Fatty acid metabolism
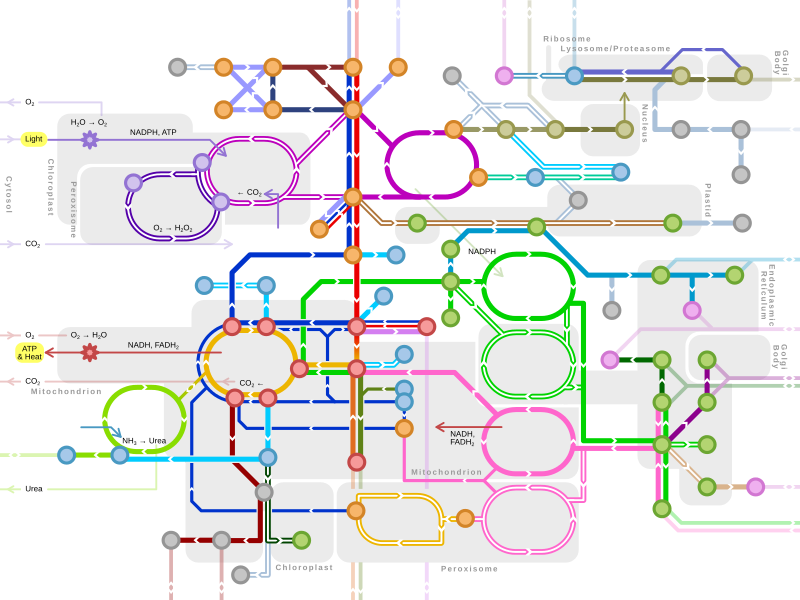
Fatty acid metabolism consists of various metabolic processes involving or closely related to fatty acids, a family of molecules classified within the lipid macronutrient category. These processes can mainly be divided into (1) catabolic processes that generate energy and (2) anabolic processes where they serve as building blocks for other compounds.[1]
In catabolism, fatty acids are metabolized to produce energy, mainly in the form of adenosine triphosphate (ATP). When compared to other macronutrient classes (carbohydrates and protein), fatty acids yield the most ATP on an energy per gram basis, when they are completely oxidized to CO2 and water by beta oxidation and the citric acid cycle.[2] Fatty acids (mainly in the form of triglycerides) are therefore the foremost storage form of fuel in most animals, and to a lesser extent in plants.
In anabolism, intact fatty acids are important precursors to triglycerides, phospholipids, second messengers, hormones and ketone bodies. For example, phospholipids form the phospholipid bilayers out of which all the membranes of the cell are constructed from fatty acids. Phospholipids comprise the plasma membrane and other membranes that enclose all the organelles within the cells, such as the nucleus, the mitochondria, endoplasmic reticulum, and the Golgi apparatus. In another type of anabolism, fatty acids are modified to form other compounds such as second messengers and local hormones. The prostaglandins made from arachidonic acid stored in the cell membrane are probably the best-known of these local hormones.
Fatty acid catabolism
[edit]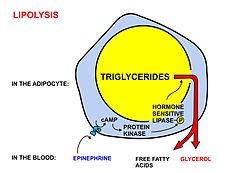


Fatty acids are stored as triglycerides in the fat depots of adipose tissue. Between meals they are released as follows:
- Lipolysis, the removal of the fatty acid chains from the glycerol to which they are bound in their storage form as triglycerides (or fats), is carried out by lipases. These lipases are activated by high epinephrine and glucagon levels in the blood (or norepinephrine secreted by sympathetic nerves in adipose tissue), caused by declining blood glucose levels after meals, which simultaneously lowers the insulin level in the blood.[1]
- Once freed from glycerol, the free fatty acids enter the blood, which transports them, attached to plasma albumin, throughout the body.[4]
- Long-chain free fatty acids enter metabolizing cells (i.e. most living cells in the body except red blood cells and neurons in the central nervous system) through specific transport proteins, such as the SLC27 family fatty acid transport protein.[5][6] Red blood cells do not contain mitochondria and are therefore incapable of metabolizing fatty acids; the tissues of the central nervous system cannot use fatty acids, despite containing mitochondria, because long-chain fatty acids (as opposed to medium-chain fatty acids[7][8]) cannot cross the blood-brain barrier[9] into the interstitial fluids that bathe these cells.
- Once inside the cell, long-chain-fatty-acid—CoA ligase catalyzes the reaction between a fatty acid molecule with ATP (which is broken down to AMP and inorganic pyrophosphate) to give a fatty acyl-adenylate, which then reacts with free coenzyme A to give a fatty acyl-CoA molecule.
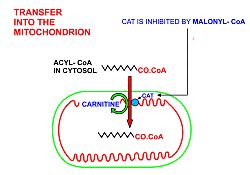
- In order for the acyl-CoA to enter the mitochondrion the carnitine shuttle is used:[10][11][12]
- Acyl-CoA is transferred to the hydroxyl group of carnitine by carnitine palmitoyltransferase I, located on the cytosolic faces of the outer and inner mitochondrial membranes.
