Isotopes of iodine
This article needs additional citations for verification. (May 2018) |
| ||||||||||||||||||||||||||||||||||||||||||||||
| Standard atomic weight Ar°(I) | ||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
There are 37 known isotopes of iodine (53I) from 108I to 144I; all undergo radioactive decay except 127I, which is stable. Iodine is thus a monoisotopic element.
Its longest-lived radioactive isotope, 129I, has a half-life of 15.7 million years, which is far too short for it to exist as a primordial nuclide. Cosmogenic sources of 129I produce very tiny quantities of it that are too small to affect atomic weight measurements; iodine is thus also a mononuclidic element—one that is found in nature only as a single nuclide. Most 129I derived radioactivity on Earth is man-made, an unwanted long-lived byproduct of early nuclear tests and nuclear fission accidents.
All other iodine radioisotopes have half-lives less than 60 days, and four of these are used as tracers and therapeutic agents in medicine. These are 123I, 124I, 125I, and 131I. All industrial production of radioactive iodine isotopes involves these four useful radionuclides.
The isotope 135I has a half-life less than seven hours, which is too short to be used in biology. Unavoidable in situ production of this isotope is important in nuclear reactor control, as it decays to 135Xe, the most powerful known neutron absorber, and the nuclide responsible for the so-called iodine pit phenomenon.
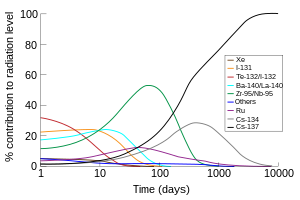
In addition to commercial production, 131I (half-life 8 days) is one of the common radioactive fission products of nuclear fission, and is thus produced inadvertently in very large amounts inside nuclear reactors. Due to its volatility, short half-life, and high abundance in fission products, 131I (along with the short-lived iodine isotope 132I, which is produced from the decay of 132Te with a half-life of 3 days) is responsible for the largest part of radioactive contamination during the first week after accidental environmental contamination from the radioactive waste from a nuclear power plant. Thus highly dosed iodine supplements (usually potassium iodide) are given to the populace after nuclear accidents or explosions (and in some cases prior to any such incident as a civil defense mechanism) to reduce the uptake of radioactive iodine compounds by the thyroid before the highly radioactive isotopes have had time to decay.
List of isotopes
| Nuclide [n 1] |
Z | N | Isotopic mass (Da) [n 2][n 3] |
Half-life [n 4] |
Decay mode [n 5] |
Daughter isotope [n 6][n 7] |
Spin and parity [n 8][n 4] |
Isotopic abundance | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Excitation energy[n 4] | |||||||||||||||||||
| 108I | 53 | 55 | 107.94348(39)# | 36(6) ms | α (90%) | 104Sb | (1)# | ||||||||||||
| β+ (9%) | 108Te | ||||||||||||||||||
| p (1%) | 107Te | ||||||||||||||||||
