Human eye
| The human eye | |
|---|---|
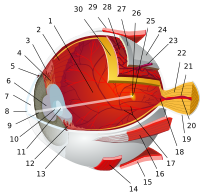
 1. vitreous body 2. ora serrata 3. ciliary muscle 4. ciliary zonules 5. canal of Schlemm 6. pupil 7. anterior chamber 8. cornea 9. iris 10. lens cortex 11. lens nucleus 12. ciliary process 13. conjunctiva 14. inferior oblique muscle 15. inferior rectus muscle 16. medial rectus muscle 17. retinal arteries and veins 18. optic disc 19. dura mater 20. central retinal artery 21. central retinal vein 22. optic nerve 23. vorticose vein 24. bulbar sheath 25. macula 26. fovea 27. sclera 28. choroid 29. superior rectus muscle 30. retina | |
| Identifiers | |
| MeSH | D005123 |
| TA98 | A01.1.00.007 A15.2.00.001 |
| TA2 | 113, 6734 |
| FMA | 54448 |
| Anatomical terminology | |
The human eye is an organ which reacts to light for several purposes. As a conscious sense organ, the mammalian eye allows vision. Rod and cone cells in the retina allow conscious light perception and vision including color differentiation and the perception of depth. The human eye can distinguish about 10 million colors.[1]
In common with the eyes of other mammals, the human eye's non-image-forming photosensitive ganglion cells in the retina receive the light signals which affect adjustment of the size of the pupil, regulation and suppression of the hormone melatonin and entrainment of the body clock.[2]

The eye is not properly a sphere, rather it is a fused two-piece unit. The smaller frontal unit, more curved, called the cornea is linked to the larger unit called the sclera. The corneal segment is typically about 8 mm (0.3 in) in radius. The sclerotic chamber constitutes the remaining five-sixths; its radius is typically about 12 mm. The cornea and sclera are connected by a ring called the limbus. The iris – he color of the eye – and its black center, the pupil, are seen instead of the cornea due to the cornea's transparency. To see inside the eye, an ophthalmoscope is needed, since light is not reflected out. The fundus (area opposite the pupil) shows the characteristic pale optic disk (papilla), where vessels entering the eye pass across and optic nerve fibers depart the globe.
Dimensions
The dimensions differ among adults by only one or two millimeters. The vertical measure, generally less than the horizontal distance, is about 24 mm among adults, at birth about 16–17 mm. (about 0.65 inch) The eyeball grows rapidly, increasing to 22.5–23 mm (approx. 0.89 in) by the age of three years. From then to age 13, the eye attains its full size. The volume is 6.5 ml (0.4 cu. in.) and the weight is 7.5 g (0.25 oz.).[citation needed]
Components
The eye is made up of three coats, enclosing three transparent structures. The outermost layer is composed of the cornea and sclera. The middle layer consists of the choroid, ciliary body, and iris. The innermost is the retina, which gets its circulation from the vessels of the choroid as well as the retinal vessels, which can be seen in an ophthalmoscope.
Within these coats are the aqueous humor, the vitreous body, and the flexible lens. The aqueous humor is a clear fluid that is contained in two areas: the anterior chamber between the cornea and the iris and exposed area of the lens. The lens is suspended to the ciliary body by the suspensory ligament (Zonule of Zinn), made up of fine transparent fibers. The vitreous body, the posterior chamber, is a clear jelly that is much larger than the aqueous humor, present behind lens and the rest, and is bordered by the sclera, zonule, and lens. They are connected via the pupil.[3]
Dynamic range
The retina has a static contrast ratio of around 100:1 (about 6.5 f-stops). As soon as the eye moves (saccades) it re-adjusts its exposure both chemically and geometrically by adjusting the iris which regulates the size of the pupil. Initial dark adaptation takes place in approximately four seconds of profound, uninterrupted darkness; full adaptation through adjustments in retinal chemistry (the Purkinje effect) are mostly complete in thirty minutes. Hence, a dynamic contrast ratio of about 1,000,000:1 (about 20 f-stops) is possible.[4] The process is nonlinear and multifaceted, so an interruption by light merely starts the adaptation process over again. Full adaptation is dependent on good blood flow; thus dark adaptation may be hampered by poor circulation, and vasoconstrictors like tobacco. [citation needed]