- Acyl-carnitine is shuttled inside by a carnitine-acylcarnitine translocase, as a carnitine is shuttled outside.
- Acyl-carnitine is converted back to acyl-CoA by carnitine palmitoyltransferase II, located on the interior face of the inner mitochondrial membrane. The liberated carnitine is shuttled back to the cytosol, as an acyl-CoA is shuttled into the mitochondrial matrix.
- Beta oxidation, in the mitochondrial matrix, then cuts the long carbon chains of the fatty acids (in the form of acyl-CoA molecules) into a series of two-carbon (acetate) units, which, combined with co-enzyme A, form molecules of acetyl CoA, which condense with oxaloacetate to form citrate at the "beginning" of the citric acid cycle.[2] It is convenient to think of this reaction as marking the "starting point" of the cycle, as this is when fuel - acetyl-CoA - is added to the cycle, which will be dissipated as CO2 and H2O with the release of a substantial quantity of energy captured in the form of ATP, during the course of each turn of the cycle and subsequent oxidative phosphorylation.
- Briefly, the steps in beta oxidation are as follows:[2]
- Dehydrogenation by acyl-CoA dehydrogenase, yielding 1 FADH2
- Hydration by enoyl-CoA hydratase
- Dehydrogenation by 3-hydroxyacyl-CoA dehydrogenase, yielding 1 NADH + H+
- Cleavage by thiolase, yielding 1 acetyl-CoA and a fatty acid that has now been shortened by 2 carbons (forming a new, shortened acyl-CoA)
- This beta oxidation reaction is repeated until the fatty acid has been completely reduced to acetyl-CoA or, in the case of fatty acids with odd numbers of carbon atoms, acetyl-CoA and 1 molecule of propionyl-CoA per molecule of fatty acid. Each beta oxidative cut of the acyl-CoA molecule eventually yields 5 ATP molecules in oxidative phosphorylation.[13][14]
- The acetyl-CoA produced by beta oxidation enters the citric acid cycle in the mitochondrion by combining with oxaloacetate to form citrate. Coupled to oxidative phosphorylation this results in the complete combustion of the acetyl-CoA to CO2 and water. The energy released in this process is captured in the form of 1 GTP and 11 ATP molecules per acetyl-CoA molecule oxidized.[2][10] This is the fate of acetyl-CoA wherever beta oxidation of fatty acids occurs, except under certain circumstances in the liver.
- The propionyl-CoA is later converted into succinyl-CoA through biotin-dependant propionyl-CoA carboxylase (PCC) and Vitamin B12-dependant methylmalonyl-CoA mutase (MCM), sequentially.[15][16] Succinyl-CoA is first converted to malate, and then to pyruvate where it is then transported to the matrix to enter the citric acid cycle.
In the liver oxaloacetate can be wholly or partially diverted into the gluconeogenic pathway during fasting, starvation, a low carbohydrate diet, prolonged strenuous exercise, and in uncontrolled type 1 diabetes mellitus. Under these circumstances, oxaloacetate is hydrogenated to malate, which is then removed from the mitochondria of the liver cells to be converted into glucose in the cytoplasm of the liver cells, from where it is released into the blood.[10] In the liver, therefore, oxaloacetate is unavailable for condensation with acetyl-CoA when significant gluconeogenesis has been stimulated by low (or absent) insulin and high glucagon concentrations in the blood. Under these conditions, acetyl-CoA is diverted to the formation of acetoacetate and beta-hydroxybutyrate.[10] Acetoacetate, beta-hydroxybutyrate, and their spontaneous breakdown product, acetone, are frequently, but confusingly, known as ketone bodies (as they are not "bodies" at all, but water-soluble chemical substances). The ketones are released by the liver into the blood. All cells with mitochondria can take up ketones from the blood and reconvert them into acetyl-CoA, which can then be used as fuel in their citric acid cycles, as no other tissue can divert its oxaloacetate into the gluconeogenic pathway in the way that this can occur in the liver. Unlike free fatty acids, ketones can cross the blood–brain barrier and are therefore available as fuel for the cells of the central nervous system, acting as a substitute for glucose, on which these cells normally survive.[10] The occurrence of high levels of ketones in the blood during starvation, a low carbohydrate diet, prolonged heavy exercise, or uncontrolled type 1 diabetes mellitus is known as ketosis, and, in its extreme form, in out-of-control type 1 diabetes mellitus, as ketoacidosis.
- The glycerol released by lipase action is phosphorylated by glycerol kinase in the liver (the only tissue in which this reaction can occur), and the resulting glycerol 3-phosphate is oxidized to dihydroxyacetone phosphate. The glycolytic enzyme triose phosphate isomerase converts this compound to glyceraldehyde 3-phosphate, which is oxidized via glycolysis, or converted to glucose via gluconeogenesis.