| 109I | 53 | 56 | 108.93815(11) | 103(5) µs | p (99.5%) | 108Te | (5/2+) | ||||||||||||
| α (.5%) | 105Sb | ||||||||||||||||||
| 110I | 53 | 57 | 109.93524(33)# | 650(20) ms | β+ (70.9%) | 110Te | 1+# | ||||||||||||
| α (17%) | 106Sb | ||||||||||||||||||
| β+, p (11%) | 109Sb | ||||||||||||||||||
| β+, α (1.09%) | 106Sn | ||||||||||||||||||
| 111I | 53 | 58 | 110.93028(32)# | 2.5(2) s | β+ (99.92%) | 111Te | (5/2+)# | ||||||||||||
| α (.088%) | 107Sb | ||||||||||||||||||
| 112I | 53 | 59 | 111.92797(23)# | 3.42(11) s | β+ (99.01%) | 112Te | |||||||||||||
| β+, p (.88%) | 111Sb | ||||||||||||||||||
| β+, α (.104%) | 108Sn | ||||||||||||||||||
| α (.0012%) | 108Sb | ||||||||||||||||||
| 113I | 53 | 60 | 112.92364(6) | 6.6(2) s | β+ (100%) | 113Te | 5/2+# | ||||||||||||
| α (3.3×10−7%) | 109Sb | ||||||||||||||||||
| β+, α | 109Sn | ||||||||||||||||||
| 114I | 53 | 61 | 113.92185(32)# | 2.1(2) s | β+ | 114Te | 1+ | ||||||||||||
| β+, p (rare) | 113Sb | ||||||||||||||||||
| 114mI | 265.9(5) keV | 6.2(5) s | β+ (91%) | 114Te | (7) | ||||||||||||||
| IT (9%) | 114I | ||||||||||||||||||
| 115I | 53 | 62 | 114.91805(3) | 1.3(2) min | β+ | 115Te | (5/2+)# | ||||||||||||
| 116I | 53 | 63 | 115.91681(10) | 2.91(15) s | β+ | 116Te | 1+ | ||||||||||||
| 116mI | 400(50)# keV | 3.27(16) µs | (7−) | ||||||||||||||||
| 117I | 53 | 64 | 116.91365(3) | 2.22(4) min | β+ | 117Te | (5/2)+ | ||||||||||||
| 118I | 53 | 65 | 117.913074(21) | 13.7(5) min | β+ | 118Te | 2− | ||||||||||||
| 118mI | 190.1(10) keV | 8.5(5) min | β+ | 118Te | (7−) | ||||||||||||||
| IT (rare) | 118I | ||||||||||||||||||
| 119I | 53 | 66 | 118.91007(3) | 19.1(4) min | β+ | 119Te | 5/2+ | ||||||||||||
| 120I | 53 | 67 | 119.910048(19) | 81.6(2) min | β+ | 120Te | 2− | ||||||||||||
| 120m1I | 72.61(9) keV | 228(15) ns | (1+, 2+, 3+) | ||||||||||||||||
| 120m2I | 320(15) keV | 53(4) min | β+ | 120Te | (7−) | ||||||||||||||
| 121I | 53 | 68 | 120.907367(11) | 2.12(1) h | β+ | 121Te | 5/2+ | ||||||||||||
| 121mI | 2376.9(4) keV | 9.0(15) µs | |||||||||||||||||
| 122I | 53 | 69 | 121.907589(6) | 3.63(6) min | β+ | 122Te | 1+ | ||||||||||||
| 123I[n 9] | 53 | 70 | 122.905589(4) | 13.2235(19) h | EC | 123Te | 5/2+ | ||||||||||||
| 124I[n 9] | 53 | 71 | 123.9062099(25) | 4.1760(3) d | β+ | 124Te | 2− | ||||||||||||
| 125I[n 9] | 53 | 72 | 124.9046302(16) | 59.400(10) d | EC | 125Te | 5/2+ | ||||||||||||
| 126I | 53 | 73 | 125.905624(4) | 12.93(5) d | β+ (56.3%) | 126Te | 2− | ||||||||||||
| β− (43.7%) | 126Xe | ||||||||||||||||||
| 127I[n 10] | 53 | 74 | 126.904473(4) | Stable | 5/2+ | 1.0000 | |||||||||||||
| 128I | 53 | 75 | 127.905809(4) | 24.99(2) min | β− (93.1%) | 128Xe | 1+ | ||||||||||||
| β+ (6.9%) | 128Te | ||||||||||||||||||
| 128m1I | 137.850(4) keV | 845(20) ns | 4− | ||||||||||||||||
| 128m2I | 167.367(5) keV | 175(15) ns | (6)− | ||||||||||||||||
| 129I[n 10][n 11] | 53 | 76 | 128.904988(3) | 1.57(4)×107 y | β− | 129Xe | 7/2+ | Trace[n 12] | |||||||||||