The eye includes a lens not dissimilar to lenses found in optical instruments such as cameras and the same principles can be applied. The pupil of the human eye is its aperture; the iris is the diaphragm that serves as the aperture stop. Refraction in the cornea causes the effective aperture (the entrance pupil) to differ slightly from the physical pupil diameter. The entrance pupil is typically about 4 mm in diameter, although it can range from 2 mm (f/8.3) in a brightly lit place to 8 mm (f/2.1) in the dark. The latter value decreases slowly with age, older people's eyes sometimes dilate to not more than 5-6mm. [citation needed]
Field of view
The approximate field of view of a human eye is 95° out, 75° down, 60° in, 60° up.[clarification needed] About 12–15° temporal and 1.5° below the horizontal is the optic nerve or blind spot which is roughly 7.5° high and 5.5° wide.[5]
Eye irritation

Eye irritation has been defined as “the magnitude of any stinging, scratching, burning, or other irritating sensation from the eye”.[6] It is a common problem experienced by people of all ages. Related eye symptoms and signs of irritation are e.g. discomfort, dryness, excess tearing, itching, grating, sandy sensation, smarting, ocular fatigue, pain, scratchiness, soreness, redness, swollen eyelids, and tiredness, etc. These eye symptoms are reported with intensities from severe to less severe. It has been suggested that these eye symptoms are related to different causal mechanisms.[7]
Several suspected causal factors in our environment have been studied so far.[8] One hypothesis is that indoor air pollution may cause eye and airway irritation.[9][10] Eye irritation depends somewhat on destabilization of the outer-eye tear film, in which the formation of dry spots results in such ocular discomfort as dryness.[9][11][12] Occupational factors are also likely to influence the perception of eye irritation. Some of these are lighting (glare and poor contrast), gaze position, a limited number of breaks, and a constant function of accommodation, musculoskeletal burden, and impairment of the visual nervous system.[13][14] Another factor that may be related is work stress.[15][16] In addition, psychological factors have been found in multivariate analyses to be associated with an increase in eye irritation among VDU users.[17][18] Other risk factors, such as chemical toxins/irritants, e.g. amines, formaldehyde, acetaldehyde, acrolein, N-decane, VOCs; ozone, pesticides and preservatives, allergens, etc. might cause eye irritation as well.
Certain volatile organic compounds that are both chemically reactive and airway irritants may cause eye irritation as well. Personal factors (e.g., use of contact lenses, eye make-up, and certain medications) may also affect destabilization of the tear film and possibly result in more eye symptoms.[7] Nevertheless, if airborne particles alone should destabilize the tear film and cause eye irritation, their content of surface-active compounds must be high.[7] An integrated physiological risk model with blink frequency, destabilization, and break-up of the eye tear film as inseparable phenomena may explain eye irritation among office workers in terms of occupational, climate, and eye-related physiological risk factors.[7]
There are two major measures of eye irritation. One is blink frequency which can be observed by human behavior. The other measures are break up time, tear flow, hyperemia (redness, swelling), tear fluid cytology, and epithelial damage (vital stains) etc., which are human beings’ physiological reactions. Blink frequency is defined as the number of blinks per minute and it is associated with eye irritation. Blink frequencies are individual with mean frequencies of < 2-3 to 20-30 blinks/minute, and they depend on environmental factors including the use of contact lenses. Dehydration, mental activities, work conditions, room temperature, relative humidity, and illumination all influence blink frequency. Break-up time (BUT) is another major measure of eye irritation and tear film stability.[19] It is defined as the time interval (in seconds) between blinking and rupture. BUT is considered to reflect the stability of the tear film as well. In normal persons, the break-up time exceeds the interval between blinks, and, therefore, the tear film is maintained.[20] Studies have shown that blink frequency is correlated negatively with break-up time. This phenomenon indicates that perceived eye irritation is associated with an increase in blink frequency since the cornea and conjunctiva both have sensitive nerve endings that belong to the first trigeminal branch.[21][22] Other evaluating methods, such as hyperemia, cytology etc. have increasingly been used to assess eye irritation.