Fatty acids as an energy source
[edit]
Fatty acids, stored as triglycerides in an organism, are a concentrated source of energy because they contain little oxygen and are anhydrous. The energy yield from a gram of fatty acids is approximately 9 kcal (37 kJ), much higher than the 4 kcal (17 kJ) for carbohydrates. Since the hydrocarbon portion of fatty acids is hydrophobic, these molecules can be stored in a relatively anhydrous (water-free) environment. Carbohydrates, on the other hand, are more highly hydrated. For example, 1 g of glycogen binds approximately 2 g of water, which translates to 1.33 kcal/g (4 kcal/3 g). This means that fatty acids can hold more than six times the amount of energy per unit of stored mass. Put another way, if the human body relied on carbohydrates to store energy, then a person would need to carry 31 kg (67.5 lb) of hydrated glycogen to have the energy equivalent to 4.6 kg (10 lb) of fat.[10]
Hibernating animals provide a good example for utilization of fat reserves as fuel. For example, bears hibernate for about 7 months, and during this entire period, the energy is derived from degradation of fat stores. Migrating birds similarly build up large fat reserves before embarking on their intercontinental journeys.[17]
The fat stores of young adult humans average between about 10–20 kg, but vary greatly depending on gender and individual disposition.[18] By contrast, the human body stores only about 400 g of glycogen, of which 300 g is locked inside the skeletal muscles and is unavailable to the body as a whole. The 100 g or so of glycogen stored in the liver is depleted within one day of starvation.[10] Thereafter the glucose that is released into the blood by the liver for general use by the body tissues has to be synthesized from the glucogenic amino acids and a few other gluconeogenic substrates, which do not include fatty acids.[1] Nonetheless, lipolysis releases glycerol which can enter the pathway of gluconeogenesis.
Carbohydrate synthesis from glycerol and fatty acids
[edit]Fatty acids are broken down to acetyl-CoA by means of beta oxidation inside the mitochondria, whereas fatty acids are synthesized from acetyl-CoA outside the mitochondria, in the cytosol. The two pathways are distinct, not only in where they occur, but also in the reactions that occur, and the substrates that are used. The two pathways are mutually inhibitory, preventing the acetyl-CoA produced by beta-oxidation from entering the synthetic pathway via the acetyl-CoA carboxylase reaction.[1] It can also not be converted to pyruvate as the pyruvate dehydrogenase complex reaction is irreversible.[10] Instead the acetyl-CoA produced by the beta-oxidation of fatty acids condenses with oxaloacetate, to enter the citric acid cycle. During each turn of the cycle, two carbon atoms leave the cycle as CO2 in the decarboxylation reactions catalyzed by isocitrate dehydrogenase and alpha-ketoglutarate dehydrogenase. Thus each turn of the citric acid cycle oxidizes an acetyl-CoA unit while regenerating the oxaloacetate molecule with which the acetyl-CoA had originally combined to form citric acid. The decarboxylation reactions occur before malate is formed in the cycle.[1] Only plants possess the enzymes to convert acetyl-CoA into oxaloacetate from which malate can be formed to ultimately be converted to glucose.[1]
However, acetyl-CoA can be converted to acetoacetate, which can decarboxylate to acetone (either spontaneously, or catalyzed by acetoacetate decarboxylase). It can then be further metabolized to isopropanol which is excreted in breath/urine, or by CYP2E1 into hydroxyacetone (acetol). Acetol can be converted to propylene glycol. This converts to pyruvate (by two alternative enzymes), or propionaldehyde, or to L-lactaldehyde then L-lactate (the common lactate isomer).[19][20][21] Another pathway turns acetol to methylglyoxal, then to pyruvate, or to D-lactaldehyde (via S-D-lactoyl-glutathione or otherwise) then D-lactate.[20][22][23] D-lactate metabolism (to glucose) is slow or impaired in humans, so most of the D-lactate is excreted in the urine; thus D-lactate derived from acetone can contribute significantly to the metabolic acidosis associated with ketosis or isopropanol intoxication.[20] L-Lactate can complete the net conversion of fatty acids into glucose. The first experiment to show conversion of acetone to glucose was carried out in 1951. This, and further experiments used carbon isotopic labelling.[21] Up to 11% of the glucose can be derived from acetone during starvation in humans.[21]
The glycerol released into the blood during the lipolysis of triglycerides in adipose tissue can only be taken up by the liver. Here it is converted into glycerol 3-phosphate by the action of glycerol kinase which hydrolyzes one molecule of ATP per glycerol molecule which is phosphorylated. Glycerol 3-phosphate is then oxidized to dihydroxyacetone phosphate, which is, in turn, converted into glyceraldehyde 3-phosphate by the enzyme triose phosphate isomerase. From here the three carbon atoms of the original glycerol can be oxidized via glycolysis, or converted to glucose via gluconeogenesis.[10]
Other functions and uses of fatty acids
[edit]Intracellular signaling
[edit]
Fatty acids are an integral part of the phospholipids that make up the bulk of the plasma membranes, or cell membranes, of cells. These phospholipids can be cleaved into diacylglycerol (DAG) and inositol trisphosphate (IP3) through hydrolysis of the phospholipid, phosphatidylinositol 4,5-bisphosphate (PIP2), by the cell membrane bound enzyme phospholipase C (PLC).[24]
Eicosanoid paracrine hormones
[edit]

One product of fatty acid metabolism are the prostaglandins, compounds having diverse hormone-like effects in animals. Prostaglandins have been found in almost every tissue in humans and other animals. They are enzymatically derived from arachidonic acid, a 20-carbon polyunsaturated fatty acid. Every prostaglandin therefore contains 20 carbon atoms, including a 5-carbon ring. They are a subclass of eicosanoids and form the prostanoid class of fatty acid derivatives.[25]
The prostaglandins are synthesized in the cell membrane by the cleavage of arachidonate from the phospholipids that make up the membrane. This is catalyzed either by phospholipase A2 acting directly on a membrane phospholipid, or by a lipase acting on DAG (diacyl-glycerol). The arachidonate is then acted upon by the cyclooxygenase component of prostaglandin synthase. This forms a cyclopentane ring roughly in the middle of the fatty acid chain. The reaction also adds 4 oxygen atoms derived from two molecules of O2. The resulting molecule is prostaglandin G2, which is converted by the hydroperoxidase component of the enzyme complex into prostaglandin H2. This highly unstable compound is rapidly transformed into other prostaglandins, prostacyclin and thromboxanes.[25] These are then released into the interstitial fluids surrounding the cells that have manufactured the eicosanoid hormone.