| 130I | 53 | 77 | 129.906674(3) | 12.36(1) h | β− | 130Xe | 5+ | ||||||||||||
| 130m1I | 39.9525(13) keV | 8.84(6) min | IT (84%) | 130I | 2+ | ||||||||||||||
| β− (16%) | 130Xe | ||||||||||||||||||
| 130m2I | 69.5865(7) keV | 133(7) ns | (6)− | ||||||||||||||||
| 130m3I | 82.3960(19) keV | 315(15) ns | - | ||||||||||||||||
| 130m4I | 85.1099(10) keV | 254(4) ns | (6)− | ||||||||||||||||
| 131I[n 10][n 9] | 53 | 78 | 130.9061246(12) | 8.02070(11) d | β− | 131Xe | 7/2+ | ||||||||||||
| 132I | 53 | 79 | 131.907997(6) | 2.295(13) h | β− | 132Xe | 4+ | ||||||||||||
| 132mI | 104(12) keV | 1.387(15) h | IT (86%) | 132I | (8−) | ||||||||||||||
| β− (14%) | 132Xe | ||||||||||||||||||
| 133I | 53 | 80 | 132.907797(5) | 20.8(1) h | β− | 133Xe | 7/2+ | ||||||||||||
| 133m1I | 1634.174(17) keV | 9(2) s | IT | 133I | (19/2−) | ||||||||||||||
| 133m2I | 1729.160(17) keV | ~170 ns | (15/2−) | ||||||||||||||||
| 134I | 53 | 81 | 133.909744(9) | 52.5(2) min | β− | 134Xe | (4)+ | ||||||||||||
| 134mI | 316.49(22) keV | 3.52(4) min | IT (97.7%) | 134I | (8)− | ||||||||||||||
| β− (2.3%) | 134Xe | ||||||||||||||||||
| 135I[n 13] | 53 | 82 | 134.910048(8) | 6.57(2) h | β− | 135Xe | 7/2+ | ||||||||||||
| 136I | 53 | 83 | 135.91465(5) | 83.4(10) s | β− | 136Xe | (1−) | ||||||||||||
| 136mI | 650(120) keV | 46.9(10) s | β− | 136Xe | (6−) | ||||||||||||||
| 137I | 53 | 84 | 136.917871(30) | 24.13(12) s | β− (92.86%) | 137Xe | (7/2+) | ||||||||||||
| β−, n (7.14%) | 136Xe | ||||||||||||||||||
| 138I | 53 | 85 | 137.92235(9) | 6.23(3) s | β− (94.54%) | 138Xe | (2−) | ||||||||||||
| β−, n (5.46%) | 137Xe | ||||||||||||||||||
| 139I | 53 | 86 | 138.92610(3) | 2.282(10) s | β− (90%) | 139Xe | 7/2+# | ||||||||||||
| β−, n (10%) | 138Xe | ||||||||||||||||||
| 140I | 53 | 87 | 139.93100(21)# | 860(40) ms | β− (90.7%) | 140Xe | (3)(−#) | ||||||||||||
| β−, n (9.3%) | 139Xe | ||||||||||||||||||
| 141I | 53 | 88 | 140.93503(21)# | 430(20) ms | β− (78%) | 141Xe | 7/2+# | ||||||||||||
| β−, n (22%) | 140Xe | ||||||||||||||||||
| 142I | 53 | 89 | 141.94018(43)# | ~200 ms | β− (75%) | 142Xe | 2−# | ||||||||||||
| β−, n (25%) | 141Xe | ||||||||||||||||||
| 143I | 53 | 90 | 142.94456(43)# | 100# ms [> 300 ns] | β− | 143Xe | 7/2+# | ||||||||||||
| 144I | 53 | 91 | 143.94999(54)# | 50# ms [> 300 ns] | β− | 144Xe | 1−# | ||||||||||||
| This table header & footer: | |||||||||||||||||||
- ^ mI – Excited nuclear isomer.
- ^ ( ) – Uncertainty (1σ) is given in concise form in parentheses after the corresponding last digits.
- ^ # – Atomic mass marked #: value and uncertainty derived not from purely experimental data, but at least partly from trends from the Mass Surface (TMS).
- ^ a b c # – Values marked # are not purely derived from experimental data, but at least partly from trends of neighboring nuclides (TNN).
- ^
Modes of decay:
EC: Electron capture IT: Isomeric transition n: Neutron emission p: Proton emission - ^ Bold italics symbol as daughter – Daughter product is nearly stable.