There are other factors that related to eye irritation as well. Three major factors that influence the most are indoor air pollution, contact lenses and gender differences. Field studies have found that the prevalence of objective eye signs is often significantly altered among office workers in comparisons with random samples of the general population.[23][24][25][26] These research results might indicate that indoor air pollution has played an important role in causing eye irritation. There are more and more people wearing contact lens now and dry eyes appear to be the most common complaint among contact lens wearers.[27][28][29] Although both contact lens wearers and spectacle wearers experience similar eye irritation symptoms, dryness, redness, and grittiness have been reported far more frequently among contact lens wearers and with greater severity than among spectacle wearers.[29] Studies have shown that incidence of dry eyes increases with age.[30][31] especially among women.[32] Tear film stability (e.g. break-up time) is significantly lower among women than among men. In addition, women have a higher blink frequency while reading.[33] Several factors may contribute to gender differences. One is the use of eye make-up. Another reason could be that the women in the reported studies have done more VDU work than the men, including lower grade work. A third often-quoted explanation is related to the age-dependent decrease of tear secretion, particularly among women after 40 years of age.,[34][35][36]
In a study conducted by UCLA, the frequency of reported symptoms in industrial buildings was investigated.[37] The study's results were that eye irritation was the most frequent symptom in industrial building spaces, at 81%. Modern office work with use of office equipment has raised concerns about possible adverse health effects.[38] Since the 1970s, reports have linked mucosal, skin, and general symptoms to work with self-copying paper. Emission of various particulate and volatile substances has been suggested as specific causes. These symptoms have been related to Sick Building Syndrome (SBS), which involves symptoms such as irritation to the eyes, skin, and upper airways, headache and fatigue.[39]
Many of the symptoms described in SBS and multiple chemical sensitivity (MCS) resemble the symptoms known to be elicited by airborne irritant chemicals.[40] A repeated measurement design was employed in the study of acute symptoms of eye and respiratory tract irritation resulting from occupational exposure to sodium borate dusts.[41] The symptom assessment of the 79 exposed and 27 unexposed subjects comprised interviews before the shift began and then at regular hourly intervals for the next six hours of the shift, four days in a row.[41] Exposures were monitored concurrently with a personal real time aerosol monitor. Two different exposure profiles, a daily average and short term (15 minute) average, were used in the analysis. Exposure-response relations were evaluated by linking incidence rates for each symptom with categories of exposure.[41]
Acute incidence rates for nasal, eye, and throat irritation, and coughing and breathlessness were found to be associated with increased exposure levels of both exposure indices. Steeper exposure-response slopes were seen when short term exposure concentrations were used. Results from multivariate logistic regression analysis suggest that current smokers tended to be less sensitive to the exposure to airborne sodium borate dust.[41]
Several actions can be taken to prevent eye irritation—
- trying to maintain normal blinking by avoiding room temperatures that are too high; avoiding relative humidities that are too high or too low, because they reduce blink frequency or may increase water evaporation[7]
- trying to maintain an intact tear film by the following actions. 1) blinking and short breaks may be beneficial for VDU users.[42][43] Increase these two actions might help maintain the tear film. 2) downward gazing is recommended to reduce the ocular surface area and water evaporation.[44][45][46] 3) the distance between the VDU and keyboard should be kept as short as possible to minimize evaporation from the ocular surface area by a low direction of the gaze.[47] And 4) blink training can be beneficial.[48]
In addition, other measures are proper lid hygiene, avoidance of eye rubbing,[49] and proper use of personal products and medication. Eye make-up should be used with care.[50]
Eye movement

The visual system in the brain is too slow to process information if the images are slipping across the retina at more than a few degrees per second.[51] Thus, for humans to be able to see while moving, the brain must compensate for the motion of the head by turning the eyes. Another complication for vision in frontal-eyed animals is the development of a small area of the retina with a very high visual acuity. This area is called the fovea centralis, and covers about 2 degrees of visual angle in people. To get a clear view of the world, the brain must turn the eyes so that the image of the object of regard falls on the fovea. Eye movements are thus very important for visual perception, and any failure to make them correctly can lead to serious visual disabilities.
Having two eyes is an added complication, because the brain must point both of them accurately enough that the object of regard falls on corresponding points of the two retinas; otherwise, double vision would occur. The movements of different body parts are controlled by striated muscles acting around joints. The movements of the eye are no exception, but they have special advantages not shared by skeletal muscles and joints, and so are considerably different.