If arachidonate is acted upon by a lipoxygenase instead of cyclooxygenase, hydroxyeicosatetraenoic acids and leukotrienes are formed. They also act as local hormones.
Prostaglandins have two derivatives: prostacyclins and thromboxanes. Prostacyclins are powerful locally acting vasodilators and inhibit the aggregation of blood platelets. Through their role in vasodilation, prostacyclins are also involved in inflammation. They are synthesized in the walls of blood vessels and serve the physiological function of preventing needless clot formation, as well as regulating the contraction of smooth muscle tissue.[26] Conversely, thromboxanes (produced by platelet cells) are vasoconstrictors and facilitate platelet aggregation. Their name comes from their role in clot formation (thrombosis).
Dietary sources of fatty acids, their digestion, absorption, transport in the blood and storage
[edit]


A significant proportion of the fatty acids in the body are obtained from the diet, in the form of triglycerides of either animal or plant origin. The fatty acids in the fats obtained from land animals tend to be saturated, whereas the fatty acids in the triglycerides of fish and plants are often polyunsaturated and therefore present as oils.
These triglycerides cannot be absorbed by the intestine.[27] They are broken down into mono- and di-glycerides plus free fatty acids (but no free glycerol) by pancreatic lipase, which forms a 1:1 complex with a protein called colipase (also a constituent of pancreatic juice), which is necessary for its activity. The activated complex can work only at a water-fat interface. Therefore, it is essential that fats are first emulsified by bile salts for optimal activity of these enzymes.[28] The digestion products consisting of a mixture of tri-, di- and monoglycerides and free fatty acids, which, together with the other fat soluble contents of the diet (e.g. the fat soluble vitamins and cholesterol) and bile salts form mixed micelles, in the watery duodenal contents (see diagrams on the right).[27][29]
The contents of these micelles (but not the bile salts) enter the enterocytes (epithelial cells lining the small intestine) where they are resynthesized into triglycerides, and packaged into chylomicrons which are released into the lacteals (the capillaries of the lymph system of the intestines).[30] These lacteals drain into the thoracic duct which empties into the venous blood at the junction of the left jugular and left subclavian veins on the lower left hand side of the neck. This means that the fat-soluble products of digestion are discharged directly into the general circulation, without first passing through the liver, unlike all other digestion products. The reason for this peculiarity is unknown.[31]

The chylomicrons circulate throughout the body, giving the blood plasma a milky or creamy appearance after a fatty meal.[citation needed] Lipoprotein lipase on the endothelial surfaces of the capillaries, especially in adipose tissue, but to a lesser extent also in other tissues, partially digests the chylomicrons into free fatty acids, glycerol and chylomicron remnants. The fatty acids are absorbed by the adipocytes[citation needed], but the glycerol and chylomicron remnants remain in the blood plasma, ultimately to be removed from the circulation by the liver. The free fatty acids released by the digestion of the chylomicrons are absorbed by the adipocytes[citation needed], where they are resynthesized into triglycerides using glycerol derived from glucose in the glycolytic pathway[citation needed]. These triglycerides are stored, until needed for the fuel requirements of other tissues, in the fat droplet of the adipocyte.