- ^ Bold symbol as daughter – Daughter product is stable.
- ^ ( ) spin value – Indicates spin with weak assignment arguments.
- ^ a b c d Has medical uses
- ^ a b c Fission product
- ^ Can be used to date certain early events in Solar System history and some use for dating groundwater
- ^ Cosmogenic nuclide, also found as nuclear contamination
- ^ Produced as a decay product of 135Te in nuclear reactors, in turn decays to 135Xe, which, if allowed to build up, can shut down reactors due to the iodine pit phenomenon
Notable radioisotopes
This section needs additional citations for verification. (May 2018) |
Radioisotopes of iodine are called radioactive iodine or radioiodine. Dozens exist, but about a half dozen are the most notable in applied sciences such as the life sciences and nuclear power, as detailed below. Mentions of radioiodine in health care contexts refer more often to iodine-131 than to other isotopes.
Of the many isotopes of iodine, only two are typically used in a medical setting: iodine-123 and iodine-131. Since 131I has both a beta and gamma decay mode, it can be used for radiotherapy or for imaging. 123I, which has no beta activity, is more suited for routine nuclear medicine imaging of the thyroid and other medical processes and less damaging internally to the patient. There are some situations in which iodine-124 and iodine-125 are also used in medicine.[4]
Due to preferential uptake of iodine by the thyroid, radioiodine is extensively used in imaging of and, in the case of 131I, destroying dysfunctional thyroid tissues. Other types of tissue selectively take up certain iodine-131-containing tissue-targeting and killing radiopharmaceutical agents (such as MIBG). Iodine-125 is the only other iodine radioisotope used in radiation therapy, but only as an implanted capsule in brachytherapy, where the isotope never has a chance to be released for chemical interaction with the body's tissues.
Iodine-123 and iodine-125
The gamma-emitting isotopes iodine-123 (half-life 13 hours), and (less commonly) the longer-lived and less energetic iodine-125 (half-life 59 days) are used as nuclear imaging tracers to evaluate the anatomic and physiologic function of the thyroid. Abnormal results may be caused by disorders such as Graves' disease or Hashimoto's thyroiditis. Both isotopes decay by electron capture (EC) to the corresponding tellurium nuclides, but in neither case are these the metastable nuclides 123mTe and 125mTe (which are of higher energy, and are not produced from radioiodine). Instead, the excited tellurium nuclides decay immediately (half-life too short to detect). Following EC, the excited 123Te from 123I emits a high-speed 127 keV internal conversion electron (not a beta ray) about 13% of the time, but this does little cellular damage due to the nuclide's short half-life and the relatively small fraction of such events. In the remainder of cases, a 159 keV gamma ray is emitted, which is well-suited for gamma imaging.
Excited 125Te resulting from electron capture of 125I also emits a much lower-energy internal conversion electron (35.5 keV), which does relatively little damage due to its low energy, even though its emission is more common. The relatively low-energy gamma from 125I/125Te decay is poorly suited for imaging, but can still be seen, and this longer-lived isotope is necessary in tests that require several days of imaging, for example, fibrinogen scan imaging to detect blood clots.
Both 123I and 125I emit copious low energy Auger electrons after their decay, but these do not cause serious damage (double-stranded DNA breaks) in cells, unless the nuclide is incorporated into a medication that accumulates in the nucleus, or into DNA (this is never the case is clinical medicine, but it has been seen in experimental animal models).[5]
Iodine-125 is also commonly used by radiation oncologists in low dose rate brachytherapy in the treatment of cancer at sites other than the thyroid, especially in prostate cancer. When 125I is used therapeutically, it is encapsulated in titanium seeds and implanted in the area of the tumor, where it remains. The low energy of the gamma spectrum in this case limits radiation damage to tissues far from the implanted capsule. Iodine-125, due to its suitable longer half-life and less penetrating gamma spectrum, is also often preferred for laboratory tests that rely on iodine as a tracer that is counted by a gamma counter, such as in radioimmunoassaying.
