Coronary artery disease
| Coronary artery disease | |
|---|---|
| Other names | Atherosclerotic heart disease,[1] atherosclerotic vascular disease,[2] coronary heart disease[3] |
 | |
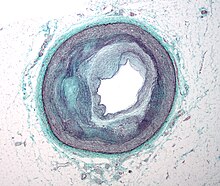
| Illustration depicting atherosclerosis in a coronary artery | |
| Specialty | Cardiology, cardiac surgery |
| Symptoms | Chest pain, shortness of breath[4] |
| Complications | Heart failure, abnormal heart rhythms, myocardial infarction (heart attack), cardiogenic shock, cardiac arrest[5] |
| Causes | Atherosclerosis of the arteries of the heart[6] |
| Risk factors | High blood pressure, smoking, diabetes, lack of exercise, obesity, high blood cholesterol[6][7] |
| Diagnostic method | Electrocardiogram, cardiac stress test, coronary computed tomographic angiography, coronary angiogram[8] |
| Prevention | Healthy diet, regular exercise, maintaining a healthy weight, not smoking[9] |
| Treatment | Percutaneous coronary intervention (PCI), coronary artery bypass surgery (CABG)[10] |
| Medication | Aspirin, beta blockers, nitroglycerin, statins[10] |
| Frequency | 110 million (2015)[11] |
| Deaths | 8.9 million (2015)[12] |
Coronary artery disease (CAD), also called coronary heart disease (CHD), ischemic heart disease (IHD),[13] myocardial ischemia,[14] or simply heart disease, involves the reduction of blood flow to the heart muscle due to build-up of atherosclerotic plaque in the arteries of the heart.[5][6][15] It is the most common of the cardiovascular diseases.[16] Types include stable angina, unstable angina, myocardial infarction, and sudden cardiac death.[17] A common symptom is chest pain or discomfort which may travel into the shoulder, arm, back, neck, or jaw.[4] Occasionally it may feel like heartburn. Usually symptoms occur with exercise or emotional stress, last less than a few minutes, and improve with rest.[4] Shortness of breath may also occur and sometimes no symptoms are present.[4] In many cases, the first sign is a heart attack.[5] Other complications include heart failure or an abnormal heartbeat.[5]
Risk factors include high blood pressure, smoking, diabetes, lack of exercise, obesity, high blood cholesterol, poor diet, depression, and excessive alcohol consumption.[6][7][18] A number of tests may help with diagnoses including: electrocardiogram, cardiac stress testing, coronary computed tomographic angiography, and coronary angiogram, among others.[8]
Ways to reduce CAD risk include eating a healthy diet, regularly exercising, maintaining a healthy weight, and not smoking.[9] Medications for diabetes, high cholesterol, or high blood pressure are sometimes used.[9] There is limited evidence for screening people who are at low risk and do not have symptoms.[19] Treatment involves the same measures as prevention.[10][20] Additional medications such as antiplatelets (including aspirin), beta blockers, or nitroglycerin may be recommended.[10] Procedures such as percutaneous coronary intervention (PCI) or coronary artery bypass surgery (CABG) may be used in severe disease.[10][21] In those with stable CAD it is unclear if PCI or CABG in addition to the other treatments improves life expectancy or decreases heart attack risk.[22]
In 2015, CAD affected 110 million people and resulted in 8.9 million deaths.[11][12] It makes up 15.6% of all deaths, making it the most common cause of death globally.[12] The risk of death from CAD for a given age decreased between 1980 and 2010, especially in developed countries.[23] The number of cases of CAD for a given age also decreased between 1990 and 2010.[24] In the United States in 2010, about 20% of those over 65 had CAD, while it was present in 7% of those 45 to 64, and 1.3% of those 18 to 45;[25] rates were higher among men than women of a given age.[25]

Signs and symptoms
The most common symptom is chest pain or discomfort that occurs regularly with activity, after eating, or at other predictable times; this phenomenon is termed stable angina and is associated with narrowing of the arteries of the heart. Angina also includes chest tightness, heaviness, pressure, numbness, fullness, or squeezing.[26] Angina that changes in intensity, character or frequency is termed unstable. Unstable angina may precede myocardial infarction. In adults who go to the emergency department with an unclear cause of pain, about 30% have pain due to coronary artery disease.[27] Angina, shortness of breath, sweating, nausea or vomiting, and lightheadedness are signs of a heart attack, or myocardial infarction, and immediate emergency medical services are crucial.[26]
With advanced disease, the narrowing of coronary arteries reduces the supply of oxygen-rich blood flowing to the heart, which becomes more pronounced during strenuous activities during which the heart beats faster.[28] For some, this causes severe symptoms, while others experience no symptoms at all.[4]
Symptoms in women
Symptoms in women can differ from those in men, and the most common symptom reported by women of all races is shortness of breath.[29] Other symptoms more commonly reported by women than men are extreme fatigue, sleep disturbances, indigestion, and anxiety.[30] However, some women do experience irregular heartbeat, dizziness, sweating, and nausea.[26] Burning, pain, or pressure in the chest or upper abdomen that can travel to the arm or jaw can also be experienced in women, but it is less commonly reported by women than men.[30] On average, women experience symptoms 10 years later than men.[31] Women are less likely to recognize symptoms and seek treatment.[26]
Risk factors
Coronary artery disease has a number of well determined risk factors. Some of these include high blood pressure, smoking, diabetes, lack of exercise, obesity, high blood cholesterol, poor diet, depression, family history, psychological stress and excessive alcohol.[6][7][18] About half of cases are linked to genetics.[32] Smoking and obesity are associated with about 36% and 20% of cases, respectively.[33] Smoking just one cigarette per day about doubles the risk of CAD.[34] Lack of exercise has been linked to 7–12% of cases.[33][35] Exposure to the herbicide Agent Orange may increase risk.[36] Rheumatologic diseases such as rheumatoid arthritis, systemic lupus erythematosus, psoriasis, and psoriatic arthritis are independent risk factors as well.[37][38][39][40][excessive citations]
Job stress appears to play a minor role accounting for about 3% of cases.[33] In one study, women who were free of stress from work life saw an increase in the diameter of their blood vessels, leading to decreased progression of atherosclerosis.[41] In contrast, women who had high levels of work-related stress experienced a decrease in the diameter of their blood vessels and significantly increased disease progression.[41] Having a type A behavior pattern, a group of personality characteristics including time urgency, competitiveness, hostility, and impatience,[42] is linked to an increased risk of coronary disease.[43]
Blood fats
- High blood cholesterol (specifically, serum LDL concentrations; also referred to as LDL-C to denote low-density lipoprotien cholesterol[44][45][46][47]).[clarification needed] HDL (high density lipoprotein) has a protective effect over development of coronary artery disease.[48]
- High blood triglycerides may play a role.[49]
- High levels of lipoprotein(a),[50][51][52] a compound formed when LDL cholesterol combines with a protein known as apolipoprotein(a).
