651,00.html |
|||
| title=Emergency Measures |
|||
| publisher=Time Asia Edition |
|||
| date=January 31, 2005 |
|||
| accessdate=2006-10-09 |
|||
| author=Bryan Walsh and Kay Johnson |
|||
}} "Avian flu is on the rise in Vietnam and is now endemic in much of Asia. Can heightened vigilance keep it at bay?" |
|||
*{{cite web |
|||
| url=http://www.fluwikie.com/ |
|||
| title=Flu Wiki |
|||
| accessdate=2006-10-09 |
|||
}} Founded in June, 2005. |
|||
*{{cite web |
|||
| url=http://www.fluTrackers.com/ |
|||
| title=FluTrackers |
|||
| accessdate=2006-10-09 |
|||
}} Blog on avian influenza. Founded February, 2006. "Dedicated to the public health of the world's citizens by advancing policies, protocols, innovations, and practices that improve the health of vulnerable populations." |
|||
*{{cite web |
|||
| url=http://www.fao.org/ag/againfo/foto/EMPRES_Watch_global_flyways.gif |
|||
| title=H5N1 outbreaks in 2005 and major flyways of migratory birds |
|||
| format=Image |
|||
| publisher=FAO |
|||
| accessdate=2006-10-09 |
|||
| date=August 30, 2005 |
|||
| accessdate=2006-10-06 |
|||
}} |
|||
*{{cite web |
|||
| url=http://declanbutler.info/blog/?p=58 |
|||
| title=The spread of avian flu with time; new maps exploiting Google Earth's time series function |
|||
| date=September 17, 2006 |
|||
| accessdate=2006-10-09 |
|||
| author=Declan Butler |
|||
}} From the personal blog of a senior reporter with ''Nature''. |
|||
*{{cite web |
|||
| url=http://www.pandemicflu.gov/plan/pdf/panflu20060313.pdf |
|||
| publisher=Department of Health and Human Services |
|||
| title=Pandemic Planning Update A Report |
|||
| author=Michael O. Leavitt |
|||
| date=March 13, 2006 |
|||
| accessdate=2006-10-09 |
|||
}} This report outlines how the 3.3 billon dollar funding is being used to help achieve HHS's five primary objectives around Pandemic Response.. |
|||
*{{cite journal |
|||
| url=http://www.commondreams.org/headlines06/0226-02.htm |
|||
| title=Factory Farms Blamed for Spread of Bird Flu |
|||
| date=February 26, 2006 |
|||
| author=Geoffrey Lean |
|||
| publisher=The Independent |
|||
| accessdate=2006-10-09 |
|||
}} |
|||
*{{cite web |
|||
| url=http://www.influenza-pandemic.com |
|||
| title=Global Influenza Pandemic |
|||
| accessdate=2006-10-09 |
|||
}} "A compendium of information on the H5N1 strain of bird flu." |
|||
*{{cite news |
|||
| url=http://www.fwi.co.uk/Articles/2006/06/01/89977/Avian+Flu+special+report.htm |
|||
| title=Avian Flu special report |
|||
| publisher=Farmer's Weekly |
|||
| date=June 1, 2006 |
|||
| accessdate=2006-10-10 |
|||
}} Special report on avian flu & its effect on UK agriculture. |
|||
{{Influenza}} |
|||
=== News sources === |
|||
*{{cite web |
|||
| url=http://news.google.com/news?q=H5N1&hl=en&lr=&sa=N&tab=wn |
|||
| title=Google news on "H5N1" |
|||
| accessdate=2006-10-10 |
|||
}} |
|||
*{{cite web |
|||
| url=http://www.scidev.net/ms/bird_flu |
|||
| title=Bird Flu News Focus |
|||
| publisher=[[scidev|SciDev.Net]] |
|||
| accessdate=2006-10-10 |
|||
}} Regularly updated with the latest news stories. |
|||
*{{cite web |
|||
| url=http://diplomacymonitor.com/stu/dm.nsf/issued?openform&cat=Bird_Flu |
|||
| title=Diplomacy Monitor - Bird Flu |
|||
| publisher=St. Thomas University School of Law |
|||
| accessdate=2006-10-10 |
|||
}} |
|||
*{{cite web |
|||
| url=http://www.newsnow.co.uk/newsfeed/?name=Bird+Flu&x=7&y=5 |
|||
| title=Bird Flu |
|||
| publisher=NewsNow |
|||
| accessdate=2006-10-10 |
|||
}} Updated every five minutes with news from over 22,000 sources |
|||
[[Category:Bird diseases]] |
|||
[[Category:Pandemics]] |
[[Category:Pandemics]] |
||
[[Category:Epidemiology]] |
[[Category:Epidemiology]] |
||
| Line 430: | Line 465: | ||
[[Category:H5N1]] |
[[Category:H5N1]] |
||
[[wa:Minêye del pesse des oujheas å virûsse H5N1]] |
|||
[[de:Influenza A/H5N1: Ausbreitung 1997-2006]] |
|||
[[fr:État de l'épidémie de grippe aviaire dans le monde]] |
|||
[[nl:H5N1-chronologie]] |
|||
[[fi:H5N1:n levinneisyys]] |
|||
Revision as of 04:04, 28 October 2006
 |
| Influenza (flu) |
|---|
 |
H5N1 flu refers to the transmission and infection of H5N1. H5N1 flu is a concern due to the global spread of H5N1 that constitutes a pandemic threat. This article is about the transmission of the H5N1 virus, infection by that virus, the resulting symptoms of that infection (having or coming down with influenza or more specifically avian flu or even more specifically H5N1 flu which can include pneumonia), and the medical response including treatment.