The liver absorbs a proportion of the glucose from the blood in the portal vein coming from the intestines. After the liver has replenished its glycogen stores (which amount to only about 100 g of glycogen when full) much of the rest of the glucose is converted into fatty acids as described below. These fatty acids are combined with glycerol to form triglycerides which are packaged into droplets very similar to chylomicrons, but known as very low-density lipoproteins (VLDL). These VLDL droplets are processed in exactly the same manner as chylomicrons, except that the VLDL remnant is known as an intermediate-density lipoprotein (IDL), which is capable of scavenging cholesterol from the blood. This converts IDL into low-density lipoprotein (LDL), which is taken up by cells that require cholesterol for incorporation into their cell membranes or for synthetic purposes (e.g. the formation of the steroid hormones). The remainder of the LDLs is removed by the liver.[32]
Adipose tissue and lactating mammary glands also take up glucose from the blood for conversion into triglycerides. This occurs in the same way as in the liver, except that these tissues do not release the triglycerides thus produced as VLDL into the blood. Adipose tissue cells store the triglycerides in their fat droplets, ultimately to release them again as free fatty acids and glycerol into the blood (as described above), when the plasma concentration of insulin is low, and that of glucagon and/or epinephrine is high.[33] Mammary glands discharge the fat (as cream fat droplets) into the milk that they produce under the influence of the anterior pituitary hormone prolactin.
All cells in the body need to manufacture and maintain their membranes and the membranes of their organelles. Whether they rely entirely on free fatty acids absorbed from the blood, or are able to synthesize their own fatty acids from blood glucose, is not known. The cells of the central nervous system will almost certainly have the capability of manufacturing their own fatty acids, as these molecules cannot reach them through the blood–brain barrier.[34] However, it is unknown how they are reached by the essential fatty acids, which mammals cannot synthesize themselves but are nevertheless important components of cell membranes (and other functions described above).
Fatty acid synthesis
[edit]
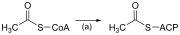
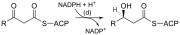
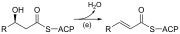
Much like beta-oxidation, straight-chain fatty acid synthesis occurs via the six recurring reactions shown below, until the 16-carbon palmitic acid is produced.[35][36]
The diagrams presented show how fatty acids are synthesized in microorganisms and list the enzymes found in Escherichia coli.[35] These reactions are performed by fatty acid synthase II (FASII), which in general contains multiple enzymes that act as one complex. FASII is present in prokaryotes, plants, fungi, and parasites, as well as in mitochondria.[37]
In animals as well as some fungi such as yeast, these same reactions occur on fatty acid synthase I (FASI), a large dimeric protein that has all of the enzymatic activities required to create a fatty acid. FASI is less efficient than FASII; however, it allows for the formation of more molecules, including "medium-chain" fatty acids via early chain termination.[37] Enzymes, acyltransferases and transacylases, incorporate fatty acids in phospholipids, triacylglycerols, etc. by transferring fatty acids between an acyl acceptor and donor. They also have the task of synthesizing bioactive lipids as well as their precursor molecules.[38]
Once a 16:0 carbon fatty acid has been formed, it can undergo a number of modifications, resulting in desaturation and/or elongation. Elongation, starting with stearate (18:0), is performed mainly in the endoplasmic reticulum by several membrane-bound enzymes. The enzymatic steps involved in the elongation process are principally the same as those carried out by fatty acid synthesis, but the four principal successive steps of the elongation are performed by individual proteins, which may be physically associated.[39][40]
| Step | Enzyme | Reaction | Description |
|---|---|---|---|
| (a) | Acetyl-CoA:ACP transacylase | Activates acetyl-CoA for reaction with malonyl-ACP | |
| (b) | Malonyl-CoA:ACP transacylase | Activates malonyl-CoA for reaction with acetyl-ACP | |
| (c) | 3-ketoacyl-ACP synthase | 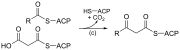 |
Reacts ACP-bound acyl chain with chain-extending malonyl-ACP |
| (d) | 3-ketoacyl-ACP reductase | Reduces the carbon 3 ketone to a hydroxyl group | |
| (e) | 3-Hydroxyacyl ACP dehydrase | Eliminates water | |
| (f) | Enoyl-ACP reductase | Reduces the C2-C3 double bond. |
Abbreviations: ACP – Acyl carrier protein, CoA – Coenzyme A, NADP – Nicotinamide adenine dinucleotide phosphate.