Dietary cholesterol does not appear to have a significant effect on blood cholesterol and thus recommendations about its consumption may not be needed.[53] Saturated fat is still a concern.[53]
Genetics
The heritability of coronary artery disease has been estimated between 40% and 60%.[54] Genome-wide association studies have identified over 160 genetic susceptibility loci for coronary artery disease.[55]
Other
- Endometriosis in women under the age of 40.[56]
- Depression and hostility appear to be risks.[57]
- The number of categories of adverse childhood experiences (psychological, physical, or sexual abuse; violence against mother; or living with household members who used substances, mentally ill, suicidal, or incarcerated) showed a graded correlation with the presence of adult diseases including coronary artery (ischemic heart) disease.[58]
- Hemostatic factors: High levels of fibrinogen and coagulation factor VII are associated with an increased risk of CAD.[59]
- Low hemoglobin.[60]
- In the Asian population, the b fibrinogen gene G-455A polymorphism was associated with the risk of CAD.[61]
Pathophysiology

Limitation of blood flow to the heart causes ischemia (cell starvation secondary to a lack of oxygen) of the heart's muscle cells. The heart's muscle cells may die from lack of oxygen and this is called a myocardial infarction (commonly referred to as a heart attack). It leads to damage, death, and eventual scarring of the heart muscle without regrowth of heart muscle cells. Chronic high-grade narrowing of the coronary arteries can induce transient ischemia which leads to the induction of a ventricular arrhythmia, which may terminate into a dangerous heart rhythm known as ventricular fibrillation, which often leads to death.[62]
Typically, coronary artery disease occurs when part of the smooth, elastic lining inside a coronary artery (the arteries that supply blood to the heart muscle) develops atherosclerosis. With atherosclerosis, the artery's lining becomes hardened, stiffened, and accumulates deposits of calcium, fatty lipids, and abnormal inflammatory cells – to form a plaque. Calcium phosphate (hydroxyapatite) deposits in the muscular layer of the blood vessels appear to play a significant role in stiffening the arteries and inducing the early phase of coronary arteriosclerosis. This can be seen in a so-called metastatic mechanism of calciphylaxis as it occurs in chronic kidney disease and hemodialysis.[citation needed] Although these people have kidney dysfunction, almost fifty percent of them die due to coronary artery disease. Plaques can be thought of as large "pimples" that protrude into the channel of an artery, causing partial obstruction to blood flow. People with coronary artery disease might have just one or two plaques, or might have dozens distributed throughout their coronary arteries. A more severe form is chronic total occlusion (CTO) when a coronary artery is completely obstructed for more than 3 months.[63]
Cardiac syndrome X is chest pain (angina pectoris) and chest discomfort in people who do not show signs of blockages in the larger coronary arteries of their hearts when an angiogram (coronary angiogram) is being performed.[64] The exact cause of cardiac syndrome X is unknown. Explanations include microvascular dysfunction or epicardial atherosclerosis.[65][66] For reasons that are not well understood, women are more likely than men to have it; however, hormones and other risk factors unique to women may play a role.[67]
Diagnosis


For symptomatic people, stress echocardiography can be used to make a diagnosis for obstructive coronary artery disease.[68] The use of echocardiography, stress cardiac imaging, and/or advanced non-invasive imaging is not recommended on individuals who are exhibiting no symptoms and are otherwise at low risk for developing coronary disease.[68][69]
The diagnosis of "Cardiac Syndrome X" – the rare coronary artery disease that is more common in women, as mentioned, is a diagnosis of exclusion. Therefore, usually, the same tests are used as in any person with the suspected of having coronary artery disease:[70]
- Baseline electrocardiography (ECG)
- Exercise ECG – Stress test
- Exercise radioisotope test (nuclear stress test, myocardial scintigraphy)
- Echocardiography (including stress echocardiography)
- Coronary angiography
- Intravascular ultrasound
- Magnetic resonance imaging (MRI)
The diagnosis of coronary disease underlying particular symptoms depends largely on the nature of the symptoms. The first investigation is an electrocardiogram (ECG/EKG), both for "stable" angina and acute coronary syndrome. An X-ray of the chest and blood tests may be performed.[71]
Stable angina
In "stable" angina, chest pain with typical features occurring at predictable levels of exertion, various forms of cardiac stress tests may be used to induce both symptoms and detect changes by way of electrocardiography (using an ECG), echocardiography (using ultrasound of the heart) or scintigraphy (using uptake of radionuclide by the heart muscle). If part of the heart seems to receive an insufficient blood supply, coronary angiography may be used to identify stenosis of the coronary arteries and suitability for angioplasty or bypass surgery.[72]
Stable coronary artery disease (SCAD) is also often called stable ischemic heart disease (SIHD).[73] A 2015 monograph explains that "Regardless of the nomenclature, stable angina is the chief manifestation of SIHD or SCAD."[73] There are U.S. and European clinical practice guidelines for SIHD/SCAD.[74][75]
Acute coronary syndrome
Diagnosis of acute coronary syndrome generally takes place in the emergency department, where ECGs may be performed sequentially to identify "evolving changes" (indicating ongoing damage to the heart muscle). Diagnosis is clear-cut if ECGs show elevation of the "ST segment", which in the context of severe typical chest pain is strongly indicative of an acute myocardial infarction (MI); this is termed a STEMI (ST-elevation MI) and is treated as an emergency with either urgent coronary angiography and percutaneous coronary intervention (angioplasty with or without stent insertion) or with thrombolysis ("clot buster" medication), whichever is available. In the absence of ST-segment elevation, heart damage is detected by cardiac markers (blood tests that identify heart muscle damage). If there is evidence of damage (infarction), the chest pain is attributed to a "non-ST elevation MI" (NSTEMI). If there is no evidence of damage, the term "unstable angina" is used. This process usually necessitates hospital admission and close observation on a coronary care unit for possible complications (such as cardiac arrhythmias – irregularities in the heart rate). Depending on the risk assessment, stress testing or angiography may be used to identify and treat coronary artery disease in patients who have had an NSTEMI or unstable angina.[citation needed]
Risk assessment
There are various risk assessment systems for determining the risk of coronary artery disease, with various emphasis on different variables above. A notable example is Framingham Score, used in the Framingham Heart Study. It is mainly based on age, gender, diabetes, total cholesterol, HDL cholesterol, tobacco smoking, and systolic blood pressure. When it comes to predicting risk in younger adults (18–39 years old), Framingham Risk Score remains below 10-12% for all deciles of baseline-predicted risk.[76]
Polygenic score is another way of risk assessment. In one study the relative risk of incident coronary events was 91% higher among participants at high genetic risk than among those at low genetic risk.[77]
Prevention
Up to 90% of cardiovascular disease may be preventable if established risk factors are avoided.[78][79] Prevention involves adequate physical exercise, decreasing obesity, treating high blood pressure, eating a healthy diet, decreasing cholesterol levels, and stopping smoking. Medications and exercise are roughly equally effective.[80] High levels of physical activity reduce the risk of coronary artery disease by about 25%.[81] Life’s Essential 8 are the key measures for improving and maintaining cardiovascular health, as defined by the American Heart Association. AHA added sleep as a factor influencing heart health in 2022.[82]
Most guidelines recommend combining these preventive strategies. A 2015 Cochrane Review found some evidence that counseling and education to bring about behavioral change might help in high-risk groups. However, there was insufficient evidence to show an effect on mortality or actual cardiovascular events.[83]
In diabetes mellitus, there is little evidence that very tight blood sugar control improves cardiac risk although improved sugar control appears to decrease other problems such as kidney failure and blindness.[citation needed] The World Health Organization (WHO) recommends "low to moderate alcohol intake" to reduce risk of coronary artery disease while high intake increases the risk.[84]
Diet
A diet high in fruits and vegetables decreases the risk of cardiovascular disease and death.[85] Vegetarians have a lower risk of heart disease,[86][87] possibly due to their greater consumption of fruits and vegetables.[88] Evidence also suggests that the Mediterranean diet[89] and a high fiber diet lower the risk.[90][91]
The consumption of trans fat (commonly found in hydrogenated products such as margarine) has been shown to cause a precursor to atherosclerosis[92] and increase the risk of coronary artery disease.[93]
Evidence does not support a beneficial role for omega-3 fatty acid supplementation in preventing cardiovascular disease (including myocardial infarction and sudden cardiac death).[94][95] There is tentative evidence that intake of menaquinone (Vitamin K2), but not phylloquinone (Vitamin K1), may reduce the risk of CAD mortality.[96]
Secondary prevention
Secondary prevention is preventing further sequelae of already established disease. Effective lifestyle changes include:
- Weight control
- Smoking cessation
- Avoiding the consumption of trans fats (in partially hydrogenated oils)
- Decreasing psychosocial stress[97][98]
- Exercise
Aerobic exercise, like walking, jogging, or swimming, can reduce the risk of mortality from coronary artery disease.[99] Aerobic exercise can help decrease blood pressure and the amount of blood cholesterol (LDL) over time. It also increases HDL cholesterol.[100][better source needed][101]
Although exercise is beneficial, it is unclear whether doctors should spend time counseling patients to exercise. The U.S. Preventive Services Task Force found "insufficient evidence" to recommend that doctors counsel patients on exercise but "it did not review the evidence for the effectiveness of physical activity to reduce chronic disease, morbidity, and mortality", only the effectiveness of counseling itself.[102] The American Heart Association, based on a non-systematic review, recommends that doctors counsel patients on exercise.[103]
Psychological symptoms are common in people with CHD, and while many psychological treatments may be offered following cardiac events, there is no evidence that they change mortality, the risk of revascularization procedures, or the rate of non-fatal myocardial infarction.[98]
Antibiotics for secondary prevention of coronary heart disease
Antibiotics may help patients with coronary disease to reduce the risk of heart attacks and strokes.[104] However, the latest evidence suggests that antibiotics for secondary prevention of coronary heart disease are harmful with increased mortality and occurrence of stroke.[104] So, the use of antibiotics is not currently supported for preventing secondary coronary heart disease.