Infected birds pass on H5N1 through their saliva, nasal secretions, and feces. Other birds may pick up the virus through direct contact with these excretions or when they have contact with surfaces contaminated with this material. Because migratory birds are among the carriers of the H5N1 virus it may spread to all parts of the world. Past outbreaks of avian flu have often originated in crowded conditions in southeast and east Asia, where humans, pigs, and poultry live in close quarters. In these conditions a virus is more likely to mutate into a form that more easily infects humans.
The majority of H5N1 flu cases have been reported in southeast and east Asia. Once an outbreak is detected, local authorities often order a mass slaughter of birds or animals affected. If this is done promptly, an outbreak of avian flu may be prevented. However, the United Nations (UN) World Health Organization (WHO) has expressed concern that not all countries are reporting outbreaks as completely as they should. China, for example, is known to have initially denied past outbreaks of severe acute respiratory syndrome (SARS) and HIV, although there have been some signs of improvement regarding its openess in recent months, particularly with regard to H5N1.
H5N1 infections in humans are generally caused by bird to human transmission of the virus. Until May 2006, the WHO estimate of the number of human to human transmission had been "two or three cases". On May 24, 2006, Dr. Julie L. Gerberding, director of the United States Centers for Disease Control and Prevention in Atlanta, estimated that there had been "at least three." On May 30, Maria Cheng, a WHO spokeswoman, said there were "probably about half a dozen," but that no one "has got a solid number."[1] A few isolated cases of suspected human to human transmission exist.[2] with the latest such case in June 2006 (among members of a family in Sumatra).[3] No pandemic strain of H5N1 has yet been found. The key point is that, at present, "the virus is not spreading efficiently or sustainably among humans."[4]
There is also concern, although no definitive proof, that other animals — particularly cats — may be able to act as a bridge between birds and humans. So far several cats have been confirmed to have died from H5N1 and the fact that cats have regular close contact with both birds and humans means monitoring of H5N1 in cats will need to continue.
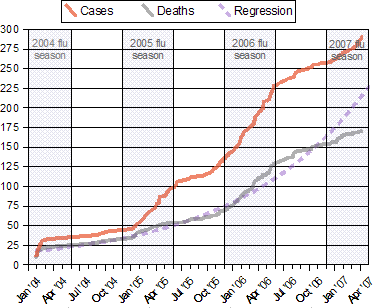 Notes:
|
H5N1 vaccines for chickens exists and is sometimes used, although there are many difficulties that make deciding if it helps more or hurts more especially difficult. H5N1 pre-pandemic vaccines exist in quanties sufficient to inoculate a few million people[5] and might be useful for priming to "boost the immune response to a different H5N1 vaccine tailor-made years later to thwart an emerging pandemic".[6] H5N1 pandemic vaccines and technologies to rapidly create them are in the H5N1 clinical trials stage but can not be verified as useful until after there exists a pandemic strain.