Note that during fatty synthesis the reducing agent is NADPH, whereas NAD is the oxidizing agent in beta-oxidation (the breakdown of fatty acids to acetyl-CoA). This difference exemplifies a general principle that NADPH is consumed during biosynthetic reactions, whereas NADH is generated in energy-yielding reactions.[34] (Thus NADPH is also required for the synthesis of cholesterol from acetyl-CoA; while NADH is generated during glycolysis.) The source of the NADPH is two-fold. When malate is oxidatively decarboxylated by “NADP+-linked malic enzyme" pyruvate, CO2 and NADPH are formed. NADPH is also formed by the pentose phosphate pathway which converts glucose into ribose, which can be used in synthesis of nucleotides and nucleic acids, or it can be catabolized to pyruvate.[34]
Glycolytic end products are used in the conversion of carbohydrates into fatty acids
[edit]In humans, fatty acids are formed from carbohydrates predominantly in the liver and adipose tissue, as well as in the mammary glands during lactation. The pyruvate produced by glycolysis is an important intermediary in the conversion of carbohydrates into fatty acids and cholesterol.[34] This occurs via the conversion of pyruvate into acetyl-CoA in the mitochondrion. However, this acetyl-CoA needs to be transported into cytosol where the synthesis of fatty acids and cholesterol occurs. This cannot occur directly. To obtain cytosolic acetyl-CoA, citrate (produced by the condensation of acetyl-CoA with oxaloacetate) is removed from the citric acid cycle and carried across the inner mitochondrial membrane into the cytosol.[34] There it is cleaved by ATP citrate lyase into acetyl-CoA and oxaloacetate. The oxaloacetate is returned to mitochondrion as malate (and then converted back into oxaloacetate to transfer more acetyl-CoA out of the mitochondrion).[41] The cytosolic acetyl-CoA is carboxylated by acetyl-CoA carboxylase into malonyl-CoA, the first committed step in the synthesis of fatty acids.[41][42]
Regulation of fatty acid synthesis
[edit]Acetyl-CoA is formed into malonyl-CoA by acetyl-CoA carboxylase, at which point malonyl-CoA is destined to feed into the fatty acid synthesis pathway. Acetyl-CoA carboxylase is the point of regulation in saturated straight-chain fatty acid synthesis, and is subject to both phosphorylation and allosteric regulation. Regulation by phosphorylation occurs mostly in mammals, while allosteric regulation occurs in most organisms. Allosteric control occurs as feedback inhibition by palmitoyl-CoA and activation by citrate. When there are high levels of palmitoyl-CoA, the final product of saturated fatty acid synthesis, it allosterically inactivates acetyl-CoA carboxylase to prevent a build-up of fatty acids in cells. Citrate acts to activate acetyl-CoA carboxylase under high levels, because high levels indicate that there is enough acetyl-CoA to feed into the Krebs cycle and produce energy.[43]
High plasma levels of insulin in the blood plasma (e.g. after meals) cause the dephosphorylation and activation of acetyl-CoA carboxylase, thus promoting the formation of malonyl-CoA from acetyl-CoA, and consequently the conversion of carbohydrates into fatty acids, while epinephrine and glucagon (released into the blood during starvation and exercise) cause the phosphorylation of this enzyme, inhibiting lipogenesis in favor of fatty acid oxidation via beta-oxidation.[34][42]
Disorders
[edit]Disorders of fatty acid metabolism can be described in terms of, for example, hypertriglyceridemia (too high level of triglycerides), or other types of hyperlipidemia. These may be familial or acquired.
Familial types of disorders of fatty acid metabolism are generally classified as inborn errors of lipid metabolism. These disorders may be described as fatty acid oxidation disorders or as a lipid storage disorders, and are any one of several inborn errors of metabolism that result from enzyme or transport protein defects affecting the ability of the body to oxidize fatty acids in order to produce energy within muscles, liver, and other cell types. When a fatty acid oxidation disorder affects the muscles, it is a metabolic myopathy.
Moreover, cancer cells can display irregular fatty acid metabolism with regard to both fatty acid synthesis[44] and mitochondrial fatty acid oxidation (FAO)[45] that are involved in diverse aspects of tumorigenesis and cell growth.
References
[edit]- ^ a b c d e f Stryer, Lubert (1995). "Fatty acid metabolism.". In: Biochemistry (Fourth ed.). New York: W.H. Freeman and Company. pp. 603–628. ISBN 0-7167-2009-4.
- ^ a b c d Oxidation of fatty acids
- ^ Zechner R, Strauss JG, Haemmerle G, Lass A, Zimmermann R (2005). "Lipolysis: pathway under construction". Curr. Opin. Lipidol. 16 (3): 333–40. doi:10.1097/01.mol.0000169354.20395.1c. PMID 15891395. S2CID 35349649.
- ^ Mobilization and cellular uptake of stored fats (triacylglycerols) (with animation)
- ^ Stahl, Andreas (1 February 2004). "A current review of fatty acid transport proteins (SLC27)". Pflügers Archiv: European Journal of Physiology. 447 (5): 722–727. doi:10.1007/s00424-003-1106-z. PMID 12856180. S2CID 2769738.
- ^ Anderson, Courtney M.; Stahl, Andreas (April 2013). "SLC27 fatty acid transport proteins". Molecular Aspects of Medicine. 34 (2–3): 516–528. doi:10.1016/j.mam.2012.07.010. PMC 3602789. PMID 23506886.
- ^ Ebert, D.; Haller, RG.; Walton, ME. (Jul 2003). "Energy contribution of octanoate to intact rat brain metabolism measured by 13C nuclear magnetic resonance spectroscopy". J Neurosci. 23 (13): 5928–35. doi:10.1523/JNEUROSCI.23-13-05928.2003. PMC 6741266. PMID 12843297.