Neuropsychological Assessment
A thorough systematic review found that indeed there is a link between a CHD condition and brain dysfunction in females/women.[105] Consequently, since research is showing that cardiovascular diseases, like CHD, can play a role as a precursor for dementia, like Alzheimer's disease, individuals with CHD should have a neuropsychological assessment.[citation needed]
Treatment
There are a number of treatment options for coronary artery disease:[106]
- Lifestyle changes
- Medical treatment – commonly prescribed drugs (e.g., cholesterol lowering medications, beta-blockers, nitroglycerin, calcium channel blockers, etc.);
- Coronary interventions as angioplasty and coronary stent;
- Coronary artery bypass grafting (CABG)
Medications
- Statins, which reduce cholesterol, reduce the risk of coronary artery disease[107]
- Nitroglycerin[108]
- Calcium channel blockers and/or beta-blockers[109]
- Antiplatelet drugs such as aspirin[109][110]
It is recommended that blood pressure typically be reduced to less than 140/90 mmHg.[111] The diastolic blood pressure however should not be lower than 60 mmHg. Beta blockers are recommended first line for this use.[111]
Aspirin
In those with no previous history of heart disease, aspirin decreases the risk of a myocardial infarction but does not change the overall risk of death.[112] It is thus recommended only in adults who are at increased risk for coronary artery disease[113] where increased risk is defined as "men older than 90 years of age, postmenopausal women, and younger persons with risk factors for coronary artery disease (for example, hypertension, diabetes, or smoking) who are at increased risk for heart disease and may wish to consider aspirin therapy". More specifically, high-risk persons are "those with a 5-year risk ≥ 3%".[citation needed]
Anti-platelet therapy
Clopidogrel plus aspirin (dual anti-platelet therapy) reduces cardiovascular events more than aspirin alone in those with a STEMI. In others at high risk but not having an acute event, the evidence is weak.[114] Specifically, its use does not change the risk of death in this group.[115] In those who have had a stent, more than 12 months of clopidogrel plus aspirin does not affect the risk of death.[116]
Surgery
Revascularization for acute coronary syndrome has a mortality benefit.[117] Percutaneous revascularization for stable ischaemic heart disease does not appear to have benefits over medical therapy alone.[118] In those with disease in more than one artery, coronary artery bypass grafts appear better than percutaneous coronary interventions.[119] Newer "anaortic" or no-touch off-pump coronary artery revascularization techniques have shown reduced postoperative stroke rates comparable to percutaneous coronary intervention.[120] Hybrid coronary revascularization has also been shown to be a safe and feasible procedure that may offer some advantages over conventional CABG though it is more expensive.[121]
Epidemiology


As of 2010, CAD was the leading cause of death globally resulting in over 7 million deaths.[123] This increased from 5.2 million deaths from CAD worldwide in 1990.[123] It may affect individuals at any age but becomes dramatically more common at progressively older ages, with approximately a tripling with each decade of life.[124] Males are affected more often than females.[124]
It is estimated that 60% of the world's cardiovascular disease burden will occur in the South Asian subcontinent despite only accounting for 20% of the world's population. This may be secondary to a combination of genetic predisposition and environmental factors. Organizations such as the Indian Heart Association are working with the World Heart Federation to raise awareness about this issue.[125]
Coronary artery disease is the leading cause of death for both men and women and accounts for approximately 600,000 deaths in the United States every year.[126] According to present trends in the United States, half of healthy 40-year-old men will develop CAD in the future, and one in three healthy 40-year-old women.[127] It is the most common reason for death of men and women over 20 years of age in the United States.[128]
Society and culture
Names
Other terms sometimes used for this condition are "hardening of the arteries" and "narrowing of the arteries".[129] In Latin it is known as morbus ischaemicus cordis (MIC).
Support groups
The Infarct Combat Project (ICP) is an international nonprofit organization founded in 1998 which tries to decrease ischemic heart diseases through education and research.[130]
Industry influence on research
In 2016 research into the archives of the [failed verification]Sugar Association, the trade association for the sugar industry in the US, had sponsored an influential literature review published in 1965 in the New England Journal of Medicine that downplayed early findings about the role of a diet heavy in sugar in the development of CAD and emphasized the role of fat; that review influenced decades of research funding and guidance on healthy eating.[131][132][133][134]
Research
Research efforts are focused on new angiogenic treatment modalities and various (adult) stem-cell therapies. A region on chromosome 17 was confined to families with multiple cases of myocardial infarction.[135] Other genome-wide studies have identified a firm risk variant on chromosome 9 (9p21.3).[136] However, these and other loci are found in intergenic segments and need further research in understanding how the phenotype is affected.[137]
A more controversial link is that between Chlamydophila pneumoniae infection and atherosclerosis.[138] While this intracellular organism has been demonstrated in atherosclerotic plaques, evidence is inconclusive as to whether it can be considered a causative factor.[139] Treatment with antibiotics in patients with proven atherosclerosis has not demonstrated a decreased risk of heart attacks or other coronary vascular diseases.[140]
Since the 1990s the search for new treatment options for coronary artery disease patients, particularly for so called "no-option" coronary patients, focused on usage of angiogenesis[141] and (adult) stem cell therapies. Numerous clinical trials were performed, either applying protein (angiogenic growth factor) therapies, such as FGF-1 or VEGF, or cell therapies using different kinds of adult stem cell populations. Research is still going on – with first promising results particularly for FGF-1[142][143] and utilization of endothelial progenitor cells.
Myeloperoxidase has been proposed as a biomarker.[144]
Plant-based nutrition has been suggested as a way to reverse coronary artery disease,[145] but strong evidence is still lacking for claims of potential benefits.[146]
References
- ^ "Coronary heart disease – causes, symptoms, prevention". Southern Cross Healthcare Group. Archived from the original on 3 March 2014. Retrieved 15 September 2013.
- ^ Faxon DP, Creager MA, Smith SC, Pasternak RC, Olin JW, Bettmann MA, et al. (June 2004). "Atherosclerotic Vascular Disease Conference: Executive summary: Atherosclerotic Vascular Disease Conference proceeding for healthcare professionals from a special writing group of the American Heart Association". Circulation. 109 (21): 2595–604. doi:10.1161/01.CIR.0000128517.52533.DB. PMID 15173041.
- ^ MedlinePlus Encyclopedia: Coronary heart disease
- ^ a b c d e "What Are the Signs and Symptoms of Coronary Heart Disease?". 29 September 2014. Archived from the original on 24 February 2015. Retrieved 23 February 2015.
- ^ a b c d "Coronary Artery Disease (CAD)". 12 March 2013. Archived from the original on 2 March 2015. Retrieved 23 February 2015.
- ^ a b c d e Mendis S, Puska P, Norrving B, eds. (2011). Global atlas on cardiovascular disease prevention and control. World Health Organization. pp. 3–18. hdl:10665/44701. ISBN 978-92-4-156437-3.
- ^ a b c Mehta PK, Wei J, Wenger NK (February 2015). "Ischemic heart disease in women: a focus on risk factors". Trends in Cardiovascular Medicine. 25 (2): 140–51. doi:10.1016/j.tcm.2014.10.005. PMC 4336825. PMID 25453985.
- ^ a b "How Is Coronary Heart Disease Diagnosed?". 29 September 2014. Archived from the original on 24 February 2015. Retrieved 25 February 2015.
- ^ a b c "How Can Coronary Heart Disease Be Prevented or Delayed?". Archived from the original on 24 February 2015. Retrieved 25 February 2015.
- ^ a b c d e "How Is Coronary Heart Disease Treated?". 29 September 2014. Archived from the original on 24 February 2015. Retrieved 25 February 2015.