Avian flu in birds
According to Avian Influenza by Timm C. Harder and Ortrud Werner:
- Following an incubation period of usually a few days (but rarely up to 21 days), depending upon the characteristics of the isolate, the dose of inoculum, the species, and age of the bird, the clinical presentation of avian influenza in birds is variable and symptoms are fairly unspecific.[7] Therefore, a diagnosis solely based on the clinical presentation is impossible. The symptoms following infection with low pathogenic AIV may be as discrete as ruffled feathers, transient reductions in egg production or weight loss combined with a slight respiratory disease.[8] Some LP strains such as certain Asian H9N2 lineages, adapted to efficient replication in poultry, may cause more prominent signs and also significant mortality.[9][10] In its highly pathogenic form, the illness in chickens and turkeys is characterised by a sudden onset of severe symptoms and a mortality that can approach 100% within 48 hours.[11][12]
Poultry farming practices have changed due to H5N1:
- killing millions of poultry
- vaccinating poultry against bird flu
- vaccinating poultry workers against human flu
- limiting travel in areas where H5N1 is found
- increasing farm hygiene
- reducing contact between livestock and wild birds
- reducing open-air wet markets
- limiting workers contact with cock fighting
- reducing purchases of live fowl
- improving veterinary vaccine availability and cost. [13]
For example, after nearly two years of using mainly culling to control the virus, the Vietnamese government in 2005 adopted a combination of mass poultry vaccination, disinfecting, culling, information campaigns and bans on live poultry in cities.[14]
Webster et al write
- Transmission of highly pathogenic H5N1 from domestic poultry back to migratory waterfowl in western China has increased the geographic spread. The spread of H5N1 and its likely reintroduction to domestic poultry increase the need for good agricultural vaccines. In fact, the root cause of the continuing H5N1 pandemic threat may be the way the pathogenicity of H5N1 viruses is masked by cocirculating influenza viruses or bad agricultural vaccines."[15]
Dr. Robert Webster explains: "If you use a good vaccine you can prevent the transmission within poultry and to humans. But if they have been using vaccines now [in China] for several years, why is there so much bird flu? There is bad vaccine that stops the disease in the bird but the bird goes on pooping out virus and maintaining it and changing it. And I think this is what is going on in China. It has to be. Either there is not enough vaccine being used or there is substandard vaccine being used. Probably both. It’s not just China. We can’t blame China for substandard vaccines. I think there are substandard vaccines for influenza in poultry all over the world." [16] In response to the same concerns, Reuters reports Hong Kong infectious disease expert Lo Wing-lok saying, "The issue of vaccines has to take top priority," and Julie Hall, in charge of the WHO's outbreak response in China, saying China's vaccinations might be masking the virus." [17] The BBC reported that Dr Wendy Barclay, a virologist at the University of Reading, UK said: "The Chinese have made a vaccine based on reverse genetics made with H5N1 antigens, and they have been using it. There has been a lot of criticism of what they have done, because they have protected their chickens against death from this virus but the chickens still get infected; and then you get drift - the virus mutates in response to the antibodies - and now we have a situation where we have five or six 'flavours' of H5N1 out there." [18]
Transmission by wild birds (waterfowl)

According to the United Nations FAO: there is no denying the fact that wild water fowl most likely play a role in the avian influenza cycle and could be the initial source for AI viruses, which may be passed on through contact with resident water fowl or domestic poultry, particularly domestic ducks. The virus undergoing mutations could circulate within the domestic and possibly resident bird populations until HPAI arises. This new virus is pathogenic to poultry and possibly to the wild birds that it arose from. Wild birds found to have been infected with HPAI were either sick or dead. This could possibly affect the ability of these birds to carry HPAI for long distances. However, the findings in Qinghai Lake-China, suggest that H5N1 viruses could possibly be transmitted between migratory birds. Additionally, the new outbreaks of HPAI in poultry and wild birds in Russia, Kazakhstan, Western China and Mongolia may indicate that migratory birds probably act as carriers for the transport of HPAI over longer distances. Short distance transmission between farms, villages or contaminated local water bodies is likewise a distinct possibility. The AI virus has adapted to the environment in ways such as: 1) the use of water for survival and to spread 2) has evolved in a reservoir (ducks) strictly tied to water. The water in turn influences movement, social behaviour and migration patterns of water bird species. It is therefore of great importance to know the ecological strategy of influenza virus as well, in order to fully understand this disease and to control outbreaks when they occur. There remains a body of data and analysis missing on the collection and detection of HPAI viruses in wild birds. Finding HPAI viruses in wild birds may be a rare event, but if the contact with susceptible species occurs it can cause an outbreak at the local level or in distant areas. [19]
Prevention
The current method of prevention in animal populations is to destroy infected animals, as well as animals suspected of being infected. In southeast Asia, millions of domestic birds have been slaughtered to prevent the spread of the virus.
The probability of a "humanized" form of H5N1 emerging through genetic recombination in the body of a human co-infected with H5N1 and another influenza virus type (a process called reassortment) could be reduced by influenza vaccination of those at risk for infection by H5N1. It is not clear at this point whether vaccine production and immunization could be stepped up sufficiently to meet this demand. Additionally, vaccination of only humans would not address the possibility or reassortment in pigs, cats, or other mammal hosts.
If an outbreak of pandemic flu does occur, its spread might be slowed by increasing hygiene in aircraft, and by examining airline cabin air filters for presence of H5N1 virus.
The American Centers for Disease Control and Prevention advises travelers to areas of Asia where outbreaks of H5N1 have occurred to avoid poultry farms and animals in live food markets [20]. Travelers should also avoid surfaces that appear to be contaminated by feces from any kind of animal, especially poultry.