- ^ Marin-Valencia, I.; Good, LB.; Ma, Q.; Malloy, CR.; Pascual, JM. (Feb 2013). "Heptanoate as a neural fuel: energetic and neurotransmitter precursors in normal and glucose transporter I-deficient (G1D) brain". J Cereb Blood Flow Metab. 33 (2): 175–82. doi:10.1038/jcbfm.2012.151. PMC 3564188. PMID 23072752.
- ^ Stryer, Lubert (1995). "Fatty acid metabolism.". In: Biochemistry (Fourth ed.). New York: W.H. Freeman and Company. pp. 770–771. ISBN 0-7167-2009-4.
- ^ a b c d e f g h i Stryer, Lubert (1995). Biochemistry (Fourth ed.). New York: W.H. Freeman and Company. pp. 510–515, 581–613, 775–778. ISBN 0-7167-2009-4.
- ^ Activation and transportation of fatty acids to the mitochondria via the carnitine shuttle (with animation)
- ^ Vivo, Darryl C.; Bohan, Timothy P.; Coulter, David L.; Dreifuss, Fritz E.; Greenwood, Robert S.; Nordli, Douglas R.; Shields, W. Donald; Stafstrom, Carl E.; Tein, Ingrid (1998). "l-Carnitine Supplementation in Childhood Epilepsy: Current Perspectives". Epilepsia. 39 (11): 1216–1225. doi:10.1111/j.1528-1157.1998.tb01315.x. ISSN 0013-9580. PMID 9821988. S2CID 28692799.
- ^ Oxidation of odd carbon chain length fatty acids
- ^ Oxidation of unsaturated fatty acids
- ^ Wongkittichote P, Ah Mew N, Chapman KA (December 2017). "Propionyl-CoA carboxylase - A review". Molecular Genetics and Metabolism. 122 (4): 145–152. doi:10.1016/j.ymgme.2017.10.002. PMC 5725275. PMID 29033250.
- ^ Halarnkar PP, Blomquist GJ (1989). "Comparative aspects of propionate metabolism". Comp. Biochem. Physiol. B. 92 (2): 227–31. doi:10.1016/0305-0491(89)90270-8. PMID 2647392.
- ^ Stryer, Lubert (1995). Biochemistry (Fourth ed.). New York: W.H. Freeman and Company. p. 777. ISBN 0-7167-2009-4.
- ^ Sloan, A.W; Koeslag, J.H.; Bredell, G.A.G. (1973). "Body composition work capacity and work efficiency of active and inactive young men". European Journal of Applied Physiology. 32: 17–24. doi:10.1007/bf00422426. S2CID 39812342.
- ^ Ruddick JA (1972). "Toxicology, metabolism, and biochemistry of 1,2-propanediol". Toxicol Appl Pharmacol. 21 (1): 102–111. Bibcode:1972ToxAP..21..102R. doi:10.1016/0041-008X(72)90032-4. PMID 4553872.
- ^ a b c Glew, Robert H. "You Can Get There From Here: Acetone, Anionic Ketones and Even-Carbon Fatty Acids can Provide Substrates for Gluconeogenesis". Nigerian Journal of Physiological Science. 25 (1). Invited review: 2–4. Archived from the original on 26 September 2013. Retrieved 7 August 2016.
- ^ a b c Park, Sung M.; Klapa, Maria I.; Sinskey, Anthony J.; Stephanopoulos, Gregory (1999). "Metabolite and isotopomer balancing in the analysis of metabolic cycles: II. Applications" (PDF). Biotechnology and Bioengineering. 62 (4): 398. doi:10.1002/(sici)1097-0290(19990220)62:4<392::aid-bit2>3.0.co;2-s. ISSN 0006-3592. PMID 9921151.
- ^ Miller DN, Bazzano G; Bazzano (1965). "Propanediol metabolism and its relation to lactic acid metabolism". Ann NY Acad Sci. 119 (3): 957–973. Bibcode:1965NYASA.119..957M. doi:10.1111/j.1749-6632.1965.tb47455.x. PMID 4285478. S2CID 37769342.
- ^ D. L. Vander Jagt; B. Robinson; K. K. Taylor; L. A. Hunsaker (1992). "Reduction of trioses by NADPH-dependent aldo-keto reductases. Aldose reductase, methylglyoxal, and diabetic complications". The Journal of Biological Chemistry. 267 (7): 4364–4369. doi:10.1016/S0021-9258(18)42844-X. PMID 1537826.
- ^ Stryer, Lubert (1995). "Signal transduction cascades.". In: Biochemistry (Fourth ed.). New York: W.H. Freeman and Company. pp. 343–350. ISBN 0-7167-2009-4.
- ^ a b Stryer, Lubert (1995). "Eicosanoid hormones are derived from fatty acids.". In: Biochemistry (Fourth ed.). New York: W.H. Freeman and Company. pp. 624–627. ISBN 0-7167-2009-4.
- ^ Nelson, Randy F. (2005). An introduction to behavioral endocrinology (3rd ed.). Sunderland, Mass: Sinauer Associates. p. 100. ISBN 978-0-87893-617-5.