Extraocular muscles
Each eye has six muscles that control its movements: the lateral rectus, the medial rectus, the inferior rectus, the superior rectus, the inferior oblique, and the superior oblique. When the muscles exert different tensions, a torque is exerted on the globe that causes it to turn, in almost pure rotation, with only about one millimeter of translation.[52] Thus, the eye can be considered as undergoing rotations about a single point in the center of the eye.
Rapid eye movement
Rapid eye movement, or REM for short, typically refers to the sleep stage during which the most vivid dreams occur. During this stage, the eyes move rapidly. It is not in itself a unique form of eye movement.
Saccades
Saccades are quick, simultaneous movements of both eyes in the same direction controlled by the frontal lobe of the brain. Some irregular drifts, movements, smaller than a saccade and larger than a microsaccade, subtend up to six minutes of arc.
Microsaccades
Even when looking intently at a single spot, the eyes drift around. This ensures that individual photosensitive cells are continually stimulated in different degrees. Without changing input, these cells would otherwise stop generating output. Microsaccades move the eye no more than a total of 0.2° in adult humans.
Vestibulo-ocular reflex
The vestibulo-ocular reflex is a reflex eye movement that stabilizes images on the retina during head movement by producing an eye movement in the direction opposite to head movement, thus preserving the image on the center of the visual field. For example, when the head moves to the right, the eyes move to the left, and vice versa.
Smooth pursuit movement
The eyes can also follow a moving object around. This tracking is less accurate than the vestibulo-ocular reflex, as it requires the brain to process incoming visual information and supply feedback. Following an object moving at constant speed is relatively easy, though the eyes will often make saccadic jerks to keep up. The smooth pursuit movement can move the eye at up to 100°/s in adult humans.
It is more difficult to visually estimate speed in low light conditions or while moving, unless there is another point of reference for determining speed.
Optokinetic reflex
The optokinetic reflex is a combination of a saccade and smooth pursuit movement. When, for example, looking out of the window at a moving train, the eyes can focus on a 'moving' train for a short moment (through smooth pursuit), until the train moves out of the field of vision. At this point, the optokinetic reflex kicks in, and moves the eye back to the point where it first saw the train (through a saccade).
Near response
The adjustment to close-range vision involves three processes to focus an image on the retina.
Vergence movement

When a creature with binocular vision looks at an object, the eyes must rotate around a vertical axis so that the projection of the image is in the centre of the retina in both eyes. To look at an object closer by, the eyes rotate 'towards each other' (convergence), while for an object farther away they rotate 'away from each other' (divergence). Exaggerated convergence is called cross eyed viewing (focusing on the nose for example). When looking into the distance, or when 'staring into nothingness', the eyes neither converge nor diverge. Vergence movements are closely connected to accommodation of the eye. Under normal conditions, changing the focus of the eyes to look at an object at a different distance will automatically cause vergence and accommodation.
Pupil constriction
Lenses cannot refract light rays at their edges as well as they can closer to the center. The image produced by any lens is therefore somewhat blurry around the edges (spherical aberration). It can be minimized by screening out peripheral light rays and looking only at the better-focused center. In the eye, the pupil serves this purpose by constricting while the eye is focused on nearby objects. In this way the pupil has a dual purpose: to adjust the eye to variations in brightness and to reduce spherical aberration.[53]
Accommodation of the lens
A change in the curvature of the lens, accommodation is carried out by the ciliary muscles surrounding the lens contracting. This narrows the diameter of the ciliary body, relaxes the fibers of the suspernsory ligament, and allows the lens to relax into a more convex shape. A more convex lens refracts light more strongly and focuses divergent light rays onto the retina allowing for closer objects to be brought into focus.[54][55]
Effects of aging
There are many diseases, disorders, and age-related changes that may affect the eyes and surrounding structures.
As the eye ages certain changes occur that can be attributed solely to the aging process. Most of these anatomic and physiologic processes follow a gradual decline. With aging, the quality of vision worsens due to reasons independent of diseases of the aging eye. While there are many changes of significance in the nondiseased eye, the most functionally important changes seem to be a reduction in pupil size and the loss of accommodation or focusing capability (presbyopia). The area of the pupil governs the amount of light that can reach the retina. The extent to which the pupil dilates decreases with age, leading to a substantial decrease in light received at the retina. In comparison to younger people, it is as though older persons are constantly wearing medium-density sunglasses. Therefore, for any detailed visually guided tasks on which performance varies with illumination, older persons require extra lighting. Certain ocular diseases can come from sexually transmitted diseases such as herpes and genital warts. If contact between eye and area of infection occurs, the STD can be transmitted to the eye.[56]
With aging a prominent white ring develops in the periphery of the cornea- called arcus senilis. Aging causes laxity and downward shift of eyelid tissues and atrophy of the orbital fat. These changes contribute to the etiology of several eyelid disorders such as ectropion, entropion, dermatochalasis, and ptosis. The vitreous gel undergoes liquefaction (posterior vitreous detachment or PVD) and its opacities — visible as floaters — gradually increase in number.