There are several H5N1 vaccines for several of the avian H5N1 varieties. H5N1 continually mutates rendering them, so far for humans, of little use. While there can be some cross-protection against related flu strains, the best protection would be from a vaccine specifically produced for any future pandemic flu virus strain. Dr. Daniel Lucey, co-director of the Biohazardous Threats and Emerging Diseases graduate program at Georgetown University has made this point, "There is no H5N1 pandemic so there can be no pandemic vaccine." [21] However, "pre-pandemic vaccines" have been created; are being refined and tested; and do have some promise both in furthering research and preparedness for the next pandemic [22]. Vaccine manufacturing companies are being encouraged to increase capacity so that if a pandemic vaccine is needed, facilities will be available for rapid production of large amounts of a vaccine specific to a new pandemic strain.
It is not likely that use of antiviral drugs could prevent the evolution of a pandemic flu virus. [23]
Environmental survival
Avian flu virus can last forever at a temperature dozens of degrees below freezing, as is found in the northern most areas that migratory birds frequent.
Heat kills H5N1 (i.e. inactivates the virus):
- Over 30 days at 0ºC (32.0ºF) (over one month at freezing temperature)
- 6 days at 37ºC (98.6ºF) (one week at human body temperature)
- 30 minutes 60ºC (140.0ºF) (half hour at a temperature that causes first and second degree burns in humans in ten seconds)[24]
Inactivation of the virus also occurs under the following conditions:
- Acidic pH conditions
- Presence of oxidizing agents such as sodium dodecyl sulfate, lipid solvents, and B-propiolactone
- Exposure to disinfectants: formalin, iodine compounds [25]
Incubation
The human incubation period of avian influenza A (H5N1) is 2 to 17 days[26]. Once infected, the virus can spread by cell-to-cell contact, bypassing receptors. So even if a strain is very hard to initially catch, once infected, it spreads rapidly within a body.[27]
Symptoms
- See also Pneumonia.
Avian influenza HA bind alpha 2-3 sialic acid receptors while human influenza HA bind alpha 2-6 sialic acid receptors. Usually other differences also exist. There is as yet no human form of H5N1, so all humans who have caught it so far have caught avian H5N1.
Human flu symptoms usually include fever, cough, sore throat, muscle aches, conjunctivitis and, in severe cases, severe breathing problems and pneumonia that may be fatal. The severity of the infection will depend to a large part on the state of the infected person's immune system and if the victim has been exposed to the strain before, and is therefore partially immune. No one knows if these or other symptoms will be the symptoms of a humanized H5N1 flu.
Highly pathogenic H5N1 avian flu in a human is far worse, killing over 50% of humans that catch it. In one case, a boy with H5N1 experienced diarrhea followed rapidly by a coma without developing respiratory or flu-like symptoms. [28]
There have been studies of the levels of cytokines in humans infected by the H5N1 flu virus. Of particular concern is elevated levels of tumor necrosis factor alpha (TNF?), a protein that is associated with tissue destruction at sites of infection and increased production of other cytokines. Flu virus-induced increases in the level of cytokines is also associated with flu symptoms including fever, chills, vomiting and headache. Tissue damage associated with pathogenic flu virus infection can ultimately result in death [29]. The inflammatory cascade triggered by H5N1 has been called a 'cytokine storm' by some, because of what seems to be a positive feedback process of damage to the body resulting from immune system stimulation. H5N1 type flu virus induces higher levels of cytokines than the more common flu virus types such as H1N1 [30] Other important mechanisms also exist "in the acquisition of virulence in avian influenza viruses" according to the CDC.[31]
The NS1 protein of the highly pathogenic avian H5N1 viruses circulating in poultry and waterfowl in Southeast Asia is currently believed to be responsible for the enhanced proinflammatory cytokine response. H5N1 NS1 is characterized by a single amino acid change at position 92. By changing the amino acid from glutamic acid to aspartic acid, researchers were able to abrogate the effect of the H5N1 NS1. This single amino acid change in the NS1 gene greatly increased the pathogenicity of the H5N1 influenza virus.
In short, this one amino acid difference in the NS1 protein produced by the NS RNA molecule of the H5N1 virus is believed to be largely responsible for an increased pathogenicity (on top of the already increased pathogenicity of its hemagglutinin type which allows it to grow in organs other than lungs) that can manifest itself by causing a cytokine storm in a patient's body, often causing pneumonia and death.
Treatment
Neuraminidase inhibitors are a class of drugs that includes zanamivir and oseltamivir, the latter being licensed for prophylaxis treatment in the United Kingdom. Oseltamivir inhibits the influenza virus from spreading inside the user's body [23]. It is marketed by Roche as Tamiflu. This drug has become a focus for some governments and organizations trying to be seen as making preparations for a possible H5N1 pandemic. In August 2005, Roche agreed to donate three million courses of o be deployed by the WHO to contain a pandemic in its region of origin. Although Tamiflu is patented, international law gives governments wide freedom to issue compulsory licenses for life-saving drugs.