- ^ a b Digestion of fats (triacylglycerols)
- ^ Hofmann AF (1963). "The function of bile salts in fat absorption. The solvent properties of dilute micellar solutions of conjugated bile salts". Biochem. J. 89 (1): 57–68. doi:10.1042/bj0890057. PMC 1202272. PMID 14097367.
- ^ Stryer, Lubert (1995). "Membrane structures and dynamics.". In: Biochemistry (Fourth ed.). New York: W.H. Freeman and Company. pp. 268–270. ISBN 0-7167-2009-4.
- ^ Gropper, Sareen S.; Smith, Jack L. (2013). Advanced nutrition and human metabolism (6th ed.). Belmont, CA: Wadsworth/Cengage Learning. ISBN 978-1133104056.
- ^ Williams, Peter L.; Warwick, Roger; Dyson, Mary; Bannister, Lawrence H. (1989). "Angiology.". In: Gray's Anatomy (Thirty-seventh ed.). Edinburgh: Churchill Livingstone. pp. 841–843. ISBN 0443-041776.
- ^ Stryer, Lubert (1995). "Biosynthesis of membrane lipids and steroids.". In: Biochemistry (Fourth ed.). New York: W.H. Freeman and Company. pp. 697–700. ISBN 0-7167-2009-4.
- ^ Stralfors, Peter; Honnor, Rupert C. (1989). "Insulin-induced dephosphorylation of hormone-sensitive lipase". European Journal of Biochemistry. 182 (2): 379–385. doi:10.1111/j.1432-1033.1989.tb14842.x. PMID 2661229.
- ^ a b c d e f Stryer, Lubert (1995). Biochemistry (Fourth ed.). New York: W.H. Freeman and Company. pp. 559–565, 614–623. ISBN 0-7167-2009-4.
- ^ a b Dijkstra, Albert J., R. J. Hamilton, and Wolf Hamm. "Fatty Acid Biosynthesis." Trans Fatty Acids. Oxford: Blackwell Pub., 2008. 12. Print.
- ^ "MetaCyc pathway: superpathway of fatty acids biosynthesis". MetaCyc Metabolic Pathway Database. BioCyc. (E. coli).
- ^ a b Christie, William W. (20 April 2011). "Fatty Acids: Straight-chain Saturated, Structure, Occurrence and Biosynthesis". In American Oil Chemists' Society (ed.). AOCS Lipid Library. Archived from the original on 2011-07-21. Retrieved 2011-05-02.
- ^ Yamashita, Atsushi; Hayashi, Yasuhiro; Nemoto-Sasaki, Yoko; Ito, Makoto; Oka, Saori; Tanikawa, Takashi; Waku, Keizo; Sugiura, Takayuki (2014-01-01). "Acyltransferases and transacylases that determine the fatty acid composition of glycerolipids and the metabolism of bioactive lipid mediators in mammalian cells and model organisms". Progress in Lipid Research. 53: 18–81. doi:10.1016/j.plipres.2013.10.001. ISSN 0163-7827. PMID 24125941.
- ^ "MetaCyc pathway: stearate biosynthesis I (animals)". MetaCyc Metabolic Pathway Database. BioCyc.
- ^ "MetaCyc pathway: very long chain fatty acid biosynthesis II". MetaCyc Metabolic Pathway Database. BioCyc.
- ^ a b Ferre, P.; F. Foufelle (2007). "SREBP-1c Transcription Factor and Lipid Homeostasis: Clinical Perspective". Hormone Research. 68 (2): 72–82. doi:10.1159/000100426. PMID 17344645. Retrieved 2010-08-30.
this process is outlined graphically in page 73
- ^ a b Voet, Donald; Judith G. Voet; Charlotte W. Pratt (2006). Fundamentals of Biochemistry, 2nd Edition. John Wiley and Sons, Inc. pp. 547, 556. ISBN 978-0-471-21495-3.
- ^ Diwan, Joyce J. "Fatty Acid Synthesis." Rensselaer Polytechnic Institute (RPI) :: Architecture, Business, Engineering, IT, Humanities, Science. Web. 30 Apr. 2011. <"Fatty Acid Synthesis". Archived from the original on 2011-06-07. Retrieved 2011-05-02.>.
- ^ Ezzeddini R, Taghikhani M, Somi MH, Samadi N, Rasaee, MJ (May 2019). "Clinical importance of FASN in relation to HIF-1α and SREBP-1c in gastric adenocarcinoma". Life Sciences. 224: 169–176. doi:10.1016/j.lfs.2019.03.056. PMID 30914315. S2CID 85532042.
- ^ Ezzeddini R, Taghikhani M, Salek Farrokhi A, Somi MH, Samadi N, Esfahani A, Rasaee, MJ (May 2021). "Downregulation of fatty acid oxidation by involvement of HIF-1α and PPARγ in human gastric adenocarcinoma and its related clinical significance". Journal of Physiology and Biochemistry. 77 (2): 249–260. doi:10.1007/s13105-021-00791-3. ISSN 1138-7548. PMID 33730333. S2CID 232300877.