125I is used as the radiolabel in investigating which ligands go to which plant pattern recognition receptors (PRRs).[6]
Iodine-124
Iodine-124 is a proton-rich isotope of iodine with a half-life of 4.18 days. Its modes of decay are: 74.4% electron capture, 25.6% positron emission. 124I decays to 124Te. Iodine-124 can be made by numerous nuclear reactions via a cyclotron. The most common starting material used is 124Te.
Iodine-124 as the iodide salt can be used to directly image the thyroid using positron emission tomography (PET).[7] Iodine-124 can also be used as a PET radiotracer with a usefully longer half-life compared with fluorine-18.[8] In this use, the nuclide is chemically bonded to a pharmaceutical to form a positron-emitting radiopharmaceutical, and injected into the body, where again it is imaged by PET scan.
Iodine-129
Iodine-129 (129I; half-life 15.7 million years) is a product of cosmic ray spallation on various isotopes of xenon in the atmosphere, in cosmic ray muon interaction with tellurium-130, and also uranium and plutonium fission, both in subsurface rocks and nuclear reactors. Artificial nuclear processes, in particular nuclear fuel reprocessing and atmospheric nuclear weapons tests, have now swamped the natural signal for this isotope. Nevertheless, it now serves as a groundwater tracer as indicator of nuclear waste dispersion into the natural environment. In a similar fashion, 129I was used in rainwater studies to track fission products following the Chernobyl disaster.
In some ways, 129I is similar to 36Cl. It is a soluble halogen, exists mainly as a non-sorbing anion, and is produced by cosmogenic, thermonuclear, and in-situ reactions. In hydrologic studies, 129I concentrations are usually reported as the ratio of 129I to total I (which is virtually all 127I). As is the case with 36Cl/Cl, 129I/I ratios in nature are quite small, 10−14 to 10−10 (peak thermonuclear 129I/I during the 1960s and 1970s reached about 10−7). 129I differs from 36Cl in that its half-life is longer (15.7 vs. 0.301 million years), it is highly biophilic, and occurs in multiple ionic forms (commonly, I− and IO3−), which have different chemical behaviors. This makes it fairly easy for 129I to enter the biosphere as it becomes incorporated into vegetation, soil, milk, animal tissue, etc. Excesses of stable 129Xe in meteorites have been shown to result from decay of "primordial" iodine-129 produced newly by the supernovas that created the dust and gas from which the solar system formed. This isotope has long decayed and is thus referred to as "extinct". Historically, 129I was the first extinct radionuclide to be identified as present in the early Solar System. Its decay is the basis of the I-Xe iodine-xenon radiometric dating scheme, which covers the first 85 million years of Solar System evolution.
Iodine-131

Iodine-131 (131
I
) is a beta-emitting isotope with a half-life of eight days, and comparatively energetic (190 keV average and 606 keV maximum energy) beta radiation, which penetrates 0.6 to 2.0 mm from the site of uptake. This beta radiation can be used for the destruction of thyroid nodules or hyperfunctioning thyroid tissue and for elimination of remaining thyroid tissue after surgery for the treatment of Graves' disease. The purpose of this therapy, which was first explored by Dr. Saul Hertz in 1941,[9] is to destroy thyroid tissue that could not be removed surgically. In this procedure, 131I is administered either intravenously or orally following a diagnostic scan. This procedure may also be used, with higher doses of radio-iodine, to treat patients with thyroid cancer.
The 131I is taken up into thyroid tissue and concentrated there. The beta particles emitted by the radioisotope destroys the associated thyroid tissue with little damage to surrounding tissues (more than 2.0 mm from the tissues absorbing the iodine). Due to similar destruction, 131I is the iodine radioisotope used in other water-soluble iodine-labeled radiopharmaceuticals (such as MIBG) used therapeutically to destroy tissues.