A second class of drugs, which include amantadine and rimantadine, target the M2 protein, but are ineffective against H5N1. Unlike zanamivir and oseltamivir, these drugs are inexpensive and widely available and the WHO had initially planned to use them in efforts to combat an H5N1 pandemic. However, the potential of these drugs was considerably lessened when it was discovered that farmers in China have been administering amantadine to poultry with government encouragement and support since the early 1990s, against international livestock regulations; the result has been that the strain of the virus now circulating in South East Asia is largely resistant to these medications and hence significantly more dangerous to humans[32].
- However, recent data suggest that some strains of H5N1 are susceptible to the older drugs. An analysis of more than 600 H5N1 viruses collected in Southeast Asia showed that most samples from China and Indonesia lacked genetic characteristics signaling resistance to amantadine, whereas most samples from Vietnam, Thailand, and Cambodia had those characteristics. The report was published by the Journal of Infectious Diseases. The new WHO guidelines were drawn up by an international group of clinicians with experience treating H5N1 patients, along with other experts, at a meeting in late March. The panel systematically reviewed and graded the evidence for the drugs' effectiveness. Since no results from controlled trials of medication use in H5N1 cases are available, "Overall, the quality of the underlying evidence for all recommendations was very low," the 138-page WHO report states. The evidence includes results of lab and animal studies and indirect evidence from studies of antiviral use in patients with seasonal influenza. The recommendations are classified as "strong" or "weak," depending on the quality of the relevant evidence. The WHO says that if a patient has a confirmed or strongly suspected H5N1 case and NIs are available, "Clinicians should administer oseltamivir treatment (strong recommendation); zanamivir might be used as an alternative (weak recommendation)." Oseltamivir comes in capsule form, whereas zanamivir is taken with an inhaler. The WHO says zanamivir has lower bioavailability outside the respiratory tract than oseltamivir, but it may be active against some strains of oseltamivir-resistant H5N1 virus.[33]
Mortality rate
 Source: WHO Confirmed Human Cases of H5N1
|
A strain of H5N1 killed chickens in 1959 in Scotland and turkeys in 1991 in England. This strain was "highly pathogenic" (deadly to birds) but caused neither illness nor death in humans.[34] "The precursor of the H5N1 influenza virus that spread to humans in 1997 was first detected in Guangdong, China, in 1996, when it caused a moderate number of deaths in geese and attracted very little attention." [35] In 1997, in Hong Kong, 18 humans were infected and 6 died in the first known case of H5N1 infecting humans. [36] H5N1 had evolved from a zero mortality rate to a 33% mortality rate.
By 2003 H5N1 infection was detected in three flocks in the Republic of Korea.[citation needed] This strain caused asymptomatic infections in humans and has died out, meaning that its low mortality level is no more relevant than the 1959 strain's low mortality rate.[37] [38] The apparently extinct strain that caused Vietnam's human deaths from H5N1 in 2003, 2004 and 2005 also had a lower case mortality rate than the currently existing strains.[38] Changes are occurring in H5N1 that are increasing its pathogenicity in mammals.[39]
In 2005, 42 of 97 people confirmed by the WHO to be infected with H5N1 died -- or 43%. From January 1 2006 to October 16 2006, the case fatality ratio has been higher, with 73 deaths among 109 WHO-confirmed cases [40]-- or 67%. This has been interpreted by some to mean that the virus itself is becoming more deadly over time. [41] The global case fatality ratio is, nonetheless, a crude summary of a complex situation with many contributing factors. In particular, if an influenza pandemic arises from one of the currently circulating strains of Asian lineage HPAI A(H5N1), the mortality rates for the resulting human adapted influenza strain cannot be predicted with any confidence.
H5N1 is currently much better adapted to birds than to other hosts, which is why the disease it causes is called a bird flu. No pandemic strain of H5N1 has yet been found. The precise nature and extent of the genetic alterations that might change one of the currently circulating avian flu strains into a human flu strain cannot be known in advance. While many of the current H5N1 strains circulating in birds can generate a dangerous cytokine storm in healthy adult humans [42][43], the ultimate pandemic strain might arise from a less-lethal strain, or its current level of lethality might be lost in the adaptation to a human host.
The global case fatality ratio looks only to the official tally of cases confirmed by the WHO. It takes no account of other cases, such as those appearing in press reports. Nor does it reflect any estimate of the global extent of mild, asymptomatic, or other cases which are undiagnosed, unreported by national governments to the WHO, or for any reason cannot be confirmed by the WHO. While the WHO's case count is clearly the most authoritative, these unavoidable limitations result in an unknown number of cases being omitted from it. The problem of overlooked but genuine cases is emphasized by occasional reports in which later serology reveals antibodies to the H5N1 infection in the blood of persons who were never known to have bird flu, and who then are confirmed by the WHO only retroactively as "cases." Press reports of such cases, often poultry handlers, have appeared in various countries. The largest number of asymptomatic cases was recently confirmed among Korean workers who had assisted in massive culls of H5N1-infected poultry.[44] This relatively benign Korean strain of H5N1 has died out, and the remaining strains of H5N1 have a higher case fatality rate in humans.