Various eye care professionals, including ophthalmologists, optometrists, and opticians, are involved in the treatment and management of ocular and vision disorders. A Snellen chart is one type of eye chart used to measure visual acuity. At the conclusion of a complete eye examination, the eye doctor might provide the patient with an eyeglass prescription for corrective lenses. Some disorders of the eyes for which corrective lenses are prescribed include myopia (near-sightedness) which affects about one-third[citation needed] of the human population, hyperopia (far-sightedness) which affects about one quarter of the population, astigmatism, and presbyopia, the loss of focusing range during aging.
Eye care professionals
The human eye contains enough complexity to warrant specialized attention and care beyond the duties of a general practitioner. These specialists, or eye care professionals, serve different functions in different countries. Each eye care professional can typically be categorized into one or a multiplicity (i.e. an ophthalmologist can perform surgery; and in some instances prescribe lenses, which is a duty often performed by optometrists) of duties of the following types of professionals:
See also
- Eye color
- Mammalian eye
- Optometry
- Ophthalmology
- Spectral sensitivity
- Blink
- Ora serrata
- Hyaloid canal
References
- ^ Judd, Deane B. (1975). Color in Business, Science and Industry. Wiley Series in Pure and Applied Optics (third edition ed.). New York: Wiley-Interscience. p. 388. ISBN 0-471-45212-2.
{{cite book}}:|edition=has extra text (help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Zimmer, Carl (2012). "Our Strange, Important, Subconscious Light Detectors". Discover Magazine. Retrieved 2012-05-05.
{{cite web}}: Unknown parameter|month=ignored (help) - ^ "eye, human."Encyclopædia Britannica from Encyclopædia Britannica 2006 Ultimate Reference Suite DVD 2009
- ^ Barton, H. and Byrne, K. Introduction to Human Vision, Visual Defects & Eye Tests (March 2007), p. 22. PDF
- ^ MIL-STD-1472F, Military Standard, Human Engineering, Design Criteria For Military Systems, Equipment, And Facilities (23 Aug 1999) PDF
- ^ Mendell MJ. Non-specific symptoms in office workers: a review and summary of the epidemiologic literature. Indoor Air 1993; 3: 227-36.
- ^ a b c d e Wolkoff, P., Skov, P., Franck, C., and Petersen, LN. “Eye irritation and environmental factors in the office environment-hypotheses, causes and a physiological model” Scandinavian Journal of Work, Environment & Health [Scand. J. Work Environ. Health]. Dec 2003, pp. 411–430. Vol. 29, No. 6.
- ^ Mendell MJ. Non-specific symptoms in office workers: a review and summary of the epidemiologic literature. Indoor Air 1993; 3: 227-36
- ^ a b Norn MS. Pollution keratoconjunctivitis. Acta Ophthalmol Scand 1992; 70: 269-73.
- ^ "Eye discomfort and air pollution". Ophthalmologica. 213 (2): 103–9. 1999. PMID 9885386.
{{cite journal}}: Unknown parameter|authors=ignored (help) - ^ Lemp MA. New strategies in the treatment of dry-eye states. Cornea 1999; 18: 625-32.
- ^ Rolando M, Zierhurt M. The ocular surface and tear film and their dysfuction in dry eye disease. Surv Ophthalmol 2001; 45: S203-S210
- ^ Murata K, Araki S, Kawakami N, Saito Y, Hino E. Central nervous system effects and visual fatigue in VDT workers. Int Arch Occup Health 1991; 63: 109-13
- ^ Rossignol AM, Morse EP, Summers VM, Pagnotto LD. Video display terminal use and reported health symptoms among Massachusetts clerical workers. J Occup Med 1987; 29: 112-8
- ^ Apter A, Bracker A, Hodgson M, Sidman J, Leung W-Y. Epidemiology of the sick building syndrome. J Allergy Clin Immunol 1994; 94: 277-88.