The high energy beta radiation (up to 606 keV) from 131I causes it to be the most carcinogenic of the iodine isotopes. It is thought to cause the majority of excess thyroid cancers seen after nuclear fission contamination (such as bomb fallout or severe nuclear reactor accidents like the Chernobyl disaster) However, these epidemiological effects are seen primarily in children, and treatment of adults and children with therapeutic 131I, and epidemiology of adults exposed to low-dose 131I has not demonstrated carcinogenicity.[10]
Iodine-135
Iodine-135 is an isotope of iodine with a half-life of 6.6 hours. It is an important isotope from the viewpoint of nuclear reactor physics. It is produced in relatively large amounts as a fission product, and decays to xenon-135, which is a nuclear poison with a very large thermal neutron cross section, which is a cause of multiple complications in the control of nuclear reactors. The process of buildup of xenon-135 from accumulated iodine-135 can temporarily preclude a shut-down reactor from restarting. This is known as xenon poisoning or "falling into an iodine pit".
Iodine-128 and other isotopes
Iodine fission-produced isotopes not discussed above (iodine-128, iodine-130, iodine-132, and iodine-133) have half-lives of several hours or minutes, rendering them almost useless in other applicable areas. Those mentioned are neutron-rich and undergo beta decay to isotopes of xenon. Iodine-128 (half-life 25 minutes) can decay to either tellurium-128 by electron capture or to xenon-128 by beta decay. It has a specific radioactivity of 2.177×106 TBq/g.
Nonradioactive iodide (127I) as protection from unwanted radioiodine uptake by the thyroid
This section possibly contains original research. (May 2018) |
Colloquially, radioactive materials can be described as "hot," and non-radioactive materials can be described as "cold." There are instances in which cold iodide is administered to people in order to prevent the uptake of hot iodide by the thyroid gland. For example, blockade of thyroid iodine uptake with potassium iodide is used in nuclear medicine scintigraphy and therapy with some radioiodinated compounds that are not targeted to the thyroid, such as iobenguane (MIBG), which is used to image or treat neural tissue tumors, or iodinated fibrinogen, which is used in fibrinogen scans to investigate clotting. These compounds contain iodine, but not in the iodide form. However, since they may be ultimately metabolized or break down to radioactive iodide, it is common to administer non-radioactive potassium iodide to insure that metabolites of these radiopharmaceuticals is not sequestered by thyroid gland and inadvertently administer a radiological dose to that tissue.
Potassium iodide has been distributed to populations exposed to nuclear fission accidents such as the Chernobyl disaster. The iodide solution SSKI, a saturated solution of potassium (K) iodide in water, has been used to block absorption of the radioiodine (it has no effect on other radioisotopes from fission). Tablets containing potassium iodide are now also manufactured and stocked in central disaster sites by some governments for this purpose. In theory, many harmful late-cancer effects of nuclear fallout might be prevented in this way, since an excess of thyroid cancers, presumably due to radioiodine uptake, is the only proven radioisotope contamination effect after a fission accident, or from contamination by fallout from an atomic bomb (prompt radiation from the bomb also causes other cancers, such as leukemias, directly). Taking large amounts of iodide saturates thyroid receptors and prevents uptake of most radioactive iodine-131 that may be present from fission product exposure (although it does not protect from other radioisotopes, nor from any other form of direct radiation). The protective effect of KI lasts approximately 24 hours, so must be dosed daily until a risk of significant exposure to radioiodines from fission products no longer exists.[11][12] Iodine-131 (the most common radioiodine contaminant in fallout) also decays relatively rapidly with a half-life of eight days, so that 99.95% of the original radioiodine has vanished after three months.
References
- Isotope masses from:
- Audi, Georges; Bersillon, Olivier; Blachot, Jean; Wapstra, Aaldert Hendrik (2003), "The NUBASE evaluation of nuclear and decay properties", Nuclear Physics A, 729: 3–128, Bibcode:2003NuPhA.729....3A, doi:10.1016/j.nuclphysa.2003.11.001
- Isotopic compositions and standard atomic masses from:
- de Laeter, John Robert; Böhlke, John Karl; De Bièvre, Paul; Hidaka, Hiroshi; Peiser, H. Steffen; Rosman, Kevin J. R.; Taylor, Philip D. P. (2003). "Atomic weights of the elements. Review 2000 (IUPAC Technical Report)". Pure and Applied Chemistry. 75 (6): 683–800. doi:10.1351/pac200375060683.