Unconfirmed cases have a potentially huge impact on the case fatality ratio. This mathematical impact is well-understood by epidemiologists, and is easy to see in theory. For example, if for each confirmed case reported by the WHO we assume that there has been another mild and unreported case, the actual global number of cases would be double the current number of WHO-confirmed cases. The fatality ratio for H5N1 infections would then be calculated as the same number of deaths, but divided by a doubled number for total cases, resulting in a hypothetical death ratio of half the currently-reported fatality ratio. Such a result would indicate to epidemiologists that the world was confronting an H5N1 virus that is less-lethal than currently assumed, although possibly one that was more contagious and difficult to track.
A case-fatality ratio based on an accurate and all-inclusive count of cases would be invaluable, but unfortunately it is impossible to attain. The ability to diagnose every case of H5N1 as it arises does not exist. A few reported studies have attempted to gather preliminary data on this crucial statistic, by carrying out systematic blood testing of neighbors and contacts of fatal cases in villages where there had been confirmed H5N1 fatalities. This testing failed to turn up any overlooked mild cases. [45] [46] These methodical studies of contacts provide significant evidence that the high death rate among confirmed cases in the villages where these studies were carried out cannot be simply attributed to a wholesale failure to detect mild cases. Unfortunately, these studies are likely to remain too few and sketchy to define the complex situation worldwide regarding the lethality of the varying H5N1 clades. The testing and reporting necessary for mass serology studies to determine the incidence of overlooked cases for each existing clade and strain of H5N1 worldwide would be prohibitively costly.
Hence the precise allocation of infections by the various H5N1 clades across the spectrum including lethal, serious, mild, and asymptomatic cases is likely to remain unknown in both humans and the hundreds of other species it can infect. Scientists are very concerned about what we do know about H5N1; but even more concerned about the vast amount of important data that we don't know about H5N1 and its future mutations.
A case fatality ratio of over 50% provides a grim backdrop for the fact that the currently circulating H5N1 strains have certain genetic similarities with the Spanish Influenza pandemic virus. In that pandemic, 50 million to 100 million people worldwide were killed during about a year in 1918 and 1919 [47].
Review of patient ages and outcomes reveals that H5N1 attacks are especially lethal in pre-adults and young adults, while older victims tend to have milder attacks and to survive. [48] This is consistent with the frequent development of a cytokine storm in the afflicted.[49] Very few persons over 50 years of age died after suffering a H5N1 attack. Instead, the age-fatality curve of H5N1 influenza attacks in humans resembles that of the 1918 Spanish pandemic flu, and is the opposite of the mortality curve of seasonal flu strains, since seasonal influenza preferentially kills the elderly and does not kill by cytokine storm.
Another factor complicating any attempt to predict lethality of an eventual pandemic strain is that many human victims of the current H5N1 influenza have been blood relatives (but rarely spouses) of other victims. This data suggests that the victims' genetic susceptibility may have played a role in the human cases registered to date.
Mortality rate in planning reports
Governments and other organisations at many levels and in many places have produced "planning" reports that, among other things, offer speculation on the mortality rate of an eventual pandemic. One such report states that "over half a million Americans could die and over 2.3 million could be hospitalized if a moderately severe strain of a pandemic flu virus hits the U.S."[50]. No one knows if "moderately severe" is an accurate guess or not. This report entitled A Killer Flu?[51] shows an assumed (guessed) contraction rate of 25% and a severity similar to low severity flu pandemics causing 180 thousand deaths in the US and a 1918 level severity rate causing one million deaths in the US. There is no evidence an H5N1 flu pandemic would be between these figures[52] as no data is available reflecting similar virulance in any earlier flu strain as it emerged. The relatively low mortality rate in these and other such reports can not, therefore, be taken as reliable predictions of what the mortality rate of an H5N1 pandemic might be. The low assumed mortality rate does, however, serve the purpose of the reports, which is to show that we are not prepared even for severity levels that have occurred in the past[53], let alone the much higher case fatality ratios seen more recently.
Notes and references
- ^ Donald G. McNeil Jr. (June 4 2006). "Human Flu Transfers May Exceed Reports". New York Times.
{{cite news}}: Check date values in:|date=(help) - ^ "Seven Indonesian Bird Flu Cases Linked to Patients". Bloomberg. May 23, 2006.
- ^ "WHO confirms human transmission< in Indonesian bird flu cluster".
- ^ "Avian influenza – situation in Indonesia – update 17". WHO. June 6 2006.
{{cite news}}: Check date values in:|date=(help) - ^ "HHS has enough H5N1 vaccine for 4 million people". CIDRAP. July 5, 2006.
- ^ "Study supports concept of 2-stage H5N1 vaccination". CIDRAP. October 13, 2006.
- ^ A.R. Elbers, G. Kock and A. Bouma (2005). "Performance of clinical signs in poultry for the detection of outbreaks during the avian influenza A (H7N7) epidemic in The Netherlands in 2003". Avian Pathol. 34: 181-7.