- ^ Thomas WD. Eye problems and visual display terminals- the facts and the fallacies. Opthalmic Physiol Opt 2001; 18: 111-9
- ^ Aronsson G, Stromberg A. Work content and eye discomfort in VDT work. Int J Occup Saf Ergon 1995; 1: 1-13
- ^ Mocci F, Serra A, Corrias GA. Psychological factors and visual fatigue in working with video display terminals. Occup Environ Med 2001; 58: 267-71
- ^ Kjaergaard, SK. Chapter 17. The irritated eye in the indoor environment, Indoor Air Quality Handbook
- ^ Wolkoff, P., Skov, P., Franck, C., and Petersen, LN. “Eye irritation and environmental factors in the office environment-hypotheses, causes and a physiological model” Scandinavian Journal of Work, Environment & Health. Dec 2003, pp. 411-430, Vol. 29, No.6
- ^ Norn Ms. External eye: methods of examination. Copenhagen: Scriptor; 1983
- ^ Sibony PA, Evinger C. Anatomy and physiology of normal and abnormal eyelid position and movement. In: Miller NR, Newman NJ, editors. Walsh & Hoyt’s clinical neuro-ophthalmology. Baltimore (MD): Williams and Wilkins; 1998. P 1509- 92
- ^ Franck C, Back E, Skov P. Prevalence of objective eye manifestations in people working in office buildings with different prevalence of the sick building syndrome compared with the general population. Int Arch Occup Health 1993; 65: 65- 9
- ^ Franck C. Fatty layer of the precorneal film in the ‘office eye syndrome’. Acta Ophthalmol Scand 1991; 69: 737- 43
- ^ Franck C, Skov P. Foam at inner eye canthus in office workers, compared with an average Danish population as control group. Acta Ophthalmol Scand 1989; 67: 61- 8
- ^ Franck C. Eye symptoms and signs in buildings with indoor climate problems (‘Office Eye Syndroms’). Acta Ophthalmol Scand 1986; 64: 306- 11
- ^ Doughty MJ, Fonn D, Richter D, Simpson T, Caffery B, Gordon K. A patient questionnaire approach to estimating the prevalence of dry eye symptoms in patients presenting to optometric practices across Canada. Optom Vis Sci 1997; 74: 424- 31.
- ^ Fonn D, Situ P, Simpsom T. Hydrogel lens dehydration and subjective comfort and dryness Ratings in symptomatic and asymptomatic contact lens wearers. Optom Vis Sci 1999; 76: 700- 4
- ^ a b Vajdic C, Holden BA, Sweeney DF, Cornish RM. The frequency of ocular symptoms during spectacle and daily soft and rigid contact lens wear. Optom Vis Sci 1999; 76: 705- 11
- ^ Seal, D. V., and I. A. Mackie. 1986. The questionable dry eye as a clinical and biochemical entity. In F. J. Holly (Ed.), the preocular tear film – In health, disease, and contact lens wear. Dry Eye Institute, Lubbock, Texas, 41- 51
- ^ Hikichi, T., A. Yoshida, Y. Fukui, T. Hamano, M. Ri, K. Araki, K. Horimoto, E. Takamura, K. Kitagawa, M. Oyama, Y. Danjo, S. Kondo, H. Fujishima, I. Toda, and K. Tsubota. 1995. Prevalence of dry eye in Japanese eye centers. Graefe’s Arch. Clin. Exp. Ophthalmol. 233: 555- 558.
- ^ McCarty, C. A., A. K. Bansal, P. M. Livingston, Y. L. Stanislovsky, and H. R. Taylor. 1998. The Epidemiology of Dry Eye in Melbourne, Australia. Ophthalmology 105: 1114- 1119
- ^ Bentivoglio AR, Bressman SB, Cassetta E. Caretta D, Tonali P, Albanese A. Analysis of blink rate patterns in normal subjects. Mov Disord 1997; 1028- 34
- ^ McCarty CA, Bansal AK, Livingston PM, Stanislavsky YL, Taylor HR. The epidemiology of dry eye in Melbourne, Australia. Ophthalmology 1998; 105: 1114- 9
- ^ Mathers WD, Lane JA, Zimmerman MB. Tear film changes associated with normal aging. Cornea 1996; 15: 229- 34
- ^ Mathers WD, Stovall D, Lane JA, Zimmerman MB, Johnson S. Menopause and tear function: the influence of prolactin and sex hormones on human tear production. Cornea 1998; 17: 353- 8
- ^ Wallingford K.M and Carpenter, J Proc. IAQ '86: Managing Indoor Air for Health and Energy Conserv., American Society for Heating, Refrigerating, and Air-Conditioning Engineers, Atlanta, 448, 1986.