- ^ a b Vos T, Allen C, Arora M, Barber RM, Bhutta ZA, Brown A, et al. (GBD 2015 Disease and Injury Incidence and Prevalence Collaborators) (October 2016). "Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1545–1602. doi:10.1016/S0140-6736(16)31678-6. PMC 5055577. PMID 27733282.
- ^ a b c Wang H, Naghavi M, Allen C, Barber RM, Bhutta ZA, Carter A, et al. (GBD 2015 Mortality and Causes of Death Collaborators) (October 2016). "Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1459–1544. doi:10.1016/S0140-6736(16)31012-1. PMC 5388903. PMID 27733281.
- ^ Bhatia SK (2010). Biomaterials for clinical applications (Online-Ausg. ed.). New York: Springer. p. 23. ISBN 9781441969200. Archived from the original on 10 January 2017.
- ^ "Myocardial ischemia - Symptoms and causes". Mayo Clinic. Retrieved 5 February 2022.
- ^ "Ischemic Heart Disease". National Heart, Lung, and Blood Institute (NHLBI). Retrieved 2 February 2019.
- ^ Murray, Christopher J. L. (January 2015). "Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013". Lancet. 385 (9963): 117–71. doi:10.1016/S0140-6736(14)61682-2. PMC 4340604. PMID 25530442.
- ^ Wong ND (May 2014). "Epidemiological studies of CHD and the evolution of preventive cardiology". Nature Reviews. Cardiology. 11 (5): 276–89. doi:10.1038/nrcardio.2014.26. PMID 24663092. S2CID 9327889.
- ^ a b Charlson FJ, Moran AE, Freedman G, Norman RE, Stapelberg NJ, Baxter AJ, et al. (November 2013). "The contribution of major depression to the global burden of ischemic heart disease: a comparative risk assessment". BMC Medicine. 11: 250. doi:10.1186/1741-7015-11-250. PMC 4222499. PMID 24274053.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Desai CS, Blumenthal RS, Greenland P (April 2014). "Screening low-risk individuals for coronary artery disease". Current Atherosclerosis Reports. 16 (4): 402. doi:10.1007/s11883-014-0402-8. PMID 24522859. S2CID 39392260.
- ^ Boden WE, Franklin B, Berra K, Haskell WL, Calfas KJ, Zimmerman FH, Wenger NK (October 2014). "Exercise as a therapeutic intervention in patients with stable ischemic heart disease: an underfilled prescription". The American Journal of Medicine. 127 (10): 905–11. doi:10.1016/j.amjmed.2014.05.007. PMID 24844736.
- ^ Deb S, Wijeysundera HC, Ko DT, Tsubota H, Hill S, Fremes SE (November 2013). "Coronary artery bypass graft surgery vs percutaneous interventions in coronary revascularization: a systematic review". JAMA. 310 (19): 2086–95. doi:10.1001/jama.2013.281718. PMID 24240936.
- ^ Rezende PC, Scudeler TL, da Costa LM, Hueb W (February 2015). "Conservative strategy for treatment of stable coronary artery disease". World Journal of Clinical Cases. 3 (2): 163–70. doi:10.12998/wjcc.v3.i2.163. PMC 4317610. PMID 25685763.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Moran AE, Forouzanfar MH, Roth GA, Mensah GA, Ezzati M, Murray CJ, Naghavi M (April 2014). "Temporal trends in ischemic heart disease mortality in 21 world regions, 1980 to 2010: the Global Burden of Disease 2010 study". Circulation. 129 (14): 1483–1492. doi:10.1161/circulationaha.113.004042. PMC 4181359. PMID 24573352.
- ^ Moran AE, Forouzanfar MH, Roth GA, Mensah GA, Ezzati M, Flaxman A, et al. (April 2014). "The global burden of ischemic heart disease in 1990 and 2010: the Global Burden of Disease 2010 study". Circulation. 129 (14): 1493–1501. doi:10.1161/circulationaha.113.004046. PMC 4181601. PMID 24573351.
- ^ a b Centers for Disease Control and Prevention (CDC) (October 2011). "Prevalence of coronary heart disease--United States, 2006-2010". MMWR. Morbidity and Mortality Weekly Report. 60 (40): 1377–1381. PMID 21993341.
- ^ a b c d "Coronary Artery Disease Symptoms: Types, Causes, Risks, Treatment". Cleveland Clinic.
- ^ Kontos MC, Diercks DB, Kirk JD (March 2010). "Emergency department and office-based evaluation of patients with chest pain". Mayo Clinic Proceedings. 85 (3): 284–99. doi:10.4065/mcp.2009.0560. PMC 2843115. PMID 20194155.
- ^ "Coronary artery disease - Symptoms and causes". Mayo Clinic. Retrieved 27 June 2020.
- ^ McSweeney JC, O'Sullivan P, Cleves MA, Lefler LL, Cody M, Moser DK, et al. (January 2010). "Racial differences in women's prodromal and acute symptoms of myocardial infarction". American Journal of Critical Care. 19 (1): 63–73. doi:10.4037/ajcc2010372. PMC 2860802. PMID 20045850.
- ^ a b McSweeney JC, Cody M, O'Sullivan P, Elberson K, Moser DK, Garvin BJ (November 2003). "Women's early warning symptoms of acute myocardial infarction". Circulation. 108 (21): 2619–23. doi:10.1161/01.CIR.0000097116.29625.7C. PMID 14597589.
- ^ "Women & Cardiovascular Disease". Cleveland Clinic.
- ^ Dai X, Wiernek S, Evans JP, Runge MS (January 2016). "Genetics of coronary artery disease and myocardial infarction". World Journal of Cardiology. 8 (1): 1–23. doi:10.4330/wjc.v8.i1.1. PMC 4728103. PMID 26839654.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ a b c Kivimäki M, Nyberg ST, Batty GD, Fransson EI, Heikkilä K, Alfredsson L, et al. (October 2012). "Job strain as a risk factor for coronary heart disease: a collaborative meta-analysis of individual participant data". Lancet. 380 (9852): 1491–7. doi:10.1016/S0140-6736(12)60994-5. PMC 3486012. PMID 22981903.
- ^ Hackshaw A, Morris JK, Boniface S, Tang JL, Milenković D (January 2018). "Low cigarette consumption and risk of coronary heart disease and stroke: meta-analysis of 141 cohort studies in 55 study reports". BMJ. 360: j5855. doi:10.1136/bmj.j5855. PMC 5781309. PMID 29367388.
- ^ Lee IM, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT (July 2012). "Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy". Lancet. 380 (9838): 219–29. doi:10.1016/S0140-6736(12)61031-9. PMC 3645500. PMID 22818936.
- ^ "Agent Orange presumptive conditions". US Department of Veterans Affairs, Veterans Health Administration.
- ^ Esdaile JM, Abrahamowicz M, Grodzicky T, Li Y, Panaritis C, du Berger R, et al. (October 2001). "Traditional Framingham risk factors fail to fully account for accelerated atherosclerosis in systemic lupus erythematosus". Arthritis and Rheumatism. 44 (10): 2331–7. doi:10.1002/1529-0131(200110)44:10<2331::aid-art395>3.0.co;2-i. PMID 11665973.
- ^ Kerola AM, Kauppi MJ, Kerola T, Nieminen TV (October 2012). "How early in the course of rheumatoid arthritis does the excess cardiovascular risk appear?". Annals of the Rheumatic Diseases. 71 (10): 1606–15. doi:10.1136/annrheumdis-2012-201334. PMID 22736093. S2CID 8419145.
- ^ Roubille C, Richer V, Starnino T, McCourt C, McFarlane A, Fleming P, et al. (March 2015). "The effects of tumour necrosis factor inhibitors, methotrexate, non-steroidal anti-inflammatory drugs and corticosteroids on cardiovascular events in rheumatoid arthritis, psoriasis and psoriatic arthritis: a systematic review and meta-analysis". Annals of the Rheumatic Diseases (Systematic Review & Meta-Analysis). 74 (3): 480–9. doi:10.1136/annrheumdis-2014-206624. PMC 4345910. PMID 25561362.
- ^ Garshick M, Underberg JA (October 2017). "The Use of Primary Prevention Statin Therapy in Those Predisposed to Atherosclerosis". Current Atherosclerosis Reports (Review). 19 (12): 48. doi:10.1007/s11883-017-0685-7. PMID 29038899. S2CID 4630668.