- ^ I. Capua and F. Mutinelli (2001). "Low pathogenicity (LPAI) and highly pathogenic (HPAI) avian influenza in turkeys and chicken". A Colour Atlas and Text on Avian Influenza: 13-20.
- ^ S. Bano S, K. Naeem K, S.A. Malik (2003). "Evaluation of pathogenic potential of avian influenza virus serotype H9N2 in chicken". Avian Dis. 47, Suppl: 17-22.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ C Li, K Yu, G TiaG, D Yu, L Liu, B Jing, J Ping, H. Chen (2005). "Evolution of H9N2 influenza viruses from domestic poultry in Mainland China". Virology. 340: 70-83.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ D.E. Swayne, D.L. Suarez (2000). "Highly pathogenic avian influenza". Rev Sci Tech. 19: 463-8.
- ^ Timm C. Harder and Ortrud Werner. "Avian Influenza". Influenza Report.
- ^ "The Threat of Global Pandemics". Council on Foreign Relations. June 16, 2005. Retrieved 2006-09-15.
- ^ "Vietnam to unveil advanced plan to fight bird flu". Reuters. April 28, 2006.
- ^ Robert G. Webster; et al. (January, 2006). "H5N1 Outbreaks and Enzootic Influenza". Emerging Infectious Diseases. Retrieved 2006-09-15.
{{cite journal}}: Check date values in:|date=(help); Explicit use of et al. in:|author=(help) - ^ "Expert: Bad vaccines may trigger China bird flu". MSNBC. December 30, 2005. Retrieved 2006-09-15.
- ^
"China H5N1 outbreak puts vaccines under spotlight". Reuters. March 19, 2006.
{{cite news}}:|access-date=requires|url=(help) This reference is apparently no longer available online via Reuters. It is available as of 21 August, 2006 at [1] - ^ "Bird flu vaccine no silver bullet". BBC. February 22, 2006. Retrieved 2006-09-15.
- ^ "Wild birds and Avian Influenza". FAO. Retrieved 2006-09-15.
- ^ National Center for Infectious Diseases, Division of Global Migration and Quarantine (March 24, 2005). "Interim Guidance about Avian Influenza A (H5N1) for U.S. Citizens Living Abroad". Travel Notices. U.S. Centers for Disease Control and Prevention. Retrieved 2006-10-27.
{{cite web}}: Check date values in:|date=(help) - ^ Jennifer Schultz (November 28 2005). "Bird flu vaccine won't precede pandemic". United Press International.
{{cite news}}:|access-date=requires|url=(help); Check date values in:|date=(help); Unknown parameter|url-http://www.upi.com/ConsumerHealthDaily/view.php?StoryID=ignored (help) - ^ Promising research into vaccines includes:
- Martin Enserink (August 12 2005). "Avian Influenza: 'Pandemic Vaccine' Appears to Protect Only at High Doses". Science. 309: 996. doi:10.1126/science.309.5737.996b.
{{cite journal}}: Check date values in:|date=(help) - "GlaxoSmithKline Initiates Human Trial Programme With Two H5N1 Pandemic Flu Vaccines" (PDF). March 30 2006. Retrieved 2006-10-27.
{{cite news}}: Check date values in:|date=(help) - "Murtha eager to speed vaccine". January 28 2006. Retrieved 2006-10-27.
{{cite news}}: Check date values in:|date=(help); Unknown parameter|source=ignored (help) A promising new bird flu vaccine developed by University of Pittsburgh researchers could provide better protection and be made more quickly than other experimental vaccines.
- Martin Enserink (August 12 2005). "Avian Influenza: 'Pandemic Vaccine' Appears to Protect Only at High Doses". Science. 309: 996. doi:10.1126/science.309.5737.996b.
- ^ a b "Oseltamivir (Tamiflu)". National Institutes of Health. January 13, 2000. Revised on January 10, 2001.
- ^ "Hot Water Burn & Scalding Graph". Retrieved 2006-09-15.
- ^ "Avian flu biofacts". CIDRAP.
- ^ Full text article online: The Writing Committee of the World Health Organization (WHO) Consultation on Human Influenza A/H5 (September 29 2005). "Avian Influenza A (H5N1) Infection in Humans". New England Journal of Medicine. 353: 1374–1385.
{{cite journal}}: Check date values in:|date=(help)CS1 maint: numeric names: authors list (link) - ^ T Jacob John (November 12, 2005). "Bird Flu: Public Health Implications for India". Economic and Political Weekly.
- ^ "Fatal Avian Influenza A (H5N1) in a Child Presenting with Diarrhea Followed by Coma". New England Journal of Medicine. 352 (7): 686–691. February 17 2005.