- ^ Jaakkola, Maritta S. and Jouni J. K. Jaakkola. "Office Equipment and Supplies: A Modern Occupational Health Concern?", American Journal of Epidemiology, 1999, pp. 1223, Vol. 150, No. 11
- ^ Nordström K., D. Norbäck, and R. Akselsson. “Influence of indoor air quality and personal factors on the sick building syndrome (SBS) in Swedish geriatric hospitals.”, Occupational and Environmental Medicine, 1995, pp. 170–176, Vol. 52.
- ^ Anderson, Crosalind C. and Julius H. Anderson. “Sensory irritation and multiple chemical sensitivity.” Toxicology and Industrial Health, 1999, pp. 339–345, Vol. 15, No. 3-4
- ^ a b c d X Hu, D H Wegman, E A Eisen, S R Woskie and R G Smith. “Dose related acute irritant symptom responses to occupational exposure to sodium borate dusts.” British Journal of Industrial Medicine 1992, pp. 706–713, Vol. 49.
- ^ Carney LG, Hill RM. The nature of normal blinking patterns. Acta Ophthalmol Scand 1982; 60: 427- 33
- ^ Henning RA, Jacques P, Kissel GV, Sullivan AB, Alteras-Webb SM. Frequent short rest breaks from computer work: effects on productivity and well-being at two field sites. Ergonomics 1997; 40: 78- 91
- ^ Nakamori K, Odawara M, Nakajima K, Mizutani T, Tsubota K. Blinking is controlled primarily by ocular surface conditions. Am Ophthalmol 1997; 124: 24-30.
- ^ Barbato G, Ficca G, Muscettola G, Fichele M, Beatrice M, Rinaldi F. Diurnal variation in spontaneous eye-blink rate. Psychiatry Res 2000; 93: 145-51.
- ^ Sotoyama M, Villanuveva MBG, Jonai H, Saito S. Ocular surface area as an informative index of visual ergonomics. Ind Health 1995; 33: 43- 56
- ^ Sotoyama M, Jonai H, Saito S, Villanuveva MBG. Analysis of ocular surface area for comfortable VDT workstation layout. Ergonomics 1996; 39: 877- 84
- ^ Collins M, Heron H, Larsen R, Lindner R. Blinking patterns in soft contact lens wearers can be altered with training. Am J Optometry Physiolog Opt 1987; 64: 100-3
- ^ Piccoli B, Assini R, Gambaro S, Pastoni F, D’Orso M, Franceshini S, et al. Microbiological pollution and ocular infection in CAS operators: an on-site investigation. Ergonomics 2001; 44: 658- 67
- ^ Lozato PA, Pisella PJ, Baudoin C. The lipid layer of the lacrimal tear film: physiology and pathology. J Fr Ophthalmol 2001; 24: 643- 58
- ^ Westheimer, Gerald & McKee, Suzanne P.; "Visual acuity in the presence of retinal-image motion". Journal of the Optical Society of America 1975 65(7), 847–50.
- ^ Roger H.S. Carpenter (1988); Movements of the eyes (2nd ed.). Pion Ltd, London. ISBN 0-85086-109-8.
- ^ Saladin, Kenneth S. Anatomy and Phyisology: The Unity of Form and Function. 5th ed. New York: McGraw-Hill, 2010. 620–22.
- ^ Saladin, Kenneth S. Anatomy and Phyisology: The Unity of Form and Function. 5th ed. New York: McGraw-Hill, 2010. 620–22.
- ^ "human eye." Encyclopædia Britannica. 2010. Encyclopædia Britannica Online. 05 Dec. 2010 <http://www.britannica.com/EBchecked/topic/1688997/human-eye>.
- ^ AgingEye Times
External links
![]() Media related to human eyes at Wikimedia Commons
Media related to human eyes at Wikimedia Commons