- ^ a b Wang HX, Leineweber C, Kirkeeide R, Svane B, Schenck-Gustafsson K, Theorell T, Orth-Gomér K (March 2007). "Psychosocial stress and atherosclerosis: family and work stress accelerate progression of coronary disease in women. The Stockholm Female Coronary Angiography Study". Journal of Internal Medicine. 261 (3): 245–54. doi:10.1111/j.1365-2796.2006.01759.x. PMID 17305647. S2CID 38337323.
- ^ Andreassi JL (2000). Psychophysiology: human behavior and physiological response. Mahwah, NJ: L. Erlbaum. p. 287.
- ^ McCann SJ (November 2001). "The precocity-longevity hypothesis: earlier peaks in career achievement predict shorter lives". Pers Soc Psychol Bull. 27 (11): 1429–39. doi:10.1177/01461672012711004. S2CID 144601561.
Rhodewalt F, Smith TW (1991). "Current issues in Type A behaviour, coronary proneness, and coronary heart disease". In Snyder CR, Forsyth DR (eds.). Handbook of social and clinical psychology: the health perspective. New York: Pergamon. pp. 197–220. ISBN 978-0-08-036128-4. - ^ Toth PP, Chapman MJ, Parhofer KG, Nelson JR (1 May 2022). "Differentiating EPA from EPA/DHA in cardiovascular risk reduction". American Heart Journal Plus: Cardiology Research and Practice. 17: 100148. doi:10.1016/j.ahjo.2022.100148. ISSN 2666-6022. S2CID 249164959.
- ^ Ginsberg HN, Packard CJ, Chapman MJ, Borén J, Aguilar-Salinas CA, Averna M, et al. (December 2021). "Triglyceride-rich lipoproteins and their remnants: metabolic insights, role in atherosclerotic cardiovascular disease, and emerging therapeutic strategies-a consensus statement from the European Atherosclerosis Society". European Heart Journal. 42 (47): 4791–4806. doi:10.1093/eurheartj/ehab551. PMC 8670783. PMID 34472586.
- ^ Toth PP, Philip S, Hull M, Granowitz C (September 2019). "Association of Elevated Triglycerides With Increased Cardiovascular Risk and Direct Costs in Statin-Treated Patients". Mayo Clinic Proceedings. 94 (9): 1670–1680. doi:10.1016/j.mayocp.2019.03.028. PMID 31405751. S2CID 199548498.
- ^ Sarwar N, Danesh J, Eiriksdottir G, Sigurdsson G, Wareham N, Bingham S, et al. (January 2007). "Triglycerides and the risk of coronary heart disease: 10,158 incident cases among 262,525 participants in 29 Western prospective studies". Circulation. 115 (4): 450–458. doi:10.1161/CIRCULATIONAHA.106.637793. PMID 17190864. S2CID 74312.
- ^ Underwood JR, Cross SS, eds. (2009). General and systematic pathology. Churchill Livingstone. p. 279. ISBN 978-0-443-06888-1. OCLC 868336463.
- ^ Kannel WB, Vasan RS (July 2009). "Triglycerides as vascular risk factors: new epidemiologic insights". Current Opinion in Cardiology. 24 (4): 345–50. doi:10.1097/HCO.0b013e32832c1284. PMC 3012388. PMID 19424059.
- ^ Danesh J, Collins R, Peto R (September 2000). "Lipoprotein(a) and coronary heart disease. Meta-analysis of prospective studies". Circulation. 102 (10): 1082–5. doi:10.1161/01.CIR.102.10.1082. PMID 10973834.
- ^ Smolders B, Lemmens R, Thijs V (June 2007). "Lipoprotein (a) and stroke: a meta-analysis of observational studies". Stroke. 38 (6): 1959–66. doi:10.1161/STROKEAHA.106.480657. PMID 17478739.
- ^ Schreiner PJ, Morrisett JD, Sharrett AR, Patsch W, Tyroler HA, Wu K, Heiss G (June 1993). "Lipoprotein[a] as a risk factor for preclinical atherosclerosis". Arteriosclerosis and Thrombosis. 13 (6): 826–33. doi:10.1161/01.ATV.13.6.826. PMID 8499402.
- ^ a b Dietary Guidelines Advisory Committee (2015). "Scientific Report of the 2015 Dietary Guidelines Advisory Committee: Advisory Report to the Secretary of Health and Human Services and the Secretary of Agriculture". Washington, DC: U.S. Department of Agriculture, Agricultural Research Service.
- ^ McPherson R, Tybjaerg-Hansen A (February 2016). "Genetics of Coronary Artery Disease". Circulation Research. 118 (4): 564–78. doi:10.1161/circresaha.115.306566. PMID 26892958.
- ^ van der Harst P, Verweij N (February 2018). "Identification of 64 Novel Genetic Loci Provides an Expanded View on the Genetic Architecture of Coronary Artery Disease". Circulation Research. 122 (3). Ovid Technologies (Wolters Kluwer Health): 433–443. doi:10.1161/circresaha.117.312086. PMC 5805277. PMID 29212778.
- ^ Mu F, Rich-Edwards J, Rimm EB, Spiegelman D, Missmer SA (May 2016). "Endometriosis and Risk of Coronary Heart Disease". Circulation: Cardiovascular Quality and Outcomes. 9 (3): 257–64. doi:10.1161/CIRCOUTCOMES.115.002224. PMC 4940126. PMID 27025928.
- ^ Albus C (October 2010). "Psychological and social factors in coronary heart disease". Annals of Medicine. 42 (7): 487–94. doi:10.3109/07853890.2010.515605. PMID 20839918. S2CID 25144107.
- ^ Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. (May 1998). "Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study". American Journal of Preventive Medicine. 14 (4): 245–58. doi:10.1016/S0749-3797(98)00017-8. PMID 9635069.
- ^ Grant PJ (July 2003). "The genetics of atherothrombotic disorders: a clinician's view". Journal of Thrombosis and Haemostasis (Review). 1 (7): 1381–90. doi:10.1046/j.1538-7836.2003.00276.x. PMID 12871271. S2CID 20395787.
- ^ Padmanaban P, Toora B (2011). "Hemoglobin: Emerging marker in stable coronary artery disease". Chronicles of Young Scientists. 2 (2): 109. doi:10.4103/2229-5186.82971. Gale A261829143.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Fajar JK (27 February 2017). "The β fibrinogen gene G-455A polymorphism in Asian subjects with coronary heart disease: A meta analysis". Egyptian Journal of Medical Human Genetics. 18 (1): 19–28. doi:10.1016/j.ejmhg.2016.06.002.
- ^ Ambrose JA, Singh M (2015). "Pathophysiology of coronary artery disease leading to acute coronary syndromes". F1000Prime Reports. 7: 08. doi:10.12703/P7-08. PMC 4311268. PMID 25705391.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Aziz S, Ramsdale DR (June 2005). "Chronic total occlusions--a stiff challenge requiring a major breakthrough: is there light at the end of the tunnel?". Heart. 91 (Suppl 3): iii42-8. doi:10.1136/hrt.2004.058495. PMC 1876352. PMID 15919653.
- ^ Lanza GA (February 2007). "Cardiac syndrome X: a critical overview and future perspectives". Heart. 93 (2): 159–66. doi:10.1136/hrt.2005.067330. PMC 1861371. PMID 16399854.
- ^ Jones E, Eteiba W, Merz NB (August 2012). "Cardiac syndrome X and microvascular coronary dysfunction". Trends in Cardiovascular Medicine. 22 (6): 161–8. doi:10.1016/j.tcm.2012.07.014. PMC 3490207. PMID 23026403.
- ^ Petersen JW, Pepine CJ (February 2015). "Microvascular coronary dysfunction and ischemic heart disease: where are we in 2014?". Trends in Cardiovascular Medicine. 25 (2): 98–103. doi:10.1016/j.tcm.2014.09.013. PMC 4336803. PMID 25454903.
- ^ Kaski JC (February 2004). "Pathophysiology and management of patients with chest pain and normal coronary arteriograms (cardiac syndrome X)". Circulation. 109 (5): 568–72. doi:10.1161/01.CIR.0000116601.58103.62. PMID 14769677. S2CID 18216111.