- Wieser, Michael E. (2006). "Atomic weights of the elements 2005 (IUPAC Technical Report)". Pure and Applied Chemistry. 78 (11): 2051–2066. doi:10.1351/pac200678112051.
- "News & Notices: Standard Atomic Weights Revised". International Union of Pure and Applied Chemistry. 19 October 2005.
- Half-life, spin, and isomer data selected from the following sources.
- Audi, Georges; Bersillon, Olivier; Blachot, Jean; Wapstra, Aaldert Hendrik (2003), "The NUBASE evaluation of nuclear and decay properties", Nuclear Physics A, 729: 3–128, Bibcode:2003NuPhA.729....3A, doi:10.1016/j.nuclphysa.2003.11.001
- National Nuclear Data Center. "NuDat 2.x database". Brookhaven National Laboratory.
- Holden, Norman E. (2004). "11. Table of the Isotopes". In Lide, David R. (ed.). CRC Handbook of Chemistry and Physics (85th ed.). Boca Raton, Florida: CRC Press. ISBN 978-0-8493-0485-9.
- ^ "Standard Atomic Weights: Iodine". CIAAW. 1985.
- ^ Prohaska, Thomas; Irrgeher, Johanna; Benefield, Jacqueline; Böhlke, John K.; Chesson, Lesley A.; Coplen, Tyler B.; Ding, Tiping; Dunn, Philip J. H.; Gröning, Manfred; Holden, Norman E.; Meijer, Harro A. J. (2022-05-04). "Standard atomic weights of the elements 2021 (IUPAC Technical Report)". Pure and Applied Chemistry. doi:10.1515/pac-2019-0603. ISSN 1365-3075.
- ^ "Nuclear Data Evaluation Lab". Archived from the original on 2007-01-21. Retrieved 2009-05-13.
- ^ Augustine George; James T Lane; Arlen D Meyers (January 17, 2013). "Radioactive Iodine Uptake Testing". Medscape.
- ^ V. R. Narra; et al. (1992). "Radiotoxicity of Some Iodine-123, Iodine-125, and Iodine-131-Labeled Compounds in Mouse Testes: Implications for Radiopharmaceutical Design" (PDF). Journal of Nuclear Medicine. 33 (12): 2196–201. PMID 1460515.
- ^ Boutrot, Freddy; Zipfel, Cyril (2017-08-04). "Function, Discovery, and Exploitation of Plant Pattern Recognition Receptors for Broad-Spectrum Disease Resistance". Annual Review of Phytopathology. 55 (1). Annual Reviews: 257–286. doi:10.1146/annurev-phyto-080614-120106. ISSN 0066-4286. PMID 28617654.
- ^ E. Rault; et al. (2007). "Comparison of Image Quality of Different Iodine Isotopes (I-123, I-124, and I-131)". Cancer Biotherapy & Radiopharmaceuticals. 22 (3): 423–430. doi:10.1089/cbr.2006.323. PMID 17651050.
- ^ BV Cyclotron VU, Amsterdam, 2016, Information on Iodine-124 for PET Archived 2017-10-26 at the Wayback Machine
- ^ Hertz, Barbara; Schuleller, Kristin (2010). "Saul Hertz, MD (1905 - 1950) A Pioneer in the Use of Radioactive Iodine". Endocrine Practice. 16 (4): 713–715. doi:10.4158/EP10065.CO. PMID 20350908.
- ^ Robbins, Jacob; Schneider, Arthur B. (2000). "Thyroid cancer following exposure to radioactive iodine". Reviews in Endocrine and Metabolic Disorders. 1 (3): 197–203. doi:10.1023/A:1010031115233. ISSN 1389-9155. PMID 11705004. S2CID 13575769.
- ^ "Frequently Asked Questions on Potassium Iodide". Food and Drug Administration. Retrieved 2009-06-06.
- ^ "Potassium Iodide as a Thyroid Blocking Agent in Radiation Emergencies". Federal Register. Food and Drug Administration. Archived from the original on 2011-10-02. Retrieved 2009-06-06.