{{cite journal}}: Check date values in:|date=(help) - ^ Robert G. Webster and Elizabeth Jane Walker (2003). "Influenza: The world is teetering on the edge of a pandemic that could kill a large fraction of the human population". American Scientist. 91: 122.
- ^ M. C. Chan; et al. (2005). "Proinflammatory cytokine responses induced by influenza A (H5N1) viruses in primary human alveolar and bronchial epithelial cells". Respiratory Research. 6: 135.
{{cite journal}}: Explicit use of et al. in:|author=(help) - ^ Martin Hirst, Caroline R. Astell, Malachi Griffith, Shaun M. Coughlin, Michelle Moksa, Thomas Zeng; et al. (December 2004). "Novel Avian Influenza H7N3 Strain Outbreak, British Columbia". Emerg Infect Dis.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Alan Sipress (June 18, 2005). "Bird Flu Drug Rendered Useless: Chinese Chickens Given Medication Made for Humans". Washington Post.
- ^ "WHO sees role for older antivirals in some H5N1 cases". CIDRAP. May 22, 2006.
- ^ "Situation (poultry) in Asia: need for a long-term response, comparison with previous outbreaks". Disease Outbreak News: Avian influenza A(H5N1). WHO. March 2 2004. Retrieved 2006-10-27.
{{cite news}}: Check date values in:|date=(help) - ^ Robert G. Webster, Malik Peiris, Honglin Chen, and Yi Guan (January 2006). "H5N1 Outbreaks and Enzootic Influenza". Emerg Infect Dis. CDC. Retrieved 2006-10-28.
{{cite web}}: CS1 maint: multiple names: authors list (link) - ^ WHO (October 28, 2005). "H5N1 avian influenza: timeline" (PDF).
- ^ "Five Koreans had H5N1 virus but no illness". CIDRAP. September 21, 2006.
- ^ a b WHO (August 18 2006). "Antigenic and genetic characteristics of H5N1 viruses and candidate H5N1 vaccine viruses developed for potential use as pre-pandemic vaccines" (PDF).
{{cite web}}: Check date values in:|date=(help) Contains latest Evolutionary "Tree of Life" for H5N1 - ^ Chen H, Deng G, Li Z, Tian G, Li Y, Jiao P, Zhang L, Liu Z, Webster RG, Yu K. (2004). "The evolution of H5N1 influenza viruses in ducks in southern China". Proc. Natl. Acad. Sci. U. S. A. 101 (28): 10452–10457. PMID 15235128.
{{cite journal}}: CS1 maint: multiple names: authors list (link) Full Text - ^ "Cumulative Number of Confirmed Human Cases of Avian Influenza A/(H5N1) Reported to WHO". WHO. October 16, 2006.
- ^ "H5N1 Getting Deadlier". based on the article "Bird Flu Fatality Rate in Humans Climbs to 64% as Virus Spreads".
- ^ "Clinical study points to cytokine storm in H5N1 cases". CIDRAP News. September 11, 2006.
- ^ Menno D de Jong; et al. (September 10, 2006). "Fatal outcome of human influenza A (H5N1) is associated with high viral load and hypercytokinemia". Nature.
{{cite journal}}: Explicit use of et al. in:|author=(help) Published online. - ^ "Five Koreans had H5N1 virus but no illness (Sep 21,2006)". CIDRAP. Retrieved 2006-08-23.
- ^ "Mild H5N1 cases weren't found missed in Cambodian outbreak study". CIDRAP. March 27, 2006.
- ^ "Cambodian study suggests mild H5N1 cases are rare". CIDRAP. September 7, 2006.
- ^ "The Threat of Pandemic Influenza: Are We Ready? Workshop Summary (2005)". NAP. Retrieved 2006-08-21.
- ^ "Human Avian Influenza A(H5N1) Cases by Age Group and Country".
- ^ "Immediate Treatment Needed for Bird Flu Cases, Study Says". New York Times. September 11, 2006.
- ^ "Pandemic Flu Projection Says More Than Half Million Could Die in U.S." Senior Journal. June 24, 2005.
- ^ "Healthy Americans Full report PDF" (PDF).
- ^ "A Dramatic Disconnect". Newsweek. estimates two million dead in the US, for example
- ^ Dr. Martin Meltzer of the Centers for Disease Control, an expert on the societal impact of diseases, warns that “There is no healthcare system anywhere in the world that can cope with even a mild pandemic like the one in 1968.” Meltzer MI, Lancet Asia Forum, Singapore, May 2006
See also
Further reading
- "WHO Avian influenza resource (updated)".
- CDC "Facts About Avian Influenza (Bird Flu) and Avian Influenza A (H5N1) Virus".
{{cite web}}: Check|url=value (help) - "FAO information on Avian Influenza - Latest news, Disease Card, Maps, Animations".
- "Avian Influenza (Bird Flu): Agricultural and Wildlife Considerations". CIDRAP.
- "Avian Influenza: Preparing for a Pandemic". American Family Physician.