- ^ a b American Society of Echocardiography (20 December 2012). "Five Things Physicians and Patients Should Question". Choosing Wisely: An Initiative of the ABIM Foundation. Archived from the original on 26 February 2013. Retrieved 27 February 2013., citing
- Douglas PS, Garcia MJ, Haines DE, Lai WW, Manning WJ, Patel AR, et al. (March 2011). "ACCF/ASE/AHA/ASNC/HFSA/HRS/SCAI/SCCM/SCCT/SCMR 2011 Appropriate Use Criteria for Echocardiography. A Report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, American Society of Echocardiography, American Heart Association, American Society of Nuclear Cardiology, Heart Failure Society of America, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, Society of Critical Care Medicine, Society of Cardiovascular Computed Tomography, and Society for Cardiovascular Magnetic Resonance Endorsed by the American College of Chest Physicians". Journal of the American College of Cardiology. 57 (9): 1126–66. doi:10.1016/j.jacc.2010.11.002. PMID 21349406.
- Gibbons RJ, Abrams J, Chatterjee K, Daley J, Deedwania PC, Douglas JS, et al. (January 2003). "ACC/AHA 2002 guideline update for the management of patients with chronic stable angina--summary article: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines (Committee on the Management of Patients With Chronic Stable Angina)". Journal of the American College of Cardiology. 41 (1): 159–68. doi:10.1016/S0735-1097(02)02848-6. PMID 12570960.
- Greenland P, Alpert JS, Beller GA, Benjamin EJ, Budoff MJ, Fayad ZA, et al. (December 2010). "2010 ACCF/AHA guideline for assessment of cardiovascular risk in asymptomatic adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines". Journal of the American College of Cardiology. 56 (25): e50-103. doi:10.1016/j.jacc.2010.09.001. PMID 21144964.
- ^ American College of Cardiology (September 2013), "Five Things Physicians and Patients Should Question", Choosing Wisely: an initiative of the ABIM Foundation, American College of Cardiology, archived from the original on 17 December 2013, retrieved 10 February 2014
- ^ Agrawal S, Mehta PK, Bairey Merz CN (August 2014). "Cardiac Syndrome X: update 2014". Cardiology Clinics. 32 (3): 463–78. doi:10.1016/j.ccl.2014.04.006. PMC 4122947. PMID 25091971.
- ^ "Coronary Artery Disease Diagnosis and Treatment". Mayo Clinic.
- ^ "Coronary Angiography". National Heart, Blood, and Lung Institute. Retrieved 10 December 2017.
- ^ a b Li YR (2015). "Overview of ischemic heart disease, stable angina, and drug therapy". Cardiovascular Diseases: From Molecular Pharmacology to Evidence-Based Therapeutics. John Wiley & Sons. pp. 245–253. ISBN 978-0-470-91537-0.
- ^ Fihn SD, Blankenship JC, Alexander KP, Bittl JA, Byrne JG, Fletcher BJ, et al. (November 2014). "2014 ACC/AHA/AATS/PCNA/SCAI/STS focused update of the guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines, and the American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons". Circulation. 130 (19): 1749–67. doi:10.1161/CIR.0000000000000095. PMID 25070666.
- ^ "ESC Guidelines on Chronic Coronary Syndromes (Previously titled Stable Coronary Artery Disease)". European Society of Cardiology.
- ^ Berry JD, Lloyd-Jones DM, Garside DB, Greenland P (July 2007). "Framingham risk score and prediction of coronary heart disease death in young men". American Heart Journal. 154 (1): 80–6. doi:10.1016/j.ahj.2007.03.042. PMC 2279177. PMID 17584558.
- ^ Khera AV, Emdin CA, Drake I, Natarajan P, Bick AG, Cook NR, et al. (December 2016). "Genetic Risk, Adherence to a Healthy Lifestyle, and Coronary Disease". The New England Journal of Medicine. 375 (24): 2349–2358. doi:10.1056/NEJMoa1605086. PMC 5338864. PMID 27959714.
- ^ McGill HC, McMahan CA, Gidding SS (March 2008). "Preventing heart disease in the 21st century: implications of the Pathobiological Determinants of Atherosclerosis in Youth (PDAY) study". Circulation. 117 (9): 1216–27. doi:10.1161/CIRCULATIONAHA.107.717033. PMID 18316498.
- ^ McNeal CJ, Dajani T, Wilson D, Cassidy-Bushrow AE, Dickerson JB, Ory M (January 2010). "Hypercholesterolemia in youth: opportunities and obstacles to prevent premature atherosclerotic cardiovascular disease". Current Atherosclerosis Reports. 12 (1): 20–8. doi:10.1007/s11883-009-0072-0. PMID 20425267. S2CID 37833889.
- ^ Naci H, Ioannidis JP (October 2013). "Comparative effectiveness of exercise and drug interventions on mortality outcomes: metaepidemiological study". BMJ. 347 (oct01 1): f5577. doi:10.1136/bmj.f5577. PMC 3788175. PMID 24473061.
- ^ Kyu HH, Bachman VF, Alexander LT, Mumford JE, Afshin A, Estep K, et al. (August 2016). "Physical activity and risk of breast cancer, colon cancer, diabetes, ischemic heart disease, and ischemic stroke events: systematic review and dose-response meta-analysis for the Global Burden of Disease Study 2013". BMJ. 354: i3857. doi:10.1136/bmj.i3857. PMC 4979358. PMID 27510511.
- ^ "Life's Essential 8". www.heart.org. Retrieved 3 July 2022.
- ^ Ebrahim S, Taylor F, Ward K, Beswick A, Burke M, Davey Smith G (January 2011). "Multiple risk factor interventions for primary prevention of coronary heart disease". The Cochrane Database of Systematic Reviews (1): CD001561. doi:10.1002/14651858.cd001561.pub3. PMC 4160097. PMID 21249647.
- ^ "5. Population nutrient intake goals for preventing diet-related chronic diseases". WHO. Archived from the original on 29 December 2015. Retrieved 26 October 2015.
- ^ Wang X, Ouyang Y, Liu J, Zhu M, Zhao G, Bao W, Hu FB (July 2014). "Fruit and vegetable consumption and mortality from all causes, cardiovascular disease, and cancer: systematic review and dose-response meta-analysis of prospective cohort studies". BMJ. 349: g4490. doi:10.1136/bmj.g4490. PMC 4115152. PMID 25073782.
- ^ Li D (January 2014). "Effect of the vegetarian diet on non-communicable diseases". Journal of the Science of Food and Agriculture. 94 (2): 169–73. doi:10.1002/jsfa.6362. PMID 23965907.
- ^ Huang T, Yang B, Zheng J, Li G, Wahlqvist ML, Li D (2012). "Cardiovascular disease mortality and cancer incidence in vegetarians: a meta-analysis and systematic review". Annals of Nutrition & Metabolism. 60 (4): 233–40. doi:10.1159/000337301. PMID 22677895.
- ^ Ginter E (2008). "Vegetarian diets, chronic diseases and longevity". Bratislavske Lekarske Listy. 109 (10): 463–6. PMID 19166134.
- ^ Walker C, Reamy BV (April 2009). "Diets for cardiovascular disease prevention: what is the evidence?". American Family Physician. 79 (7): 571–8. PMID 19378874.
- ^ Threapleton DE, Greenwood DC, Evans CE, Cleghorn CL, Nykjaer C, Woodhead C, et al. (December 2013). "Dietary fibre intake and risk of cardiovascular disease: systematic review and meta-analysis". BMJ. 347: f6879. doi:10.1136/bmj.f6879. PMC 3898422. PMID 24355537.
- ^ Reynolds A, Mann J, Cummings J, Winter N, Mete E, Te Morenga L (February 2019). "Carbohydrate quality and human health: a series of systematic reviews and meta-analyses". Lancet. 393 (10170): 434–445. doi:10.1016/S0140-6736(18)31809-9. PMID 30638909. S2CID 58632705.
- ^ Lopez-Garcia E, Schulze MB, Meigs JB, Manson JE, Rifai N, Stampfer MJ, et al. (March 2005). "Consumption of trans fatty acids is related to plasma biomarkers of inflammation and endothelial dysfunction". The Journal of Nutrition. 135 (3): 562–6. doi:10.1093/jn/135.3.562. PMID 15735094.
- ^ Mozaffarian D, Katan MB, Ascherio A, Stampfer MJ, Willett WC (April 2006). "Trans fatty acids and cardiovascular disease". The New England Journal of Medicine. 354 (15): 1601–13. doi:10.1056/NEJMra054035. PMID 16611951.
- ^ Rizos EC, Ntzani EE, Bika E, Kostapanos MS, Elisaf MS (September 2012). "Association between omega-3 fatty acid supplementation and risk of major cardiovascular disease events: a systematic review and meta-analysis". JAMA. 308 (10): 1024–33. doi:10.1001/2012.jama.11374. PMID 22968891.
- ^ Kwak SM, Myung SK, Lee YJ, Seo HG (May 2012). "Efficacy of omega-3 fatty acid supplements (eicosapentaenoic acid and docosahexaenoic acid) in the secondary prevention of cardiovascular disease: a meta-analysis of randomized, double-blind, placebo-controlled trials". Archives of Internal Medicine. 172 (9): 686–94. doi:10.1001/archinternmed.2012.262. PMID 22493407.
- ^ Erkkilä AT, Booth SL (February 2008). "Vitamin K intake and atherosclerosis". Current Opinion in Lipidology. 19 (1): 39–42. doi:10.1097/MOL.0b013e3282f1c57f. PMID 18196985. S2CID 205828596.
- ^ Linden W, Stossel C, Maurice J (April 1996). "Psychosocial interventions for patients with coronary artery disease: a meta-analysis". Archives of Internal Medicine. 156 (7): 745–52. doi:10.1001/archinte.1996.00440070065008. PMID 8615707.
- ^ a b Richards SH, Anderson L, Jenkinson CE, Whalley B, Rees K, Davies P, et al. (Cochrane Heart Group) (April 2017). "Psychological interventions for coronary heart disease". The Cochrane Database of Systematic Reviews. 4 (2): CD002902. doi:10.1002/14651858.CD002902.pub4. PMC 6478177. PMID 28452408.
- ^ Swardfager W, Herrmann N, Cornish S, Mazereeuw G, Marzolini S, Sham L, Lanctôt KL (April 2012). "Exercise intervention and inflammatory markers in coronary artery disease: a meta-analysis". American Heart Journal. 163 (4): 666–76.e1–3. doi:10.1016/j.ahj.2011.12.017. PMID 22520533.
- ^ How to Increase Your HDL Cholesterol Levels Archived 14 July 2006 at the Wayback Machine; accessed 26 October 2015.
- ^ "Coronary Heart Disease (CHD)". Penguin Dictionary of Biology. 2004.
- ^ U.S. Preventive Services Task Force (August 2002). "Behavioral counseling in primary care to promote physical activity: recommendation and rationale". Annals of Internal Medicine. 137 (3): 205–7. doi:10.7326/0003-4819-137-3-200208060-00014. PMID 12160370. S2CID 38338385.
- ^ Thompson PD, Buchner D, Pina IL, Balady GJ, Williams MA, Marcus BH, et al. (June 2003). "Exercise and physical activity in the prevention and treatment of atherosclerotic cardiovascular disease: a statement from the Council on Clinical Cardiology (Subcommittee on Exercise, Rehabilitation, and Prevention) and the Council on Nutrition, Physical Activity, and Metabolism (Subcommittee on Physical Activity)". Circulation. 107 (24): 3109–16. doi:10.1161/01.CIR.0000075572.40158.77. PMID 12821592.
- ^ a b Sethi NJ, Safi S, Korang SK, Hróbjartsson A, Skoog M, Gluud C, Jakobsen JC, et al. (Cochrane Heart Group) (February 2021). "Antibiotics for secondary prevention of coronary heart disease". The Cochrane Database of Systematic Reviews. 2 (5): CD003610. doi:10.1002/14651858.CD003610.pub4. PMC 8094925. PMID 33704780.
- ^ Narvaez Linares NF, Poitras M, Burkauskas J, Nagaratnam K, Burr Z, Labelle PR, Plamondon H (August 2021). "Neuropsychological Sequelae of Coronary Heart Disease in Women: A Systematic Review". Neuroscience and Biobehavioral Reviews. 127: 837–851. doi:10.1016/j.neubiorev.2021.05.026. PMID 34062209. S2CID 235245540.
- ^ Jameson JN, Kasper DL, Harrison TR, Braunwald E, Fauci AS, Hauser SL, Longo DL (2005). Harrison's principles of internal medicine (16th ed.). New York: McGraw-Hill Medical Publishing Division. ISBN 978-0-07-140235-4. OCLC 54501403. Archived from the original on 19 February 2014. Retrieved 26 October 2015.
- ^ Gutierrez J, Ramirez G, Rundek T, Sacco RL (June 2012). "Statin therapy in the prevention of recurrent cardiovascular events: a sex-based meta-analysis". Archives of Internal Medicine. 172 (12): 909–19. doi:10.1001/archinternmed.2012.2145. PMID 22732744.
- ^ MedlinePlus Encyclopedia: Nitroglycerin Sublingual
- ^ a b Ohman EM (March 2016). "CLINICAL PRACTICE. Chronic Stable Angina". The New England Journal of Medicine. 374 (12): 1167–76. doi:10.1056/NEJMcp1502240. PMID 27007960.
- ^ Grove EL, Würtz M, Thomas MR, Kristensen SD (2015). "Antiplatelet therapy in acute coronary syndromes". Expert Opinion on Pharmacotherapy (Review). 16 (14): 2133–47. doi:10.1517/14656566.2015.1079619. PMID 26293612. S2CID 9841653.
- ^ a b Rosendorff C, Lackland DT, Allison M, Aronow WS, Black HR, Blumenthal RS, et al. (May 2015). "Treatment of hypertension in patients with coronary artery disease: a scientific statement from the American Heart Association, American College of Cardiology, and American Society of Hypertension". Circulation. 131 (19): e435-70. doi:10.1161/cir.0000000000000207. PMC 8365343. PMID 25829340.
- ^ Guirguis-Blake JM, Evans CV, Senger CA, O'Connor EA, Whitlock EP (June 2016). "Aspirin for the Primary Prevention of Cardiovascular Events: A Systematic Evidence Review for the U.S. Preventive Services Task Force". Annals of Internal Medicine (Systematic Review and Meta-Analysis). 164 (12): 804–13. doi:10.7326/M15-2113. PMID 27064410.
- ^ U.S. Preventive Services Task Force (January 2002). "Aspirin for the primary prevention of cardiovascular events: recommendation and rationale". Annals of Internal Medicine. 136 (2): 157–60. doi:10.7326/0003-4819-136-2-200201150-00015. PMID 11790071.
- ^ Squizzato A, Bellesini M, Takeda A, Middeldorp S, Donadini MP (December 2017). "Clopidogrel plus aspirin versus aspirin alone for preventing cardiovascular events". The Cochrane Database of Systematic Reviews. 12: CD005158. doi:10.1002/14651858.CD005158.pub4. PMC 6486024. PMID 29240976.
- ^ "FDA Drug Safety Communication: FDA review finds long-term treatment with blood-thinning medicine Plavix (clopidogrel) does not change risk of death". FDA. 6 November 2015. Archived from the original on 4 February 2016. Retrieved 25 January 2016.
- ^ Elmariah S, Mauri L, Doros G, Galper BZ, O'Neill KE, Steg PG, et al. (February 2015). "Extended duration dual antiplatelet therapy and mortality: a systematic review and meta-analysis". Lancet. 385 (9970): 792–8. doi:10.1016/S0140-6736(14)62052-3. PMC 4386690. PMID 25467565.
- ^ Braunwald E, Antman EM, Beasley JW, Califf RM, Cheitlin MD, Hochman JS, et al. (October 2002). "ACC/AHA guideline update for the management of patients with unstable angina and non-ST-segment elevation myocardial infarction--2002: summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on the Management of Patients With Unstable Angina)". Circulation. 106 (14): 1893–900. doi:10.1161/01.CIR.0000037106.76139.53. PMID 12356647.
- ^ Stergiopoulos K, Boden WE, Hartigan P, Möbius-Winkler S, Hambrecht R, Hueb W, et al. (February 2014). "Percutaneous coronary intervention outcomes in patients with stable obstructive coronary artery disease and myocardial ischemia: a collaborative meta-analysis of contemporary randomized clinical trials". JAMA Internal Medicine. 174 (2): 232–40. doi:10.1001/jamainternmed.2013.12855. PMID 24296791.
- ^ Sipahi I, Akay MH, Dagdelen S, Blitz A, Alhan C (February 2014). "Coronary artery bypass grafting vs percutaneous coronary intervention and long-term mortality and morbidity in multivessel disease: meta-analysis of randomized clinical trials of the arterial grafting and stenting era". JAMA Internal Medicine. 174 (2): 223–30. doi:10.1001/jamainternmed.2013.12844. PMID 24296767.
- ^ Zhao DF, Edelman JJ, Seco M, Bannon PG, Wilson MK, Byrom MJ, et al. (February 2017). "Coronary Artery Bypass Grafting With and Without Manipulation of the Ascending Aorta: A Network Meta-Analysis". Journal of the American College of Cardiology. 69 (8): 924–936. doi:10.1016/j.jacc.2016.11.071. PMID 28231944.
- ^ Reynolds AC, King N (August 2018). "Hybrid coronary revascularization versus conventional coronary artery bypass grafting: Systematic review and meta-analysis". Medicine. 97 (33): e11941. doi:10.1097/MD.0000000000011941. PMC 6112891. PMID 30113498.
- ^ "WHO Disease and injury country estimates". World Health Organization. 2009. Archived from the original on 11 November 2009. Retrieved 11 November 2009.
- ^ a b Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. (December 2012). "Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010". Lancet. 380 (9859): 2095–128. doi:10.1016/S0140-6736(12)61728-0. hdl:10536/DRO/DU:30050819. PMID 23245604. S2CID 1541253.
- ^ a b Finegold JA, Asaria P, Francis DP (September 2013). "Mortality from ischaemic heart disease by country, region, and age: statistics from World Health Organisation and United Nations". International Journal of Cardiology. 168 (2): 934–45. doi:10.1016/j.ijcard.2012.10.046. PMC 3819990. PMID 23218570.
- ^ Indian Heart Association Why South Asians Facts Archived 18 May 2015 at the Wayback Machine, 29 April 2015; accessed 26 October 2015.
- ^ Kochanek KD, Xu J, Murphy SL, Miniño AM, Kung HC (December 2011). "Deaths: final data for 2009" (PDF). National Vital Statistics Reports. 60 (3): 1–116. PMID 24974587.
- ^ Rosamond W, Flegal K, Friday G, Furie K, Go A, Greenlund K, et al. (February 2007). "Heart disease and stroke statistics--2007 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee". Circulation. 115 (5): e69-171. doi:10.1161/CIRCULATIONAHA.106.179918. PMID 17194875.
- ^ American Heart Association:Heart Disease and Stroke Statistics-2007 Update. AHA, Dallas, Texas, 2007 Archived 1 July 2007 at the Wayback Machine
- ^ "Other Names for Coronary Heart Disease". 29 September 2014. Archived from the original on 13 February 2015. Retrieved 23 February 2015.
- ^ "Our Mission". Infarct Combat Project.
- ^ O'Connor, Anahad, "How the Sugar Industry Shifted Blame to Fat" Archived 28 February 2017 at the Wayback Machine, The New York Times, 12 September 2016. Retrieved 12 September 2016.
- ^ Nestle M (November 2016). "Food Industry Funding of Nutrition Research: The Relevance of History for Current Debates". JAMA Internal Medicine. 176 (11): 1685–1686. doi:10.1001/jamainternmed.2016.5400. PMID 27618496.
- ^ Kearns CE, Schmidt LA, Glantz SA (November 2016). "Sugar Industry and Coronary Heart Disease Research: A Historical Analysis of Internal Industry Documents". JAMA Internal Medicine. 176 (11): 1680–1685. doi:10.1001/jamainternmed.2016.5394. PMC 5099084. PMID 27617709.
- ^ Ifill G (13 September 2016). "How the sugar industry paid experts to downplay health risks". PBS NewsHour. Archived from the original on 20 August 2017.
- ^ Farrall M, Green FR, Peden JF, Olsson PG, Clarke R, Hellenius ML, et al. (May 2006). "Genome-wide mapping of susceptibility to coronary artery disease identifies a novel replicated locus on chromosome 17". PLOS Genetics. 2 (5): e72. doi:10.1371/journal.pgen.0020072. PMC 1463045. PMID 16710446.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Roberts R, Stewart AF (January 2012). "9p21 and the genetic revolution for coronary artery disease". Clinical Chemistry. 58 (1): 104–12. doi:10.1373/clinchem.2011.172759. PMID 22015375.
- ^ Dandona S, Stewart AF, Roberts R (March 2010). "Genomics in coronary artery disease: past, present and future". The Canadian Journal of Cardiology. 26 (Suppl A): 56A–59A. doi:10.1016/s0828-282x(10)71064-3. PMID 20386763.
- ^ Saikku P, Leinonen M, Tenkanen L, Linnanmäki E, Ekman MR, Manninen V, et al. (February 1992). "Chronic Chlamydia pneumoniae infection as a risk factor for coronary heart disease in the Helsinki Heart Study". Annals of Internal Medicine. 116 (4): 273–8. doi:10.7326/0003-4819-116-4-273. PMID 1733381.
- ^ Grayston JT, Belland RJ, Byrne GI, Kuo CC, Schachter J, Stamm WE, Zhong G (February 2015). "Infection with Chlamydia pneumoniae as a cause of coronary heart disease: the hypothesis is still untested". Pathogens and Disease. 73 (1): 1–9. doi:10.1093/femspd/ftu015. PMC 4492408. PMID 25854002.
- ^ Andraws R, Berger JS, Brown DL (June 2005). "Effects of antibiotic therapy on outcomes of patients with coronary artery disease: a meta-analysis of randomized controlled trials". JAMA. 293 (21): 2641–7. doi:10.1001/jama.293.21.2641. PMID 15928286.
- ^ Simons M, Bonow RO, Chronos NA, Cohen DJ, Giordano FJ, Hammond HK, et al. (September 2000). "Clinical trials in coronary angiogenesis: issues, problems, consensus: An expert panel summary". Circulation. 102 (11): E73-86. doi:10.1161/01.CIR.102.11.e73. PMID 10982554.
- ^ Stegmann TJ (December 1998). "FGF-1: a human growth factor in the induction of neoangiogenesis". Expert Opinion on Investigational Drugs. 7 (12): 2011–5. doi:10.1517/13543784.7.12.2011. PMID 15991943.
- ^ Wagoner LE, Merrill W, Jacobs J, Conway G, Boehmer J, Thomas K, et al. (16 October 2007). "Abstract 2048: Angiogenesis Protein Therapy With Human Fibroblast Growth Factor (fgf-1): Results Of A Phase I Open Label, Dose Escalation Study In Subjects With CAD Not Eligible For PCI Or CABG". Circulation. 116 (suppl_16): II_443. doi:10.1161/circ.116.suppl_16.II_443-b (inactive 31 July 2022).
{{cite journal}}: CS1 maint: DOI inactive as of July 2022 (link) - ^ Loria V, Dato I, Graziani F, Biasucci LM (2008). "Myeloperoxidase: a new biomarker of inflammation in ischemic heart disease and acute coronary syndromes". Mediators of Inflammation. 2008: 135625. doi:10.1155/2008/135625. PMC 2276594. PMID 18382609.
- ^ Esselstyn CB, Gendy G, Doyle J, Golubic M, Roizen MF (July 2014). "A way to reverse CAD?" (PDF). The Journal of Family Practice. 63 (7): 356–364b. PMID 25198208.
- ^ Freeman AM, Morris PB, Barnard N, Esselstyn CB, Ros E, Agatston A, et al. (March 2017). "Trending Cardiovascular Nutrition Controversies". Journal of the American College of Cardiology. 69 (9): 1172–1187. doi:10.1016/j.jacc.2016.10.086. PMID 28254181.
External links
- Risk Assessment of having a heart attack or dying of coronary artery disease, from the American Heart Association.
- "Coronary Artery Disease". MedlinePlus. U.S. National Library of Medicine.
